Abstract
Pain in patients in the intensive care unit (ICU) who are on mechanical ventilators has a range of consequences that impact both their physical and mental recovery. Therefore, this study aims to assess the severity of pain at rest and the factors associated with it among patients on mechanical ventilators in the intensive care units. A multi-center prospective observational study was conducted among patients on mechanical ventilators in the intensive care unit of comprehensive specialized hospitals in the Amhara Region of North-West Ethiopia, from October 10, 2024, to January 15, 2025. Data were collected using a semi-structured questionnaire. Pain status was assessed every four hours on the first day of ICU admission using the Behavioral Pain Scale (BPS). Consecutive sampling was employed to select participants. Data were entered into EPI-data version 4.6 and transferred to Stata version 17 for analysis. Both bivariable and multivariable logistic regression analyses were performed to identify factors associated with pain. This study was conducted among 234 patients. We found the severity of pain as follows: 60 patients (25.64%) experienced no pain, 118 patients (50.43%) experienced mild pain, and 56 patients (23.93%) experienced unacceptable (significant) pain. Additionally, in this study, being female (AOR = 2.45, 95% CI 1.42–4.22), surgical cause of admission (AOR = 2.27, 95% CI 1.31–3.93)), anxiety (AOR = 3.78, 95% CI 2.03–7.04), and Combination of analgesia (opioid and non-opioid) (AOR = 0.37, 95% CI 0.21–0.65) had a significant association with pain. This study revealed that a significant proportion of patients (23.93%) experienced unacceptable levels of pain. Factors significantly associated with increased pain severity included being female, having a surgical cause for admission, and experiencing anxiety. Conversely, the use of a combination of opioid and non-opioid analgesics was significantly linked to reduced pain severity. These findings underscore the importance of recognizing demographic, clinical, and psychological factors in pain assessment. Based on the findings, it is recommended to prioritize routine pain assessments, especially for female and surgical patients. Additionally, anxiety screening and management should be integrated into patient care, and the use of combined opioid and non-opioid analgesics should be encouraged to effectively reduce pain severity.
Similar content being viewed by others
Introduction
The Revised International Association for the Study of Pain (IASP) defines pain as an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage1. Pain is a frequent occurance in intensive care unit (ICU) patients in medical, surgical, and trauma intensive care units (ICU) typically experience pain, both at rest and under routine ICU care2,3. The rates of uncontrolled pain in critically ill patients remain unacceptably high1,4,5. More than 50% of critically ill patients experience pain during their stay in ICU5,6,7. Moreover, pain is common in over 80% of mechanically ventilated patients3. Most critically ill patients experience moderate to severe pain while in the intensive care unit (ICU)3,8.
Patients in ICU experience pain due to multiple causes such as their underlying health condition, pre-existing chronic pain, acute postsurgical pain, and pain associated with various ICU procedures and devices, as well as immobility3,8,9,10. Factors that may increase the risk of higher pain level during these procedures include, but are not limited to, the patient’s age, the type of procedure being performed, the administration of analgesic medication one hour before the procedure, and the patient’s pain levels before these procedures6,11,12.
Untreated pain can negatively impact individuals and increase the risk of adverse psychological and physiological consequences, including life-threatening conditions. The physiological response to pain may result in unstable hemodynamic status, deteriorating respiratory and cardiac functions, alteration the immune system, hyperglycemia, and increased release of catecholamines, cortisol, and antidiuretic hormones13,14. furthermore, uncontrolled pain is associated with various psychosocial effects, including depression, anxiety, delirium, and post-traumatic stress disorder. As a result, untreated pain is linked to increased morbidity and mortality, prolonged recovery periods, and higher healthcare costs15,16,17.
Assessing pain in mechanically ventilated patients in intensive care units (ICUs) is crucial yet challenging due to their inability to communicate. Several observational tools have been developed to evaluate pain effectively in these patients, including the Critical Care Pain Observation Tool (CPOT) and the Behavioral Pain Scale (BPS)18,19. These tools have demonstrated high reliability and validity in assessing pain, which is essential for appropriate pain management and improving patient outcomes18,19,20.
Pain management in critically ill patients is a complex issue due to communication barriers, the prevalence of chronic pain, and the challenges in accurately assessing pain levels. Effective pain management is crucial, as poorly controlled pain can lead to chronic pain syndromes, psychological distress, and adverse long-term outcomes21. Given the high incidence of pain in the ICU population, many papers and guidelines recommend an analgesia-based sedation, or “analgosedation”, approach to managing ICU patients22.
