Abstract
Subarachnoid hemorrhage (SAH) from ruptured intracranial aneurysms causes significant morbidity and mortality. Although prophylactic lumbar cerebrospinal fluid (CSF) management is widely used, the relative benefits of continuous lumbar cerebrospinal fluid drainage compared to intermittent lumbar puncture remain undefined. This study compared clinical outcomes between these two approaches in patients with aneurysmal SAH. This single-center retrospective study included 222 patients with aneurysmal SAH treated between January 2023 and December 2023. Patients were assigned to continuous lumbar cerebrospinal fluid drainage (n = 103) or intermittent lumbar puncture (n = 119). The primary outcome was the modified Rankin Scale (mRS) score at 6 months, categorized as good (0–2) or poor (3–6). Secondary outcomes included secondary infarcts, intracranial infections, hydrocephalus, and mortality. At 6 months, the lumbar drainage group exhibited significantly better outcomes (79% vs. 58%, relative risk [RR] 1.36, 95% CI [0.70, 0.85], p = 0.002) and lower rates of intracranial infection (0% vs. 11%, p = 0.002) and hydrocephalus (6.8% vs. 23.5%, RR 0.29, 95% CI [0.03, 0.13], p = 0.001) compared to the lumbar puncture group. Secondary infarcts occurred in 17.4% of the lumbar drainage group versus 28% of the lumbar puncture group (RR 0.63, 95% CI [0.11, 0.26], p = 0.099). No significant difference in mortality was observed between the groups (5.8% vs. 7.5%, RR 0.79, 95% CI [-1.35, 0.79], p = 0.608). Continuous lumbar cerebrospinal fluid drainage was associated with improved clinical outcomes, fewer intracranial infections, and reduced hydrocephalus incidence compared to intermittent lumbar puncture in patients with aneurysmal SAH. These findings advocate for the early adoption of continuous lumbar cerebrospinal fluid drainage in clinical practice.
Similar content being viewed by others
Introduction
Subarachnoid hemorrhage (SAH) from ruptured intracranial aneurysms is a type of stroke that often results in death or permanent disability in most patients1. Vasospasm occurs in approximately 70% of patients, with delayed cerebral ischemia(DCI) developing in around 40% of cases. While prophylactic nimodipine reduces adverse outcomes, it does not directly affect the cerebrovascular system2.
The standard treatment for ruptured aneurysms involves two surgical approaches: cranial aneurysm clipping or endovascular coil embolization, typically performed within 48 h of bleeding onset. Endovascular embolization is preferred when both methods are feasible3. The EARLYDRAIN randomized clinical trial shows that early postoperative prophylactic lumbar pool drainage reduces secondary infarcts at discharge and lowers adverse outcomes at six months4. However, this trial did not evaluate the prognostic impact of lumbar cerebrospinal fluid drainage rates below or above 5 mL per hour. Additionally, it did not compare the effects of intermittent lumbar puncture drainage, a common clinical practice, on patient outcomes.
To address these gaps, we conducted a retrospective study comparing intermittent lumbar puncture with lumbar cerebrospinal fluid drainage in patients with aneurysmal SAH. Our hypothesis was that continuous lumbar cerebrospinal fluid drainage would yield better clinical outcomes than intermittent lumbar puncture. The primary outcome was the modified Rankin Scale (mRS) score at 6 months, with secondary outcomes focusing on improvements in patient prognosis.
Methods
Trial design and oversight
This single-centre retrospective controlled study enrolled patients with ruptured intracranial aneurysms and subarachnoid haemorrhage from the neurosurgical department and intensive care unit of the Huai’an First People’s Hospital between 1 January 2023 and 31 December 2023. This centre performs at least 400 aneurysm surgeries annually. All patients provided informed consent, and the study was approved by the Huai’an First People’s Hospital Ethics Committee. All methods adhered to relevant guidelines and regulations.
Participants
Eligible patients must be at least 18 years and have an acute subarachnoid haemorrhage diagnosed by computed tomography (CT) and confirmed as an intracranial aneurysm by CTA or digital subtraction angiography (DSA). Aneurysm treatment was required within 48 h of subarachnoid haemorrhage. Exclusion criteria included contraindications to the placement of lumbar cerebrospinal fluid drainage, therapeutic anticoagulation, pregnancy, participation in another interventional trial, and non-aneurysmal bleeding.
