Abstract
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification, based on percent predicted forced expiratory volume in 1 s (ppFEV1), has been widely adopted for assessment of chronic obstructive pulmonary disease (COPD) severity. However, the STaging of Airflow obstruction by Ratio (STAR) system, based on the ratio of FEV1 to forced vital capacity, was recently proposed as an alternative classification. This study aimed to compare the prognostic performance of the GOLD and STAR classifications for prediction of mortality and exacerbation risk in individuals with COPD. This 5-year prospective, multicenter cohort study enrolled 370 individuals with COPD at 29 medical centers. All-cause mortality risk across GOLD and STAR stages was evaluated with Kaplan-Meier curves and Cox proportional hazards models. The risk of moderate to severe COPD exacerbations across GOLD and STAR stages was examined with cumulative incidence function (CIF) curves and Fine and Gray models. Both classification systems showed a significant association with mortality and exacerbation risk (P < 0.01 for trend). The GOLD classification provided a better separation of Kaplan-Meier and CIF curves for advanced stages, whereas the STAR classification showed a clearer distinction between stages I and II. These associations remained consistent after multivariable adjustments. The GOLD classification was superior for prediction of prognosis in advanced COPD, whereas the STAR classification provided better differentiation in early-stage disease. These findings highlight the complementary roles of the GOLD and STAR classifications in assessment of COPD severity.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a progressive respiratory disorder associated with a risk of exacerbation and mortality, with accurate assessment of its severity being essential for optimization of treatment strategy and the appropriate allocation of medical resources1. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification is based on percent predicted forced expiratory volume in 1 s (ppFEV1) and has been widely adopted for such assessment1. Several studies have shown that GOLD staging, or its defining factor ppFEV1, is strongly associated with mortality risk2,3,4,5. However, the lack of a significant survival difference between patients with COPD stage I and healthy individuals6,7 is a key limitation of this classification that has raised concerns about its sensitivity for capturing disease severity at early stages.
The STaging of Airflow obstruction by Ratio (STAR) system, based on the ratio of FEV1 to forced vital capacity (FVC), was recently proposed as an alternative classification for COPD severity6. This system may better reflect early-stage airflow limitation because it identifies COPD stage I patients as having worse survival than healthy individuals. However, few studies have directly assessed the prognostic performance of the GOLD and STAR classifications for COPD patients. Large-scale cohort studies have reported similar prediction abilities for overall survival (OS) between the two classifications6,7,8, whereas a single-center study suggested that GOLD provided better separation of survival curves across stages9. It has therefore remained unclear which system more effectively predicts COPD outcome.
Given this background, we aimed to evaluate and compare the prognostic performance of the GOLD and STAR classifications in a multicenter cohort of COPD patients according to a 5-year prospective study design.
Methods
Study design and population
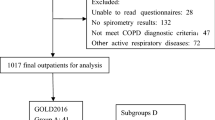
This prospective, multicenter observational study was performed at 29 general hospitals in the Fukuoka Tobacco-Related Lung Disease registry study group10,11,12. The cohort initially included 374 individuals with COPD who were aged ≥ 20 years, consented to participate in the study between 1 September 2013 and 30 April 2016, and were followed longitudinally for 5 years. After exclusion of four individuals without smoking pack-year information, the remaining 370 patients were enrolled in the study. COPD was diagnosed according to the criteria of GOLD, with a cutoff based on an FEV1/FVC ratio of < 70%1. Participants were divided into four groups on the basis of GOLD stage: stage I (n = 57), ppFEV1 ≥ 80%; stage II (n = 137), 50% ≤ ppFEV1 < 80%; stage III (n = 109), 30% ≤ ppFEV1 < 50%; and stage IV (n = 67), ppFEV1 < 30%1. They were also analyzed by assignment to four additional groups according to STAR grading: stage I (n = 87), 60% ≤ FEV1/FVC < 70%; stage II (n = 98), 50% ≤ FEV1/FVC < 60%; stage III (n = 88), 40% ≤ FEV1/FVC < 50%; and stage IV (n = 97), FEV1/FVC < 40%6. The distributions of patients by disease severity according to GOLD and STAR stages are shown in Figure S1 in the Supporting Information.