To the authors’ knowledge, this study is the first of its kind globally to comprehensively examine the severity of pain and its associated factors in mechanically ventilated patients, a group often underserved due to communication barriers. Addressing this gap is critically important, as unmanaged pain in these patients can lead to serious complications, including agitation, delirium, increased physiological stress, and long-term psychological effects. By identifying the determinants and modifiable factors related to pain in this vulnerable population, the study aims to inform the development of targeted and proactive pain management strategies. This approach has the potential to improve patient outcomes, reduce ICU stays and medication use, and ultimately enhance the overall quality of care in intensive care settings.
Methods and materials
Study design, period, and settings
A multi-center prospective observational study was conducted from October 10, 2024, to January 15, 2024, to determine the severity of pain and associated factors in critically ill patients on mechanical ventilators in the intensive care units of comprehensive specialized hospitals in the Amhara region, North-West Ethiopia. The study follows the Enhancing the Quality and Transparency of Health Research (EQUATOR) guideline, Strengthening the Reports of Observational Studies in Epidemiology (STROBE)23 to ensure methodological rigor and transparency in reporting.
The study involved five hospitals: the University of Gondar, Felege Hiwot, Tibebe Ghion, Debre Tabor, and Debre Markos. The University of Gondar Comprehensive Specialized Hospital, located in Gondar town, has separate medical and surgical ICUs with a total of 19 beds and an average monthly admission of 82 patients. Debre Tabor Comprehensive Specialized Hospital, located in Debre Tabor town, operates a mixed medical-surgical ICU with 5 beds and an average monthly admission of 25 patients. Tibebe Ghion and Felege Hiwot Comprehensive Specialized Hospitals, both located in Bahir dar town, each have mixed medical-surgical ICUs with a combined total of 20 beds and an average monthly admission of 74 patients. Debre Markos Comprehensive Specialized Hospital, located in Debre Markos town, also operates a mixed medical-surgical ICU with 4 beds and an average monthly admission of 16 patients. These hospitals provide a wide range of critical care services, supported by diverse healthcare teams.
Inclusion criteria
All patients aged 18 years and older who were admitted to the ICUs and placed on mechanical ventilators (MV) during the study period were included.
Exclusion criteria
Patients who died within 24 h of admission, extubated within 24 h of admission, those with unavailable medical records, patients admitted to the ICU more than once during the study period, quadriplegic patients, patients with diagnosed peripheral neuropathy, and those receiving neuromuscular blocking agents for 24 h or more were excluded from the study.
Sample size
The sample size was determined using a single population proportion formula based on the assumption that, to the author’s knowledge, no previous studies on this topic have been conducted in the study area. It was assumed that the prevalence of pain in intensive care units for patients on MV is 50%, with a 95% confidence interval and a 5% margin of error. The sample size is calculated as follows.
where: n = sample size, Za/2 = the standard normal value at 95% CI, P = prevalence, and d = margin of error.
Therefore, the sample size \({\text{n}} = \frac{{({1}.{96})^{{2}} \times \, 0.{5}\left( {{1} - 0.{5}} \right)}}{{\left( {0.0{5}} \right)^{{2}} }} \approx {384}\).
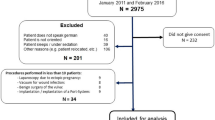
The calculated sample size was 384; however, during the data collection period, only 305 patients were mechanically ventilated. Of these, 234 patients met the inclusion criteria and were included in the study (Fig. 1).
Sampling technique
Consecutive sampling was used to select participants. The number of adult patients on mechanical ventilators (MV) during the study period was manageable in terms of budget and time, so all adult patients on MV who met the inclusion criteria were included in the study.
Study variables
Dependent variable
Pain (No pain/ Mild pain/ unacceptable (significant) pain).
Independent Variable
Socio-demographic characteristics-related factors (i.e. age, sex, height, weight, and BMI),
Clinical characteristics-related factors (i.e. Anxiety, temperature, oxygen saturation, blood pressure, cause of ICU admission, indwelling catheters, mode of mechanical ventilator, history of chronic medical illness, sedation level, analgesic medications, and sedative medications),
Operational definitions
Pain: Based on Behavioral Pain Scale (BPS); a score is 3 indicates no pain, if a score is 4–5 it indicates mild pain, if the score is greater than or equal to 6 it indicates unacceptable (significant) pain24,25.
