Abstract
We studied the characteristics and survival of patients with sorafenib-treated HCC and impact of underlying etiology on outcomes. This retrospective multicenter study recruited patients with sorafenib-treated advanced HCC (12/2016 to 4/2023) till death or the study end (2/2024). Time to progression (TTP) and overall survival (OS) were recorded. We evaluated; Clinico-laboratory and imaging predictors of OS, The impact of underlying etiology on tumor variables, outcomes and tolerance for sorafenib > 6 months. This study included 706 patients. Median duration of Sorafenib therapy was 240.00 (90.00–360.00) days. Median OS was 314.00(146.00–601.00) days. Median TTP was 180.00(90.00–330.00) days. COX regression revealed that the independent factors of mortality were baseline AST, Tumor size, hepatic vein thrombosis (HVT), development of jaundice and shifting to Regorafenib. Advanced HCCs were more common on top of non-cirrhotic non-viral and HBV-related liver disease. Adverse events, TTP and tumor response didn’t differ with the underlying etiology. Median OS was lower in non-viral-related HCC than HCV-related HCC (218.00 versus 326.50 days, P-value = 0.048). Patients who continued sorafenib > 6 months had lower AFP, HVT, adverse effects and better tumor response after 3 months. OS is lower in non-viral Sorafenib-treated HCC compared with viral-related HCC and Sorafenib was well-tolerated among different HCC etiologies.
Similar content being viewed by others
Introduction
Globally, hepatocellular carcinoma (HCC) is ranked as the third most common contributor to cancer-related mortality and the sixth most common cancer1. HCC can be triggered by chronic hepatitis B or C viral infections, alcohol misuse, and metabolic syndrome. Liver cirrhosis, which affects 85–95% of HCC patients, is the main risk factor2. The majority of HCC patients receive their diagnosis too late, missing the best window of opportunity for surgery3,4.
Since 20085, Sorafenib, a multi-targeted tyrosine kinase inhibitor (TKI), has been the accepted line of treatment for advanced HCC. Regorafenib, on the other hand, is authorized as a second chance for non-responders to sorafenib. When compared to the placebo in the RESORCE trial, Regorafenib dramatically increased both OS and progression-free survival6. Systemic therapies for HCC have progressed to the point where Lenvatinib and, later, immunotherapy combinations of Atezolizumab plus Bevacizumab have been approved as first-line treatments. As a second-line treatment option, Cabozantinib, Ramucirumab, immune checkpoint inhibitors (ICIs) Pembrolizumab, and Nivolumab plus Ipilimumab are now offered7.
Although sorafenib has been successfully used to treat advanced HCC, essential predictors of its effectiveness remain to be determined8. Sorafenib-related side effects include diarrhea, hypertension, and hand-foot syndrome (HFS)5. Even though some side effects can predict effectiveness or signal the need for dose modification, there are no established guidelines to adhere to9. Even though Regorafenib’s overall safety profiles were comparable to those of sorafenib and its representative adverse effects were rare, 25% of patients in the RESORCE trial stopped receiving therapy as a result of the drug’s side effects6. These results are unexpected and reveal differences in the mechanisms underpinning the negative effects generated by Sorafenib and Regorafenib, as well as the mechanisms governing their anti-tumor actions, despite the very similar chemical structures of the two drugs6. While comprehensive data was required to examine this clinical query, no report offered a comparison of the two medications’ individual levels of safety and efficacy.
This research includes, for the first time, a large Egyptian population that received Sorafinib and the second line, Regorafenib. There is never enough information available from clinical trials about how patients with HCC from the Middle East and North Africa (MENA) area react to such medications. There is conflicting evidence about the impact of underlying etiology on sorafinib response. The SHARP study, which resulted in the approval of sorafenib, did not conduct thorough etiology-based subgroup analysis10, and the findings of further research have been inconclusive. While previous real-world trials indicate modestly better survival in patients with viral-related HCC11,12, Hiraoka et al.13 found no significant differences in sorafenib effectiveness across HBV, HCV, and non-viral subgroups.