Clinical evaluation and laboratory measurements
Each participant completed a self-administered questionnaire regarding their smoking habits, inhalational treatment, and history of asthma. On the basis of smoking habits, individuals were categorized as never smokers or current/former smokers. Given that smoking exposure levels were not normally distributed, we established three groups: 0 pack years, 0 < pack years < 20, and ≥20 pack years. Information on the presence or absence of prescriptions for inhaled corticosteroid (ICS) and long-acting bronchodilator (LABD) medications was collected with regard to inhalation therapy. LABDs included long-acting muscarinic antagonists (LAMAs) and long-acting β2-agonists (LABAs). Body mass index (BMI) was calculated as body weight/height2. Pulmonary function tests were performed according to the guidelines of the American Thoracic Society/European Respiratory Society13, with all values recorded without bronchodilator inhalation. Predicted values of FEV1 were calculated with a reference equation provided by the Japan Respiratory Society in 201414. Blood tests were performed at the time of study inclusion to obtain data on C-reactive protein (CRP) concentration. Positive CRP status was defined as a CRP level of ≥ 0.30 mg/dL15. Follow-up surveillance was conducted annually for 5 years to assess mortality. Causes of death were evaluated and classified into six categories: respiratory disease, cardiovascular disease (CVD), infectious disease, primary lung cancer, other malignancies, and other/unspecified causes. Respiratory disease–related deaths included exacerbation of COPD and pneumonia, given that they often overlapped, making it difficult to determine definitively which was the actual cause of death. Deaths due to infectious disease did not include pneumonia-related mortality. CVD-related deaths were defined as deaths resulting from myocardial infarction, chronic heart failure, pulmonary hypertension, aortic disease, or other cardiovascular events. Neoplasm-related deaths were divided into deaths from primary lung cancer and other malignancies. Moderate or severe exacerbations of COPD were defined as exacerbation events of COPD requiring the use of systemic steroids or antibiotics (or both), according to GOLD criteria1. Among the 303 patients with available modified Medical Research Council scale data, the age, dyspnea, and airflow obstruction (ADO) index was calculated16, and patients were classified into four groups according to ADO quartiles: 0–3, 4, 5, and ≥ 6. A modified ADO (mADO) index, in which the FEV1/FVC ratio was used instead of ppFEV16, was also assessed in the same population, and patients were similarly categorized into four groups based on mADO quartiles: 0–3, 4, 5, and ≥ 6.
Statistical analysis
All statistical analysis was performed with R software version 4.4.0 (R Foundation for Statistical Computing, Vienna, Austria). A two-sided P value of < 0.05 was considered to indicate statistical significance. For baseline characteristics, heterogeneity among COPD severity stages (GOLD and STAR stages) was evaluated with the chi-square test (or Monte Carlo simulations), one-way analysis of variance, or the Kruskal-Wallis test. Concordance between the GOLD and STAR severity classification schemes was assessed descriptively with a Bangdiwala plot and quantified for agreement between multiple classes with the weighted Bangdiwala B value, which adjusts for the frequency of each severity class17,18. Kaplan-Meier curves were constructed to depict OS for each GOLD stage group. Linear trends in the association between GOLD stages and OS were estimated as hazard ratios (HRs) and 95% confidence intervals (CIs) with both unadjusted and multivariable-adjusted Cox proportional hazards models. Adjustments were made for age, sex, BMI, smoking exposure level, use of an ICS, use of an LABD, history of asthma, and CRP level. Pairwise comparisons of mortality risk between groups were performed with Bonferroni correction to account for multiple comparisons. Given that post hoc comparisons were performed for six pairs in the four-group analysis (among GOLD stages I–IV), the 95% CIs were adjusted to 99.17% with Bonferroni correction. A trend in the relation between the GOLD classification and cause-specific death rates was evaluated with Cox proportional hazards models. Mortality due to respiratory disease, the leading cause of death in the cohort, was examined across GOLD stages with multivariable-adjusted Cox proportional hazards models, and with post hoc pairwise comparisons being conducted with the use of Bonferroni correction. With consideration of death as a competing risk, cumulative incidence function (CIF) curves were generated to depict the incidence of moderate or severe exacerbation across GOLD stage groups. The association between the GOLD classification and the risk of moderate or severe exacerbation of COPD was estimated as a subdistribution hazard ratio (SHR) with the Fine and Gray proportional subdistribution hazards model. For multivariable adjustment, the adjustment factors were the same as those adopted in the Cox proportional hazards analysis mentioned above. Post hoc pairwise comparisons were performed with Bonferroni correction. In the same manner, we investigated the association between STAR stages and mortality or exacerbation risk with application of the relevant models.
