Abstract
This retrospective study evaluated the comparative efficacy and safety of short-term spinal cord stimulation (st-SCS) and pulsed radiofrequency (PRF) therapy in 275 patients with thoracic herpes zoster-associated neuralgia (ZAN) treated between January 2022 and August 2024. Patients were stratified by disease duration into acute (≤ 30 days), subacute (30–90 days), and postherpetic (≥ 90 days) phases. The st-SCS group (n = 127) demonstrated superior pain relief at 3, 6, and 12 months post-treatment compared to the PRF group (n = 148), particularly in subacute and postherpetic phases (P < 0.05). While no significant intergroup difference was observed in the acute phase (P > 0.05), st-SCS showed significantly better outcomes in subsequent phases. The st-SCS group exhibited higher preoperative PQSI scores during the acute phase (P < 0.05) and improved BPI scores at 1-month follow-up (P < 0.05). Both interventions significantly reduced HADS-A and HADS-D scores at all time points (P < 0.05), with st-SCS demonstrating superior long-term improvement in depression scores (P < 0.05). These findings suggest that st-SCS provides more effective and sustained pain relief, along with greater improvements in sleep quality, emotional well-being, and quality of life compared to PRF in the management of thoracic herpes zoster-associated neuralgia.
Similar content being viewed by others
Introduction
Herpes zoster is an acute infectious disease caused by the reactivation of the varicella-zoster virus (VZV) that lies dormant in the ganglia, and it mainly occurs in the thoracic region. During the herpes outbreak and after the herpes has healed, it can cause severe neuropathic pain in the skin of the affected area, namely zoster-associated neuralgia (ZAN). Pain is the main symptom affecting the quality of life of patients and is also the most common reason for patients to seek medical treatment1,2. Three stages can be distinguished in ZAN: (1) Acute herpetic neuralgia (AHN): pain that occurs within 30 days of the rash developing; (2) Subacute herpetic neuralgia (SHN): pain that occurs between 30 and 90 days after the rash appears; (3) Clinically significant pain that lasts more than 90 days following the rash’s start is known as postherpetic neuralgia (PHN)3. At least 3% of people will get herpes zoster in their lifetime, and the risk of getting it rises with aging and immunosuppression. According to a recent systematic evaluation of 130 research from 26 countries, people with herpes zoster had a 5–30% chance of developing PHN4. Furthermore, over 30% of PHN patients suffer from persistent pain lasting beyond one year, leading to substantial impairment in quality of life and significant physical and psychological distress5. Current therapeutic approaches focus on three primary objectives: pain management during the acute phase, control of rash progression and duration, and prevention or mitigation of chronic pain conditions including PHN, along with other potential acute and chronic complications.
The management of Zoster-Associated Neuralgia (ZAN) has emerged as a significant clinical challenge, necessitating more effective therapeutic strategies. Current treatment protocols primarily focus on symptomatic relief, with pharmacotherapy serving as the cornerstone of clinical management. First-line pharmacological interventions, particularly Pregabalin and Gabapentin, demonstrate limited therapeutic efficacy despite their widespread use2,6. The persistent inadequacy of pain control, even with combined oral medication regimens, highlights the complex pathophysiology of ZAN7. In cases refractory to conventional pharmacotherapy, advanced interventional approaches are typically employed. These include nerve block techniques and neuromodulation therapies, with Pulse Radio Frequency (PRF) and Spinal Cord Stimulation (SCS) emerging as particularly promising modalities in recent years4,8,9.
PRF and SCS have demonstrated clinical efficacy in managing chronic refractory neuropathic pain. SCS encompasses two modalities: short-term SCS (st-SCS) and permanent SCS. The st-SCS approach, characterized by its minimally invasive nature and reversibility, offers enhanced safety and has been successfully implemented in treating various neuropathic pain conditions, including Zoster-Associated Neuralgia (ZAN)4,10,11. Nevertheless, the comparative safety profiles and therapeutic efficacy of these techniques for ZAN remain inconclusive, as evidenced by inconsistent findings in previous studies comparing SCS and PRF outcomes12,13,14. Given the predominant thoracic localization of ZAN manifestations, this study aims to evaluate and compare the therapeutic effectiveness of st-SCS and PRF across different disease stages of thoracic ZAN.