Regional and ethnic differences may affect adverse events pattern and OS as reported by the GIDEON trial14. For example, compared to Western populations, patients from the Asia–Pacific area, who were primarily of East Asian origin, tended to have a worse OS. This might be due to variations in liver function, treatment accessibility, and disease stage upon diagnosis. Similarly, despite similar disease control rates, a sub-analysis of the SHARP and Asia–Pacific trials showed that the median OS in the Asia–Pacific cohort was 6.5 months, which was much shorter than the 10.7 months seen in the SHARP trial (Western population)9,15. Due to pharmacogenomic variations in sorafenib metabolism or drug sensitivity, Asian patients seem to experience greater rates of certain toxicities, such as diarrhea and hand-foot skin reaction16,17. On the other hand, fatigue and hypertension are more common in Western patients.
In addition to examining the effects of the patients’ underlying disease etiology on treatment success, this work seeks to evaluate the characteristics, adverse events, treatment duration and outcomes, and OS of patients with sorafenib-treated advanced HCC.
Patients and methods
This study is a retrospective multicenter effort. Six tertiary care centers provided patients for the treatment of HCC:
-
1.
Viral hepatitis center, National medical institute of Damanhur, Boheira Governorate
-
2.
National Liver Institute, Menoufia University, Menoufia Governorate
-
3.
Multidisciplinary HCC clinic, Cairo University, Cairo Governorate
-
4.
Assuit Hepatoma Group, Assuit University, Assuit Governorate
-
5.
Hepatoma group, Tropical Medicine Department, Ain-Shams University, Cairo Governorate
-
6.
Endemic medicine department, Helwan University, Cairo Governorate
All Sorafenib-treated Patients were recruited during the study period from December 2016 to April 2023, and follow-up continued till death or the end of the study in February 2024. No particular grant from a public, private, or nonprofit organization has been provided for this research. This study adhered to the World Medical Association’s 1975 Code of Ethics (Declaration of Helsinki) and its subsequent revisions. An informed consent was obtained from all participants of the study. The protocol was approved by the ethics committees of Cairo University’s Faculty of Medicine (number: N-336-2023), Ain-Shams University’s Faculty of Medicine (number: FMASU-R36-2024), and Assiut University’s Faculty of Medicine (number: 04-2023-300142).For every patient, we gathered baseline demographic information, ECOG performance status, Child–Pugh Score and laboratory investigations (Complete blood count (CBC), hepatic and renal function tests, HBsAg, Anti-HCV Ab and Alpha-fetoprotein (AFP)). As well, Echocardiogram (ECG) was done, and if needed Echocardiography.
In compliance with globally accepted recommendations, the diagnosis of HCC was verified using either a Triphasic CT or a dynamic MRI18. The Barcelona Clinic Liver Cancer (BCLC) staging was performed upon diagnosis. We included patients with BCLC B or C. Patients then started sorafenib therapy (200 mg once daily, increased to 200 mg twice daily, then if the previous dose is tolerated increase to 400 mg BID). Tumor response was evaluated using the modified Response Evaluation Criteria in Solid Tumors (modified RECIST)19.
Follow-up
The initial evaluation of response was performed after 1 month by Triphasic CT or dynamic MRI, or PET CT if needed, then every 3 months. Also, patients were assessed for compliance with treatment and the development of adverse events (AEs). The severity of AEs was evaluated if necessitating dose modification, stopping treatment, or shifting to other drugs. Follow-up was performed until a patient’s death or until the end of the study for surviving patients.
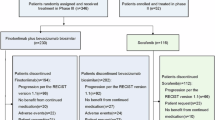
Follow-up laboratory investigations including CBC, hepatic and renal function tests, AFP, after 1 month and then every 3 months. In addition, an ECG was done every month for every patient. Regorafenib was the available second-line therapy for patients with progressive disease (160 mg PO daily for the first 21 days of each 28-day cycle). Regorafenib-related AEs, follow-up laboratory data, and the modified RECISET criteria after Regorafenib were recorded. Time to progression (TTP) was calculated from the date of treatment start until the occurrence of tumor progression. Overall survival (OS) was calculated from the date of treatment start till patient death or the study end.
Due to the conflicting results reported about the effect of underlying liver disease etiology on the outcome of Sorafenib treatment, we divided the patients into hepatitis C-related HCC, Hepatitis-B related HCC and non-viral HCC to examine the effects of the underlying disease etiology on patients characteristics, adverse events, treatment duration and outcomes, and OS. The primary endpoint of the study was the overall survival (OS) of the recruited patients and time to progression (TTP), treatment related adverse events. The Secondary endpoints: effect of duration of treatment on treatment outcome.