Stratified analysis according to the presence or absence of inhalation therapy was conducted, accounting for differences in usage frequency across the severity stages of the GOLD and STAR classifications. In the multivariable-adjusted Cox proportional hazards analysis, all of the aforementioned potential confounders, with the exception of prescriptions for ICS and LABD medications, were included. When investigating the associations of the ADO and mADO indices with all-cause mortality and exacerbation risk, Cox proportional hazards models and Fine–Gray proportional subdistribution hazards models were used. Adjustments were made for sex, BMI, smoking exposure level, use of an ICS, use of an LABD, history of asthma, and CRP level. Age was not included as a covariate because it is already incorporated into both the ADO and mADO indices. Post hoc pairwise comparisons were conducted with Bonferroni correction.
Results
Demographic and clinical characteristics stratified by GOLD stage
Table S1 in the Supporting Information summarizes the demographic and clinical characteristics of the study cohort. The majority of subjects were male, had a history of smoking, and were prescribed LABD. Approximately half of the cohort were users of ICS. The mean values of ppFEV1 and FEV1/FVC were 53.9% and 48.9%, respectively.
Stratification of the study cohort according to GOLD severity stages revealed that mean BMI decreased progressively from stages I to IV (23.2, 22.3, 21.7, and 20.3 kg/m2, respectively; P < 0.01 for heterogeneity) (Table 1). The frequency of individuals with a history of asthma was highest for stage III and lowest for stage I (8.8%, 15.3%, 26.6%, and 14.9% for stages I–IV, respectively; P = 0.01 for heterogeneity). ICS and LABD mediations were prescribed more frequently in stages III and IV (ICS, 65.1% and 74.6%; LABD, 96.3% and 94.0%, respectively) compared with stages I and II (ICS, 29.8% and 39.4%; LABD, 77.2% and 89.1%, respectively), with P < 0.01 for heterogeneity in each instance. With regard to LABD prescriptions, higher disease stages were associated with an increased preference for LAMA/LABA combination therapy over LAMA or LABA monotherapy. Mean values of FEV1, ppFEV1, and FEV1/FVC decreased with stage progression (P < 0.01 for heterogeneity in each case). The proportions of males and smokers, mean age, median smoking pack-years, and CRP level did not differ significantly among stages.
Demographic and clinical characteristics stratified by STAR stage
Demographic and clinical characteristics according to STAR severity stages are summarized in Table 2. Similar to the results for the GOLD classification, mean values of BMI, FEV1, ppFEV1, and FEV1/FVC decreased progressively from STAR stages I to IV (P < 0.01 for heterogeneity in each instance). Prescriptions for ICS and LABD mediations also increased significantly with STAR stage progression (ICS, 33.3%, 43.9%, 58.0%, and 71.1%; LABD, 81.6%, 89.8%, 92.0%, and 96.9% for stages I–IV, respectively, with P < 0.01 for heterogeneity in each case). As the STAR stage increased, a greater proportion of patients were prescribed LAMA/LABA combination therapy. Unlike the GOLD classification, however, no significant difference was apparent among STAR stages for the frequency of individuals with a history of asthma (P = 0.33 for heterogeneity). There were also no statistically significant differences in age, sex distribution, smoking exposure, or CRP level.
A Bangdiwala plot for agreement between GOLD and STAR severity stages is shown in Figure S2 in the Supporting Information. The agreement (weighted Bandiwala B value) between the two classification systems was 0.85.
Association between GOLD and STAR stages and mortality
The median follow-up period was 5.0 years, and 48 participants (13.0% of the entire cohort) died during follow-up. The all-cause mortality rate (per 1000 person-years) for GOLD stages I to IV was 11.6, 11.7, 34.7, and 87.6, respectively. Kaplan-Meier curves (Fig. 1A) revealed a significant trend for all-cause mortality among GOLD stages (P < 0.01 for trend). OS for stages I, II, or III was significantly longer than that for stage IV (adjusted P value of < 0.01 for stages I and II and of 0.02 for stage III versus stage IV). However, Kaplan-Meier curves for stages I and II overlapped substantially. The tendency for death rate across GOLD stages was broadly consistent regardless of prescription status for inhalation therapy, with P < 0.01 for trend in each instance (Figure S3 in the Supporting Information). Among individuals receiving inhaler treatment, the mortality rate for stages I, II, or III was more favorable than that for stage IV (adjusted P value of 0.04 for stage I, < 0.01 for stage II, and 0.03 for stage III versus stage IV), although the survival curve for stage I was paradoxically below that for stage II.
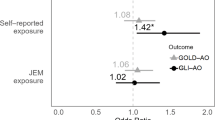
Cox proportional hazards analysis adjusted for multiple variables revealed that the association between OS and GOLD stages remained significant (P < 0.01 for trend). Compared with stage IV, multivariable-adjusted HRs for stages I to III were all significantly lower (HR [adjusted CI] and adjusted P of 0.13 [0.02–0.77] and 0.01, 0.12 [0.03–0.41] and < 0.01, and 0.34 [0.14–0.83] and < 0.01, respectively) (Fig. 2).
