Abstract
The correlation between body mass index (BMI) and the outcomes for patients receiving surgical intervention for abdominal aortic aneurysm (AAA) is still debated. Consequently, this study seeks to investigate the association between BMI and mortality following elective open abdominal aortic aneurysm repair (EOAR). This study involves a secondary analysis derived from data collected in a prospective cohort framework. It focuses on individuals who received EOAR across ten vascular surgery centers in Denmark from January 1, 2000, to December 31, 2014. The analysis employed a Cox proportional hazards regression model to examine the connection between BMI and mortality following EOAR. To detect any potential nonlinear associations, Cox regression with cubic spline functions and smooth curve fitting was utilized. Furthermore, we performed numerous sensitivity and subgroup evaluations to ensure the reliability of our results. Upon controlling confounding variables, the analysis demonstrated a clear inverse correlation between BMI and mortality following EOAR. Specifically, each 1 kg/m² increase in BMI corresponded to a 2.7% reduction in mortality risk (HR = 0.973; 95% CI: 0.958–0.988). Compared to individuals with normal weight, those classified as underweight faced a 62.6% higher risk of mortality (HR = 1.626; 95% CI: 1.142–2.314), whereas overweight and obese individuals experienced a reduction in mortality risk by 18.2% (HR = 0.818; 95% CI: 0.722–0.928) and 15.8% (HR = 0.842; 95% CI: 0.721–0.998), respectively. Additionally, the study identified a nonlinear relationship between BMI and postoperative mortality, with a critical point at a BMI of 25.78 kg/m². Below this inflection point, each 1 kg/m² decrease in BMI significantly increased mortality risk by 8% (HR = 0.920; 95% CI: 0.893–0.949). Beyond this inflection point, further increases in BMI did not significantly impact mortality risk. In patients undergoing EOAR, an increase in BMI is significantly negatively associated with postoperative mortality. Additionally, a specific nonlinear relationship exists between BMI and postoperative mortality, with a BMI inflection point at 25.78 kg/m². Clinicians should carefully weigh surgical risks for patients with a BMI under 25.78 kg/m² and consider delaying surgery to enhance nutrition. In contrast, those overweight or obese may not require pre-surgery weight management.
Similar content being viewed by others
Introduction
Abdominal Aortic Aneurysm (AAA) is a vascular disorder associated with aging, characterized by pathological expansion and persistent weakening of the aortic wall1. It ranks among the most prevalent aneurysm types, bearing high incidence and mortality risk23,; with about 5% prevalence in the general population4. In Western countries, approximately 9% of adults over the age of 65 are affected by AAA, leading to a significant number of deaths5. Annually, AAA accounts for an estimated 150,000 to 200,000 deaths worldwide, creating considerable social and economic burdens6. The primary treatment for AAA is surgical intervention, primarily through endovascular abdominal aortic aneurysm repair (EVAR) or open abdominal aortic aneurysm repair (OAR). Identifying prognostic predictive markers for surgical intervention in AAA patients is crucial for risk stratification, informed clinical decision-making, and accurate prognosis evaluation. Key prognostic factors for patients undergoing AAA surgery include age, type of surgical intervention, obesity, diabetes, cardiac conditions, and hypertension7,8,9.
On a global scale, the increasing prevalence of obesity has become a pressing concern for public health. As a critical risk factor, obesity contributes to the development of a wide range of chronic illnesses, including diabetes, hypertension, non-alcoholic fatty liver disease, kidney disorders, and cardiovascular conditions10,11,12. Interestingly, research has identified an unexpected relationship between obesity and clinical outcomes in certain patient populations, where a higher body mass index (BMI) appears to confer a survival advantage, while a lower BMI is linked to poorer outcomes13,14. This counterintuitive phenomenon, known as the “obesity paradox,” was first identified in the groundbreaking work of Gruberg and colleagues in 200215. Their investigation revealed that individuals with elevated body mass and coronary artery disease demonstrated markedly reduced mortality compared to their leaner counterparts. This paradox has also been noted in the context of AAA disease16. For instance, a meta-analysis by Naiem et al. highlighted a lower 30-day mortality rate for obese patients undergoing EVAR compared to non-obese patients17. Similarly, a Korean cohort study suggested that individuals with a higher body mass index (BMI ≥ 25 kg/m²) had improved overall survival following elective open abdominal aortic aneurysm repair (EOAR)18. However, findings that challenge the obesity paradox exist. For example, two studies utilizing the Vascular Quality Initiative (VQI) database explored the BMI-prognosis relationship for OAR. One study found that both low (BMI < 18.5) and high (BMI > 34) BMI were linked to increased mortality19 while another indicated that very low (BMI < 18.5) and very high (BMI ≥ 40) BMI were associated with greater 30-day mortality for both EVAR and EOAR20. Additionally, a meta-analysis pointed out that obesity is not a risk factor for short-term mortality after AAA repair compared to non-obese individuals21. Some research even suggests obesity markedly raises the mortality risk following AAA repair22. Therefore, the relationship between obesity and the prognosis after AAA repair remains highly controversial, necessitating further comprehensive research and in-depth understanding.
It is crucial to recognize that most research predominantly utilizes linear regression to assess the association between BMI and outcomes of AAA repair, with limited focus on exploring nonlinear dynamics. These studies also vary significantly in terms of timing, surgical methods, BMI ranges, gender proportions, and adjustment variables. Consequently, there is a need for further investigation into the association between BMI and prognosis after AAA repair. This study seeks to investigate both linear and nonlinear associations between BMI and postoperative mortality in patients undergoing EOAR, leveraging data from a Danish cohort study.