Methods and materials
General information
This retrospective study was registered with the Chinese Clinical Trial Registry (Registration number: ChiCTR2200064457; available at www.chictr.org.cn) and received ethical approval from the Institutional Review Board of the Affiliated Hospital of Southwest Medical University (Ethics Committee of Clinical Trials, Affiliated Hospital of Southwest Medical University, Approval number: KY2024546). Given the retrospective nature of the study, informed consent was waived by the Ethics Committee of Clinical Trials, Affiliated Hospital of Southwest Medical University. All study procedures were conducted in strict accordance with relevant guidelines and regulations. We systematically reviewed medical records of patients who underwent either st-SCS or intercostal nerve PRF treatment at our pain management department between January 2022 and August 2024. Following strict application of inclusion criteria, we conducted post-discharge follow-up assessments spanning 6 to 12 months. The study cohort comprised 275 thoracic Zoster-Associated Neuralgia (ZAN) patients, stratified into two intervention groups: the st-SCS group (n = 127) and the intercostal nerve PRF group (n = 148). Both groups received standardized pharmacological management, including Pregabalin for neuropathic pain control and Mecobalamin for neural nutrition support.
Inclusion and exclusion criteria
Inclusion Criteria:
-
1.
Confirmed diagnosis of thoracic Zoster-Associated Neuralgia (ZAN) based on established clinical criteria.
-
2.
Disease duration not exceeding 6 months from symptom onset.
-
3.
Completion of standardized pharmacological therapy combined with either intercostal nerve PRF or st-SCS at our institution.
-
4.
Availability of comprehensive clinical documentation, including treatment protocols and follow-up data.
-
5.
Ersistent severe pain (NRS score ≥ 4) despite standardized pharmacological management.
Exclusion Criteria:
Patients were excluded for the following reasons:
-
1.
Failure to meet established diagnostic criteria for ZAN.
-
2.
Comorbid chronic systemic conditions, including diabetes mellitus or severe cardiopulmonary/renal dysfunction.
-
3.
History of malignancy or autoimmune disorders.
-
4.
Coagulation abnormalities or bleeding diatheses.
-
5.
Radiological evidence of intrathecal pathology on thoracic or lumbar magnetic resonance imaging (MRI).
-
6.
Incomplete clinical documentation, including treatment records or follow-up data.
-
7.
Severe psychiatric disorders or inability to comply with treatment protocols.
-
8.
Concurrent or sequential treatment with both PRF and SCS modalities.
Treatment methods
In this study, we evaluated the effectiveness of st-SCS and intercostal nerve pulsed radiofrequency in alleviating ZAN at different stages of the disease course, aiming to prevent the progression of pain to chronic PHN. Based on the duration of the disease course, patients were categorized into the acute phase (≤ 30 days), subacute phase (30–90 days), and sequelae phase (≥ 90 days). The efficacy of the two treatment modalities in improving pain across these different phases was analyzed separately.
stSCS Group (Group A):
Short-term Spinal Cord Stimulation Group (Group A): Patients were positioned prone, and following standard disinfection and local anesthesia, an epidural puncture was performed. Under fluoroscopic guidance (C-arm), a spinal nerve stimulation electrode (TL3213, Pins Medical) was advanced into the posterior epidural space, with electrodes 3–5 positioned at the spinal level corresponding to the area of maximal pain. Postoperatively, stimulation parameters and electrode contacts were optimized to achieve paresthesia coverage of the painful area. Patients received continuous electrical stimulation therapy for 10–14 days.
PRF Group (Group B):
PRF treatment was performed under real-time ultrasound guidance with precise targeting of the affected intercostal nerves. The intervention was administered twice during hospitalization, specifically on the second and fifth days. The procedure involved ultrasound-guided percutaneous insertion of a radiofrequency thermocoagulation cannula in proximity to the target intercostal nerve. Proper needle placement was confirmed through sensory stimulation at 0.2–0.3 V (50 Hz), with successful localization evidenced by the reproduction of characteristic symptoms (pain, distension, or paresthesia) in the corresponding dermatomal distribution. PRF parameters were standardized at 70 V, 2 Hz pulse frequency, and 20 ms pulse width, delivered in two consecutive cycles: 42 °C for 6 min followed by 45 °C for 6 min.