Data collection
Patients included in this trial were followed up to their death or 6 months after randomization. We collected baseline demographic and processes-of-care data from the first 5 days, descriptive radiologic imaging, and 6 months’ outcome.
Procedures
The decision regarding the timing of extubation upon admission was determined by the emergency team, and the approach of choice included aneurysm clamping or interventional embolisation, as outlined in the Chinese Guidelines for the Management of Ruptured Aneurysms and the Expert Consensus on the Management of Critical Aneurysmal Subarachnoid Haemorrhage5,6 .The neurosurgical team was responsible for the decision-making process concerning the performance of desmoid decompression, extraventricular drainage, and haematoma debridement.
Postoperative cranial CT confirmed safety. A senior neurosurgeon with over 10 years of experience then discussed the risks and benefits of intermittent lumbar puncture versus continuous lumbar cerebrospinal fluid drainage with the patient or family. The patient or family then decided on the treatment approach. If intracranial pressure (ICP) monitoring readings exceed 25 mmHg, lumbar pool drainage and lumbar puncture procedures are delayed. For patients undergoing lumbar pool drainage, the drain remains in place for at least four days, with flow rates controlled at 6–8 mL/hour (150 mL/day), supervised by nursing staff and family members. For patients undergoing lumbar puncture, daily procedures are performed for four consecutive days, with a minimum of 25 mL of cerebrospinal fluid removed each time. In cases of suspected vasospasm, DSA, CTA and TCD were performed. In all patients, nimodipine was routinely administered to prevent vasospasm, while in patients with a high suspicion of vasospasm, TCD monitoring was employed in conjunction with antispasmodic vasodilatation, induced elevation of blood pressure, and inhibition of platelet aggregation. To prevent DCI, CTA or DSA was routinely performed on days 7–10 after the initial subarachnoid haemorrhage.Treatment of proven vasospasm involved the administration of antispasmodic vasodilators to raise blood pressure.
Primary and secondary outcomes
The primary end outcome was the incidence of adverse outcomes after subarachnoid hemorrhage measured with the mRS7. The mRS is a 7-point scale ranging from 0 (no health impairment) to 6 (death).Scores were obtained by telephone interview or personal visit by an investigator from the neurosurgical department who was not involved in clinical decision-making, acute care, and had no knowledge of the patient’s course.For the primary outcome, the mRS was categorised as 0–2 (good outcome) or 3–6 (poor outcome).
The primary secondary outcomes included the incidence of no secondary infarcts following aneurysm surgery, and the occurrence of secondary infarcts on the final CT or MRI before discharge8. Other secondary outcomes of interest included mortality rates, the incidence of vasospasm, infections (device infections, intracranial infections, and pulmonary infections), and the prevalence of hydrocephalus in the two groups.
Statistical analysis
Data were analyzed using R-4.3.2. Categorical variables were compared using chi-square tests, while continuous variables were reported as medians with interquartile ranges. Data processing and analysis were performed using Pandas, and visualizations were created with Matplotlib, including stacked bar graphs with gradient colors and borders.
Logistic regression was used to analyze primary and secondary outcomes, converting odds ratios to risk ratios9. We analyzed mRS scores for confounders, including age, pre-onset chronic diseases (hypertension, hyperglycemia, etc.), Hunt-Hess grade at admission, and presence of intracerebroventricular or intraparenchymal hemorrhage. We compared mortality rates between groups using a Cox proportional hazards model.
Results
Patient characteristics
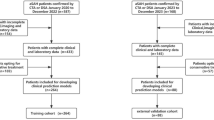
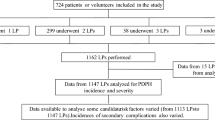
The CONSORT flowchart (Fig. 1) illustrates patient inclusion and exclusion. Ten patients who received neither lumbar pool drainage nor lumbar puncture were excluded. Of the 222 included patients, 150 (67.5%) were female. All 222 patients were analyzed using an intention-to-treat principle. The lumbar pool drainage group included 103 patients with a median age of 59 years, while the lumbar puncture group included 119 patients with a median age of 61 years (Fig. 1). Lumbar pool drainage was initiated after postoperative cranial CT confirmed safety on days 1 to 2. Baseline comparisons showed that the lumbar puncture group had a higher proportion of patients classified as Hunt-Hess grades 3–5 and a greater number assigned modified Fisher grade 4. Intracranial infections were less frequent in the lumbar pool drainage group than in the lumbar puncture group (p = 0.002). (Table 1).