Methods
Data source and study population
This cohort study examined data from individuals who underwent EOAR across 10 vascular surgery centers in Denmark, covering the period from January 1, 2000, to December 31, 201423. The dataset was sourced from a published article titled “Red blood cell transfusion associated with increased morbidity and mortality in patients undergoing elective open abdominal aortic aneurysm repair.” As stipulated by the Creative Commons Attribution-NonCommercial (CC BY-NC 4.0) license, this open-access article allows for distribution, reproduction, modification, and the creation of derivative works, provided that appropriate credit is given to the original authors and source23.
The initial cohort consisted of 10,599 individuals listed in the Danish Vascular Registry (Karbase). Of these, 6,683 were excluded for various reasons23. The original study’s exclusion criteria included: (i) patients with suprarenal, iliac, symptomatic, ruptured, mycotic, dissecting, pseudo-, or thrombotic aneurysms (n = 4,885); (ii) cases with incomplete data or duplicates (n = 423); and (iii) patients who underwent EVAR(n = 1,405). Consequently, the original study retained 3,876 individuals who underwent EOAR. In our analysis, we further excluded participants lacking BMI records (n = 498). This resulted in a final sample size of 3,378 participants for our study. The participant selection process is illustrated in Fig. 1.
Ethical approval
Data for this study were sourced from the Danish Vascular Registry (Karbase), a comprehensive national database in Denmark documenting all vascular surgeries. The initial study and the subsequent data extraction received authorization from the Danish Data Protection Agency (Datatilsynet), under approval number 2015-41-4135, adhering to the Helsinki Declaration’s principles. Since all personal identifiers were fully anonymized, the Danish Data Protection Agency specified that informed consent was unnecessary for using this data. Consequently, this secondary analysis does not require further ethical approval23.
Body mass index
BMI is measured as a continuous variable, calculated using the formula: BMI = weight/height2 (kg/m2). It is pertinent to mention that height and weight data were recorded at baseline. Based on the World Health Organization’s obesity classification, participants were categorized as follows: underweight (BMI < 18.5 kg/m2), normal weight (18.5 ≤ BMI < 25 kg/m2), overweight (25 ≤ BMI < 30 kg/m2), and obese (BMI ≥ 30 kg/m2)24.
Endpoint events
The primary outcome of this study was the long-term survival status (15 years post-surgery) of patients undergoing EOAR, expressed as a binary variable (0 for survival, 1 for mortality). Survival status was determined on July 1, 2015, using data from the Danish Civil Registration System (CPR)23.
Collection and definition of covariates
In this study, covariates were chosen based on a combination of established research and clinical expertise23,25. Included among these covariates were age, sex, preoperative hemoglobin (HGB) levels, total blood transfusions, perioperative serum creatinine (Scr), perioperative bleeding, and the American Society of Anesthesiologists (ASA) score. Additionally, data were collected on smoking and documented cerebrovascular diseases, cardiac disease, diabetes mellitus (DM), hypertension, and respiratory diseases. Cerebrovascular disease was defined as a history of transient ischemic attack (TIA) or stroke. Cardiac disease was defined as a history of acute myocardial infarction, stable/unstable angina, or having undergone cardiac surgery, including percutaneous coronary intervention. Anemia was defined as HGB levels less than 134 g/L in men or less than 118 g/L in women. Respiratory diseases included ongoing treatment for lung diseases and experiencing shortness of breath while speaking or at rest. Moreover, data on postoperative complications, such as issues with respiration and cardiac function, intestinal ischemia, dialysis, and embolic disorders, were collected23.
Handling missing data
Missing data often presents a challenge in observational studies and is generally unavoidable. In this analysis, missing data were noted for variables such as DM (16 cases, 0.47%), respiratory diseases (19 cases, 0.56%), hypertension (30 cases, 0.89%), cerebrovascular diseases (30 cases, 0.89%), cardiac diseases (32 cases, 0.95%), Scr (75 cases, 2.22%), perioperative bleeding (7 cases, 0.21%) smoking status (34 cases, 1.01%), HGB (88 cases, 2.61%), cardiac complications(6 cases, 0.18%), pulmonary complications(6 cases, 0.18%), intestinal ischemia(11 cases, 0.33%), and ASA score (284 cases, 8.41%). To address the potential bias introduced by these missing variables, a multiple imputation technique was employed26,27. For this process, a linear regression imputation model with 10 iterations was used, incorporating variables such as age, sex, HGB, Scr, perioperative bleeding, total blood transfusion, smoking status, heart and cerebrovascular diseases, hypertension, DM, respiratory conditions, ASA score, along with postoperative in-hospital complications (respiratory and cardiac issues, ischemic bowel disease, hemodialysis, embolic disease). The imputation assumed that the data was missing at random (MAR)27.
Statistical analysis
The analysis of the study data was conducted using R software (version 3.4.5) alongside Empower Stats (version 4.2), establishing a significance threshold at P < 0.05 for two-sided tests. Participants were classified into four BMI categories—underweight, normal weight, overweight, and obese—based on the World Health Organization’s obesity criteria. Categorical variables are summarized as counts and percentages, whereas continuous variables are expressed either as medians with interquartile ranges or means with standard deviations. To assess differences among the BMI categories, the Kruskal-Wallis H test was applied for non-normally distributed data, one-way ANOVA for normally distributed data, and the chi-square test for categorical variables.