Observation indicators and evaluation criteria
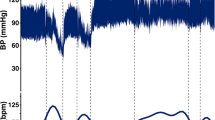
Pain assessment
Pain intensity was assessed using the Numeric Rating Scale (NRS), with scores ranging from 0 (no pain) to 10 (severe pain). Patients selected a number corresponding to their perceived pain intensity. Assessments were conducted preoperatively and at 3 days, 1 month, 3 months, 6 months, and 12 months postoperatively.
Sleep quality assessment
Sleep quality was evaluated using the Pittsburgh Sleep Quality Index (PSQI), which comprises 7 categories and 24 items, with a total score of 21. Assessments were performed preoperatively and at 1 month, 3 months, 6 months, and 12 months postoperatively. Sleep quality was categorized as follows: 0–5 (excellent), 6–10 (good), 11–15 (moderate), and 16–21 (poor). Higher scores indicate poorer sleep quality.
Quality of life assessment
The Brief Pain Inventory (BPI) was used to assess the impact of pain on daily life. The BPI evaluates seven domains: general activity, mood, walking ability, work (including housework), relationships, sleep, and enjoyment of life. Each domain is scored from 0 (no impact) to 10 (complete impact), with a total score of 70. Higher scores indicate greater pain interference with daily life. Assessments were conducted preoperatively and at 1 month, 3 months, 6 months, and 12 months postoperatively.
Negative emotion assessment
Anxiety and depression were evaluated using the Hospital Anxiety and Depression Scale (HADS), which includes two subscales: the Anxiety Subscale (HADS-A) and the Depression Subscale (HADS-D). Each subscale consists of 7 items, scored from 0 to 3, with a total score of 21. Scores were interpreted as follows: 0–7 (no significant symptoms), 8–10 (mild symptoms), 11–14 (moderate symptoms), and 15–21 (severe symptoms). Assessments were performed preoperatively and at 1 month, 3 months, 6 months, and 12 months postoperatively.
Complications
ntraoperative and postoperative complications were monitored and followed up for 6 months. Complications included pneumothorax, hematoma, local infection, peripheral nerve injury, spinal cord injury, and skin numbness.
Efficacy evaluation
Treatment efficacy was determined by the reduction in NRS scores at postoperative time points compared to baseline. Efficacy was categorized as follows: ≥75% reduction (significant effect), 50–74.9% reduction (good effect), 25–49.9% reduction (moderate effect), and < 25% reduction (no effect). Patients achieving significant or good effects were classified as having received effective treatment.
Statistical methods
Statistical analysis was performed using SPSS 26.0, and graphs were created using GraphPad Prism 9.0.0. Data were subjected to statistical description and homogeneity of variance analysis. For normally distributed measurement data, mean ± standard deviation (x ± SD) was used. Differences between groups were compared using independent samples t-tests, while within-group comparisons were performed using one-way ANOVA, with repeated comparisons conducted using the Bonferroni method. For non-normally distributed data, percentiles were used, and count data were expressed as frequencies and rates, with differences compared using the chi-square (X²) test. Rank data were compared using non-parametric rank-sum tests. A P-value < 0.05 was considered statistically significant and denoted by the symbol “*”, where “*” indicates P < 0.05, “**” indicates P < 0.01, and “***” indicates P < 0.001.
Results
Comparison of preoperative general conditions and postoperative complication rates
The preoperative general conditions, including gender, age, disease duration, affected side, NRS scores, PSQI scores, HADS scores, and BPI scores, as well as the postoperative complication rates, were compared between the two groups (Table 1). The preoperative comparison data showed no statistically significant differences in gender, affected side, VAS scores, sleep quality, quality of life, or anxiety and depression scores between the two groups, indicating comparability. There was also no statistically significant difference in the incidence of postoperative complications between the two groups. However, the average age of patients in the SCS group was significantly higher than that in the pulsed radiofrequency group (P < 0.05). Additionally, the distribution of disease duration differed between the two groups, with the majority of patients in the subacute phase and the fewest in the sequelae phase, and this difference was statistically significant (P < 0.01).