The lumbar cerebrospinal fluid drainage group drained 150 mL of cerebrospinal fluid daily, compared to 27 mL in the lumbar puncture group. Patients undergoing lumbar pool drainage exhibited lower ICP than those in the lumbar puncture group. No significant differences were observed between groups in mean daily arterial pressure, fever burden, transcranial Doppler findings, hemoglobin levels, fluid balance, blood glucose, or electrolyte levels (sFig.1–9 in the Supplement).
Primary end point
No patients were lost to follow-up during primary endpoint evaluation. At 6 months, 22 of 103 patients (21.3%) in the lumbar cerebrospinal fluid drainage group and 50 of 119 patients (42%) in the lumbar puncture group experienced unfavourable outcomes. This corresponded to an uncorrected relative risk of 0.70 (absolute risk difference − 0.16; P = 0.01).(Fig. 2).
Scores on the Modified Rankin Scale (mRS) at 6 Months. Scores on the mRS range from 0 to 6, with 0 indicating no symptoms; 1, no clinically significant disability; 2, minor functional impairment; 3, moderate disability with preserved ability to walk; 4, moderate severe functional impairment without ability to walk without assistance; 5, severe functional impairment requiring constant care; and 6, death.
Secondary outcomes
Secondary infarcts were identified on pre-discharge brain imaging in 18 patients (17.4%) in the lumbar cerebrospinal fluid drainage group and 23 patients (19.3%) in the lumbar puncture group. Within 6 months, 6 patients (5.8%) in the lumbar cerebrospinal fluid drainage group and 9 patients (7.5%) in the lumbar puncture group died (risk ratio 0.79, P = 0.608, 95% CI [-1.35, 0.79]) (sFig. 10 in the Supplement). No differences in cause of death were observed between groups (sTable1 in the Supplement), and no deaths were attributed to complications from lumbar cerebrospinal fluid drainage or lumbar puncture. Intracranial infections occurred in 13 patients (13.9%) in the lumbar puncture group, compared to none in the lumbar pool drainage group (P = 0.002). Hydrocephalus developed in 7 patients (6.8%) in the lumbar pool drainage group versus 28 patients (23.5%) in the lumbar puncture group (P = 0.007). (Table 2)
Subgroup analysis
We analyzed multiple factors related to 6-month mRS scores, including patient age, sex, pre-morbid chronic conditions (e.g., hypertension, hyperglycemia), Hunt-Hess grade at admission, and WFNS grade (Table 3; sFig. 11–22 in the Supplement). Results showed that l lumbar cerebrospinal fluid drainage was associated with significantly better 6-month outcomes in female patients, those without preoperative diabetes, and patients with Hunt-Hess grades 3–5 or WFNS grades 4–5.
Hunt-Hess and World Federations of Neurosurgical Societies (WFNS) scales are severity gradings scales, with 1 indicating the least severe and 5 indicating the worst neurological status on admission. The modified Fisher classification is a radiological grading scale of subarachnoid hemorrhage severity ranging from 1 to 4, with higher scores indicating more severity. EVD indicates external ventricular drain; mRS, modified Rankin Scale.
Post hoc analysis
The occurrence of infarction at discharge in patients exhibiting vasospasm was correlated by clinical observation, DSA and transcranial Doppler ultrasound detection. We found that 136 patients (75.1%) with asymptomatic vasospasm and 18 patients (43.9%) with clinically suspected vasospasm had no infarcts at discharge. Among those monitored by TCD, 124 patients (68.5%) without suspected vasospasm and 19 patients (46.3%) with suspected vasospasm also had no infarcts at discharge. Infarcts at discharge were linked to poor outcomes at 6 months, with 24 patients (58.5%) experiencing poor outcomes if they had an infarct, versus 129 patients (71.3%) with good outcomes if they did not. This difference was statistically significant(sTable 2–4 in the Supplement).