Sedation level: Based on Richmond Agitation-Sedation Scale (RAAS); if the score is between -5 and 0 indicates sedated and if the score is between + 1 and + 4 indicates agitated26,27.
Anxious: According to the Faces Anxiety Scale (FAS), a patient is considered to be anxious when there is a little bit more up to the extreme of anxiety face28,29.
Data collection tools and procedures
A semi-structured questionnaire was utilized for data collection. Pain levels were assessed using the Behavioral Pain Scale (BPS) developed by Payen et al. The BPS consists of 12 items that evaluate pain based on three behavioral indicators: facial expressions, movement of the upper limbs, and compliance with ventilation. Each behavioral indicator includes four descriptors rated on a scale of 1–4. The total score on the scale ranges from 3 (indicating no pain) to 12 (representing the highest level of pain), with the following score categories: a score of 3 indicates no pain, 4–5 indicates mild pain, and a score of 6 or greater indicates unacceptable (significant) pain. The scale has a high inter-rater reliability of 0.95 (95% CI 0.94–0.97)25. Pain intensity at rest or during periods not involving routine procedures (such as suctioning, wound care, positioning, and intravenous line placement) was assessed every four hours for the first 24 h of ICU admission. The mean pain score was then used for the final analysis.
Demographic data, including the patient’s age and sex, as well as variables such as oxygen saturation, blood pressure, cause of ICU admission, history of chronic medical illness, and medications, were recorded from the patient’s chart. When the history of chronic medical illness was not recorded in the chart, it was obtained through interviews with the patient if their RASS value was -1 or higher, or from caregivers if the patient was uncooperative. Information on the presence of catheters and the mode of mechanical ventilation was collected through observation. Height was measured, and ideal body weight was calculated accordingly. Anxiety levels and sedation status were recorded every four hours using the Faces Anxiety Scale (FAS) and the Richmond Agitation Sedation Scale (RASS), respectively.
Data quality control
To ensure data quality, a pretest was conducted on 5% of patients on mechanical ventilation in the ICU at Dessie Comprehensive Specialized Hospital, which was not included in the main study. This pretest occurred three weeks before the actual data collection, and the contents were modified accordingly. Data collectors and supervisors received one day of training on the study’s objectives and data collection methods from the principal investigator to familiarize themselves with the study. Nurses with BSc degrees working in the ICUs collected the data, while assigned senior anesthetists supervised the data collection process. Data were checked for completeness and clarity.
Data processing and analysis
The data were entered into EpiData version 4.6 and then transferred to STATA version 17.0 for analysis. Descriptive results were presented in text, tables, and figures. The distribution of continuous data was assessed using the Shapiro–Wilk test, and non-normally distributed data were reported as medians with interquartile ranges.
The association between independent factors and the outcome variable was determined using the chi-squared test, along with bivariable and multivariable logistic regression. Crude and adjusted odds ratios, as well as 95% confidence intervals, were used to estimate the strength of these associations. Statistically significant variables identified in the bivariable analysis were deemed eligible for inclusion in the multivariable logistic regression model. Statistical significance was set at a P-value of less than 0.2 for bivariable analysis and less than 0.05 for multivariable logistic regression. Multicollinearity was assessed using variance inflation factors, and model goodness of fit was evaluated using the Hosmer and Lemeshow test.
Ethical consideration
The study was conducted per the Declaration of Helsinki for human data. Ethical clearance and permission to conduct the research were obtained from the ethics committee of the College of Health Science, Debre Tabor University, with the approval number CHS/167/2024. Additionally, ethical approvals and permission letters were secured from all comprehensive specialized hospitals where the study took place. After a brief explanation of the study’s benefits and risks, written informed consent was obtained from the families or caregivers of each participant. Confidentiality was maintained by concealing personal identifiers and securely storing completed questionnaires and results. Participants who experienced pain, anxiety, or agitation during data collection were referred to their respective clinicians for treatment.
Results
A total of 305 patients were on mechanical ventilators in the study area during the data collection period; however, only 234 were ultimately included in the study, while the remaining 71 were excluded (Fig. 2).