To thoroughly investigate the link between BMI and postoperative mortality in patients undergoing EOAR, a series of multivariable Cox proportional hazard models were constructed with sequential adjustments for various factors. The outcomes are reported as hazard ratios (HR) with 95% confidence intervals (CI). Model I did not adjust for any variables. Model II adjusted for age, sex, and smoking status. Model III further expanded the range of adjustments to include age, sex, perioperative bleeding, hypertension, DM, smoking status, hemoglobin HGB, Scr, ASA score, total transfusion volume, cardiac and cerebrovascular diseases, intestinal ischemia, cardiac and pulmonary complications, and embolic events. The variables used for multivariable adjustment were primarily selected based on the results of univariable analysis, previous studies, and clinical expertise20,21,23,25.
To ensure the robustness of our findings, we conducted three sensitivity analyses based on the fully adjusted Model III:(i). Sensitivity Analysis 1 omitted participants diagnosed with DM at the start of the study. (ii). Sensitivity Analysis 2 excluded those with hypertension at baseline. (iii). Sensitivity Analysis 3 considered only participants who did not have cardiac disease. Moreover, to evaluate the potential impact of unmeasured confounding on the association between BMI and postoperative mortality in patients undergoing EOAR, the E-value was calculated28,29.
Upon establishing the association between BMI and postoperative mortality in patients undergoing EOAR through a linear regression model, a Cox proportional hazards regression model with smooth curve fitting was employed to investigate any potential nonlinear relationships. Should a nonlinear relationship be detected, a recursive algorithm was applied to determine the inflection point. Subsequently, Cox proportional hazards regression models were constructed for each segment on either side of this inflection point. The log-likelihood ratio test was used to identify the best model describing the relationship between BMI and postoperative mortality. Furthermore, exploratory stratified Cox proportional hazards regression analyses were performed across various subgroups, including age, sex, respiratory diseases, cerebrovascular diseases, smoking status, and ASA score, to further explore the BMI-postoperative mortality relationship in patients undergoing EOAR. Differences between these subgroups were evaluated using the likelihood ratio test.
Results
Participant characteristics
The study analyzed 3,378 patients who underwent EOAR, with 2,761 being male, representing 81.73% of the sample. The mean age was 70.26 years, with a standard deviation of 7.02 years. BMI values were normally distributed, ranging from 14.39 to 54.29 kg/m², with an average of 26.30 kg/m² and a standard deviation of 4.16 kg/m² (Fig. 2). Table 1 detailed the anthropometric and biochemical characteristics of the participants, classified according to the World Health Organization’s obesity criteria. The data clearly demonstrate that parameters such as weight, height, and perioperative bleeding increased significantly with higher BMI levels. In contrast, age tended to decrease as BMI increased. Additionally, the proportions of individuals with DM, non-smokers, males, cardiac disease, and hypertension rose with higher BMI, whereas the proportions of females, current smokers, and those with preoperative anemia decreased. There were no significant differences among the different BMI categories in terms of follow-up time, total transfusion, preoperative Scr, the proportion of dialysis, respiratory diseases, cerebrovascular diseases, postoperative intestinal ischemia complication, and pulmonary complication.
All-cause mortality of patients undergoing open repair for AAA
As outlined in Table 2, over a median follow-up duration of 4.94 years, 1260 participants passed away. The overall mortality for patients who underwent EOAR was 70.69 per 1,000 person-years. When broken down by BMI category, the mortality rates were as follows: 153.96 per 1,000 person-years for underweight individuals, 81.69 for those of normal weight, 64.45 for the overweight group, and 58.02 for obese patients. The cumulative mortality for patients undergoing EOAR was observed to be 37.37%. More specifically, this rate was 56.67% for underweight, 42.78% for normal weight, 34.42% for overweight, and 29.85% for obese individuals, as highlighted in Table 2.
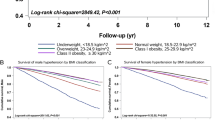
In the age stratification of < 60 years, 60 to < 70 years, 70 to < 80 years, and ≥ 80 years, female patients receiving EOAR had higher mortality in every age group except for the 60 to < 70 years group. Additionally, mortality for both males and females increased with age (Fig. 3). In addition, the 30-day, 90-day, 1-year, and 15-year mortality among different BMI categories were compared. It was found that no significant differences were observed in the 30-day, 90-day, and 1-year mortality across the BMI categories. However, the overall 15-year all-cause mortality was found to differ significantly, with higher BMI being associated with a lower long-term mortality risk (Supplementary Table S1).
The factors affecting mortality in patients undergoing EOAR were examined using univariate Cox proportional hazards regression analysis
The results indicated that mortality among patients undergoing EOAR was inversely associated with BMI and HGB, with statistical significance (P < 0.05). Conversely, mortality showed a positive correlation with total blood transfusion volume, Scr, and perioperative bleeding. Additionally, patients with anemia, elevated ASA scores, cardiac disease, respiratory disease, cerebrovascular diseases, and those experiencing perioperative complications such as cardiac, respiratory, and intestinal ischemia had a higher likelihood of mortality (P < 0.05), as detailed in Supplementary Table S2. In contrast, factors such as hypertension, smoking status, sex, and embolus did not demonstrate a significant association with mortality in patients undergoing EOAR (P > 0.05).