Statistical methods
The statistical software for the social sciences (SPSS) version 28 (IBM Corp., Armonk, NY, USA) was utilised to code and enter the data. For quantitative variables, the data was summarized using the median and interquartile range; for categorical variables, the data was summarized using frequencies (number of cases) and relative frequencies (percentages). Non-parametric Mann–Whitney and Kruskal–Wallis tests were utilised to compare quantitative variables. We used the Chi-square (2) test to compare categorical data. When the expected frequency is less than five, an exact test was utilized in its place. The Spearman correlation coefficient was utilized to perform correlations between quantitative variables. In both univariate and multivariate regression models, the Cox proportional hazards were used to evaluate independent prognostic variables. P-values were regarded as statistically significant if they were P < 0.05.
Results
This multicenter retrospective work included 706 consecutive patients with Sorafenib-treated HCC. The median age of the studied patients was 62 years with male predominance (76.1%), 98% of our patients had cirrhosis, with the majority had Child–Pugh class A (96.5%) (Table 1). Regarding tumor characteristics, 55.5% had a single focal lesion and 27.3% had main portal vein thrombosis, 59.5% had BCLC stage-B (Table 2). The median (IQR) duration of Sorafenib treatment was 240.00 (90.00–360.00) days. The most common causes of treatment discontinuation were Liver decompensation (26.3%) followed by patient demand (16.4%). On the other hand, 177 (25.1%) patients are still on treatment (Table 3).
Sorafenib-related adverse events are reported in Table 4. Jaundice is the most commonly reported adverse event (30.9%) followed by fatigue (24.6%), anemia (19.3%), and elevated liver enzymes (15.4%) (Fig. 1). None of the patients who continued sorafenib treatment for more than 6 months developed grade 3 or 4 elevations of liver enzymes. Changes in laboratory parameters and ECOG performance status are shown in Supplementary Tables 1, 2
The modified RECIST criteria were available for 480 (68%) of patients. None of the patients achieved a complete response. One hundred (20.83%) patients achieved partial response. On the other hand, 219 (45.63%) patients had a stable disease and 161 (33.54%) patients showed progressive disease (Table 3).
By the end of the study, 379 (53.7%) patients died. The median (IQR) OS after Sorafenib treatment was 314.00 (146.00–601.00) days (10.47 months (4.87–20.03). The median (IQR) time to progression was 180.00 (90.00- 330.00) days (Table 3). We found no difference in the median OS between patients below 65 years-old and elderly patients above 65 years old (314.00 (139.00- 612.00) and 314.50 (154.00- 594.00) respectively, P-value 0.986). In addition, we found no difference in the median OS between patients with Child–Pugh A and B (310.50 (143.00–601.00) and 373.50 (228.00–608.00) days, respectively, P-value 0.529) or between patients with BCLC B and C (307.00 (141.00–594.00) and 334.00 (154.00–608.00) days, respectively, P-value 0.406).
Spearman correlation coefficient revealed a strong positive correlation between the duration of treatment with sorafenib and the median survival time (r = 0.732, P-value < 0.001) and a negative correlation between the duration of sorafenib treatment and baseline AFP (r = − 0.202, P-value < 0.001) (Supplementary Table 3). Comparison between baseline laboratory data and data before treatment stop revealed significant reduction in blood counts and deterioration of liver function tests with no significant changes in serum Creatinine or AFP (Supplementary Table 4).
Univariate COX regression analysis revealed that factors affecting survival after Sorafenib treatment are cigarette smoking, performance status, the presence of splenomegaly, serum bilirubin and AST, in addition to the number, site and size of the hepatic focal lesions, the presence of hepatic vein thrombosis, the development of fatigue, and shifting to Regorafenib (Table 5). Multivariate regression analysis revealed that the independent factors affecting mortality were baseline serum AST (P value < 0.001, Hazard ratio (HR) 1.005, 95.0% CI (1.002–1.007)), size of HCC (P value 0.007, HR 1.039, 95.0% CI (1.010–1.068)), the presence of hepatic vein thrombosis before treatment carries 1.739 times higher risk of mortality (P value 0.013, HR 1.739, 95.0% CI (1.125–2.688)), the development of jaundice during sorafenib treatment carries 2.192 times higher mortality risk (P value < 0.001, HR 2.192, 95.0% CI (1.756–2.737)), on the other hand shifting to Regorafenib is associated with 0.340 lower risk of mortality (P value < 0.001, Hazard ratio (HR) 0.340, 95.0% CI (0.205–0.566)).