Demographic characteristics of participants
A total of 234 intubated patients were included in the study from this 147 (62.82%) of participants were males. The median age of study participants was 40 with (IQR: 28, 53) years. (Table 1).
Chronic medical illness and cause of ICU admission-related findings
Twenty-one participants (8.97%) had a history of chronic medical illness. Among these, the most common comorbidity was chronic obstructive pulmonary disease (COPD), affecting 9 individuals (42.86%) with chronic medical conditions. For the majority of participants, 139 (59.40%), the causes of ICU admission were surgical. (Table 2).
NOTE: In the "History of Chronic Medical Illness" section of Table 1, simply adding the frequency of each comorbidity does not yield the total number of participants with chronic medical illness, as some individuals had two or more comorbidities.
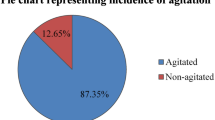
Clinically related variables
In this study, 172 participants (73.50%), reported experiencing anxiety. Additionally, a combination of opioid and non-opioid analgesics was administered to 157 participants (67.09%). Nearly half of the participants, 113 (48.29%), were on volume mode ventilation. Most participants, 183 (78.21%), exhibited agitation, and 229 (97.86%) had indwelling catheters. (Table 2).
Severity of pain
In this study, the severity of pain was assessed as follows: no pain was experienced by 60 participants (25.64%, 95% CI 20.24–31.65%), mild pain by 118 participants (50.43%, 95% CI 44.02–56.82%), and unacceptable (significant) pain by 56 participants (23.93%, 95% CI 18.87–29.85%) (Fig. 3).
Factors associated with the levels of pain
In this study, being female (AOR = 2.45, 95% CI 1.42–4.22), surgical cause of admission (AOR = 2.27, 95% CI 1.31–3.93)), anxiety (AOR = 3.78, 95% CI 2.03–7.04), and Combination of analgesia (opioid and non-opioid) (AOR = 0.37, 95% CI 0.21–0.65) had a significant association with pain. (Table 3).
The odds of experiencing higher levels of pain (mild or unacceptable [significant] pain) versus lower levels of pain (no pain) were 2.45 times greater for female patients than for male patients controlling for other variables. Additionally, the odds of experiencing higher levels of pain (mild or unacceptable (significant) pain) versus lower levels of pain (no pain) were 2.27 times higher for patients admitted to the ICU for surgical reasons compared to those admitted for medical reasons. (Table 3).
When other variables were kept constant, the odds of developing a higher level of pain versus no pain for patients with anxiety were 3.78 times higher compared with their counterparts. However, the odds of experiencing a higher level of pain compared to no pain in patients who received a combination of opioid and non-opioid analgesia were 63% lower than in those who did not take a combination. (Table 3).
Discussion
Untreated pain in adult mechanically ventilated patients can lead to pulmonary and cardiac dysfunction, complicate the weaning process from mechanical ventilation, and increase hemodynamic instability and hyperglycemia, all of which can further compromise patient health. Additionally, acute pain can induce neurohumoral changes, potentially resulting in chronic pain states.
The purpose of this study was to assess the severityof pain and the factors contributing to it among participants on mechanical ventilators in the adult intensive care units of Comprehensive and Specialized Hospitals in the Amhara region of Northwest Ethiopia.
This study classified participants’ pain severity into three categories: no pain (25.64%), mild pain (50.43%), and unacceptable (significant) pain (23.93%). The majority (76.07%) experienced either no pain or only mild pain, suggesting that most found their discomfort minimal or manageable. This indicates the potential effectiveness of the intervention or procedure in controlling pain. However, nearly a quarter of participants reported unacceptable (significant) pain, highlighting the need for further investigation into factors contributing to heightened pain perception.
This variation in pain severity may be influnced by genetic, neurological, and psychological factors, as well as by anxiety, stress, and previous pain experiences. Additionally, demographic and physiological characteristics including age, gender, and underlying health conditions, may affect pain sensitivity. Identifying subgroups more prone to unacceptable (significant) pain could help refine pain management strategies.
Although no directly comparable studies exist, prior research highlights the complex interplay of psychological and physiological factors in pain perception30,31. Our findings support the understanding that pain responses are multifactorial. This underscores the need for further research to explore the key determinants of pain severity. Future studies should utilize larger sample sizes, take prior pain experiences into account, and investigate strategies for effectively reducing pain perception.In the current study, being female, the surgical cause of admission, anxiety, and a combination of analgesia (opioid and non-opioid) were statistically significant association with pain.