Multivariable-adjusted HRs for all-cause mortality across GOLD and STAR stages. Adjustments were made for age, sex, body mass index, smoking exposure, use of inhaled corticosteroids, use of long-acting bronchodilators, history of asthma, and C-reactive protein level. As a result of a nonnormal distribution, smoking exposure was categorized into three groups: 0 pack-years, 0 < pack-years < 20, and ≥20 pack-years. C-reactive protein levels were dichotomized as ≥ 0.30 or < 0.30 mg/dL on the basis of their nonnormal distribution. Abbreviations: HR, hazard ratio; CI, confidence interval; GOLD, Global Initiative for Chronic Obstructive Lung Disease; STAR, STaging of Airflow obstruction by Ratio.
Cause-specific mortality according to GOLD stage is summarized in Table S2 in the Supporting Information. Most deaths were related to respiratory disease, the death rate for which increased with stage progression (3.9, 3.4, 13.0, and 51.8 per 1000 person-years for stages I–IV, respectively; P < 0.01 for trend). This positive trend in the association of the GOLD classification with respiratory disease–related death remained apparent after multivariable adjustment (P < 0.01 for trend). The multivariable-adjusted HRs for stages II and III were significantly lower than that for stage IV (HR [adjusted CI] and adjusted P of 0.08 [0.01–0.66] and 0.10, and 0.25 [0.06–0.99] and 0.048 for stages II and III, respectively) (Figure S4 in the Supporting Information).
Regarding the STAR classification, all-cause mortality rate (per 1000 person-years) was 13.1, 21.6, 32.5, and 54.9 for stages I to IV, respectively. As was the case for the GOLD classification system, there was a significant trend for OS according to STAR stages (P < 0.01 for trend). Of note, and in contrast to the results for GOLD stages, the survival curve for STAR stage I was mostly higher than that for stage II, although the difference was not statistically significant. Bonferroni-adjusted P values for all-cause death rates relative to stage IV were 0.02 for stage I, 0.11 for stage II, and 0.84 for stage III (Fig. 1B). A similar trend in death rates was observed across STAR stages regardless of prescription status for inhalation therapy (P < 0.01 for trend among individuals with inhalation therapy, and P = 0.02 for trend among those without), although no statistically significant differences were observed between stages I, II, or III and stage IV (Figure S5 in the Supporting Information).
The positive linear association between STAR stages and all-cause mortality was robust after adjustment for possible confounders (P < 0.01 for trend). Although multivariable-adjusted HRs for stages I to III were not significantly decreased compared with stage IV, a gradual progression of HRs was apparent (Fig. 2).
The incidence of respiratory disease–related death, which accounted for most mortality, also increased significantly with STAR stage progression (P < 0.01 for trend) (Table S3 in the Supporting Information). This positive trend also remained significant after multivariable adjustment (P < 0.01 for trend). However, the HRs for stages I, II, and III were not significantly different from that for stage IV (Figure S4 in the Supporting Information).
Association between GOLD and STAR stages and exacerbation risk
During the follow-up period, 91 individuals (24.6% of the cohort) experienced moderate to severe exacerbations of COPD. Similar to the case for OS, CIF curves revealed a positive trend for the cumulative incidence of exacerbations among GOLD stages (P < 0.01 for trend; adjusted P < 0.01 for stages I, II, or III versus stage IV), although the CIF curves for stages I and II were closely aligned (Fig. 3A). The results remained unchanged after multivariable adjustment, with the multivariable-adjusted SHRs for stages I, II, and III being significantly lower than that for stage IV (SHR [adjusted CI] and adjusted P of 0.11 [0.02–0.51] and < 0.01, 0.13 [0.05–0.35] and < 0.01, and 0.40 [0.20–0.79] and < 0.01 for stages I–III, respectively; P < 0.01 for trend) (Fig. 4).
Cumulative incidence function curves for the probability of moderate to severe COPD exacerbations according to GOLD (A) or STAR (B) severity stages. Abbreviations: COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease; STAR, STaging of Airflow obstruction by Ratio.
