Abstract
Ulcerative colitis (UC) is a chronic, idiopathic inflammatory disease affecting the gastrointestinal tract. Hongyuyin (HYY), a traditional Chinese botanical formulation, has been effectively treating UC for over three decades; however, its underlying biological mechanism of action in UC-associated intestinal fibrosis (IF) remains unclear. This study investigated the mechanisms of action of HYY on IF through in vivo experiments using a dextran sulfate sodium (DSS)-induced mouse colitis model. Clinical symptoms, colonic pathological damage, inflammation, and fibrosis were monitored across all groups. Both transcriptomic analysis and network pharmacology (NP) techniques were utilized to elucidate the mechanistic insights. HYY treatment substantially reduced inflammation, fibroblast activation, and collagen deposition in UC mice. KEGG analyses suggested that HYY treatment modulated multiple signaling pathways, notably the TNF, IL-17, and PI3K-Akt signaling pathways. Combined analysis identified the PI3K-Akt signaling pathway as a major contributor, with high enrichment factors and numerous enrichment genes involved (IL-6, CSF3, SPP1, AKT1, PIK3CA, and so on) in UC-associated IF. Western blotting confirmed significant reductions in both p-AKT/AKT and p-mTOR/mTOR ratios after HYY treatment. Collectively, HYY alleviates UC-associated IF by reducing the phosphorylation of PI3K-Akt pathway factors, thereby inhibiting fibroblast activation and collagen deposition. This research provides novel insights into HYY’s mechanism of action in UC-associated IF management.
Similar content being viewed by others
Introduction
Ulcerative colitis (UC) is one of the two key forms of inflammatory bowel disease (IBD), it is characterized by chronic and recurring inflammation of the gastrointestinal tract1. The global incidence of UC continues to rise, leading the World Health Organization to classify it as a “modern intractable disease”. Its recurrent nature and unpredictable progression impose a substantial financial burden on medical treatment2. Patients with UC present with abnormal intestinal immune responses, where disruption of the mucosal barrier results in ulceration, edema, erosion, bleeding, and electrolyte loss. Intestinal fibrosis (IF) is a common IBD complication3. Whereas fibrotic complications frequently occur in IBDs affecting the ileum, IF further manifests in colonic Crohn’s disease and UC. IF leads to abnormal colonic motility, anorectal dysfunction, and rectal urgency, often accompanied by fecal incontinence. It may progress to intestinal narrowing and bowel obstruction, considerably diminishing quality of life4. The prevalence of IF among patients with chronic and progressive UC reaches 11% and may result in substantial colonic shortening5. However, the pathogenesis of IF remains poorly understood. Research findings support the classification of UC-related IF as a progressive disease, with extracellular matrix (ECM) deposition across the full thickness of the colonic wall in both adults and pediatric patients with UC6. Inflammation is central to triggering IF; nonetheless, existing anti-inflammatory therapies offer limited efficacy in preventing or alleviating IF. Considering the correlation between IF severity and inflammatory activity, a UC-associated IF model may serve as a valuable platform for developing future anti-IF treatments, emphasizing the importance of research advancements in IF prevention and therapy.
Traditional Chinese Medicine has shown promise in UC management because of its theoretical developments and advantages, including minimal adverse effects7,8,9. Hongyuyin (HYY) has been clinically utilized for over three decades. It effectively alleviates UC inflammation, protects mucosal barrier function, prevents IBD-related anal fistula, reduces healing time, and improves induration symptoms. Previous studies have provided quantifiable, pathological, and molecular biology evidence supporting HYY’s effectiveness in UC management10,11,12,13,14. Furthermore, several HYY-derived drug monomers have effectively managed UC through in vitro experiments15,16.
Nevertheless, detailed and systematic investigations into the efficacy and mechanisms underlying HYY in inhibiting UC-associated IF are lacking. High-throughput transcriptomic sequencing enables investigating drug mechanisms in key signaling pathways associated with intestinal inflammation and fibrosis in UC17. Concurrently, a network pharmacology (NP) approach utilizing publicly available databases and identified compounds facilitates investigating HYY’s compounds from a molecular perspective. This study, combining transcriptomics and NP, represents the first investigation into HYY’s role in regulating IF in a UC mouse model.
Results
Ultra-performance liquid chromatography coupled to quadrupole time-of-flight mass spectrometry(UPLC-Q-TOF-MS) analysis
Through multi-level mass spectrum data, together with the Natural Products HR-MS/MS Spectral Library 1.0 and relevant literature, 43 compounds were identified in HYY. These compounds were: uridine, gallic acid, guanosine, 5-hydroxymethylfurfural, 7-o-galloyl-sedoheptulose, vanillic acid 1-o-β-d-glucopyranoside, 3,4-dihydroxyphenethyl glucoside, erigeside C, salidroside, cuneataside C, (2R,3R,4R,5R)-N-[(4-ethenylphenyl)methyl]-2,3,6-trihydroxy-5-methyl-4-[(2R,3R,4 S,5R,6R)-3,4,5-trihydroxy-6-(hydroxymethyl)oxan-2-yl]oxyhexanamide, 8-epiloganin; morroniside, chlorogenic acid, cryptochlorogenic acid, 1-O-α-rhamnopyranosyl-(1’’→6’)-O-β-D-glucopyranosyl-2-methoxy-4-acetylphenol, 1,7-di-O-galloyl-D-sedoheptulose, sweroside, loganin, isovitexin 7,2’’-di-O-glucoside; isovitexin-7-O-glucoside, logmalicid A, logmalicid B, isoorientin, liriodendrin, calycosin-7-O-β-D-glucoside, isovitexin, calceolarioside B, acanthoside B, cornuside, calycosin, ononin, apigenin-7-O-β-D-glucuronide, calycosin-7-O-β-D-glucoside-6’’-O-acetate, methylnissolin-3-O-glucoside, acacetin, formononetin, (3β,4β,20α,22β)-29-(β-D-Glucopyranosyloxy)-22, 23-dihydroxy-29-oxoolean-12-en-3-yl2-O-β-D-xylopyranosyl-β-D-glucopyranosiduronic acid, astragaloside IV, sargentodoxoside A, astragaloside II, astragaloside I, and isoastragaloside I. The chromatogram is shown in (Fig. 1), and detailed compound information is summarized in Supplementary Tab. S1.
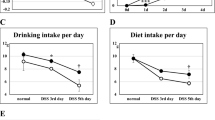
HYY alleviates clinical symptoms of UC
Animal experiments were conducted per the established protocol. Clinical symptoms of UC, including bloody stool, diarrhea, weight loss, and elevated Disease Activity Index (DAI), were observed in all mice in the DSS group. However, UC mice treated with HYY demonstrated significantly reduced body weight loss (Fig. 2A) and lower DAI scores (Fig. 2B) than untreated mice. Anatomical examination suggested that the intestinal contents of the DSS + HYY group maintained healthy morphology, without loose stools or obstruction. The intestinal surface appeared smooth, lacking noticeable inflammation or tissue thickening. In contrast, the DSS group mice exhibited marked adhesion between the colon and surrounding tissues, shortened colons, and thickened and edematous intestinal walls, along with partial submucosal congestion, bleeding, and ulcers (Fig. 2C). Colonic lengths were compared among groups to further evaluate the anti-UC effect of HYY. HYY prevented colon shortening in DSS-induced UC mice (Fig. 2D). Collectively, HYY effectively ameliorated clinical symptoms of UC.
HYY alleviates clinical symptoms of UC. (A) Body weight, (B) DAI. The DSS group exhibits significantly elevated DAI and reduced body weight than the Norm group. Data are presented as the mean ± standard deviation (SD) (n = 10 per group). ### p-value <0.001 vs. Norm group. ** and *** respectively indicate p-values of <0.01 and 0.001 vs. DSS group, respectively. (C,D) Colonic length. The protective effect of HYY in DSS-induced reduction in colon length. Data are presented as the mean ± SD (n = 10 per group). * and ** indicate p-values of <0.05 and 0.01, respectively.