Figure 4 illustrated the Kaplan-Meier survival curves segmented by BMI categories. The survival probabilities among patients undergoing EOAR differ significantly across these BMI groups, as confirmed by the log-rank test (P < 0.001). Participants classified as overweight and obese exhibit lower rates of postoperative mortality, whereas those who are underweight face a heightened risk of mortality.
The relationship between BMI and the all-cause mortality of patients undergoing open repair for AAA
To investigate the relationship between BMI and mortality in patients undergoing EOAR, three Cox proportional hazards regression models were developed, as shown in Table 3. In Model I, a 1 kg/m2 increase in BMI was associated with a 4.1% reduction in mortality (HR = 0.959, 95% CI: 0.945, 0.973). Model II demonstrated that a similar increase in BMI corresponded to a 2.3% decrease in mortality (HR = 0.977, 95% CI: 0.962, 0.992). In Model III, which was fully adjusted, the HR was 0.973 (95% CI:0.958, 0.988), suggesting a 2.7% reduction in mortality risk for each additional 1 kg/m2 of BMI.
Furthermore, the study explored BMI as a categorical variable by reintroducing it into the model after this transformation. Using individuals with normal weight as a baseline reference, the multivariable-adjusted Model indicated different HRs for each BMI category, as detailed in Table 3. Underweight individuals exhibited a 62.6% higher risk of mortality (HR = 1.626, 95% CI: 1.142, 2.314). In contrast, overweight participants demonstrated a18.2% reduced mortality risk (HR = 0.818, 95% CI: 0.722, 0.928), and those classified as obese had a 15.8% lower risk (HR = 0.842, 95% CI: 0.721–0.998) compared to their normal-weight counterparts (Table 3 Model III).
Sensitivity analysis
To validate the robustness of our findings, we undertook various sensitivity analyses. Initially, BMI was redefined into categories based on WHO’s obesity criteria and incorporated into the regression model. The observed effect size trend aligned with those results when BMI was treated as a continuous variable, as demonstrated in Table 3. Furthermore, a Generalized Additive Model (GAM) was utilized to include continuous covariates as curves in the equation. Model IV outcomes (HR = 0.973; 95%CI:0.958, 0.989), shown in Table 3, were closely similar to the fully adjusted model (Table 3 Model III). We also conducted a sensitivity analysis excluding participants with hypertension (n = 1234). After controlling for confounding factors such as age, sex, perioperative bleeding, DM, smoking status, HGB, Scr, ASA score, total transfusion, cardiac diseases, cerebrovascular diseases, intestinal ischemia, cardiac, and pulmonary complications, embolus, the analysis revealed a negative association between BMI and mortality in patients undergoing EOAR (HR = 0.966, 95% CI: 0.941, 0.992). In a separate sensitivity analysis excluding patients with DM and adjusting for similar variables, BMI continued to show a negative correlation with mortality (HR = 0.970, 95% CI: 0.954, 0.987). In addition, when the analysis was confined to individuals without cardiac disease, and all potential confounders were adjusted for, the HR between BMI and mortality was reported as 0.978 (95% CI: 0.960, 0.998), as indicated in Table 4. The variables specifically adjusted for in each sensitivity analysis model are detailed in Table 4.
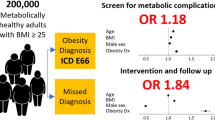
The sensitivity to unmeasured confounding factors was evaluated by calculating the E-value. An E-value of 1.18 was obtained, which surpasses the relative risk of 1.16 between BMI and unmeasured confounders. This suggested that unknown or unmeasured factors are unlikely to have a significant impact on the association between BMI and mortality in patients undergoing EOAR. Evidently, the robustness of our results is confirmed by all sensitivity assessments, and the reliability of our findings is clearly supported by the analysis conducted.
Subgroup analysis results
Within both predefined and exploratory subgroups, factors such as sex, age, ASA score, respiratory conditions, smoking habits, and cerebrovascular diseases did not alter the association between BMI and all-cause mortality in patients undergoing EOAR, as detailed in Table 5. In other words, there was no statistically significant interaction between BMI and these variables (P for interaction > 0.05).
Cox proportional hazards regression with smooth curve fitting to address nonlinear issues
Utilizing Cox proportional hazards regression with smooth curve fitting, we observed a nonlinear association between BMI and postoperative mortality among EOAR patients, as depicted in Fig. 5. The log-likelihood ratio test yielded a P-value below 0.05, indicating statistical significance. Through a recursive approach, a BMI inflection point was identified at 25.78 kg/m². Subsequently, a two-segment Cox proportional hazards regression model was employed to calculate effect sizes and confidence intervals on either side of this inflection point. Below 25.78 kg/m², an increase of 1 kg/m² in BMI corresponded to an 8% reduction in mortality risk for patients following EOAR (HR = 0.920, 95% CI: 0.893–0.949). Conversely, above this point, the HR was 1.014 with a 95% CI of 0.989–1.039, indicating no statistically significant difference (see Table 6).
Discussion
This study investigated the link between BMI and postoperative mortality in patients undergoing EOAR. The findings revealed that an increase in BMI is significantly linked to a lower risk of mortality in these patients. Those classified as underweight exhibited a higher mortality risk, whereas overweight and obese individuals showed a reduced risk. Furthermore, an inflection point was identified, revealing differing relationships between BMI and mortality on either side of this point for patients undergoing EOAR.