Regarding Regorafenib therapy, Sixty-eight (9.6%) patients were shifted to Regorafenib as a second-line therapy. None of the patients achieved complete response while 17 (27.4%) patients achieved partial response. The most prevalent adverse event was mild elevation of liver enzymes followed by hepatic decompensation and then hypertension. The most common cause of Regorafenib discontinuation was hepatic decompensation (64.2%) (Table 3).
We divided our patients according to the etiology of their underlying chronic liver disease into 3 groups: 622 (88.1%) patients with HCV-related HCC, 15 (2.1%) patients with HBV-related HCC, and 69 (9.8%) patients with non-viral-related HCC. Patients with HBV-related HCC were significantly younger with significantly lower baseline total leucocytes count. Baseline ALT was significantly lower in patients with HCV-related HCC. Baseline AST was significantly higher in patients with HBV-related HCC. These advanced unresectable HCC lesions developed on top of non-cirrhotic liver in 7.1% of patients with HBV and 7.1% of patients with non-viral etiology. On the other hand, it developed on top of 1.3% of patients with non-cirrhotic HCV infection. Extra-hepatic spread was significantly more common in patients with HBV-related HCC (Table 6).
We found no significant difference in the adverse events or the number of patients shifted to Regorafenib among the 3 groups (Supplementary table 4, 5). The median time to progression and the tumor response to treatment with Sorafenib and Regorafenib did not differ between the 3 groups. The median survival time was significantly lower in patients with non-viral-related HCC (218.00 (111.00–454.00)) than in patients with HCV-related HCC 326.50 (151.00- 608.00) P-value 0.048) (Table 6).
As we noticed that some patients could tolerate Sorafenib therapy for longer than 6 months while others did not, we divided our patients according to the duration of sorafenib treatment into those treated < 6 months and those treated > 6 months to study the characteristics of each group. Patients who continued treatment for less than 6 months (38.43%) showed higher baseline AFP, significantly lower number of patients with BCLC-B and more prevalent hepatic vein thrombosis, extra-hepatic spread and significantly worse survival (Table 7).
Patients who continued sorafenib for > 6 months were significantly less likely to develop hypertension, skin lesions, abdominal pain, jaundice, elevated liver enzymes, ascites, and anemia. On the other hand, they were more likely to develop hepatic encephalopathy. They had significantly better performance status after 1 and 3 months of treatment. They also showed better tumor response after 3 months of treatment (P-value < 0.001) with higher incidence of shifting to Regorafenib (Table 7).
Discussion
Sorafenib is one of the HCC therapy guidelines either alone in the advanced stage or combined with loco-regional therapy in the intermediate stage after adequate multidisciplinary assessment. This study reported the characteristics, adverse events and outcome of patients with unresectable HCC treated with Sorafenib and Regorafenib and the impact of the underlying etiology of chronic liver disease.
We recruited our patients following the guidelines of the Egyptian National committee for control of viral hepatitis. The median age of our patients was 62 years with male predominance, 98% of our patients had cirrhosis, with the majority had Child–Pugh class A, 59.5% had BCLC stage B and the others had BCLC C stage, which was in harmony with previous studies20,21.
In our study, the median duration of treatment with Sorafenib was about 8 months. The most common causes for treatment discontinuation were Liver decompensation followed by patient demand. Jaundice was the most prevalent adverse event followed by fatigue, anemia, and elevated liver enzymes. A study by Raoul and colleagues, recruited 188 patients with Sorafenib-treated HCC with variable underlying etiologies (hepatitis C, alcoholic liver disease, NAFLD or undiagnosed), they had a median duration of therapy of 5.4 months. They reported the causes of sorafenib discontinuation as: another therapeutic option, major AEs or patient refusal, or no clear explanation. Their main reported AEs were skin toxicities (29%), elevated liver enzymes (22%), fatigue and weight loss (13%), diarrhea (10%), and hypertension (2%)22.