HYY alleviates colon pathological damage and inflammation in UC mice
Hematoxylin and eosin (H&E) staining (Fig. 3A) suggested that the Norm group exhibited intact colonic mucosa with well-preserved epithelial architecture, natural folds, elongated columnar colonocytes, abundant goblet cells, and intact crypts. In contrast, the DSS group demonstrated extensive damage to crypts and goblet cells, replacement by connective tissue, and the absence of epithelial cell regeneration (yellow solid lines). Additionally, inflammatory cell infiltration extended from the mucosal layer to the submucosa (yellow arrows). HYY treatment ameliorated DSS-induced histological damage, as evidenced by crypt regeneration, the restoration of mucosal integrity, and significantly reduced inflammatory infiltration, with only minimal inflammatory cells remaining in the mucosa. The H&E score for the DSS + HYY group was significantly lower than that for the DSS group (Fig. 3B). Moreover, serum levels of pro-inflammatory factors suggested that HYY treatment substantially reduced IL-6 and TNF-α levels than in untreated UC mice (Fig. 3C).
HYY attenuates colonic damage and inflammation in UC mice. (A) H&E-stained images of colonic tissue (×200 magnification). Black arrows indicate intact crypts. Yellow solid lines outline areas with crypt destruction, goblet cell loss, and connective tissue replacement. Yellow arrows indicate inflammatory infiltration. (B) H&E score analysis (n = 10 mice per group). (C) Serum levels of IL-6 and TNF-α, as determined using ELISA (n = 3 per group). Data are presented as the mean ± SD. *, **, ***, and ***** indicate p-values of < 0.05, 0.01, 0.001, and 0.00001, respectively. Each experiment was conducted in triplicate.
HYY attenuates fibrosis in colitis
Colonic fibrosis is characterized by the excessive accumulation of collagen and the elevated expression of fibrosis-related factors. In this study, colonic tissues from various experimental groups underwent Masson’s trichrome staining to elucidate the effect of HYY treatment on collagen deposition and fibrosis. The DSS group demonstrated collagen deposition and hyperplasia of colonic fibrous connective tissue compared with the Norm group, as evidenced by blue-stained regions. However, mice of HYY-treated group showed significant reductions in the collagen deposition and collagen volume fraction (CVF) (Fig. 4A,C). The mucosal layer maintained its integrity, with regularly organized glands and goblet cells. Additionally, it exhibited no signs of fibrotic hyperplasia.
Immunohistochemical staining with α-smooth muscle actin (α-SMA) antibody suggested increased α-SMA expression in the basal region of the mucosa in the DSS group, identified by brown-stained regions (Fig. 4B), suggesting fibroblast activation. In the DSS + HYY group, the mucosa maintained relative integrity, with less α-SMA expression. In parallel, reduced mRNA expression of the pro-fibrotic genes, including transforming growth factor-β1 (TGF-β1) and α-SMA, was observed in colonic tissue homogenates in the DSS + HYY group, compared with the DSS group (Fig. 4D). Thus, HYY effectively inhibited collagen deposition and IF development. Collectively, HYY shows promising translational potential for the management of inflammation and fibrosis in UC.
HYY alleviates UC-associated IF. (A) Masson’s trichrome staining of colonic tissue (×200 magnification), blue stain (arrows indicate) = collagen. (B) Immunohistochemical staining with α-SMA antibody, brown stain (arrows indicate) = α-SMA. (C) Collagen volume fraction (CVF) of Masson’s trichrome staining (n = 10 per group). (D) RT-qPCR analysis of TGF-β1 and α-SMA mRNA expression levels in intestinal tissues (n = 5 per group), with experiments performed in triplicate. Data are presented as the mean ± SD. *, **, and *** indicate p-values of <0.05, 0.01, and 0.001, respectively.
Identification of the differentially expressed genes (DEGs) associated with the anti-IF effect of HYY
RNA-seq analysis was conducted to investigate the primary MOA of HYY in UC-associated IF management. DEGs were identified between the DSS and Norm groups, as well as between the DSS + HYY and DSS groups (Fig. 5A). A total of 148 genes were upregulated after DSS induction, of which 31 were subsequently downregulated after HYY treatment, potentially contributing to UC and IF progression. Additionally, 32 genes were downregulated after DSS induction, with three upregulated after HYY treatment, possibly exhibiting an inhibitory effect on UC and IF (Fig. 5B). Comparison of the 34 DEGs with IF-related target genes using the Venn diagram tool (https://bioinfogp.cnb.csic.es/tools/venny/) identified 27 overlapping targets, indicating potential transcriptomic targets for HYY in UC-associated IF.
GO term and KEGG pathway enrichment analyses of potential anti-IF targets of HYY
GO enrichment analysis identified 345 BPs, 17 Cellular Components (CC), and 37 Molecular Functions (MF) (Fig. 5C-A). The leading 10 enriched terms in each domain were visualized using a bubble chart. In BP domain, the predominant terms were “response to bacteria”, “cellular response to lipid”, and “cellular response to cytokine stimulus”. The CC analysis identified “specific granules”, “secretory granule lumen”, and “tertiary granule lumen” as the leading terms. The MF analysis identified “cytokine activity”, “chemokine activity”, “G protein-coupled receptor binding”, and “receptor-ligand activity” as the leading terms. KEGG pathway enrichment analysis visualized the leading 20 pathways using a bar chart (Fig. 5C-B). They predominantly comprised TNF, IL-17, PI3K-Akt, and cytokine-cytokine receptor interaction signaling pathways.
PPI network construction and validation of HYY-associated key anti-IF genes
A PPI network was constructed using the STRING database (https://cn.string-db.org/) based on the 27 DEGs. Furthermore, gene interactions were visualized using Cytoscape 3.9.1 software (Fig. 5D). The cytoHubba plugin identified 20 hub genes using Degree algorithms (Fig. 5E). The leading 10 genes (IL-6, LCN2, CSF3, CCL20, CXCL1, LTF, CXCL2, CAMP, SPP1, and MMP3) were identified as key targets, with IL-6 emerging as the hub gene. These 10 genes were validated using qPCR (Fig. 5F). The colonic expression of key genes was elevated in the DSS group, compared with the Norm group. In contrast, HYY treatment resulted in reduced colonic expression levels, aligning with the transcriptome sequencing results.
Transcriptomic analysis of the anti-IF MOA of HYY in DSS-induced UC mice. (A) Volcano plots showing DEGs between the DSS and Norm groups, as well as between the DSS + HYY and DSS groups (n = 3 per group). (B) Venn diagram showing the overlap of upregulated and downregulated DEGs. Twenty-seven common genes associated with both IF and HYY’s anti-UC effect are shown. (C-A,B) The 10 most enriched GO pathways (BP, CC, and MF) and 20 most enriched KEGG pathways18,19 are identified using Metascape (http://metascape.org/). (D) PPI network constructed using Cytoscape 3.9.1 software, with upregulated genes in red and downregulated genes in blue. (E) Leading 20 DEGs defined by Degree analysis in the cytoHubba plugin. Ellipses represent individual genes, and lines represent gene interactions. The gradient color from red to orange to yellow indicates the interaction strength, from high to low. (F) Validation of the leading 10 anti-IF genes involved in HYY treatment of UC mice. Data are presented as the mean ± SD (n = 5 per group), with experiments performed in triplicate. #, ##, and ### respectively indicate p-values of <0.05, 0.01, and 0.001 vs. the Norm group. *, **, and *** respectively indicate p-values of <0.05, 0.01, and 0.001 vs. the DSS group.
Prediction of HYY candidate targets in UC-associated IF
Compounds identified in HYY by UPLC-Q-TOF-MS underwent NP analysis. Target fishing identified 2,327 HYY-related targets. Using “ulcerative colitis” and “intestinal fibrosis” as the keywords, 3,956 UC-related and 9,318 IF-related targets were retrieved. A Venn diagram tool (https://bioinfogp.cnb.csic.es/tools/venny/) yielded 384 overlapping genes among the HYY-, UC-, and IF-related targets. They were identified as candidate targets for HYY treatment of UC-associated IF (Fig. 6A).