Pain assessment
The changes in NRS scores were compared between the two groups across different time periods, regardless of disease duration, as well as specifically for the acute phase, subacute phase, and sequelae phase (Fig. 1). After treatment, the NRS scores of patients in all disease courses decreased compared with those before the operation.
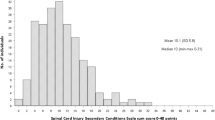
Observations on PQSI and simplified BPI scores
The PQSI and BPI scores of patients in both groups were compared across different stages of the disease course, including the acute phase, subacute phase, and sequelae phase, without distinguishing the duration of the disease (Fig. 2). After treatment, the PQSI and BPI scores of patients in all stages of the disease course showed a decrease compared to the pre-treatment scores.
PQSI and BPI at Different Periods. 2a. PQSI (unstratified), 2b. PQSI (acute phase), 2c. PQSI (subacute phase), 2d. PQSI (sequelae phase); 2e. BPI (unstratified), 2f. BPI (acute phase), 2g. BPI (subacute phase), 2h. BPI (sequelae phase). “*” indicates P < 0.05, “**” indicates P < 0.01,“***” indicates P < 0.001.
HADS score evaluation
The changes in anxiety scores (HADS-A) and depression scores (HADS-D) were compared between the two groups across different stages of the disease course, including the acute phase, subacute phase, and sequelae phase, without distinguishing the duration of the disease. After treatment, the anxiety scores (HADS-A) of patients in all stages of the disease course showed a significant decrease compared to the pre-treatment scores (Fig. 3).
HADS at Different Periods. 3a. HADS-A (unstratified), 3b. HADS-A (acute phase), 3c. HADS-A (subacute phase), 3d. HADS-A (sequelae phase); 3e. HADS-D (unstratified), 3f. HADS-D (acute phase), 3g. HADS-D (subacute phase), 3 h. HADS-D (sequelae phase).“*” indicates P < 0.05, “**” indicates P < 0.01,“***” indicates P < 0.001.
Comparison of postoperative efficacy
Postoperative efficacy was evaluated by comparing the Numerical Rating Scale (NRS) scores of patients at 3 days, 1 month, 3 months, 6 months, and 12 months post-surgery with their preoperative baseline scores. Efficacy was classified into four categories based on the percentage reduction in NRS scores: Significant effect: NRS reduction ≥ 75%, Good effect: NRS reduction between 50% and 75%, Moderate effect: NRS reduction between 25% and 50%, No effect: NRS reduction < 25%.
Postoperative 3 day efficacy comparison
The efficacy outcomes and corresponding data analyses for the two groups at 3 days postoperatively are summarized in Table 2. Prior to stratifying by disease course, no statistically significant difference in efficacy was observed between the two groups at this time point (Table 2). Similarly, for patients in both the acute and sequelae phases, no significant differences in efficacy were noted between the groups at 3 days postoperatively (Table 2). However, in the subacute phase, the electrical stimulation group demonstrated statistically superior efficacy compared to the radiofrequency group (Table 2).
Postoperative 1 month efficacy comparison
The efficacy results and data analyses for the two groups at 1 month postoperatively are detailed in Table 2. Without stratification by disease course, no statistically significant difference in efficacy was observed between the groups at this time point (Table 2). This lack of significant difference persisted across all disease phases, including the acute, subacute, and sequelae phases (Table 2).
Postoperative 3 month efficacy comparison
The efficacy outcomes and data analyses for the two groups at 3 months postoperatively are presented in Table 2. Before stratifying by disease course, a statistically significant difference in efficacy was observed, with the electrical stimulation group outperforming the radiofrequency group (Table 2). While no significant differences were noted for patients in the acute and subacute phases, those in the sequelae phase exhibited significantly better efficacy in the electrical stimulation group compared to the radiofrequency group (Table 2).