The response rate in our study was 14.2% while 32% of patients achieved stable disease and 22.8% had progressive disease. In a study done by Ferreira et al., the mean duration of sorafenib therapy was 9.7 months. 84% of their Brazilian patients received 800 mg per day, and the rest received half the dose. Their reported adverse events were diarrhea (33%), hand-foot syndrome (20.5%), mucositis (11.4%), fatigue and nausea (11.4%). They reported HCC progression in 48.4% of patients21.
On the other hand, Lee and his colleagues (2019) reported that of 222 Sorafenib-treated patients; eight (3.6%) achieved partial response (PR), 82 (36.9%) had stable disease (SD), 132 (59.5%) had progressive disease (PD) and none achieved complete response. Correlation between adverse events (AEs) and therapeutic responses revealed; hand-foot syndrome, hypertension, and diarrhea were (62.4%, 37.5%, and 25%) in the PR group, 40.8%, 13.4%, and 34.6% in the SD group and in PD group were (25%, 6.9%, and 15.9%)23.
In our study the median OS was 314 days (10.47 months (4.87–20.03)). The independent factors increasing mortality were baseline serum AST, size of HCC, hepatic vein thrombosis, the development of jaundice during treatment while shifting to Regorafenib was associated with lower risk of mortality. Similar to Rovesti et al.24, An independent predictor of a worse prognosis was AST. AST is often elevated by pathological processes that cause tissue damage, increased tumor cell turnover, and a greater proliferative state. We found no difference in survival between elderly and non-elderly patients similar to the retrospective study by Rovesti et al.16, and the prospective cohort study by Di Costanzo et al.25. This suggested that for senior people, sorafenib is deemed safe and effective.
The median OS of Sorafenib-treated patients reported in different studies ranges from 4 up to 17.4 months. It depends on the HCC stage, hepatic efficiency, performance status, and vascular invasion21,22,26,27,28. In addition, the reported predictors affecting OS among different studies are either patient-related factors (age, sex, race, PS, underlying liver disease etiology, albumin-bilirubin grade, neutrophil-to-lymphocyte ratio, Child–Pugh score, AFP, body mass index), tumor-related factors (number and size of the lesions, BCLC staging, extrahepatic spread, vascular invasion, and sorafenib dosage21,22,26,27,28. Our study reports higher survival time than previously reported in Egyptian patients by Nada et al.26 who recruited patients in 2015 (5 months) and Abdel-Rahman et al.29 who recruited patients in 2012 (6.25 months). This could be related to better patients’ selection and higher experience of the medical staff in patients’ management.
Regarding Regorafenib therapy, Bruix et al.6, proved that second line therapy with Regorafenib was associated with a significantly better OS, compared to placebo [10.6 versus 7.8 months, respectively]. A different phase II research conducted in 2013 by Bruix et al.30 with 36 patients with HCC shown good anticancer efficacy and accepted tolerability of Regorafenib, with a median OS of 13.8 months and a TTP of 4.3 months. In the Granito et al. study31, 216 Asian patients with Regorafenib-treated HCC achieved an OS of 10.6 months compared to 7.8 months with placebo with a 37% reduction in the risk of mortality and a 54% reduction in the risk of progression. They reported objective response in 11% of patients. Their reported AEs were hypertension (15%), hand-foot syndrome (13%), fatigue (9%), and diarrhea (3%). Regorafenib discontinuation was due to: elevated AST (2%), hand-foot syndrome (2%) and elevated ALT (1%).
We reported that OS was significantly lower in non-viral patients with sorafenib-treated HCC compared to viral-related HCC. Rovesti et al.24 reported that Sorafenib-treated patients with non-viral etiology had poorer OS than patients with viral etiologies. This could be attributed to non-screening of patients with non-viral chronic liver diseases, thus their HCC is diagnosed at an advanced stages. In addition, subgroup analysis of the SHARP and AP trials suggested a different sorafenib efficacy in patients with viral etiology. The mechanisms of action of Sorafenib, together with the diversity in tumor microenvironment, are capable of justifying the dissimilar antitumor profile. Bruix et al., reported a survival benefit favoring sorafenib over placebo was observed in patients with hepatitis C, low NLR and without extrahepatic spread32.