Multivariable-adjusted SHRs for moderate to severe COPD exacerbations across GOLD and STAR stages. Adjustments were made for age, sex, body mass index, smoking exposure, use of inhaled corticosteroids, use of long-acting bronchodilators, history of asthma, and C-reactive protein level. As a result of a nonnormal distribution, smoking exposure levels were categorized into three groups: 0 pack-years, 0 < pack-years < 20, and ≥20 pack-years. C-reactive protein levels were dichotomized as ≥ 0.30 or < 0.30 mg/dL on the basis of their nonnormal distribution. Abbreviations: COPD, chronic obstructive pulmonary disease; SHR, subdistribution hazard ratio; CI, 95% confidence interval; GOLD, Global Initiative for Chronic Obstructive Lung Disease; STAR, STaging of Airflow obstruction by Ratio.
The CIF curves for STAR stages also revealed a positive trend (P < 0.01 for trend), with the CIF curve for stage II being distinctly separated from that for stage I and positioned higher (Fig. 3B). Multivariable-adjusted SHRs also increased gradually with STAR stage progression (P < 0.01 for trend), although only the SHR for stage I was significantly lower than that for stage IV (SHR [adjusted CI] of 0.26 [0.08–0.85]) (Fig. 4).
Association of ADO and mADO indices with morbidity and mortality
In subjects with available ADO and mADO index data (n = 303), Kaplan–Meier curves, multivariable-adjusted HRs for all-cause mortality, CIF curves, and multivariable-adjusted SHRs for moderate to severe exacerbations of COPD stratified by quartiles of each index are presented in Figures S6–S9 of the Supporting Information, respectively. When stratified by ADO index quartiles, the Kaplan–Meier survival curves and forest plots of multivariable-adjusted HRs for all-cause mortality appeared similar to those based on the GOLD classification (Figs. 1A and 2), with limited separation between stages I and II. Conversely, the CIF curves and forest plots of multivariable-adjusted SHRs for COPD exacerbations showed more visually apparent differences in prognosis between stages I and II compared to the GOLD classification (Figs. 3A and 4). However, no significant differences were found between the highest (ADO index ≥ 6) and second-highest (ADO index = 5) quartile groups (crude analysis: adjusted P = 0.29; multivariable-adjusted analysis: adjusted P = 0.89). The survival and morbidity patterns observed using mADO index quartiles resembled those of the STAR classification (Figs. 1B, 2 and 3B, and 4), particularly in that clear visual differences were observed between the lowest (mADO index = 0–3) and third-highest (mADO index = 4) quartile groups. However, in contrast to the STAR classification, the distinction between the second-highest (mADO index = 5) and third-highest (mADO index = 4) quartile groups was less pronounced.
Discussion
Our study has revealed significant associations of both GOLD and STAR classifications with mortality and the incidence of moderate to severe exacerbations in individuals with COPD. In the case of the GOLD classification, significant differences in all-cause mortality rate and the cumulative incidence of exacerbations were apparent for stage IV versus stages II and III as well as stage I. In contrast, the STAR classification provided a clearer distinction between stages I and II, as reflected in both the Kaplan-Meier and CIF curves. As far as we are aware, our study is the first to prospectively evaluate differences in prognostic performance between the GOLD and STAR classifications in COPD patients.
Few previous studies have statistically evaluated and compared the prognostic characteristics of the GOLD and STAR classifications for COPD. Large-scale cohort studies—namely the COPDGene Study and the combined Pittsburgh cohort—as well as population-based research, specifically the Rotterdam Study and the National Health and Nutrition Examination Survey, have reported descriptively similar prognostic performance for the GOLD and STAR classifications, although statistical analysis was not performed6,7,8. On the other hand, a single-center study in Japan indicated that the GOLD classification delineated survival curves more distinctly across stages, which enhanced its prognostic reliability, compared with the STAR classification9. Which staging system is superior has therefore remained unresolved. In addition, in these previous studies, excluding the COPDGene Study and Pittsburgh cohort, subjects with COPD were classified into three groups (stage I, stage II, and stages III–IV) because of the relatively small number of participants with COPD of GOLD or STAR stage III or IV. It was therefore difficult to assess differences in prognostic value between GOLD or STAR stages III and IV. In the present study, the GOLD classification showed more pronounced differences in prognosis between stage IV and stages II and III, whereas the STAR classification demonstrated better separation between stages I and II. These findings highlight the importance of selective utilization of the GOLD and STAR classifications to improve the prediction of survival outcome in COPD.
We identified positive trends across stages for both the GOLD and STAR systems with relation to the risk of moderate to severe COPD exacerbations, mirroring the trends apparent for mortality. These results are consistent with previous studies of the GOLD system19,20. In contrast, only one previous study has examined the association between STAR stages and exacerbation risk6, and its results were consistent with ours. Given that exacerbation events are well-established surrogate markers for mortality in COPD1,21, it has been reasonable to assume that STAR stages, like GOLD stages, are also associated with exacerbation risk.