Globally, obesity is on the rise and has become a major healthcare concern30. It serves as a significant risk factor for chronic diseases such as DM, hypertension, non-alcoholic fatty liver disease (NAFLD), cancer, and kidney disease, as well as a critical risk factor for cardiovascular diseases14,31–35. However, in certain populations with specific conditions, obesity is linked to more favorable prognoses, whereas lower body weight is connected to poorer outcomes14. This phenomenon is termed the “obesity paradox,” a concept first introduced by Gruberg et al. in 2002, when they observed that obese individuals with coronary artery disease had significantly lower mortality rates compared to their non-obese peers15. This so-called obesity paradox has been verified across various surgical populations, including both cardiac and non-cardiac surgeries36,37,38,39,40,41. A large cohort study focused on general surgery showed that overweight and moderately obese patients undergoing general surgical procedures have a reduced risk of mortality compared to “normal” weight patients. The adjusted odds ratios (OR) with 95%CI were 0.85 (0.75–0.99) for overweight and 0.73 (0.57–0.94) for obese individuals41. Additionally, a meta-analysis involving 557,720 cardiac surgery patients demonstrated that overweight and obese patients also exhibited lower mortality rates. Compared to normal-weight patients, the OR for overweight and obese patients were 0.79 and 0.81, respectively40. Therefore, we speculate that the relationship between BMI and mortality in patients undergoing AAA surgery may also exhibit the obesity paradox.
A recent meta-analysis revealed that the 30-day mortality rate for obese patients undergoing EVAR was 31% lower than that for non-obese individuals, with an OR of 0.69 (95% CI: 0.50–0.96)17. A cohort study involving 668 patients undergoing EOAR indicated that underweight individuals had higher mortality rates in comparison to those of normal weight (HR = 3.67; 95% CI, 1.02–13.18), while obesity was linked to reduced mortality rates relative to normal-weight patients (HR, 0.73; 95% CI, 0.53–1.0)18. In addition, a study utilizing data from the VQI database showed that compared to EOAR patients with a BMI of 25–29.9 kg/m², those with a normal BMI (18.5–24.9 kg/m²) had a 50% increased risk (OR = 1.5, 95% CI 1.13–1.86). Participants with a BMI of 30–34.9 kg/m² and 35–39.9 kg/m² had a 10% increased risk, but these differences were not statistically significant. In other words, compared to patients with a normal BMI (18.5–24.9 kg/m²), those with a BMI of 25–40 kg/m² had a lower 30-day postoperative mortality rate, partially confirming the obesity paradox. The study also found that EOAR patients with morbid obesity (BMI ≥ 40 kg/m²) had a significantly higher 30-day postoperative mortality rate compared to patients with a BMI of 25–29.9 kg/m²20. Another study, also utilizing VQI data, investigated the relationship between BMI and 30-day mortality in EOAR patients and reached inconsistent conclusions, reporting that EOAR patients with a high BMI (> 34 kg/m²) had an increased 30-day mortality19. A study from the United States also confirmed that morbidly obese (BMI > 40 kg/m²) EOAR patients have a higher mortality42. Our study supports the conclusion of an obesity paradox in EOAR patients and complements the existing literature. However, unlike the two large cohort studies based on VQI data, our study did not find a relationship between morbid obesity and the long-term prognosis of EOAR patients. This discrepancy is likely due to the narrower BMI range in our study, with only a small number of patients classified as morbidly obese. Specifically, only 90 patients in our study had a BMI greater than 35 kg/m², and 20 patients had a BMI greater than 40 kg/m², accounting for 2.7% and 0.59% of the total cohort, respectively. In contrast, the VQI cohort studies included 810 patients with a BMI > 35 kg/m² and 229 patients with a BMI > 40 kg/m², representing 8.5% and 2.4% of their respective cohorts. Additionally, the primary endpoints investigated in our study differed from those in previous studies. Our study focused on long-term mortality (15-year all-cause mortality), whereas previous studies primarily examined 30-day postoperative mortality. Furthermore, differences in gender distribution, study period, and adjustment factors are also potential reasons for the discrepancies. This study examined BMI both as a categorical and continuous variable to understand its link with postoperative all-cause mortality in patients following EOAR, minimizing data loss and quantifying this relationship. Sensitivity analyses specifically focused on participants without reported cardiac disease, DM, or hypertension, reaffirming the association within this subset of participants and bolstering the reliability of our findings. In conclusion, our results emphasize considering BMI in the preoperative evaluation of patients scheduled for EOAR. Underweight patients may necessitate enhanced monitoring and personalized nutritional support to improve outcomes. Overweight and obese patients might not immediately require weight reduction, offering healthcare providers guidance for handling weight in patients needing elective AAA surgery. Nonetheless, this does not endorse obesity but highlights the nuanced and complex connection between BMI and prognosis in specific medical and surgical contexts. However, whether morbid obesity has a negative impact on the long-term survival of EOAR patients still requires further exploration through large-sample studies. This study corroborates a negative relationship between BMI and postoperative mortality in patients undergoing EOAR, highlighting the obesity paradox. Although the mechanisms driving this phenomenon remain elusive, several potential explanations exist. Firstly, obese individuals generally have greater fat, muscle mass, and metabolic reserves. These reserves can supply additional energy and nutrition during recovery from illness or surgery, enabling better management of acute stress, a benefit lacking in underweight patients43,44. Secondly, obesity may be linked to elevated levels of certain anti-inflammatory cytokines, potentially offering protective effects in specific disease conditions. For instance, adipokines like leptin and adiponectin might influence immune regulation45,46. Lastly, obese patients may receive more intensive postoperative care and monitoring, potentially enhancing their prognosis. Previous study has confirmed that obese patients undergoing AAA repair have higher rates of wound infections and other complications42. However, our study found no significant differences between obese and normal-weight participants in terms of postoperative complications such as intestinal ischemia, embolism, pulmonary complications, and cardiac complications among patients undergoing abdominal aortic aneurysm repair. This may be due to the relatively small number of obese participants in our study.