Postoperative 6 month efficacy comparison
The efficacy results and data analyses for the two groups at 6 months postoperatively are outlined in Table 2. Prior to stratifying by disease course, the electrical stimulation group demonstrated statistically superior efficacy compared to the radiofrequency group (Table 2). Although no significant difference was observed for patients in the acute phase, those in the subacute and sequelae phases showed significantly better outcomes in the electrical stimulation group (Table 2).
Postoperative 12 month efficacy comparison
The efficacy outcomes and data analyses for the two groups at 12 months postoperatively are summarized in Table 2. Without stratification by disease course, the electrical stimulation group exhibited statistically superior efficacy compared to the radiofrequency group (Table 2). While no significant difference was observed for patients in the acute phase, those in the subacute and sequelae phases demonstrated significantly better efficacy in the electrical stimulation group (Table 2).
Discussion
PHN, the most common complication of Herpes Zoster (HZ), poses significant therapeutic challenges. Despite the availability of diverse treatment options, clinical outcomes often remain suboptimal. The persistent and severe pain associated with PHN profoundly affects patients’ quality of life, daily functioning, occupational capacity, and psychological well-being. Early identification of high-risk patients and the implementation of personalized treatment strategies are crucial for effective management. Recent advancements in pain management have enabled the integration of neuromodulation techniques with conventional pharmacotherapy, particularly for medication-refractory cases. This combined approach not only enhances pain relief and improves quality of life but also reduces the required dosage of pharmacological agents, thereby minimizing potential adverse effects. Among the available neuromodulation techniques, PRF and SCS have emerged as the most widely studied and utilized modalities1,15,16.
SCS involves the epidural placement of electrodes that deliver electrical impulses to modulate pain signal transmission to the brain. It includes two main modalities: st-SCS and permanent SCS. While permanent SCS provides sustained analgesia, its clinical application is limited by high costs and a relatively high complication rate17. In contrast, st-SCS, characterized by its minimally invasive and reversible nature, demonstrates a superior safety profile, with minimal risk of severe adverse events such as cerebrospinal fluid leakage or epidural hematoma. Clinical evidence supports its efficacy in managing various neuropathic pain conditions, including ZAN4,11,18.
PRF therapy utilizes radiofrequency waves to generate an electric field, producing controlled electrical stimulation and intermittent pulsed currents at the electrode tip to modulate neural activity and alleviate pain19,20. Emerging research suggests that PRF’s field effects may mitigate both peripheral and central sensitization by influencing cytokine expression, cellular responses, and gene regulation pathways, thereby providing relief for ZAN10,21.
While both PRF and st-SCS have shown efficacy in managing ZAN, their comparative safety and therapeutic outcomes remain inadequately characterized. Further research is needed to establish optimal treatment protocols and identify patient-specific factors that may predict better outcomes with either modality.
To address regional variability and focus on the most commonly affected area, this study enrolled 275 patients with thoracic ZAN, randomized into two groups: st-SCS (n = 127) and intercostal nerve PRF (n = 148). Treatment outcomes were systematically evaluated using validated metrics, including the NRS from pre-treatment to 12 months post-treatment, the PSQI, the BPI, the HADS-A and HADS-D, and clinical efficacy measures.
Preoperative analysis indicated that both modalities had low complication rates, reflecting procedural safety and institutional expertise. Notably, the st-SCS group had a significantly higher mean age compared to the PRF group, likely due to age being a well-established risk factor for PHN development22. This is further supported by the distribution of 64 patients in the sequelae phase, with 38 (59.4%) opting for st-SCS. Significant between-group differences in disease duration were observed, likely influenced by the study’s retrospective design and sample size. These findings highlight the necessity for future multicenter randomized controlled trials to validate and extend these results.
Zoster-Associated Neuralgia (ZAN) progresses through three distinct phases: AHN, SHN, and PHN3. Our analysis of NRS score trajectories across disease stages revealed both st-SCS and PRF significantly reduced pain intensity. However, st-SCS demonstrated superior analgesic efficacy, with significantly lower NRS scores at 3 days, 3 months, 6 months, and 12 months post-intervention compared to PRF, indicating enhanced short- and long-term pain control.