According to reports from 200833, Egypt has the greatest HCV load in the world, with over 94% of patients having genotype 434,35. Since the advent of direct-acting antiviral treatment (DAAs), the seroprevalence of HCV infection has decreased to 6.3%5 in 201536, with an overall estimated 30% decrease in prevalence37. By 2018, nearly 2 million CHC patients got DAAs, accounting for 40% of the infected population, and SVR rates exceeded 90%38. This is why most patients in our study have HCV-related HCC. After the nationwide HBV vaccination in 1992, chronic hepatitis B, which was formerly Egypt’s second leading cause of HCC after HCV, dropped to third position.
NAFLD-related HCC was the most likely underlying etiology of the non-viral HCC in our patients. We excluded a number of underlying chronic liver diseases in our patients with nonviral HCC based on their medical history, lab test results, and clinical characteristics. These conditions included hemochromatosis, Wilson disease, primary sclerosing cholangitis, primary biliary cholangitis, and autoimmune liver disease. None of our patients had ever consumed alcohol since they were all pious Muslims.
In this study, Patients who continued treatment for less than 6 months (38.43%) showed higher baseline AFP, less patients with BCLC-C than B and more prevalent hepatic vein thrombosis, extra-hepatic spread and with significantly worse OS. Chan et al.39 reported that 15.49% of their patients could tolerate Sorafenib therapy for at least 6 months, decreasing to only 4.9% with sorafenib treatment > 12 months. They mentioned that it could be attributed to Sorafenib dose, performance status and the HCC tumor characteristics. It was reported that Sorafenib is only beneficial for about 30% of patients, but within 6 months, most of these individuals develop drug resistance40. For this reason, we decided to use the 6-month period to split our patients based on how long they had been receiving sorafinib medication. Therefore, it is essential to carefully assess each patient’s features and the events that have occurred during their sorafenib treatment in order to determine which individuals are best suited to continue on sorafenib and which ones should undergo Regorafenib as a second-line treatment.
Limitations of the study include its retrospective design. The number of patients with HCV-related HCC markedly exceeds the 2 other etiological groups but this reflects the true percentage of each etiology in the Egyptian patients with HCC. In addition, limited Regorafenib subgroup analysis (small in number) weaken generalizability and Only 68% of patients had evaluable mRECIST criteria as some patients lost follow-up before they perform the first on-treatment imaging modality either due to patients’ death, unwillingness to continue therapy or patient absence and could not be reached. Our study’s key advantages are its considerable sample size and patient participation across multiple centers. We examined medical data that was gathered in real-world settings, simulating typical medical care and offering significant external validity.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Arnold, M. et al. Global burden of 5 major types of gastrointestinal cancer. Gastroenterology 159(1), 335-349.e15 (2020).
Heimbach, J. K. et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67(1), 358–380 (2018).
Erstad, D. J. & Tanabe, K. K. Hepatocellular carcinoma: early-stage management challenges. J. Hepatocell Carcinoma. 4, 81–92 (2017).
Lei, C. et al. Curative effect of endostar combined with oxaliplatin in the treatment of primary hepatic carcinoma and its influence on immune cells. Oncol. Lett. 17(4), 3665–3670 (2019).
Cheng, A. L. et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 10(1), 25–34 (2009).
Bruix, J. et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 389(10064), 56–66 (2017).
Bruix, J., Chan, S. L., Galle, P. R., Rimassa, L. & Sangro, B. Systemic treatment of hepatocellular carcinoma: An EASL position paper. J. Hepatol. 75(4), 960–974 (2021).
Inuzuka, T. et al. Complete response of advanced hepatocellular carcinoma with multiple lung metastases treated with sorafenib: A case report. Oncology 81(Suppl 1), 152–157 (2011).
Vincenzi, B. et al. Early skin toxicity as a predictive factor for tumor control in hepatocellular carcinoma patients treated with sorafenib. Oncologist 15(1), 85–92 (2010).
Llovet, J. M. et al. Sorafenib in advanced hepatocellular carcinoma. N Engl. J. Med. 359(4), 378–390. https://doi.org/10.1056/NEJMoa0708857 (2008).