Discussion
This retrospective study included patients with ruptured aneurysms and subarachnoid hemorrhage, including those with severe aneurysms (Hunt-Hess grade 5 or WFNS grade 5). In contrast, many previous studies excluded patients with poor aneurysm scores2,10,11. Our findings showed that in patients with subarachnoid hemorrhage, lumbar cerebrospinal fluid drainage reduced the incidence of infarcts, intracranial infections, and hydrocephalus at discharge, and improved 6-month mRS scores compared to intermittent lumbar puncture.
In subarachnoid hemorrhage cases, blood is predominantly found in the basal cisterns and ventricular system. Red blood cells in the cerebrospinal fluid tend to settle due to gravity, making continuous lumbar drainage (lumbar puncture or lumbar cerebrospinal fluid drainage) more feasible than external ventricular drainage. When both ventricular and lumbar drains are used, the color difference between their outputs is visually distinct, as noted by the chief physician and imaging physician.
In patients with ICP monitoring, the lumbar cerebrospinal fluid drainage group showed lower ICP than the lumbar puncture group. This difference may be attributed to the higher drainage volume in the lumbar cerebrospinal fluid drainage. Additionally, ICP spikes can trigger widespread depolarization, potentially indicating impending cerebral infarction12.
In patients with aneurysmal subarachnoid hemorrhage, early cerebrospinal fluid drainage is associated with a more favorable prognosis than no drainage4,8. Clinical management of aneurysmal subarachnoid hemorrhage often involves intermittent lumbar puncture or continuous lumbar cerebrospinal fluid drainage. A retrospective study found neither method was associated with procedure-related adverse effects. Continuous lumbar cerebrospinal fluid drainage reduced hydrocephalus incidence and improved 6-month mRS scores while reducing pain from repeated punctures. Draining 150 mL daily (6.25 mL/hour) enhanced mRS scores and reduced hydrocephalus more effectively than the EARLYDRAIN trial’s 5 mL/hour regimen. In contrast, lumbar puncture drained only 27 mL per procedure (1.125 mL/hour), showing no significant benefits. Further research is needed to determine the optimal hourly drainage volume.
In this study, we compiled patients’ pre-admission data, particularly noting hypertension and diabetes, both of which showed improvement compared to the EARLYDRAIN study. Additionally, the Montreal Cognitive Assessment was administered to discharged patients to evaluate cognitive impairment across all aneurysm grades13. The results obtained revealed that patients in the lumbar cerebrospinal fluid drainage exhibited mild cognitive impairment (sFig.23–24 in the Supplement).
Vasospasm, regardless of its definition, is linked to secondary infarction development. Beyond vasospasm of cerebral vessels, other mechanisms contributing to secondary infarcts include microthrombus embolism, impaired cerebral autoregulation, and cortical spreading depolarization14. Advancing techniques such as local brain tissue oxygenation monitoring, cortical spreading depolarization detection, and continuous surface electroencephalography recordings are needed to further explore this field15.
This study has several limitations. Firstly, the study is a single-center retrospective analysis and may be subject to selection bias and confounding factors. Future research should consider prospective randomized controlled trials to further validate these findings. Secondly, our techniques for monitoring vasospasm and secondary infarction were limited. Due to practical constraints, not all patients could undergo DSA imaging when vasospasm was suspected. We plan to optimize this process in the future. Additionally, MRI was not routinely used for discharged patients. However, we have recently implemented continuous EEG monitors in the ICU.and MRI was not routinely used for discharged patients. However, we have recently begun continuous electroencephalographic monitoring in the ICU. Thirdly, the timing of postoperative lumbar cerebrospinal fluid drainage and lumbar puncture was inconsistent due to the need to consult specialists to rule out obstructive fluid before procedures in patients with external ventricular drains. Additionally, data from patients who did not undergo either procedure were not included. Future studies could compare these three groups to better determine optimal hourly drainage volumes for prognosis. Finally, we did not assess CT changes in subarachnoid hemorrhage at each time point, which could be combined with imaging histology and machine learning in future work to predict vasospasm and patient outcomes16.
Conclusion
In patients with aneurysmal subarachnoid haemorrhage, continuous lumbar cerebrospinal fluid drainage reduces infarction at discharge, decreases the incidence of intracranial infection and hydrocephalus, and reduces the incidence of adverse outcomes at 6 months compared with intermittent lumbar puncture drainage. Our findings support the early use of lumbar pool continuous drainage tubes.