In the current study being female was significant association with higher pain levels compared with males. The finding is supported by studies conducted in the USA32, and Italy33. Women may experience pain differently than men due to biological factors, such as hormonal fluctuations that affect pain perception and response. For instance, menstrual cycles can influence pain sensitivity. Additionally women are more likely than men to have chronic pain conditions, which can impact their experience of acute pain in the ICU. A history of chronic pain can influence how women respond to new pain and their overall pain threshold. Some studies suggest that women may be more prone to ruminate on their pain, while men might be more effective at distracting themselves34,35,36,37.
In this study, patients with surgical causes of ICU admission were more likely to have pain as compared to those with medical causes, when other variables were kept constant. The finding is supported by studies conducted in Jordan4,38. This might be because surgical interventions typically involve incisions, tissue manipulation, and other invasive techniques, leading to significant postoperative pain. The level of pain experienced is directly influenced by the extent and type of surgery performed. After surgery, acute pain often a normal part of the healing process. This pain can be exacerbated by factors such as inflammation, muscle spasms, and the body’s response to trauma. In some cases, surgeries may inadvertently damage nerves, leading to neuropathic pain that can be more challenging to manage and may persist beyond the immediate postoperative period. Additionally, surgical patients may develop complications like infections, hematomas, or abscesses, which can contribute to heightened pain levels and necessitate further interventions. Post-surgery, patients often face reduced mobility due to pain, weakness, or sedation from anesthesia; this limited mobility can result in muscle stiffness and further exacerbate discomfort, creating a painful cycle. The stress of undergoing surgery and being in an ICU environment can elevate anxiety and fear, which may amplifying the perception of pain. Additionally, patients with pre-existing anxiety or depression may be particularly vulnerable to experiencing severe pain after surgery39,40,41,42.
In our study, anxiety had a significant positive influence on pain development compared to those without anxiety. This finding is supported by the studies conducted in the Netherlands43 and, the Republic of Korea44. This may be because anxiety can amplify the perception of pain, causes the body to enter a heightened state of arousal and making individuals more sensitive to painful stimuli. As a reuslt, even moderate pain may feel more intense for anxious patients. Anxiety triggers the body’s stress response, releasing hormones like cortisol and adrenaline, which can increase muscle tension and exacerbate pain sensations. This creates a cycle where pain leads to anxiety, which in turn intensifies the pain. Additionally, anxiety can hinder a patient’s ability to cope with pain effectively; anxious individuals may struggle with relaxation techniques or distraction methods that could help mitigate their pain experience. Physical symptoms associated with anxiety, such as muscle tension, can further contribute to discomfort and worsen pain, especially during post-surgical recovery, where muscle relaxation is crucial for healing. Additionally, patients with pre-existing anxiety disorders may have a history of chronic pain or heightened sensitivity, making them more vulnerable in the ICU setting44,45,46,47.
Patients who had received combined opioid and non-opioid analgesics were less likely to have pain than patients who had not received combined opioid and non-opioid analgesics. The result is supported by studies done in Italy48, and the USA49. This might be because combining opioids with non-opioid analgesics represents a multimodal approach to pain management, targeting different pain pathways and mechanisms. This strategy enhances analgesic effects and reduces reliance on any single medication. Non-opioid analgesics, such as non-steroidal anti-inflammatory drugs (NSAIDs), can have synergistic effects when used alongside opioids. While NSAIDs reduce inflammation and peripheral pain signaling, opioids primarily act on the central nervous system to modulate pain perception. Together, this combination can lead to improved overall pain control. Furthermore, using combined analgesics allows for continuous assessment and adjustment of pain management strategies based on patient feedback and clinical observations, which is crucial in the dynamic environment of the ICU50,51,52,53,54.
To the authors’ knowledge, this study is the first of its kind globally to comprehensively examine the severity of pain and its associated factors in mechanically ventilated patients. Additionally, it was a multi-center study that utilized primary data. While the study aims to assess the severity of pain and its associated factors, it does not evaluate participant outcomes or pain management practices. Furthermore, the analysis of the mean pain level score and its predictors was limited to a single day and did not examine pain status at various points during the follow-up period or its predictor variables. Additionally, the BPS tool has limited behavioral indicators, as it is based on just three behavioral domains: facial expression, upper limb movement, and compliance with ventilation. Consequently, many critically ill patients may not exhibit typical pain behaviors due to deep sedation, paralysis from neuromuscular blockers, or neurological impairment.