PPI network construction and analysis
The STRING database (https://cn.string-db.org/) facilitated constructing a PPI network based on the 384 candidate targets involved in the inhibitory effect of HYY on UC-associated IF. Overall, 342 nodes with 2,173 edges were generated (Fig. 6B). Larger and darker-colored nodes indicate higher degrees of connectivity and influence. Table 1 lists the leading 10 targets ranking by degree, including EGFR, AKT1, SRC, STAT3, IL-6, TNF, and so on. The leading 10 hub genes were also identified using the MCC algorithm in the cytoHubba plugin, including EGFR, AKT1, SRC, PIK3CA, PIK3R1, PTPN11, PTK2, PIK3CB, LYN, and VAV1 (Fig. 6C).
GO term and KEGG pathway enrichment analyses of candidate targets
GO term enrichment analysis indicated 2,824 BP, 208 CC, and 345 MF terms. The enriched BP items primarily comprised “cellular response to nitrogen compounds”, “phosphorylation”, and “positive regulation of cell migration and motility” (Fig. 6D-A). The leading CC terms were “Cytoplasmic vesicle lumen”, “vesicle lumen”, and “secretory granule lumen”. The leading MF terms were “Kinase activity”, “phosphotransferase activity”, “transcription factor binding”, “oxidoreductase activity”, and “cell adhesion molecule binding”. KEGG pathway enrichment analysis (Fig. 6D-B) highlighted significantly enriched pathways associated with candidate targets, including the PI3K-Akt, cancer, and other related pathways.
Compound–target–pathway network for HYY treatment of UC-associated IF
A compound-target-pathway network comprising 186 nodes and 633 interacting edges was constructed using Cytoscape 3.9.1 based on the active compounds, candidate targets, and KEGG pathways (Fig. 6E). The nodes correspond to 37 chemical compounds, 139 targets, and 10 pathways. Analysis of the topological parameters yielded the leading 15 compounds (Table 2).
NP analysis of the MOA of HYY in UC-associated IF. (A) Venn diagram depicting the intersection among HYY-, UC-, and IF-related targets. (B) PPI network diagram comprising 342 target proteins and 2,173 interacting edges. Node sizes and colors indicate degree values, with larger dark-colored nodes representing higher connectivity. (C) Network diagram shows hub genes, identified using the MCC algorithm. (D-A,B) GO and KEGG pathway18,19 enrichment analyses of candidate targets for HYY treatment in UC-associated IF. (E) Compound–target–pathway network containing 186 nodes and 633 interacting edges. Blue circles represent compounds, yellow rhombi represent targets, and red v-shaped nodes represent the 10 KEGG pathways.
Joint transcriptomic and NP analyses of the inhibitory effect of HYY on UC-associated IF
To provide comprehensive insights into the MOA of HYY in UC-associated IF, a network was established using Cytoscape 3.9.1. It consisted of 21 potential genes, 6 common targets (IL-6, MMP3, LTF, FGF23, SLC6A4, and SPHK1), and 378 candidate targets, establishing a Potential Target-Candidate Target network diagram (Fig. 7A). Of these, IL-6, MMP3, and LTF demonstrated the highest degree values, indicating their key role. Transcriptomic analysis suggested that IL-6, MMP3, and LTF are key anti-IF genes involved in HYY treatment in UC mice, which was further confirmed through RT-qPCR (Fig. 5F).
Common pathways identified through transcriptomic and NP analyses were selected using the Venn diagram tool (https://bioinfogp.cnb.csic.es/tools/venny/). Two pathways were identified: PI3K-Akt and chemokine signaling pathways (Fig. 7B). The PI3K-Akt pathway exhibited a higher enrichment factor (EF) and encompassed more genes, including IL-6, CSF3, and SPP1 (key genes from transcriptomics) and AKT1, PIK3CA (hub genes from NP). It was selected as the primary pathway for further investigating the inhibitory effect of HYY on UC-associated IF.
Subsequently, WB analysis was conducted to investigate the mechanism by which HYY inhibits UC-associated IF via the PI3K/Akt/mTOR pathway. Changes were observed in both p-AKT/AKT and p-mTOR/mTOR ratios (Fig. 7C-A,B). HYY treatment decreased the expression levels of p-AKT and p-mTOR, which were markedly elevated in the DSS group. Nonetheless, the total expression levels of AKT and mTOR remained unchanged. Notably, significant differences persisted in both p-AKT/AKT and p-mTOR/mTOR ratios between the DSS + HYY and Norm groups. Furthermore, target protein expression in the DSS + HYY group was not comparable to those in the Norm group. Additionally, the DSS group exhibited reduced expression of E-cadherin, compared with the Norm and DSS + HYY groups, suggesting the presence of EMT in the DSS group’s intestinal tissues.
Joint analysis and further validation of the MOA of HYY in UC-associated IF. (A) Potential target-candidate target network diagram. Anti-fibrotic genes identified through transcriptomic analysis are marked as pink circles; anti-fibrotic candidate targets identified through NP analysis are marked as blue circles. Orange squares represent common targets, whereas colors transitioning from red to orange to yellow indicate decreasing interaction. (B) Common pathways identified through transcriptomic and NP analyses. The PI3K-Akt signaling pathway, characterized by higher EF and more enriched genes, is the primary pathway underlying the anti-IF effects of HYY on UC mice. (C-A,B) WB analysis showing protein expression of the PI3K/Akt/mTOR signaling pathway in intestinal tissues of the UC-associated IF mouse model. Full blots are showed in Supplementary Information. HYY treatment decreases expression levels of p-AKT and p-mTOR, whereas both proteins are significantly elevated in the DSS group. The DSS group shows reduced E-cadherin expression, indicating EMT in the intestinal tissue. Data are presented as the mean ± SD (n = 4, 5, and 5), with all experiments conducted in triplicate. *, ***, ****, and ***** indicate p-values of < 0.05, 0.001, 0.0001, and 0.00001, respectively.
Discussion
UC is a chronic inflammatory disease with a rising global prevalence. Its complex and multifactorial pathophysiology involves intricate interactions among environmental, genetic, microbiome-related, and immunological risk factors, together with other potential contributors20. Advancements in DNA sequencing and analysis have substantially enhanced our understanding of the molecular mechanisms underlying UC21,22,23. DSS colitis model that that can simulate the pathological characteristics of UC is an effective tool for evaluating potential therapeutic compounds relevant to human IBDs, particularly UC. In this study, DSS induction produced severe symptoms, including extensive rectal bleeding, considerable body weight loss, severe colitis, intestinal damage, and excessive collagen deposition, all of which are characteristic features of chronic UC and IF. Over secreting of pro-inflammatory factors (IL-6, TNF-α), pro-fibrogenic (TGF-β1), and contractile proteins α-SMA constructed a fibrotic microenvironment from chemical signals and biomechanical pathways, which may result in chronic IF. Treatment with HYY ameliorated these pathological changes in UC mice and restored several parameters to near-normal levels, demonstrating its potential therapeutic benefits in colitis and IF.
DEG analysis identified 27 potential HYY targets in UC-associated IF at the transcriptome level. PPI analysis further highlighted the importance of 10 key genes in UC-associated IF, which were subsequently validated via RT-qPCR. Among these, interleukin-6 (IL-6), colony-stimulating factor 3 (CSF3), lipocalin-2 (LCN2), and osteopontin (SPP1)24 are pro-inflammatory factors from the cytokine family. CCL20, CXCL1, and CXCL2 belong to the chemokine family. MMP3 is a member of matrix metalloproteinases (MMPs), which degrade the ECM, compromise the intestinal epithelial barrier, and facilitate fibroblast migration and proliferation in UC25. Cathelin-related antimicrobial peptide (CAMP), an AMP in mice, exhibits broad-spectrum antimicrobial and immunomodulatory functions and contributes to maintaining epithelial barrier integrity26. UC progression in DSS colitis models of mouse is driven by upregulated genetic regulatory networks involving cytokines, chemokines, additional pro-inflammatory factors, and ECM-degrading enzymes27,28.
Consistent with these findings, HYY-regulated genes are associated with reduced inflammatory signals (IL-6, CCL20, CXCL1, CXCL2, LCN2, and SPP1) and decreased expression of transcripts mediating ECM disruption within colonic MMP3. These molecular changes suggest the inhibition of both colitis and fibrosis29,30. Therefore, the key HYY-targeted genes demonstrating anti-inflammatory and anti-fibrotic properties may serve as potential biomarkers for further investigation.