Analysis of NRS scores across disease stages revealed distinct treatment response patterns. In acute-phase patients, both interventions demonstrated comparable efficacy, with no significant between-group differences in pain reduction. Subacute-phase patients receiving st-SCS achieved significantly lower pain scores at 3 days and 12 months post-treatment compared to PRF, indicating faster onset and sustained analgesia. For sequelae-phase patients, st-SCS showed superior outcomes, with significantly reduced pain scores at 3, 6, and 12 months, suggesting enhanced long-term efficacy for chronic cases.
Comparative analysis of treatment efficacy revealed distinct temporal patterns: st-SCS demonstrated superior pain reduction compared to PRF at 3, 6, and 12 months postoperatively across all disease stages. Stage-specific analysis showed no significant difference in acute-phase patients. However, st-SCS achieved significantly better outcomes in subacute-phase patients at 3 days, 6 months, and 12 months, and in sequelae-phase patients at 3, 6, and 12 months. These findings, based on both absolute NRS scores and their reduction magnitude, indicate st-SCS’s superior efficacy for subacute and chronic phases, while demonstrating equivalent effectiveness for acute-phase management.
Recent evidence supports our findings, with a 12-month study of 70 PHN patients demonstrating st-SCS’s superiority over PRF in reducing VAS scores and improving efficacy rates at 3, 6, and 12 months12. Similarly, a randomized controlled trial (n = 91) reported enhanced pain relief with st-SCS versus PRF at 1 and 6 months for AHN and SHN patients. However, conflicting results emerged from a study of 63 SHN/PHN patients showing equivalent outcomes at 24 weeks13. These discrepancies likely reflect methodological variations in sample size, follow-up duration, and our stratified analysis of distinct disease phases.
ZAN frequently induces sleep disturbances and diminished quality of life, potentially exacerbating anxiety and depression in a cyclical manner. Our analysis of PSQI, BPI, HADS-A, and HADS-D scores across disease stages revealed both interventions improved sleep quality and quality of life, with st-SCS demonstrating superior long-term benefits. Notably, acute-phase patients with higher baseline PSQI scores preferentially selected st-SCS, while PRF provided better short-term quality-of-life improvements in this subgroup. These findings suggest PRF may be preferable for acute-phase patients with less severe sleep disturbances, offering advantages of reduced hospitalization, cost-effectiveness, and lower risk. Repeat PRF sessions can maintain analgesia, providing an alternative for SCS-ineligible patients. For subacute and chronic phases, st-SCS consistently outperformed PRF in enhancing sleep quality and quality of life, corroborating previous findings16.
Analysis of HADS-A and HADS-D scores revealed both interventions significantly alleviated anxiety and depression, with st-SCS demonstrating superior long-term efficacy. Stage-specific analysis showed st-SCS provided enhanced anxiety reduction in acute-phase patients, better depression improvement in subacute-phase patients, and superior outcomes for both conditions in chronic-phase patients, consistent with previous findings4. The antidepressant effects may be mediated through spinal sensory pathways, as evidenced by transcutaneous spinal direct current stimulation’s efficacy in major depressive disorder23. While SCS primarily modulates central pain processing24, its additional anxiolytic and antidepressant effects may result from central nervous system modulation via spinal pathways. In contrast, PRF’s peripheral mechanism may limit its psychological benefits. Further clinical and preclinical studies are warranted to elucidate the neural mechanisms underlying SCS’s dual analgesic and psychotropic effects.
Current evidence supports st-SCS as a primary intervention for AHN and SHN, while early PHN (< 6 months) represents a relative indication due to its favorable safety profile. Patients with chronic PHN (> 6 months) may also benefit from st-SCS11,25. Our findings confirm st-SCS’s efficacy in SHN and PHN management, potentially preventing SHN-to-PHN progression. For AHN patients, preoperative PSQI and BPI scores may guide treatment selection, with higher scores favoring st-SCS. In subacute and chronic phases, st-SCS offers rapid, effective analgesia with additional benefits in quality of life, sleep, and mood. However, variable treatment responses suggest limitations in maintaining long-term efficacy with short-term neuromodulation, possibly reflecting the disease’s self-limiting nature. These findings highlight the potential need for combined therapeutic approaches or permanent SCS implantation to achieve sustained clinical benefits.