Additionally, a multivariable Cox proportional hazards regression was utilized to explore the connection between categorized BMI and postoperative mortality. The varying levels of significance observed for obese patients across different models can be attributed to the following factors: Sample Size and Statistical Power: The proportion of obese patients in our study was relatively small, which may have limited the statistical power to detect significant associations in some models, particularly when additional confounders were introduced. Impact of Confounders: Model II adjusted for only two confounders, age and gender. This limited adjustment may not have fully accounted for other factors influencing the relationship between obesity and outcomes in EOAR patients, resulting in a relatively attenuated effect of obesity. In contrast, Model III incorporated a broader range of clinically relevant confounders, which may have allowed for a more precise estimation of the obesity effect, thereby regaining significance. Model IV applied a smoothing adjustment (GAM), further modifying how confounding variables were accounted for. It is worth noting that, despite the lack of statistical significance in some models, the overall effect size and trend remained consistent across the models. Taking normal weight as the baseline, the adjusted model yielded a HR of 1.626 for underweight patients, 0.818 for those overweight, and 0.842 for obese individuals. This reveals a declining trend in postoperative mortality risk from underweight to obese patients undergoing EOAR, with comparable outcomes for overweight and obese categories. These findings hint at a possible non-linear association between BMI and postoperative mortality in those undergoing EOAR. Consequently, we employed a Cox regression model with smoothed curve fitting to confirm a saturation curve effect between BMI and postoperative mortality. The critical BMI point was determined to be 25.78 kg/m². Below this threshold, each 1 kg/m² increase in BMI corresponded to an 8% reduction in postoperative mortality. Conversely, above 25.78 kg/m², there was no significant correlation. Essentially, as BMI rose, mortality decreased until leveling off at about 25.78 kg/m². Identifying a curvilinear relationship between BMI and postoperative mortality in patients with EOAR holds substantial clinical significance, offering targeted guidance for clinical decisions. Specifically, for patients with a BMI below this threshold, careful consideration of surgical risks versus benefits is recommended, or an improvement in nutritional status should be pursued before proceeding with surgery.
This study boasts several key strengths. Firstly, it employs both categorical and continuous BMI as independent variables to evaluate their association with postoperative mortality in patients undergoing EOAR. This dual approach minimizes information loss and allows for a more precise quantification of the relationship. Secondly, the study effectively addresses missing data through multiple imputation techniques, a method known for boosting statistical power and reducing bias from absent covariate data. Thirdly, compared to previous studies, our research has made significant improvements in handling non-linearity. Additionally, we performed extensive sensitivity analyses to verify the consistency of our results. These analyses involved re-evaluating the BMI-postoperative mortality relationship after excluding participants with conditions such as diabetes, hypertension, and heart disease. Moreover, E-values were computed to gauge the influence of potential unmeasured confounders, further affirming the robustness of our conclusions.
Be aware of potential limitations. Firstly, the participants were exclusively Danish, which raises questions about the generalizability of the findings to other ethnic groups, necessitating further validation. Secondly, BMI was recorded only at the time of admission, with no follow-up measurements. Consequently, any changes in BMI post-discharge or due to behavioral changes remain unknown, highlighting an area for future investigation. Thirdly, in this study, the number of participants with a BMI over 35 kg/m² was very small, which limited our ability to investigate the relationship between extreme BMI and the long-term prognosis of EOAR patients. Whether morbid obesity negatively impacts the long-term survival of EOAR patients still needs to be further explored through large-sample studies. Fourth, as with all observational studies, despite controlling for known confounders, there may still be unaccounted or unmeasured confounding variables. Additionally, this study is a secondary analysis of existing data, limiting the ability to adjust for variables not included in the dataset, such as waist circumference and medication use. However, we calculated the E-value to assess the potential influence of unmeasured confounders, suggesting that such factors are unlikely to account for the observed results. In addition, the original data only provided information on all-cause mortality and did not include detailed cause-of-death information, which limited our ability to conduct further analysis. In future studies or collaborations with other researchers, we will strive to collect more detailed cause-of-death information to better understand the impact of surgical and disease-related factors on mortality. Lastly, being an observational study, it cannot establish a causal link between BMI and postoperative mortality in patients undergoing EOAR, but only establish an association between the two.
Conclusions
This study demonstrated a negative relationship between BMI and postoperative mortality in patients undergoing elective open abdominal aortic repair, thereby supporting the obesity paradox. Importantly, the association between BMI and postoperative mortality in these patients is non-linear. Specifically, a BMI below 25.78 kg/m² is linked to higher mortality rates, where lower BMI corresponds to increased risk, whereas overweight and obese individuals show a diminished mortality risk. This provides a reference for clinical decision-making, suggesting that for patients with a BMI below approximately 25 kg/m², the risks and benefits of surgery should be carefully balanced, or surgery might be postponed to improve nutritional status, ultimately enhancing patient prognosis.