We found that the STAR classification provided clearer distinctions in prognosis between stage I and stage II, whereas the GOLD classification more effectively distinguished the prognosis of more advanced stages. With regard to pulmonary function in individuals with COPD, ppFEV1 tends to decline slowly during the early stages as a result of lung hyperinflation, whereas FVC increases, leading to a noticeable reduction in the FEV1/FVC ratio22,23. In contrast, as the disease progresses, an accelerated decline in FVC occurs as a result of increasing residual volume, leading to a slower decline in FEV1/FVC, whereas ppFEV1 decreases markedly together with FVC24. STAR, the FEV1/FVC-based classification, may therefore more sensitively reflect prognostic gradients in early-stage COPD, whereas GOLD, the ppFEV1-based classification, may more effectively capture these gradients in advanced-stage COPD.
The strengths of our study include a relatively balanced distribution of a large number of participants across GOLD and STAR stages I to IV and an extended follow-up period, which together provided a robust framework for evaluation of long-term prognosis. However, there are also several potential limitations of our study. First, both ppFEV1 and FEV1/FVC values were based on a single measurement, which may have led to misclassification of GOLD and STAR stages and attenuated the observed associations, potentially biasing the results toward the null hypothesis. Second, it was possible that some participants had asthma-COPD overlap, given that lung function was measured without bronchodilator administration and data on type 2 inflammation biomarkers (such as blood eosinophil count) were unavailable. However, asthma was adequately differentiated by respiratory specialists during cohort enrollment, and a history of asthma was included as a covariate in the multivariable adjustment model. This limitation is therefore not likely to have altered the study conclusions. Third, as a consequence of the study design, the frequency of inhaler prescriptions was uneven across stages—the earlier the stage, the lower the frequency—regardless of whether the system adopted was GOLD or STAR. This situation might have improved the prognosis of patients with advanced-stage COPD, potentially attenuating the associations observed in the present study. However, the OS trends across both GOLD and STAR stages remained broadly consistent regardless of inhaler prescription status, suggesting that the impact of this limitation on the study results was likely minimal. Fourth, given that the study was not a randomized controlled trial, residual confounding cannot be entirely ruled out. However, the consistency of results after multivariable adjustment is suggestive of a minimal impact on the findings. Fifth, the limited number of deaths from nonrespiratory causes, including CVD and lung cancer, may have restricted the ability to fully assess prognostic differences among GOLD or STAR stages for cause-specific mortality beyond respiratory disease–related deaths. Sixth, we categorized all users of LAMA, LABA, and LAMA/LABA therapies into a single group of LABD users. This approach may have obscured differences in treatment effects, as LAMA/LABA combination therapy has been shown to be more effective than monotherapy in reducing exacerbations25,26. However, in both the GOLD and STAR classifications, the proportion of patients receiving LAMA/LABA increased with the advancing disease stage; the true effect of LABD may have been underestimated in our analysis due to the fact that all LABD therapies were grouped together. Therefore, the overall impact of this potential limitation on our findings is likely to be minor. Lastly, due to the lack of data on 6-minute walk distance, we were unable to assess the BMI, airflow obstruction, dyspnea, and exercise capacity (BODE) index for each patient. Instead of the BODE index, we investigated the associations of the ADO and mADO indices with morbidity and mortality in COPD, which demonstrated a certain degree of similarity to the GOLD and STAR stages, respectively. We are currently planning further research to explore the prognostic value of various markers, including but not limited to the ADO and mADO indices.
Conclusions
In conclusion, our study suggests that the GOLD classification is more effective for prediction of prognosis in advanced-stage COPD, whereas the STAR classification provides valuable insights into early-stage disease. These findings underscore the complementary roles of the GOLD and STAR classification systems in COPD prognosis. Further research is warranted to explore how these systems can be integrated or selectively applied to improve prognostic accuracy and inform treatment strategies.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- COPD:
-
chronic obstructive pulmonary disease
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- pp:
-
percent predicted
- FEV1 :
-
forced expiratory volume in 1 s
- STAR:
-
STaging of Airflow obstruction by Ratio
- FVC:
-
forced vital capacity
- OS:
-
overall survival
- ICS:
-
inhaled corticosteroid
- LABD:
-
long-acting bronchodilator
- LAMA:
-
long-acting muscarinic antagonists
- LABA:
-
long-acting β2-agonists
- BMI:
-
body mass index
- CRP:
-
C-reactive protein
- CVD:
-
cardiovascular disease
- ADO:
-
age, dyspnea, and airflow obstruction
- mADO:
-
modified ADO
- HR:
-
hazard ratio
- 95% CI:
-
95% confidence interval
- CIF:
-
cumulative incidence function
- SHR:
-
subdistribution hazard ratio
- BODE:
-
BMI, airflow obstruction, dyspnea, and exercise capacity
References
Agustí, A. et al. Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am. J. Respir Crit. Care Med. 207, 819–837 (2023).