Conclusion and recommendations
This study revealed that a significant proportion of patients (23.93%) experienced unacceptable levels of pain. Factors significantly associated with increased pain severity included being female, having a surgical cause for admission, and experiencing anxiety. Conversely, the use of a combination of opioid and non-opioid analgesics was significantly linked to reduced pain severity. These findings underscore the importance of recognizing demographic, clinical, and psychological factors in pain assessment. By identifying these associations, the study provides valuable evidence to inform targeted interventions and improve pain monitoring practices, ultimately contributing to more precise and effective management of pain severity in hospital settings. Based on the findings, it is recommended to prioritize routine pain assessments, especially for female and surgical patients. Additionally, anxiety screening and management should be integrated into patient care, and the use of combined opioid and non-opioid analgesics should be encouraged to effectively reduce pain severity. Furthermore, we recommend that future researchers should conduct a longitudinal study to assess the short- and long-term impact of pain on patient outcomes in adult intensive care units. They should also analyze pain status at various points during the follow-up period, along with its predictive variables over an extended timeframe, as many clinically relevant factors influencing ICU patients’ pain experiences manifest and evolve over time.
Data availability
The data used and analyzed during the study are available from the corrosponding author upon rresionable request.
Abbreviations
- AOR:
-
Adjusted odds ratio
- BMI:
-
Body mass index
- BPS:
-
Behavioral pain scale
- Cl:
-
Confidence interval
- COR:
-
Crude odds ratio
- CSH:
-
Comprehensive specialized hospital
- FAS:
-
Face anxiety scale
- ICU:
-
Intensive care unit
- IQR:
-
Inter quartile range
- MV:
-
Mechanical ventilator
- RASS:
-
Richmond agitation sedation scale
- STATA:
-
Statistical software package
References
Raja, S. N. et al. The revised international association for the study of pain definition of pain: Concepts, challenges, and compromises. Pain 161(9), 1976–1982 (2020).
Dziruni, T. B., Hutchinson, A. M., Coomer, J., Keppich-Arnold, S. & Bucknall, T. Realist synthesis of a rapid response system in managing mental state deterioration in acute hospital settings. Int. J. Ment. Health Nurs. 33(5), 1993–1531 (2024).
Pota, V. et al. Pain in intensive care: A narrative review. Pain Ther. 11(2), 359–367 (2022).
Ayasrah, S. M. Pain among non-verbal critically Ill mechanically ventilated patients: Prevalence, correlates and predictors. J. Crit. Care 49, 14–20 (2019).
Stites, M. Observational pain scales in critically ill adults. Crit. Care Nurse 33(3), 68–78 (2013).
Al Sutari, M. M., Abdalrahim, M. S., Hamdan-Mansour, A. M. & Ayasrah, S. M. Pain among mechanically ventilated patients in critical care units. J Res Med Sci. 19(8), 726–732 (2014).
Robleda, G. et al. Evaluation of pain during mobilization and endotracheal aspiration in critical patients. Med Intensiva. 40(2), 96–104 (2016).
Udeh, C. Pain in the critically ill patient. In Fundamentals of Pain Medicine (eds Cheng, J. & Rosenquist, R. W.) 339–347 (Springer International Publishing, 2018). https://doi.org/10.1007/978-3-319-64922-1_36.
Coutaux, A. et al. Care related pain in hospitalized patients: A cross-sectional study. Eur J Pain. 12(1), 3–8 (2008).
Li, D., Puntillo, K. & Miaskowski, C. A review of objective pain measures for use with critical care adult patients unable to self-report. J Pain. 9(1), 2–10 (2008).
Arroyo-Novoa, C. M. et al. Pain related to tracheal suctioning in awake acutely and critically ill adults: A descriptive study. Intensive Crit Care Nurs. 24(1), 20–27 (2008).
Puntillo, K. A. et al. Determinants of procedural pain intensity in the intensive care unit. The Europain® study. Am. J. Respir Crit. Care Med. 189(1), 39–47 (2014).