Additionally, NP analysis was conducted to investigate the molecular MOA of HYY in UC-associated IF. Hub genes (such as EGFR, AKT1, SRC, PIK3CA, PIK3R1, PTPN11, PTK2, PIK3CB, IL-6) were identified by Degree and MCC algorithm. Combined NP and transcriptomic analyses identified six common targets potentially involved in HYY’s anti-IF effect on UC. Furthermore, RT-qPCR experiments indicated significant differences in IL-6, MMP3, and LTF mRNA expression levels, suggesting that these three genes may serve as key MOA targets of HYY in UC-associated IF at both transcriptome and molecular levels. These findings warrant further investigation in future studies.
GO term and KEGG pathway enrichment analyses were conducted based on potential targets or candidate targets separately. GO term analyses indicated that HYY primarily affected biological processes, namely “cellular response to cytokine stimulus”, “phosphorylation” and “positive regulation of cell migration and motility”, together with molecular functions, including “cytokine activity”, “chemokine activity”, “kinase activity”, “phosphotransferase activity”, and “cell adhesion molecule binding”. KEGG analyses suggested that HYY treatment modulated multiple signaling pathways, notably the TNF, IL-17, and PI3K-Akt signaling pathways. Joint pathway analysis identified the PI3K-Akt and chemokine signaling pathways in both transcriptomic and NP KEGG pathway enrichment analyses.
Tumor necrosis factor (TNF), Interleukin-17 (IL-17), and Chemokine signaling pathways are important inflammatory pathways and are closely related to wound healing and fibrosis. In UC, intestinal barrier is damaged, innate immune cells mediate host defense responses, inflammation, and tissue healing, by producing cytokines and chemokines, activating the complement cascade and phagocytosis, or activating the adaptive immune response via presenting antigens31. Because cytokines (such as IL-1β, IL-6, and TNF-α), chemokines (such as CXCL2, CXCL10, CCL8), and growth factors (such as M-CSF, G-CSF) formed a chemotactic gradients, neutrophils are recruited from the circulation to the inflamed tissue32. Macrophages recruit to sections of ulceration following the initial neutrophil inrush. Once at the wound site, macrophages phagocytose ECM and cell debris, and “spent” neutrophils. Meanwhile, mesenchymal cells are exposed to a complex microenvironment which consists of luminal contents and multiple inflammatory mediators. This environment is very likely critical for initiation and perpetuation of IF33. With the extension of inflammation, fibroblasts, myofibroblasts, and smooth muscle cell increase in quantity, migrate to sites of injury and lay down ECM34. Deposition of ECM is a physiological process required for tissue repair, but it becomes excessive and uncontrolled over time in IBD, causing tissue stiffness and functional impairment. Inflammation is necessary to initiate fibrogenesis in UC, suppression of inflammation and subsequent healing do not prevent development of fibrosis35.
TNF and TNF-like ligand 1 A (TL1A)are considered as the principal drivers involved in IBD development, because they promotes inflammation by inducing the production of other pro-inflammatory cytokines (IL-1β, IL-6, IL-17, and so on). TNF and TL1A also indirectly drive IF by furthering inflammation or by acting directly on mesenchymal cells36.TNF promotes fibrosis through increasing the production of collagen I and IV of intestinal myofibroblasts37 and upregulating the expression of TGF-β and tissue inhibitor of matrix metalloproteinases 1 (TIMP1) in colonic epithelial cells38. In this study, HYY treatment inhibited the expression of multiple pro-inflammatory mediators, and downregulated TNF signaling pathway, which may be the main anti-inflammatory MOA of HYY in colitis and IF.
TGF-β1 is widely regarded as the dominant pro-fibrotic growth factor and is upregulated in essentially all fibrotic diseases39. TGF-β1 upregulates α-SMA, collagen I, and fibronectin in human fibroblasts, smooth muscle cell, and in intestinal organoid-associated mesenchymal cells40. Whereas the Smads are seen as the major TGF-β family transducers, TGF-β family proteins also induce non-Smad signaling, including PI3K/AKT/mTOR pathways41. Additional crosstalk between TGF-β-induced AKT activation and Smad complexes explains the requirement for AKT activation in TGF-β-induced EMT42.
The PI3K-Akt signaling pathway regulates cell growth and survival and has been implicated in chronic inflammatory fibrosis across multiple organs and tissues. After lipopolysaccharide (LPS) stimulation of hepatic stellate cells (HSCs), the TLR4 signaling pathway activates the PI3K/Akt/mTOR cascade, which interacts with the downstream Smad3 signaling pathway. This, in turn, leads to HSC activation and ECM production43. Pharmaceutical compounds, such as asiatic acid44tanshinol45and resveratrol46regulate the PI3K/Akt/mTOR pathway, suppressing HSC activation and ECM production, thus mitigating liver fibrosis progression. SHIP, a PI3K-Akt inhibitor, inhibits this pathway upon upregulation, thereby preventing diabetic glomerulosclerosis and renal tubulointerstitial fibrosis.
Limited research exists on the role of the PI3K/Akt/mTOR pathway in UC-associated IF. SHIP-deficient mice develop spontaneous intestinal inflammation and arginase-dependent fibrosis47. The class I PI3K catalytic subunit P110δ serves as a primary driver of intestinal fibrosis in mice48. Furthermore, mast cell tryptase promotes fibroblast differentiation into fibrotic myofibroblasts by activating the PAR-2/Akt/mTOR pathway49. Phellodendrine reduces UC-induced intestinal injury by promoting autophagy through regulation of the AMPK-mTOR signaling pathway50. Collectively, the PI3K/Akt/mTOR signaling pathway may affect UC-induced IF by regulating fibroblast differentiation, although the precise MOA remains unclear.
In this study, PI3K-Akt signaling pathway was selected for WB based on its gene count and high enrichment. Consistent with previous research, elevated p-AKT and p-mTOR levels affirmed the activation of the PI3K-Akt signaling pathway after DSS exposure. HYY treatment, however, reversed this activation. Hence, HYY ameliorates UC-associated IF, partially through the PI3K-Akt signaling pathway.
Besides TGF-β, the pro-inflammatory cytokine IL-17 A was identified as a key inducer of fibrosis51. Evidence showed the regulatory effects of IL-17 in the development of fibrosis in multiple organs, including the lung, liver, kidney, heart, and skin. But its contribution to IBD and IF is still unclear in some extent52. IL-17 signaling is markedly activated in the colon of patients with UC53. In this study, KEGG analyses suggested that HYY treatment modulated IL-17 signaling pathway. The related pharmacodynamic and drug action mechanism, especially, their roles in the development of IF, deserve further study.
Conclusions
In summary, this research advances our understanding of the molecular MOA of HYY treatment in UC-associated IF (Fig. 8)4. HYY reduces UC-associated IF by inhibiting inflammation and decreasing the phosphorylation of core factors in the PI3K-Akt pathway, thereby inhibiting fibroblast activation and collagen deposition. These results provide major insights into the biological MOA of HYY in UC-associated IF. However, the study has some limitations, including only partial, rather than complete, restoration was observed in clinical symptoms, pathological damage, and molecular factors. Future animal studies are warranted to enhance our understanding of individual contributions of HYY compounds or to investigate combination therapies to improve treatment efficacy. Furthermore, in vitro experiments are warranted to evaluate dose-response relationships and confirm the involved cellular pathways.
Experiments and methodology
Experimental design
This study validated the anti-fibrotic effects of HYY on UC-associated IF and elucidated its underlying MOA. The investigation proceeded in several phases. First, UC-associated IF mouse model was established using DSS exposure, followed by the monitoring of clinical symptoms, colonic pathological damage, inflammation, and fibrosis across experimental groups. Second, transcriptomic analysis identified essential genes and pathways, whereas NP analysis was conducted using compounds identified in HYY via UPLC-Q-TOF-MS. The results were integrated to identify key signaling pathways involved in the effects of HYY on UC-associated IF. Finally, the MOA was determined by investigating key signaling pathways and associated targets using WB and RT-qPCR.