Tejero, E. et al. Classification of airflow limitation based on z-score underestimates mortality in patients with chronic obstructive pulmonary disease. Am. J. Respir Crit. Care Med. 196, 298–305 (2017).
Cadham, C. J. et al. The prevalence and mortality risks of prism and COPD in the united states from NHANES 2007–2012. Respir Res. 25, 1–11 (2024).
Hansen, E. F., Phanareth, K., Laursen, L. C., Kok-Jensen, A. & Dirksen, A. Reversible and irreversible airflow obstruction as predictor of overall mortality in asthma and chronic obstructive pulmonary disease. Am. J. Respir Crit. Care Med. 159, 1267–1271 (1999).
Oga, T., Nishimura, K., Tsukino, M., Sato, S. & Hajiro, T. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health status. Am. J. Respir Crit. Care Med. 167, 544–549 (2003).
Bhatt, S. P. et al. FEV1/FVC severity stages for chronic obstructive pulmonary disease. Am. J. Respir Crit. Care Med. 208, 676–684 (2023).
Bertels, X., Riemann, S., Vauterin, D., Lahousse, L. & Brusselle, G. G. All-cause mortality of staging of airflow obstruction by ratio-categorized patients with chronic obstructive pulmonary disease among the general population. Am. J. Respir Crit. Care Med. 210, 1374–1376 (2024).
Backman, H., Vanfleteren, L. E. G. W., Mannino, D. M. & Ekström, M. Severity of airflow obstruction based on FEV1/FVC vs FEV1% predicted in the general U.S. Population. Am. J. Respir Crit. Care Med. 210, 1308–1316 (2024).
Nishimura, K., Kusunose, M., Shibayama, A. & Nakayasu, K. Comparison of disease severity classifications of chronic obstructive pulmonary disease: GOLD vs. STAR in clinical practice. Diagnostics 14, 1–11 (2024).
Ogata-Suetsugu, S. et al. Characteristics of tobacco-related lung diseases in fukuoka prefecture, japan: a prospective, multi-institutional, observational study. Respir Investig. 58, 74–80 (2020).
Tsubouchi, K. et al. Survival and acute exacerbation for patients with idiopathic pulmonary fibrosis (IPF) or non-IPF idiopathic interstitial pneumonias: 5-year follow-up analysis of a prospective multi-institutional patient registry. BMJ Open. Respir Res. 10, e001864 (2023).
Takano, T. et al. Update of prognosis and characteristics of chronic obstructive pulmonary disease in a real-world setting: a 5-year follow-up analysis of a multi-institutional registry. BMC Pulm Med. 24, 556 (2024).
Graham, B. L. et al. Standardization of spirometry 2019 update. An official american thoracic society and european respiratory society technical statement. Am. J. Respir Crit. Care Med. 200, E70–E88 (2019).
Kubota, M. et al. Reference values for spirometry, including vital capacity, in japanese adults calculated with the LMS method and compared with previous values. Respir Investig. 52, 242–250 (2014).
Shine, B., de Beer, F. C. & Pepys, M. B. Solid phase radioimmunoassays for human C-reactive protein. Clin. Chim. Acta. 117, 13–23 (1981).
Puhan, M. A. et al. Expansion of the prognostic assessment of patients with chronic obstructive pulmonary disease: the updated BODE index and the ADO index. Lancet 374, 704–711 (2009).
Bangdiwala, S. I., Haedo, A. S., Natal, M. L. & Villaveces, A. The agreement chart as an alternative to the receiver-operating characteristic curve for diagnostic tests. J. Clin. Epidemiol. 61, 866–874 (2008).
Bangdiwala, S. I. & Shankar, V. The agreement chart. BMC Med. Res. Methodol. 13, 97 (2013).
Han, M. K. et al. Frequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohort. Lancet Respir Med. 5, 619–626 (2017).
Hurst, J. R. et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl. J. Med. 363, 1128–1138 (2010).
Soler-Cataluña, J. J. et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 60, 925–931 (2005).
Deesomchok, A. et al. Lung hyperinflation and its reversibility in patients with airway obstruction of varying severity. COPD J. Chronic Obstr. Pulm Dis. 7, 428–437 (2010).