Data availability
The data is accessible for download from the PLOS ONE database at the following URL: https://journals.plos.org/plosone/.
Abbreviations
- BMI:
-
Body mass index
- GAM:
-
Generalized additive models
- Scr:
-
Serum creatinine
- HGB:
-
Hemoglobin
- OR:
-
Odds ratio
- DM:
-
Diabetes mellitus
- EVAR:
-
Endovascular abdominal aortic aneurysm repair
- EOAR:
-
Elective open abdominal aortic aneurysm repair
- Ref:
-
Reference
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
References
Sakalihasan, N., Limet, R. & Defawe, O. D. Abdominal aortic aneurysm. Lancet 365, 1577–1589 (2005).
Golledge, J., Muller, J., Daugherty, A. & Norman, P. Abdominal aortic aneurysm: pathogenesis and implications for management. Arterioscler. Thromb. Vasc Biol. 26, 2605–2613 (2006).
Alshaikh, H. N., Bohsali, F., Gani, F., Nejim, B. & Malas, M. Statin intensity and postoperative mortality following open repair of intact abdominal aortic aneurysm. Bjs Open. 2, 411–418 (2018).
Nordon, I. M., Hinchliffe, R. J., Loftus, I. M. & Thompson, M. M. Pathophysiology and epidemiology of abdominal aortic aneurysms. Nat. Rev. Cardiol. 8, 92–102 (2011).
Burillo, E. et al. Apoa-I/Hdl-C levels are inversely associated with abdominal aortic aneurysm progression. Thromb. Haemost. 113, 1335–1346 (2015).
Golledge, J. Abdominal aortic aneurysm: update on pathogenesis and medical treatments. Nat. Rev. Cardiol. 16, 225–242 (2019).
Jones, M., Faris, P. & Moore, R. Mortality and risk factors for ruptured abdominal aortic aneurysm after repair endovascular (Rare). J. Vasc Surg. Cases Innov. Tech. 9, 101165 (2023).
Duchesne, G. et al. Risk factors and mortality in Dialysis patients with abdominal aortic aneurysm: A retrospective cohort study. J. Invest. Med. 72, 287–293 (2024).
Rastogi, V. et al. Association between diabetes status and Long-Term outcomes following open and endovascular repair of infrarenal abdominal aortic aneurysms. J. Vasc Surg. 80(6), 1685–1696 (2024).
Zhou, W. et al. Body mass index, abdominal fatness, and hypertension incidence: A Dose-Response Meta-Analysis of prospective studies. J. Hum. Hypertens. 32, 321–333 (2018).
Samson, R., Ennezat, P. V., Jemtel, L., Oparil, S. & T. H. & Cardiovascular disease risk reduction and body mass index. Curr. Hypertens. Rep. 24, 535–546 (2022).
Rafiq, S., Jeppesen, P. B., Body Mass & Index Vitamin D, and Type 2 Diabetes: A Systematic Review and Meta-Analysis. Nutrients. 10, (2018).
Elagizi, A. et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc. Dis. 61, 142–150 (2018).
Amundson, D. E., Djurkovic, S. & Matwiyoff, G. N. The obesity paradox. Crit. Care Clin. 26, 583–596 (2010).
Gruberg, L. et al. The impact of obesity on the Short-Term and Long-Term outcomes after percutaneous coronary intervention: the obesity paradox?? J. Am. Coll. Cardiol. 39, 578–584 (2002).
Lu, F. et al. Obesity and the obesity paradox in abdominal aortic aneurysm. Front. Endocrinol. 15, 1410369 (2024).
Naiem, A. A., Kim, A. Y., Mahmoud, I. & Gill, H. L. A systematic review and Meta-Analysis evaluating the impact of obesity on outcomes of abdominal aortic aneurysm treatment. J. Vasc Surg. 75, 1450–1455 (2022).
Park, J. K., Park, Y. J., Yang, S. S., Kim, D. I. & Kim, Y. W. Impact of serum albumin levels and body mass index on outcomes of open abdominal aortic aneurysm repair in Korean population. Ann. Vasc Surg. 101, 139–147 (2024).
Bellamkonda, K. S. et al. The contemporary impact of body mass index on open aortic aneurysm repair. J. Vasc Surg. 19, S0741–5214 (2023).
D’Oria, M. et al. The association between body mass index and death following elective endovascular and open repair of abdominal aortic aneurysms in the vascular quality initiative. Eur. J. Vasc Endovasc Surg. 66, 27–36 (2023).
Zonneveld, B., Vu, D., Kardys, I., van Dalen, B. M. & Snelder, S. M. Short-Term mortality and postoperative complications of abdominal aortic aneurysm repair in obese versus Non-Obese patients. J. Obes. Metab. Syndr. 30, 377–385 (2021).
Kennedy, N. A. et al. The evaluation of morbidity and mortality in abdominal aortic aneurysm repair patients as related to body mass index. Am. J. Surg. 199, 369–371 (2010).
Wedel, C., Møller, C. M., Budtz-Lilly, J. & Eldrup, N. Red blood cell transfusion associated with increased morbidity and mortality in patients undergoing elective open abdominal aortic aneurysm repair. Plos One. 14, e219263 (2019).
Flegal, K. M., Kit, B. K. & Graubard, B. I. Body mass index categories in observational studies of weight and risk of death. Am. J. Epidemiol. 180, 288–296 (2014).