Botanical drugs preparation
The four botanical components of HYY (Table 3) were obtained from Longhua Hospital, Shanghai University of Traditional Chinese Medicine. These components underwent soaking, decoction, filtration, concentration, and freeze-drying. They yielded a dry powder at 17.4%. The lyophilized powder was dissolved in purified water (0.108 g/mL, equivalent to 0.62 g crude drug /mL), sterilized under high temperature and pressure, and stored at 4 °C.
Botanical drug characterization
Primary HYY compounds were identified using a Waters H-Class UPLC system (Waters Technology Co., Ltd.) coupled with an AB Sciex Triple TOF® 4,600 high-resolution mass spectrometer (SCIEX). UPLC separation was conducted on a Waters ACQUITY UPLC HSS T3 column (2.1 × 100 mm, 1.6 μm) at 30 °C, with 2 µl injection volumes and 190 to 400 nm detection wavelength. The mobile phases consisted of acetonitrile (A) and distilled water containing 0.1% formic acid (B) delivered at a flow rate of 0.3 ml/min. The mass spectrometer operated in both ESI-negative and ESI-positive ion modes. Gradient conditions and mass parameters are presented in Supplementary Tab. S2, S3. Analyst TF 1.7.1 served as data acquisition software, whereas Peakview 1.2 was used for data processing. Compound identification prioritized matching mass spectrometry data with items in the Natural Products HR-MS/MS Spectral Library 1.0 (Shanghai Standard Technology Co., Ltd.). The library contains multi-level mass spectra of compounds analyzed under various conditions, without any speculated data, ensuring high matching accuracy. Compounds absent from the database were identified through literature reports and mass spectrometric fragmentation patterns.
Experimental animal housing and treatments
Female C57BL/6 mice of SPF-grade, weighing 20 to 22 g, were obtained from Zhejiang Vitonlihua Laboratory Animal Technology Co., Ltd. They were handled per the Laboratory Animal Care guidelines of Shanghai University of Traditional Chinese Medicine, following the recommendations of the US National Institutes of Health and the ARRIVE guidelines (https://arriveguidelines.org) (Ethical approval number: PZSHUTCM210326013). Animals were housed in filter-top cages under pathogen-free conditions at 22 to 25 °C, 50–70% humidity, and a 12-h/12-h light/dark cycle. Standard rodent chow was provided ad libitum. After a 1-week acclimatization period, mice were randomly assigned to three groups (n = 10 per group): a normal control group (Norm group), a UC model group induced with DSS (DSS group), and a DSS-induced UC model group treated with HYY (DSS + HYY group). The DSS and DSS + HYY groups received 2.5% (W/V) reagent-grade DSS (MW 36–50 kDa, MP Biomedicals, Irvine, CA, USA) in drinking water ad libitum for 7 consecutive days (days 1–7, UC induction phase). From day 8 onward, these groups received DSS-free, sterilized distilled water ad libitum for an additional 7 days (fibrosis development phase)54. The Norm group received sterilized distilled water throughout the experiment. Beginning on day 8, the DSS + HYY group received daily gavage with HYY dry powder solution at 1.08 g/kg body weight (five times the clinically equivalent dose) for 7 consecutive days. The Norm and DSS groups received equivalent volumes of sterilized distilled water via gavage. The experimental protocol is illustrated in (Fig. 9).
Disease activity index assessment
Colitis severity was evaluated using the DAI, calculated according to Cooper’s scoring criteria based on body weight, stool consistency, and gross bleeding. DAI was calculated by averaging the scores for body weight loss (0 = none, 1 = 1–5%, 2 = 5–10%, 3 = 10–15%, and 4 = > 15%), stool consistency (0 = normal, 1–2 = loose stool, and 3–4 = diarrhea), and stool bleeding (0 = negative, 1 = +, 2 = ++, 3 = +++, and 4 = ++++).
Sample collection
After treatment completion, mice underwent cervical dislocation. Blood samples were collected and centrifuged at 3,500 rpm for 10 min at 4 °C, and the upper serum layer was stored at − 20 °C for subsequent analysis. The entire colon was extracted from the anus to the ileocecal junction and measured in a relaxed state. After measurement, the colon was longitudinally dissected and rinsed with ice-cold physiological saline. Colonic tissues from the affected area were stored in liquid nitrogen for mRNA transcriptome analysis and molecular and protein factor analyses. A 1 to 2 cm section from the proximal rectal region was immersed in 4% paraformaldehyde for 24 h before histological analysis.
Histopathology
Three-micrometer-thick tissue sections were prepared from paraffin-embedded samples and mounted on glass slides. H&E staining was conducted per standard protocols (H&E, D006-1-4, Nanjingjiancheng, China). Stained sections were examined under a light microscope (OLYMPUS BX43) and photographed. Double-blind scoring was based on the colorectal histopathology scoring standard. Intestinal injury was assessed based on the following parameters: inflammation severity scores (0: none, 1: mild, and 2: severe), invasion depth scores (0: none, 1: mucosal involvement, 2: mucosal and submucosal involvement, and 3: full-thickness colon), and ulcer depth scores (0: none, 1: epithelium, 2: lamina propria, and 3: muscularis mucosae).
Collagen fiber distribution in colonic tissue was visualized using a Masson’s Trichrome Staining kit (G1340, Solarbio, China), where collagen fibers appear blue. Stained sections were examined and photographed under a light microscope. Using Image-Pro Plus 6.0 software, semiquantitative analysis of the collagen volume fraction (CVF), which represents the ratio of the collagen area to the total area of tissue, was performed by adjusting the grayscale values.
Subsequently, tissue sections were deparaffinized and rehydrated through a graded series of ethanol. After antigen retrieval in sodium citrate buffer, sections were treated with 3% H2O2 for 10 min to inactivate endogenous peroxidase. Sections were blocked with 2.5% serum for 1 h and incubated overnight at 4 °C with α-SMA antibody (ab124964, Abcam, Cambridge, UK) (1:1000). They were rinsed three times with PBS and incubated with a secondary antibody for 30 min at room temperature. DAB was applied for color development, with brownish-yellow stain indicating positive immunoreactivity. Images were captured under a light microscope to assess immunohistochemistry changes.
Enzyme-linked immunosorbent assay
Serum levels of IL-6 and TNF-α were measured using ELISA kits (Jiancheng, Biotechnology, Nanjing, China) following the manufacturer’s protocols. Optical density (OD) values were measured on DENLEY DRAGON Wellscan MK 3 (Thermo, Vantaa, Finland), and concentrations were determined using standard curves. IL-6 and TNF-α levels are expressed as pg/mL.
Acquisition of disease-related target genes
Target genes associated with UC and IF were extracted from five databases: DisGeNET (https://www.disgenet.org/), GeneCards (https://www.genecards.org/), On line Mendelian Inheritance in Man (OMIM, https://omim.org/), Therapeutic Target Database (TTD, http://db.idrblab.net/ttd/), and PharmGBK (https://www.pharmgkb.org/) using “ulcerative colitis” and “intestinal fibrosis” as keywords. Genes were standardized and uploaded to the UniProt database (https://www.uniprot.org/) to retrieve UniProt IDs. Duplicate entries were removed to compile the final list of IDs.