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files). If someone wants to request the data from this study, please contacted the First Author.
References
Macdonald, R. L. Delayed neurological deterioration after subarachnoid haemorrhage. Nat. Reviews Neurol. 10 (1), 44–58 (2014).
Macdonald, R. L. et al. Clazosentan, an endothelin receptor antagonist, in patients with aneurysmal subarachnoid haemorrhage undergoing surgical clipping: a randomised, double-blind, placebo-controlled phase 3 trial (CONSCIOUS-2). Lancet Neurol. 10 (7), 618–625 (2011).
Molyneux, A. et al. International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet (London England). 360 (9342), 1267–1274 (2002).
Wolf, S. et al. Effectiveness of lumbar cerebrospinal fluid drain among patients with aneurysmal subarachnoid hemorrhage: A randomized clinical trial. JAMA Neurol. 80 (8), 833–842 (2023).
Chinese Society of Neurosurgery, Chinese Stroke Association. National Centre for Neurological Disorders, et al. Clinical management guidelines for ruptured intracranial aneurysms in China (2024 edition)[J]. Chinese Medical Journal,2024,104(21):1940–1971. https://doi.org/10.3760/cma.j.cn112137-20240222-00374
Yueqiao, X. U. et al. Expert consensus on the management of severe aneurysmal subarachnoid haemorrhage (2023). %J Chin. J. Cerebrovasc. Disease. 20 (02), 126–145 (2023).
McKevitt, C., Dundas, R. & Wolfe, C. Two simple questions to assess outcome after stroke: a European study. Stroke 32 (3), 681–686 (2001).
Lee, K. S. et al. Effectiveness of cerebrospinal fluid lumbar drainage among patients with aneurysmal subarachnoid hemorrhage: an updated systematic review and Meta-Analysis. World Neurosurg. ;183: (2024). 246 – 53.e12.
Grant, R. L. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. Bmj 348 (jan24 1), f7450–f (2014).
Carlson, A. P. et al. Single-Dose intraventricular nimodipine microparticles versus oral nimodipine for aneurysmal subarachnoid hemorrhage. Stroke 51 (4), 1142–1149 (2020).
Macdonald, R. L. et al. NEWTON-2 cisternal (Nimodipine microparticles to enhance recovery while reducing toxicity after subarachnoid Hemorrhage): A Phase 2, Multicenter, Randomized, Open-Label Safety Study of Intracisternal EG-1962 in Aneurysmal subarachnoid Hemorrhage. Neurosurgery 88 (1), E13–e26 (2020).
Dreier, J. P. et al. Spreading depolarizations in ischaemia after subarachnoid haemorrhage, a diagnostic phase III study. Brain: J. Neurol. 145 (4), 1264–1284 (2022).
Nasreddine, Z. S. et al. The Montreal cognitive assessment, moca: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53 (4), 695–699 (2005).
Rass, V. & Helbok, R. How to diagnose delayed cerebral ischaemia and symptomatic vasospasm and prevent cerebral infarction in patients with subarachnoid haemorrhage. Curr. Opin. Crit. Care. 27 (2), 103–114 (2021).
Meinert, F. et al. Less-invasive subdural electrocorticography for investigation of spreading depolarizations in patients with subarachnoid hemorrhage. Front. Neurol. 13, 1091987 (2022).
Zarrin, D. A. et al. Machine learning predicts cerebral vasospasm in patients with subarachnoid haemorrhage. eBioMedicine ;105. (2024).
Acknowledgements
We express our gratitude to the patient’s family members for their co-operation.
Conflict of Interest Statement.
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Contributions
Jiahui Liu: Conceptualization; data curation; formal analysis; methodology; project administration; resources; supervision; writing – original draft; Qiushi Chen: Conceptualization; data curation; resources; writing – review and editing.Kun Sun: Methodology; project administration; resources; Lianshu Ding: Conceptualization; data curation; formal analysis; investigation; methodology; project administration; resources; supervision; writing – review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, J., Chen, Q., Sun, K. et al. Comparative analysis of lumbar cerebrospinal fluid drainage versus lumbar puncture effectiveness in patients with aneurysmal subarachnoid hemorrhage. Sci Rep 15, 21642 (2025). https://doi.org/10.1038/s41598-025-05358-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-05358-6