Joffe, A. M., Hallman, M., Gélinas, C., Herr, D. L. & Puntillo, K. Evaluation and treatment of pain in critically ill adults. Semin. Respir Crit. Care Med. 34(2), 189–200 (2013).
Stites, M. Observational pain scales in critically ill adults. Crit. Care Nurse. 33(3), 68–78 (2013).
Ahlers, S. J. et al. Comparison of different pain scoring systems in critically ill patients in a general ICU. Crit. Care. 12(1), R15 (2008).
Li, D., Miaskowski, C., Burkhardt, D. & Puntillo, K. Evaluations of physiologic reactivity and reflexive behaviors during noxious procedures in sedated critically ill patients. J. Crit. Care. 24(3), 472.e9–13 (2009).
Marmo, L. & Fowler, S. Pain assessment tool in the critically ill post-open heart surgery patient population. Pain Manag. Nurs. 11(3), 134–140 (2010).
Arjyal, B. et al. Comparison of pain assessment by critical care pain observation tool and physiological variables in mechanically ventilated patients. J. Nepalese Soc. Crit. Care Med. 1(2), 10–15 (2023).
Bahramnezhad, F., Salamat, E., Sharifi, F. & Hasanloie, M. A. V. Comparing pain intensity of two instruments in predicting the outcomes of patients under mechanical ventilation admitted to intensive care units. Indian J. Pain. 37(Suppl 1), S15–S21 (2023).
Afenigus, A. D. Evaluating pain in non-verbal critical care patients: a narrative review of the critical care pain observation tool and Its clinical applications. Front. Pain Res. 5, 1481085 (2024).
Jaremko, K., Krish, B., Nikolic, K. & Rayaz, H. 490 Pain in Critically Ill Patients. In Pain Management in Vulnerable Populations (eds Christo, P. J. et al.) (Oxford University Press, 2024).
Barr, J. et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit. Care Med. 41(1), 263–306 (2013).
Von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 370(9596), 1453–1457 (2007).
Ahlers, S. J., van der Veen, A. M., van Dijk, M., Tibboel, D. & Knibbe, C. A. The use of the behavioral pain scale to assess pain in conscious sedated patients. Anesth. Analg. 110(1), 127–133 (2010).
Payen, J.-F. et al. Assessing pain in critically ill sedated patients by using a behavioral pain scale. Crit. Care Med. 29(12), 2258–2263 (2001).
Nassar Junior, A. P., Pires Neto, R. C., Figueiredo, WBd. & Park, M. Validity, reliability and applicability of Portuguese versions of sedation-agitation scales among critically ill patients. Sao Paulo Med. J. 126(4), 215–9 (2008).
Sessler, C. N. et al. The richmond agitation-sedation scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 166(10), 1338–1344 (2002).
Gustad, L. T., Chaboyer, W. & Wallis, M. Performance of the faces anxiety scale in patients transferred from the ICU. Intensive Crit. Care Nurs. 21(6), 355–360 (2005).
McKinley, S., Coote, K. & Stein-Parbury, J. Development and testing of a faces scale for the assessment of anxiety in critically ill patients. J. Adv. Nurs. 41(1), 73–79 (2003).
Apkarian, A. V., Hashmi, J. A. & Baliki, M. N. Pain and the brain: Specificity and plasticity of the brain in clinical chronic pain. Pain 152(3), S49–S64 (2011).
Wiech, K., Ploner, M. & Tracey, I. Neurocognitive aspects of pain perception. Trends Cogn. Sci. 12(8), 306–313 (2008).
Bartsch, A., Anderson, F. L., Fredericson, M. & Sherman, S. L. Biomechanical and biological factors of sexual dimorphism in anterior knee pain: Current concepts. J. ISAKOS. 9(4), 788–793 (2024).
Casale, R. et al. Pain in women: A perspective review on a relevant clinical issue that deserves prioritization. Pain Ther. 10, 287–314 (2021).
Osborne, N.R., Davis, K.D. Sex and gender differences in pain. International Review of Neurobiology. 164: Elsevier, p. 277–307 (2022).
Bartley, E. J. & Palit, S. Gender and pain. Curr. Anesthesiol. Rep. 6, 344–353 (2016).
Gutiérrez Lombana, W. & Gutiérrez Vidál, S. E. Pain and gender differences. A clinical approach. Colombian J. Anestesiol. 40(3), 207–12 (2012).