Transcriptome sequencing and DEG analysis
Three colon samples were randomly selected from each group as biological replicates. They underwent lysis using RNAiso Plus. Total RNA was extracted using the Trizol Reagent (Invitrogen Life Technologies). RNA concentration, quality, and integrity were assessed using a NanoDrop spectrophotometer (Thermo Scientific). The TruSeq RNA Sample Preparation Kit (Illumina, San Diego, CA, USA) was used to generate sequencing libraries. mRNA was purified from total RNA using poly-T oligo-attached magnetic beads. mRNA was fragmented using divalent cations under elevated temperature and an Illumina proprietary fragmentation buffer. First-strand cDNA synthesis was conducted using random oligonucleotides and SuperScript II, followed by second-strand cDNA synthesis using DNA Polymerase I and RNase H. Exonuclease/polymerase converted the remaining overhangs into blunt ends. Furthermore, the 3′ ends were adenylated. Illumina PE adapters were ligated to enable hybridization. The AMPure XP system (Beckman Coulter, Beverly, CA, USA) purified library fragments to select cDNA fragments of 200 to 300 bp. DNA fragments with ligated adaptor molecules underwent selective enrichment using Illumina PCR Primer Cocktail in a 15-cycle PCR reaction. Final products were purified (AMPure XP system) and quantified using the assay on a Bioanalyzer 2100 system (Agilent) with high-sensitivity DNA Agilent. Sequencing was conducted on the NovaSeq 6000 platform (Illumina, San Diego, CA, USA) by Shanghai Personal Biotechnology Cp. Ltd. RNA sequencing reads were trimmed using Cutadapt 1.18 to remove poly-A tails and low-quality reads. Additionally, they were aligned to the Mus musculus GRCm38 genome via Ensembl. HTseq 0.9.1 generated gene-level count summaries. Differential expression analysis was conducted using the R package DESeq, with a fold change threshold ≥ 1.5 and p-value < 0.05. The R package ggplot2 generated volcano plots. Common DEGs involved in both HYY-induced inhibition of UC and IF-related diseases were identified using the Venn diagram tool (https://bioinfogp.cnb.csic.es/tools/venny/)55. These DEGs may represent common targets at the transcriptome level, contributing to the MOA of HYY in UC-associated IF.
GO term and KEGG pathway enrichment analyses based on transcriptomics
DEG-based enrichment analysis was conducted using Metascape (http://metascape.org/). Enriched GO terms (p-values < 0.05) were identified in the MF, CC, and biological process (BP) domains. The R package ggplot2 visualized the leading 10 GO terms and the leading 20 KEGG pathways, based on the lowest p-values, using bubble or bar charts.
PPI network construction
A PPI network was constructed to assess relationships among the DEGs. The DEGs were submitted to the STRING database (https://cn.string-db.org/), and the analysis involved Homo sapiens proteins with a confidence score ≥ 0.7. Cytoscape 3.9.1 visualized the resulting network. The cytoHubba plugin identified core subnetworks using the Degree algorithm. Consequently, mouse expression of major HYY-associated hub genes was validated.
Prediction of compound targets based on NP analysis
The primary HYY compounds, identified through UPLC-Q-TOF-MS, underwent network pharmacology analysis. SMILES data for these compounds were obtained from the PubChem database (https://pubchem.ncbi.nlm.nih.gov) and analyzed using SuperPred (https://prediction.charite.de/), Pharm Mapper (https://www.lilab-ecust.cn/pharmmapper/), and Swiss Target Prediction (https://www.swisstargetprediction.ch/) to predict potential targets. These targets were standardized to official gene symbols using the UniProt database (https://www.uniprot.org/)56. The Venn diagram tool (https://bioinfogp.cnb.csic.es/tools/venny/) was used to identify intersecting targets among HYY, UC, and IF, which were considered candidate molecular targets for HYY in UC-associated IF management.
PPI network construction and target analysi
Candidate targets were entered into the STRING database (https://cn.string-db.org/) to construct another PPI network, utilizing Homo sapiens proteins with a confidence score ≥ 0.7. The resulting network was exported and visualized using Cytoscape 3.9.1. Three topology parameters, including Degree, Betweenness, and Closeness, were calculated. Hub genes were identified using the Degree and MCC algorithm in the cytoHubba plugin57.
GO term and KEGG pathway enrichment analyses based on NP analysis
Enrichment analyses of the candidate targets were conducted using Metascape (http://metascape.org/). The leading 10 GO terms and leading 20 KEGG pathways, identified by their lowest p-values, were visualized using bubble or bar charts generated using the R package ggplot2.
Construction of compound–target–pathway network for HYY in UC-associated IF
A compound-target-pathway network was established using Cytoscape 3.9.1 to investigate the mechanisms underlying HYY’s impact on UC-associated IF. Key network topology parameters were assessed to identify major compounds and core targets associated with the leading 10 enriched KEGG pathways.
Combination of transcriptomic and NP analyses
An integrated PPI network was developed using Cytoscape 3.9.1 to assess the MOA of HYY in UC-associated IF. Common KEGG pathways were identified by intersecting results from NP and transcriptomic analysis using the Venn tool (https://bioinfogp.cnb.csic.es/tools/venny/). Key genes from the selected pathways were further validated through WB.
Quantitative real-time PCR
Total RNA was extracted using the tissue RNA purification kit (EZBRN001plus, EZBioscience, China). A reverse transcription kit (A0010CGQ, ZBioscience) was used to synthesize complementary DNA (cDNA). Target gene expression was quantified using the Color SYBR Green qPCR Master Mix (A0012-R2, EZBioscience), following the manufacturer’s protocol. The PCR conditions were as follows: 95℃ for 5 s, followed by 95℃ for 15 s and 60℃ for 30 s. GAPDH expression facilitated normalizing target gene expression, and the values were quantified using the 2−∆∆Ct method58. Primer sequences were as follows: TGF-β1, forward GGCGGTGCTCGCTTTGTA, reverse GATGGCGTTGTTGCGGTC; α-SMA, forward CCCTGAAGAGCATCCGACA, reverse CTCCAGAGTCCAGCACAATACC; IL-6, forward AAATGATGGATGCTACCAAACTG, reverse CTCTGGCTTTGTCTTTCTTGTTATC; CSF3, forward CCACCTTGGACTTGCTTCAG, reverse CGCTGGAAGGCAGAAGTG; CXCL1, forward CATGGCTGGGATTCACCTC, reverse ACACCTTTTAGCATCTTTTGGAC; and MMP3, forward TGGTTGCTGCTCATGAACTTG, reverse TCCATAGAGGGACTGAATACCATC. All primers are listed in Supplementary Tab. S4.
Western blotting
Total intestinal protein was extracted using a standard lysis buffer containing protease inhibitors. Total protein concentration was measured using the BCA Protein Assay Kit (cat: G2026, Servicebio, Wuhan, China). Proteins were separated by SDS-PAGE and transferred onto PVDF membranes. They were blocked with skim milk for 1.5 h and incubated overnight at 4 °C with the following primary antibodies (1:1,000) PI3K p110α (CST #4249), AKT (CST #9272), p-AKT(Ser473) (CST #4060), mTOR (CST #2983), p-mTOR (S2448) (ab109268), E-cadherin (CST #14472), and β-tubulin (CST #2146). These antibodies were obtained from CST (Danvers, MA, USA) and Abcam (Cambridge, UK). After washing, the membranes were further incubated with the corresponding secondary antibodies for 1.5 h, at room temperature59.
Statistical analyses
Statistical analyses were conducted using GraphPad Prism 9.0 software, with data expressed as mean ± SD. For normally distributed data, a two-tailed unpaired Student’s t-test was used. Welch’s correction was applied for unequal variances. The Mann–Whitney test was utilized for non-normally distributed data. For multiple group comparisons, one-way ANOVA followed by a Bonferroni test was conducted on normally distributed data. In contrast, the Kruskal–Wallis test with Dunn’s post hoc adjustment was conducted for non-normally distributed data. Statistical significance was set at p-values < 0.05.
Data availability
The RNA-seq datasets generated and/or analyzed during the study are available in the [NCBI (National Center for Biotechnology Information)] repository [https://www.ncbi.nlm.nih.gov/sra/PRJNA1240085].
References
Wangchuk, P., Yeshi, K. & Loukas, A. Ulcerative colitis: clinical biomarkers, therapeutic targets, and emerging treatments. Trends Pharmacol. Sci. 45, 892–903. https://doi.org/10.1016/j.tips.2024.08.003 (2024).
Ng, S. C. et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390, 2769–2778. https://doi.org/10.1016/S0140-6736(17)32448-0 (2017).
Rieder, F., Fiocchi, C. & Rogler, G. Mechanisms, management, and treatment of fibrosis in patients with inflammatory bowel diseases. Gastroenterology 152, 340–350.e6. https://doi.org/10.1053/j.gastro.2016.09.047 (2017).