Gagnon, P. et al. Walking exercise response to bronchodilation in mild COPD: a randomized trial. Respir Med. 106, 1695–1705 (2012).
Culver, B. H. Obstructive? Restrictive? Or a ventilatory impairment? Chest 140, 568–569 (2011).
Wedzicha, J. A. et al. Tiotropium/olodaterol decreases exacerbation rates compared with tiotropium in a range of patients with COPD: pooled analysis of the TONADO®/DYNAGITO® trials. Adv. Ther. 37, 4266–4279 (2020).
Sion, K. Y. J., Huisman, E. L., Punekar, Y. S., Naya, I. & Ismaila, A. S. A network meta-analysis of long-acting muscarinic antagonist (LAMA) and long-acting β2-agonist (LABA) combinations in COPD. Pulm Ther. 3, 297–316 (2017).
Acknowledgements
We thank the study patients, their families, and all of the investigators participating in the Fukuoka Tobacco-Related Lung Disease (FOLD) registry group, as well as Clinical Research Support Center Kyushu for their official work on the study.
Funding
This study was supported by a grant from the Ministry of Education, Culture, Sports, Science and Technology of Japan; by the Broad-Area, Network-Based Project to Drive Clinical Research at Kyushu University Hospital; by a grant to the Diffuse Lung Diseases Research Group from the Ministry of Health, Labor, and Welfare of Japan; and by a grant from the Clinical Research Promotion Foundation 2024 of Japan.
Author information
Authors and Affiliations
Contributions
H.O., K. Tsubouchi, T.T., and I.O. contributed to the literature search, figure preparation, study design, data collection, data analysis, data interpretation, and writing of the manuscript. Y.N. contributed to the literature search, study design, data collection, and data interpretation. K.I., R.T., S.T., N.N., M.Y., Y.K., K. Tobino, E.H., H.W., H.I., T.M., M.K., M.F., K.Y., and Y.Z. contributed to the literature search, data collection, and data interpretation. All authors approved the final version of the manuscript. H.O. accepts full responsibility for the work and conduct of the study, had access to the data, and controlled the decision to publish.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This prospective, multicenter observational study was approved by the Institutional Review Board of Kyushu University (#25–135, 23 August 2013; #555-00, 27 August 2013) and by the institutional review boards of all participating hospitals. Written informed consent was obtained from all participants. All study procedures were performed according to the ethical standards in the Declaration of Helsinki.
Competing interests
K.Tsubouchi has received grants from Nippon Boehringer Ingelheim. S.T. has received personal fees from AstraZeneca, Boehringer Ingelheim Japan, Novartis Pharma, Sanofi, Bristol-Meyers Squibb, GlaxoSmithKline, Teijin Pharma, and Kyorin Pharmaceutical. K.Y. has received grants and personal fees from Chugai Pharmaceutical Co, Eli Lilly Japan K.K., TAIHO Phamaceutical Co., Ltd., Daiichi Sankyo Company, Limited., Shionogi & Co., Ltd., Insmed Incorporated., Nippon Boehringer Ingelheim Co. Ltd., Takeda Pharmaceutical Company Limited., and GlaxoSmithKline K.K.; grants from Sumitomo Pharma Co., Ltd., Kyowa Kirin Co., Ltd., FUJIFILM Toyama Chemical Co., Ltd., and TEIJIN HEALTHCARE LIMITED.; and personal fees from Sanofi K.K., KYORIN Pharmaceutical Co.,Ltd., Novartis Pharma K.K., Teijin Home Healthcare Limited., Asahi Kasei Pharma Corporation., AstraZeneca K.K., ONO PHARMACEUTICAL CO., LTD., MSD K.K, TOA EIYO LTD., and Meiji Seika Pharma Co., Ltd. Y.Z. has received personal fees from Nippon Boehringer Ingelheim Co. Ltd. I.O. has received grants and personal fees from Daiichi Sankyo, Chugai Pharma, Eli Lilly Japan, AstraZeneca, Taiho Pharmaceutical, Nippon Boehringer Ingelheim, and Ono Pharmaceutical; grants from Bristol-Myers Squibb and MSD Oncology; and personal fees from Takeda Pharmaceutical and Novartis Pharma. All other authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ogata, H., Tsubouchi, K., Takano, T. et al. Mortality and exacerbation risk according to GOLD and STAR severity stages of COPD: a 5-year multicenter prospective cohort study. Sci Rep 15, 19097 (2025). https://doi.org/10.1038/s41598-025-05033-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-05033-w