Kudo, M. et al. Real-world sorafenib use in patients with advanced hepatocellular carcinoma: The GIDEON study. Liver Canc. 5(3), 204–216. https://doi.org/10.1159/000367745 (2016).
Zhang, X. et al. Efficacy of sorafenib in patients with HBV vs HCV-related hepatocellular carcinoma: A meta-analysis. Hepatol. Int. 11(5), 361–369. https://doi.org/10.1007/s12072-017-9807-4 (2017).
Hiraoka, A. et al. Impact of liver disease etiology on the therapeutic efficacy of sorafenib: Real-world data from a Japanese registry. Cancer Med. 9(21), 8164–8173. https://doi.org/10.1002/cam4.3419 (2020).
Kudo, M. et al. GIDEON (Global Investigation of therapeutic DEcisions in hepatocellular carcinoma and of its treatment with sorafeNib): Second interim analysis. Liver Cancer. 5(3), 204–216. https://doi.org/10.1159/000367745 (2016).
Cheng, A. L. et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: A phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 10(1), 25–34. https://doi.org/10.1016/S1470-2045(08)70285-7 (2009).
Ikeda, M. et al. Analysis of adverse events of sorafenib in Japanese patients with hepatocellular carcinoma: Special reference to skin toxicities. Oncology 87(6), 327–336. https://doi.org/10.1159/000367939 (2014).
Zhu, A. X. et al. Biomarkers and molecular profiling of sorafenib efficacy in hepatocellular carcinoma: A review. Cancer 121(11), 1989–2001. https://doi.org/10.1002/cncr.29240 (2015).
Marrero, J. A. et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American association for the study of liver diseases. Hepatology 68(2), 723–750 (2018).
Lencioni, R. & Llovet, J. M. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 30(1), 52–60 (2010).
Cardoso, H. et al. Hepatocellular carcinoma treatment with sorafenib: Real-life evaluation of prognostic factors and a practical clue for patient management. GE Port J. Gastroenterol. 23(5), 243–248 (2016).
Ferreira, C. P. D. C., Ribeiro, M. A. & Szutan, L. A. Overall survival predictors in hepatocellular carcinoma patients treated with sorafenib. Rev. Assoc. Med. Bras. (1992) 66(3), 275–283 (2020).
Raoul, J. L. et al. Sorafenib: Experience and better management of side effects improve overall survival in hepatocellular carcinoma patients: a real-life retrospective analysis. Liver Canc. 8(6), 457–467 (2019).
Lee, S. W. et al. Sorafenib-Related adverse events in predicting the early radiologic responses of hepatocellular carcinoma. Gastroenterol. Res. 12(1), 16–20 (2019).
Rovesti, G. et al. Impact of Baseline characteristics on the overall survival of hcc patients treated with sorafenib: Ten years of experience. Gastrointest Tumors. 6(3–4), 92–107 (2019).
Di Costanzo, G. G. et al. Impact of age on toxicity and efficacy of sorafenib-targeted therapy in cirrhotic patients with hepatocellular carcinoma. Med. Oncol. 30(1), 446 (2019).
Nada, Y. et al. Outcomes of treatment with sorafenib in Egyptian patients with hepatocellular carcinoma: A retrospective cohort study. Expert Rev. Gastroenterol. Hepatol. 12(1), 99–107 (2018).
Straś, W. et al. Overall survival in patients with hepatocellular carcinoma treated with sorafenib: A polish experience. Med. Sci. Monit. 27, e931856 (2021).
Soria, A. et al. Survival and adverse events of elderly patients treated with sorafenib for hepatocellular carcinoma. Front Oncol. 12, 829483 (2022).
Abdel-Rahman, O. et al. Sorafenib for Egyptian patients with advanced hepatocellular carcinoma; single center experience. J. Egypt Natl. Canc. Inst. 26(1), 9–13 (2014).
Bruix, J. et al. Regorafenib as second-line therapy for intermediate or advanced hepatocellular carcinoma: Multicentre, open-label, phase II safety study. Eur J Cancer. 49(16), 3412–3419 (2013).
Granito, A. et al. Experience with regorafenib in the treatment of hepatocellular carcinoma. Therap. Adv. Gastroenterol. 14, 17562848211016960 (2021).