D’Alessio, S. et al. Revisiting fibrosis in inflammatory bowel disease: the gut thickens. Nat. Rev. Gastroenterol. Hepatol. 19, 169–184. https://doi.org/10.1038/s41575-021-00543-0 (2022).
Gordon, I. O. et al. Fibrosis in ulcerative colitis is directly linked to severity and chronicity of mucosal inflammation. Aliment. Pharmacol. Ther. 47, 922–939. https://doi.org/10.1111/apt.14526 (2018).
Gordon, I. O. et al. Paediatric ulcerative colitis is a fibrotic disease and is linked with chronicity of inflammation. J. Crohns Colitis. 16, 804–821. https://doi.org/10.1093/ecco-jcc/jjab216 (2022).
Liu, Y. et al. Platycodon grandiflorus polysaccharide regulates colonic immunity through mesenteric lymphatic circulation to attenuate ulcerative colitis. Chin. J. Nat. Med. 21, 263–278. https://doi.org/10.1016/S1875-5364(23)60435-2 (2023).
Xie, X. et al. Luteolin ameliorates ulcerative colitis in mice via reducing the depletion of NCR + ILC3 through Notch signaling pathway. Chin. J. Nat. Med. 22, 991–1002. https://doi.org/10.1016/S1875-5364(24)60568-6 (2024).
Cheng, S. et al. Paeonol alleviates ulcerative colitis by modulating PPAR-γ and nuclear factor-κB activation. Sci. Rep. 14, 18390. https://doi.org/10.1038/s41598-024-68992-6 (2024).
Wang, J. W. et al. A retrospective study on therapeutic effect of Hongyuyin combined with cut and suture-dragging therapy for perianal fistulizing crohn’s disease. Shanghai J. TCM. 55, 53–57. https://doi.org/10.16305/j.1007-1334.2021.2104011 (2021).
Dong, R. X., Jiang, X. Y., Lu, J. G. & Wang, J. W. Effects of Hongyuyin on inflammatory bowel disease induced by dextran sodium sulfate in mice. Chin. Traditional Patent Med. 45, 1803–1809. https://doi.org/10.3969/j.issn.1001-1528.2023.06.010 (2023).
Dong, R. X., Lu, J. G. & Wang, J. W. Effects of Hongyuyin inhibiting oxidative stress on inflammatory bowel disease induced by dextran sodium sulfate in mice based on Nrf2/HO-1 signaling pathway. Lishizhen Med. Materia Med. Res. 35, 89–93. https://doi.org/10.3969/j.issn.1008-0805.2024.01.22 (2024).
Chen, X., Dong, Y. & Cao, Y. Q. Effects of Hongyu Decoction on pyroptosis pathway of NLRP3/Caspase-1/ASC cells in mice with ulcerative colitis. China J. Traditional Chin. Med. Pharm. 38, 2901–2907 (2023).
Xu, X. et al. Clinical efficacy of Hongyuyin in promoting wound healing after anal fistula surgery. World J. Integr. Traditional Western Med. 18, 2268–2274. https://doi.org/10.13935/j.cnki.sjzx.231125 (2023).
Wang, J. W., Pan, Y. B., Cao, Y. Q., Zhou, W. & Lu, J. G. Salidroside regulates the expressions of IL-6 and defensins in LPS-activated intestinal epithelial cells through NF-κB/MAPK and STAT3 pathways. Iran. J. Basic. Med. Sci. 22, 31–37. https://doi.org/10.22038/ijbms.2018.26994.6602 (2019).
Wang, J. W. et al. Loganin alleviates LPS-activated intestinal epithelial inflammation by regulating TLR4/NF-κB and JAK/STAT3 signaling pathways. Kaohsiung J. Med. Sci. 36, 257–264. https://doi.org/10.1002/kjm2.12160 (2020).
Zhu, Y. L. et al. Ameliorative effect of ethanolic echinacea purpurea against hyperthyroidism-induced oxidative stress via AMRK and PPAR signal pathway using transcriptomics and network Pharmacology analysis. Int. J. Mol. Sci. 24, 187. https://doi.org/10.3390/ijms24010187 (2022).
Kanehisa, M., Furumichi, M., Sato, Y., Matsuura, Y. & Ishiguro-Watanabe, M. KEGG: biological systems database as a model of the real world. Nucleic Acids Res. 53, D672–D677. https://doi.org/10.1093/nar/gkae909 (2025).
Kanehisa, M. Toward Understanding the origin and evolution of cellular organisms. Protein Sci. 28, 1947–1951. https://doi.org/10.1002/pro.3715 (2019).
Ananthakrishnan, A. N. et al. Environmental triggers in IBD: a review of progress and evidence. Nat. Rev. Gastroenterol. Hepatol. 15, 39–49. https://doi.org/10.1038/nrgastro.2017.136 (2018).
Agrawal, M., Allin, K. H., Petralia, F., Colombel, J. F. & Jess, T. Multiomics to elucidate inflammatory bowel disease risk factors and pathways. Nat. Rev. Gastroenterol. Hepatol. 19, 399–409. https://doi.org/10.1038/s41575-022-00593-y (2022).
Zhang, Y. R., Thomas, J. P., Korcsmaros, T. & Gul, L. Integrating multi-omics to unravel host-microbiome interactions in inflammatory bowel disease. Cell. Rep. Med. 5, 101738. https://doi.org/10.1016/j.xcrm.2024.101738 (2024).
Chen, J. et al. Multi-omic insight into the molecular networks of mitochondrial dysfunction in the pathogenesis of inflammatory bowel disease. E Bio Med. 99, 104934. https://doi.org/10.1016/j.ebiom.2023.104934 (2024).
Bui, T. M. et al. Tissue-specific reprogramming leads to angiogenic neutrophil specialization and tumor vascularization in colorectal cancer. J. Clin. Invest. 134, e174545. https://doi.org/10.1172/JCI174545 (2024).
O’Sullivan, S., Gilmer, J. F. & Medina, C. Matrix metalloproteinases in inflammatory bowel disease: an update. Mediat. Inflamm. https://doi.org/10.1155/2015/ (2015).
Jiang, N. et al. Alterations in metabolome and microbiome: new clues on cathelicidin-related antimicrobial peptide alleviates acute ulcerative colitis. Front. Microbiol. 15, 1306068. https://doi.org/10.3389/fmicb.2024.1306068 (2024).
Wen, Y. F. et al. Transcriptional landscape of intestinal environment in DSS-induced ulcerative colitis mouse model. BMC Gastroenterol. 24, 60. https://doi.org/10.1186/s12876-024-03128-8 (2024).
Zhu, F. T. et al. MiR-146a alleviates inflammatory bowel disease in mice through systematic regulation of multiple genetic networks. Front. Immunol. 15, 1366319. https://doi.org/10.3389/fimmu.2024.1366319 (2024).
Chen, H. J. et al. Thalidomide prevented and ameliorated pathogenesis of crohn’s disease in mice via regulation of inflammatory response and fibrosis. Front. Pharmacol. 10, 1486. https://doi.org/10.3389/fphar.2019.01486 (2019).
Steere, B. et al. Mirikizumab regulates genes involved in ulcerative colitis disease activity and anti-TNF resistance: results from a phase 2 study. Clin. Transl Gastroenterol. 14, e00578. https://doi.org/10.14309/ctg.0000000000000578 (2023).
Saez, A., Herrero-Fernandez, B., Gomez-Bris, R., Sánchez-Martinez, H. & Gonzalez-Granado, J. M. Pathophysiology of inflammatory bowel disease: innate immune system. Int. J. Mol. Sci. 24, 1526. https://doi.org/10.3390/ijms24021526 (2023).
Martin, P., Pardo-Pastor, C., Jenkins, R. G. & Rosenblatt, J. Imperfect wound healing sets the stage for chronic diseases. Science 386, eadp2974. https://doi.org/10.1126/science.adp2974 (2024).
Friedrich, M., Pohin, M. & Powrie, F. Cytokine networks in the pathophysiology of inflammatory bowel disease. Immunity 50, 992–1006. https://doi.org/10.1016/j.immuni.2019.03.017 (2019).