Han, Y., Zhang, S., Zhang, J., Ji, C. & Eckstein, H. H. Outcomes of endovascular abdominal aortic aneurysm repair in octogenarians: Meta-Analysis and systematic review. Eur. J. Vasc Endovasc Surg. 54, 454–463 (2017).
Groenwold, R. H. et al. Missing covariate data in clinical research: when and when not to use the Missing-Indicator method for analysis. Can. Med. Assoc. J. 184, 1265–1269 (2012).
White, I. R., Royston, P. & Wood, A. M. Multiple imputation using chained equations: issues and guidance for practice. Stat. Med. 30, 377–399 (2011).
Burne, R. M. & Abrahamowicz, M. Adjustment for Time-Dependent unmeasured confounders in marginal structural Cox models using validation sample data. Stat. Methods Med. Res. 28, 357–371 (2019).
VanderWeele, T. J. & Ding, P. Sensitivity analysis in observational research: introducing the E-Value. Ann. Intern. Med. 167, 268–274 (2017).
Ng, M. et al. Global, regional, and National prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the global burden of disease study 2013. Lancet 384, 766–781 (2014).
Ohno, R. et al. Association of body mass index and its change with incident diabetes mellitus. J. Clin. Endocrinol. Metab. 108, 3145–3153 (2023).
Pagadala, M. R. & McCullough, A. J. Non-Alcoholic fatty liver disease and obesity: not all about body mass index. Am. J. Gastroenterol. 107, 1859–1861 (2012).
Khan, S. S. et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. Jama Cardiol. 3, 280–287 (2018).
Basen-Engquist, K. & Chang, M. Obesity and Cancer risk: recent review and evidence. Curr. Oncol. Rep. 13, 71–76 (2011).
Tsur, A. M. et al. Adolescent body mass index and early chronic kidney disease in young adulthood. Jama Pediatr. 178, 142–150 (2024).
Valentijn, T. M. et al. The obesity paradox in the surgical population. Surg. J. R Coll. Surg. Edinb. Irel. 11, 169–176 (2013).
Habib, R. H. et al. Effects of obesity and small body size on operative and Long-Term outcomes of coronary artery bypass surgery: A Propensity-Matched analysis. Ann. Thorac. Surg. 79, 1976–1986 (2005).
Oreopoulos, A. et al. Effect of obesity on Short- and Long-Term mortality postcoronary revascularization: A Meta-Analysis. Obesity 16, 442–450 (2008).
Mullen, J. T. et al. Impact of body mass index on perioperative outcomes in patients undergoing major Intra-Abdominal Cancer surgery. Ann. Surg. Oncol. 15, 2164–2172 (2008).
Mariscalco, G. et al. Body mass index and mortality among adults undergoing cardiac surgery: A nationwide study with a systematic review and Meta-Analysis. Circulation 135, 850–863 (2017).
Mullen, J. T., Moorman, D. W. & Davenport, D. L. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann. Surg. 250, 166–172 (2009).
Giles, K. A. et al. The impact of body mass index on perioperative outcomes of open and endovascular abdominal aortic aneurysm repair from the National surgical quality improvement program, 2005–2007. J. Vasc Surg. 52, 1471–1477 (2010).
Caleyachetty, R. et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. J. Am. Coll. Cardiol. 70, 1429–1437 (2017).
Schulze, M. B. & Stefan, N. Metabolically healthy obesity: from epidemiology and mechanisms to clinical implications. Nat Rev. Endocrinol. 20(11), 633–646 (2024).
Galic, S., Oakhill, J. S. & Steinberg, G. R. Adipose tissue as an endocrine organ. Mol. Cell. Endocrinol. 316, 129–139 (2010).
Meier, U. & Gressner, A. M. Endocrine regulation of energy metabolism: review of pathobiochemical and clinical chemical aspects of leptin, ghrelin, adiponectin, and resistin. Clin. Chem. 50, 1511–1525 (2004).
Acknowledgements
The primary data and methodology for this secondary analysis are derived from the study by Charlotte Wedel et al., titled “Red Blood Cell Transfusion is Associated with Increased Morbidity and Mortality in Patients Undergoing Elective Open Abdominal Aortic Aneurysm Repair.” We sincerely thank the authors of this study for providing the foundation for our study.
Funding
Shenzhen Second People’s Hospital Clinical Research Fund of Shenzhen High-level Hospital Construction Project provided financial support for this study under Grant No. 20243357011.
Author information
Authors and Affiliations
Contributions
The study’s design and the initial draft of the manuscript were developed by Qin Zhang, Jinsong Zhou, Haofei Hu, and Changchun Cao. The responsibilities for statistical analysis and data interpretation were undertaken by Haofei Hu and Yong Han. Furthermore, Yong Han, Haofei Hu, and Changchun Cao contributed to the discussion and reviewed the manuscript. Every author has rigorously reviewed and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The data for this study were sourced from the Danish Vascular Registry (Karbase), a comprehensive national database documenting all vascular surgeries. Both the initial study and subsequent data extraction received authorization from the Danish Data Protection Agency (Datatilsynet), with approval number 2015-41-4135,adhering to the Helsinki Declaration’s principles. Since all personal identifiers have been fully anonymized, the Danish Data Protection Agency waived the requirement for informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Q., Zhou, J., Cao, C. et al. Body mass index and mortality after elective open abdominal aortic aneurysm repair in a fifteen year multicenter cohort study. Sci Rep 15, 19402 (2025). https://doi.org/10.1038/s41598-025-05123-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-05123-9