Bruix, J. et al. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: Analysis of two phase III studies. J Hepatol. 67(5), 999–1008 (2017).
Alem, S. A. et al. Long-term clinical outcomes in sustained responders with chronic hepatitis C after treatment with direct-acting antivirals. Eur. J. Gastroenterol. Hepatol. https://doi.org/10.1097/MEG.0000000000002240 (2021).
Kouyoumjian, S. P., Chemaitelly, H. & Abu-Raddad, L. J. Characterizing hepatitis C virus epidemiology in Egypt: Systematic reviews, meta-analyses, and meta-regressions. Sci. Rep. 8(1), 1661 (2018).
El-Ghitany, E. M. Hepatitis C virus infection in Egypt: Current situation and future perspective. JHIPH 49(1), 1–9 (2019).
El-Nahaas, S. M. et al. High sustained virologic response rate using generic directly acting antivirals in the treatment of chronic hepatitis C virus Egyptian patients: single-center experience. Eur. J. Gastroenterol. Hepatol. 30(10), 1194–1199 (2018).
Shousha, H. I. et al. Assessment of facility performance during mass treatment of chronic hepatitis C in Egypt: Enablers and obstacles. J. Infect Public Health. 13(9), 1322–1329 (2020).
Waked, I. et al. Screening and treatment program to eliminate hepatitis C in Egypt. N Engl. J. Med. 382(12), 1166–1174 (2020).
Chan, K. M. et al. Implementation of sorafenib treatment for advanced hepatocellular carcinoma: An illustration of current practice in Taiwan. Cancer Manag Res. 11, 1013–1021 (2019).
Tang, W. et al. The mechanisms of sorafenib resistance in hepatocellular carcinoma: Theoretical basis and therapeutic aspects. Signal Transduct Target Ther. 5(1), 87 (2020).
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
Eman MF Barakat, Mohamed El-Kassas, Mohamed Kohla, Hend Ibrahim Shousha, Ehab F. Moustafa, were responsible for Conceptualization of the work, Hossam Dabees, Mohamed Omar Abdelmalek, Aly Azmy, Walaa Mosaad Aboganob , Hossam Taha, Ahmed Radwan, Dalia Ghoraba, Mostafa Elhelbawy, Mohamed A. Medhat, Safaa Ragab Askar, Eman Marwan, Eman Rewisha, Tamer Elbaz, Sayed Hassan Ahmed, Nevien Fouad elfouly, Nermeen Abdeen, Ahmed Hosni Abdelmaksoud, Asmaa A. Abdeltawab, Mostafa Abd Alfattah Shamkh, Ammar Alrajhi, Ahmed Ramadan were responsible for the methodology, Mohamed Mahmoud nabeel, Anwar Nassief performed the statistical analysis, Ahmed Tawheed, Rania Lithy, Mohamed Kohla, Hamdy Sayed, Dalia Ghoraba, Nevien Fouad elfouly, wrote the original draft of the manuscript, Ashraf Omar Abdelaziz, Mohamed Said, Hend Ibrahim Shousha, Mona Shoukry Aziz, Eman Elkhateeb, Yasser Arafat Abdelrazek, Mohamed Bassam, Sayed Ahmed Sayed, Rasha Salah Hussein, Allam Elsayed Allam, Omnia A. Seyam reviewed and edited the manuscript. All authors read and approved the final manuscript
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The protocol was approved by the ethics committees of Cairo University’s Faculty of Medicine (number: N-336-2023), Ain-Shams University’s Faculty of Medicine (number: FMASU-R36-2024), and Assiut University’s Faculty of Medicine (number: 04-2023-300142).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Barakat, E.M.F., Kohla, M., Dabees, H. et al. Tyrosine kinase inhibitors were well-tolerated among patients with different etiologies of advanced HCC with lower survival in non-viral patients. Sci Rep 15, 20323 (2025). https://doi.org/10.1038/s41598-025-05828-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-05828-x
Keywords
This article is cited by
-
Real-world outcomes and predictive factors in hepatocellular carcinoma patients treated with sorafenib: an 18-month ambispective cohort analysis
Future Journal of Pharmaceutical Sciences (2025)