Rieder, F., Mukherjee, P. K., Massey, W. J., Wang, Y. & Fiocchi, C. Fibrosis in IBD: from pathogenesis to therapeutic targets. Gut 73, 854–866. https://doi.org/10.1136/gutjnl-2023-329963 (2024).
Gundersen, M. D. et al. Fibrosis mediators in the colonic mucosa of acute and healed ulcerative colitis. Clin. Transl Gastroenterol. 10, e00082. https://doi.org/10.14309/ctg.0000000000000082 (2019).
Diez-Martin, E. et al. Inflammatory bowel disease: a comprehensive analysis of molecular bases, predictive biomarkers, diagnostic methods, and therapeutic options. Int. J. Mol. Sci. 25, 7062. https://doi.org/10.3390/ijms25137062 (2024).
Okuno, T. et al. Interleukin-1beta and tumor necrosis factor-alpha induce chemokine and matrix metalloproteinase gene expression in human colonic subepithelial myofibroblasts. Scand. J. Gastroenterol. 37, 317–324. https://doi.org/10.1080/003655202317284228 (2002).
Drygiannakis, I. et al. Proinflammatory cytokines induce crosstalk between colonic epithelial cells and subepithelial myofibroblasts: implication in intestinal fibrosis. J. Crohns Colitis. 7, 286–300. https://doi.org/10.1016/j.crohns.2012.04.008 (2013).
Henderson, N. C., Rieder, F. & Wynn, T. A. Fibrosis: from mechanisms to medicines. Nature 587, 555–566. https://doi.org/10.1038/s41586-020-2938-9 (2020).
Rodansky, E. S., Johnson, L. A., Huang, S., Spence, J. R. & Higgins, P. D. Intestinal organoids: a model of intestinal fibrosis for evaluating anti-fibrotic drugs. Exp. Mol. Pathol. 98, 346–351. https://doi.org/10.1016/j.yexmp.2015.03.033 (2015).
Zhang, Y. E. Non-Smad signaling pathways of the TGF-β family. Cold Spring Harb Perspect. Biol. 9, a022129. https://doi.org/10.1101/cshperspect.a022129 (2017).
Wang, H. et al. Stabilization of snail through AKT/GSK-3β signaling pathway is required for TNF-α-induced epithelial-mesenchymal transition in prostate cancer PC3 cells. Eur. J. Pharmacol. 714, 48–55. https://doi.org/10.1016/j.ejphar (2013).
Kao, Y. H. et al. Lipopolysaccharides induce Smad2 phosphorylation through PI3K/Akt and MAPK cascades in HSC-T6 hepatic stellate cells. Life Sci. 184, 37–46. https://doi.org/10.1016/j.lfs.2017.07.004 (2017).
Wei, L. W. et al. Asiatic acid attenuates CCl4-induced liver fibrosis in rats by regulating the PI3K/AKT/mTOR and Bcl-2/Bax signaling pathways. Int. Immunopharmacol. 60, 1–8. https://doi.org/10.1016/j.intimp.2018.04.016 (2018).
Peng, R. Q. et al. Antifibrotic effects of Tanshinol in experimental hepatic fibrosis by targeting PI3K/AKT/mTOR/p70S6K1 signaling pathways. Discov Med. 23, 81–94 (2017).
Zhang, D. Q. et al. Resveratrol regulates activated hepatic stellate cells by modulating NF-κB and the PI3K/Akt signaling pathway. J. Food Sci. 81, H240–245. https://doi.org/10.1111/1750-3841.13157 (2016).
Mclarren, K. W. et al. SHIP-deficient mice develop spontaneous intestinal inflammation and arginase-dependent fibrosis. Am. J. Pathol. 179, 180–188. https://doi.org/10.1016/j.ajpath.2011.03.018 (2011).
Lo, Y., Sauve, J. P., Menzies, S. C., Steiner, T. S. & Sly, L. M. Phosphatidylinositol 3-kinase p110δ drives intestinal fibrosis in SHIP deficiency. Mucosal Immunol. 12, 1187–1200. https://doi.org/10.1038/s41385-019-0191-z (2019).
Liu, B. et al. Mast cell tryptase promotes inflammatory bowel disease-induced intestinal fibrosis. Inflamm. Bowel Dis. 27, 242–255. https://doi.org/10.1093/ibd/izaa125 (2021).
Su, S. et al. Phellodendrine promotes autophagy by regulating the ampk/mtor pathway and treats ulcerative colitis. J. Cell. Mol. Med. 25, 5707–5720. https://doi.org/10.1111/jcmm.16587 (2021).
Barron, L. & Wynn, T. A. Fibrosis is regulated by Th2 and Th17 responses and by dynamic interactions between fibroblasts and macrophages. Am. J. Physiol. Gastrointest. Liver Physiol. 300, G723–728. https://doi.org/10.1152/ajpgi.00414.2010 (2011).
Latella, G. & Viscido, A. Controversial contribution of Th17/IL-17 toward the immune response in intestinal fibrosis. Dig. Dis. Sci. 65, 1299–1306. https://doi.org/10.1007/s10620-020-06161-1 (2020).
Ma, J., Wang, F. Y. & Tang, X. D. Involvement of the NLRP3/IL-1β pathway in activation and effector functions of γδT17 cells in patients with ulcerative colitis. World J. Gastroenterol. 31, 98174. https://doi.org/10.3748/wjg.v31.i12.98174 (2025).
Koga, H., Yang, H., Adler, J., Zimmermann, E. M. & Teitelbaum, D. H. Transanal delivery of angiotensin converting enzyme inhibitor prevents colonic fibrosis in a mouse colitis model: development of a unique mode of treatment. Surgery 144, 259–268. https://doi.org/10.1016/j.surg.2008.03.043 (2008).
Cheng, Z. et al. Traditional herbal pair portulacae herba and granati Pericarpium alleviates DSS-induced colitis in mice through IL-6/STAT3/SOCS3 pathway. Phytomedicine 126, 155283. https://doi.org/10.1016/j.phymed.2023.155283 (2024).
Shang, L. R. et al. Mechanism of Sijunzi Decoction in the treatment of colorectal cancer based on network Pharmacology and experimental validation. J. Ethnopharmacol. 302, 115876. https://doi.org/10.1016/j.jep.2022.115876 (2023). Pt A.
Ji, L. et al. Identification of bioactive compounds and potential mechanisms of scutellariae radix-coptidis rhizoma in the treatment of atherosclerosis by integrating network Pharmacology and experimental validation. Biomed. Pharmacother. 165, 115210. https://doi.org/10.1016/j.biopha.2023.115210 (2023).
Zhang, Y. et al. β-arrestin 2 as an activator of cGAS-STING signaling and target of viral immune evasion. Nat. Commun. 11, 6000. https://doi.org/10.1038/s41467-020-19849-9 (2020).
Peng, K. Y. et al. Salvia miltiorrhiza stems and leaves total phenolic acids combination with Tanshinone protect against DSS-induced ulcerative colitis through inhibiting TLR4/PI3K/AKT/mTOR signaling pathway in mice. J. Ethnopharmacol. 264, 113052. https://doi.org/10.1016/j.jep.2020.113052 (2021).
Funding
This work was supported by National Natural Science Foundation of China (No. 82074441); the Scholars of Longhua Hospital Clinical Science and Technology Innovation Project Foundation of Shanghai (No. KC2022004); Shanghai Sinus and Fistula Disease Research Center (No. 2023ZZ02003).
Author information
Authors and Affiliations
Contributions
Q.Q. Conceptualization, Funding acquisition, Validation, Writing—original draft, Writing—review & editing. D. Q. Formal Analysis, Funding acquisition, Investigation, Resources, Writing—review & editing. P.Y. Software, Writing—original draft. W.C. Conceptualization, Funding acquisition, Writing—review & editing. L. J. Conceptualization, Supervision, Writing—review & editing. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This animal study was reviewed and approved by the Ethics Committee of Shanghai University of Traditional Chinese Medicine.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qin, Q., Dong, Q., Pan, Y. et al. Hongyuyin attenuates intestinal fibrosis in ulcerative colitis in mice revealed by transcriptomic and network pharmacology analyses. Sci Rep 15, 22509 (2025). https://doi.org/10.1038/s41598-025-06021-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-06021-w