Keogh, E. The gender context of pain. Health Psychol. Rev. 15(3), 454–481 (2021).
Al Sutari, M. M., Abdalrahim, M. S., Hamdan-Mansour, A. M. & Ayasrah, S. M. Pain among mechanically ventilated patients in critical care units. J. Res. Med. Sci. 19(8), 726 (2014).
Glare, P., Aubrey, K. R. & Myles, P. S. Transition from acute to chronic pain after surgery. Lancet 393(10180), 1537–1546 (2019).
Hanley, C. et al. Association of postoperative complications with persistent post-surgical pain: A multicentre prospective cohort study. Br. J. Anaesth. 128(2), 311–320 (2022).
Pogatzki-Zahn, E. M., Segelcke, D. & Schug, S. A. Postoperative pain—from mechanisms to treatment. Pain reports. 2(2), e588 (2017).
Richebé, P., Capdevila, X. & Rivat, C. Persistent postsurgical pain pathophysiology and preventative pharmacologic. Anesthesiology 129(3), 590 (2018).
de Heer, E. W. et al. The association of depression and anxiety with pain: A study from NESDA. PLoS ONE 9(10), e106907 (2014).
Park, S. et al. Pain and anxiety and their relationship with medication doses in the intensive care unit. J. Crit. Care 47, 65–69 (2018).
Docherty, C. et al. The relationship between pain, anxiety and depression in patients with post-intensive care syndrome. J. Crit. Care 78, 154359 (2023).
Gerrits, M. M., van Marwijk, H. W., van Oppen, P., van der Horst, H. & Penninx, B. W. Longitudinal association between pain, and depression and anxiety over four years. J. Psychosom. Res. 78(1), 64–70 (2015).
Oh, J. et al. Mutual relationship between anxiety and pain in the intensive care unit and its effect on medications. J. Crit. Care 30(5), 1043–1048 (2015).
Varrassi, G. et al. The expanding role of the COX inhibitor/opioid receptor agonist combination in the management of pain. Drugs 80(14), 1443–1453 (2020).
Li, J.-X. Combining opioids and non-opioids for pain management: current status. Neuropharmacology 158, 107619 (2019).
de Renato Lucas, P. et al. Impact of a multimodal analgesia protocol in an intensive care unit: A pre-post cohort study. Cureus https://doi.org/10.7759/cureus.22786 (2022).
Hamrick, K. L., Beyer, C. A., Lee, J. A., Cocanour, C. S. & Duby, J. J. Multimodal analgesia and opioid use in critically ill trauma patients. J. Am. College Surg. 228(5), 769–75 (2019).
Helander, E. M. et al. Multimodal analgesia, current concepts, and acute pain considerations. Curr. Pain Headache Rep. 21, 1–10 (2017).
Kohler, M., Chiu, F., Gelber, K. M., Webb, C. A. & Weyker, P. D. Pain management in critically ill patients: A review of multimodal treatment options. Pain Management. 6(6), 591–602 (2016).
Widehem, R. et al. Effect of a multimodal analgesia strategy on remifentanil daily consumption in mechanically ventilated adult ICU patients: study protocol for a randomised, placebo-controlled, double-blind, parallel-group clinical trial. BMJ Open 15(1), e090396 (2025).
Acknowledgements
Our special gratitude goes to the study participants and their caregivers for their willingness and cooperation during data collection, as well as to the data collectors. Furthermore, we extend our appreciation to our colleagues for their invaluable support and to the members of the Intensive Care Units for their cooperation and assistance in providing the necessary data with cordial help.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
T.B. A. was involved in the conception and design of the study, acquisition of the data, analysis and interpretation of data, and drafting of the manuscript. G.D.G., N.Z. G., H.B. W., M.A. T., W.A. A., A.A. M., G.M. D., A.D. M., D.G. D., B.Y. M., A.G. A., T.M. S., and A.T. A, was approved of the final version of the manuscript for publication. All authors revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Asmare, T.B., Gobezie, N.Z., Wubet, H.B. et al. Severity and factors associated with pain in patients on mechanical ventilators in Amhara region, North-West Ethiopia: a multi-center prospective observational study. Sci Rep 15, 22135 (2025). https://doi.org/10.1038/s41598-025-05810-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-05810-7