Limitations
This study has several limitations inherent to its retrospective design. First, potential documentation variability among physicians may introduce bias. Second, stringent inclusion/exclusion criteria limited sample size, potentially affecting results. Third, single-center recruitment from a tertiary pain clinic and 6–12 month follow-up duration constrain generalizability. Long-term st-SCS efficacy requires validation through multicenter studies with larger cohorts and extended observation periods. Despite these limitations, our findings provide preliminary evidence supporting st-SCS’s effectiveness in pain management. Future multicenter randomized controlled trials with adequate power are needed to confirm these results and optimize neuromodulation strategies for Zoster-Associated Pain.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Min, R. et al. Progress in Radiofrequency Therapy for Zoster-Associated Pain About Parameters, Modes, Targets, and Combined Therapy: A Narrative Review [J]. Pain Ther. 13(1), (2023).
Gerd, E. G. et al. S2k guidelines for the diagnosis and treatment of herpes zoster and postherpetic neuralgia [J]. J. Dtsch. Dermatol. Ges 18(1), 55–78 (2020).
Robert, W. J. et al. Herpes zoster epidemiology, management, and disease and economic burden in Europe: a multidisciplinary perspective [J]. Ther. Adv. Vaccines 3(4), 109–120 (2015).
Lei, Z. et al. Clinical study of short-term spinal cord stimulation for herpes zoster-associated pain [J]. Eur. J. Med. Res. 29(1), 603 (2024).
Kawai, K. & Gebremeskel, B. Systematic review of incidence and complications of herpes zoster: towards a global perspective [J]. BMJ Open. 4(6), e004833 (2014).
Nanna Brix, F., Rohini, K. & Troels Staehelin, J. Neuropathic Pain: From Mechanisms to Treatment [J]. Physiol. Rev. 101(1), (2020).
Yaojun, W. et al. Non-oral pharmacological interventions in the management of herpes zoster-related pain: a review of current research [J]. Front. Pain Res. (Lausanne) 5(0), 1485113 (2024).
Li, D. et al. Combined therapy of pulsed radiofrequency and nerve block in postherpetic neuralgia patients: a randomized clinical trial [J]. PeerJ 6, e4852 (2018).
Xixia, F. et al. Efficacy of Higher-Voltage Long-Duration Pulsed Radiofrequency for Spinal Zoster-Associated Pain: A Randomized Controlled Trial [J]. Pain Physician 27(10), E1073–E1083 (2024).
Dağıstan, G. Efficacy and Safety of Pulsed Radiofrequency of Dorsal Root Ganglion in Elderly Patient Population With Acute and Subacute Zoster-Related Pain. Pain research & management 6586167 (2024).
Dao-Song, D. et al. Efficacy of Short-Term Spinal Cord Stimulation in Acute/Subacute Zoster-Related Pain: A Retrospective Study [J]. Pain Physician 20(5), E633–E645 (2017).
Lei, S. et al. Short-Term Spinal Cord Stimulation or Pulsed Radiofrequency for Elderly Patients with Postherpetic Neuralgia: A Prospective Randomized Controlled Trial [J]. Neural Plast. (2022) (2022(0).).
Botao, L. et al. Clinical Study of Spinal Cord Stimulation and Pulsed Radiofrequency for Management of Herpes Zoster-Related Pain Persisting Beyond Acute Phase in Elderly Patients [J]. Pain Physician 23(3), 263 (2020).
Cheng-Fu, W. Efficacy of Pulsed Radiofrequency or Short-Term Spinal Cord Stimulation for Acute/Subacute Zoster-Related Pain: A Randomized, Double-Blinded, Controlled Trial [J]. Pain Physician 24(3), 215–222 (2021).
Junpeng, Y. et al. Risk factors for poor prognosis in patients with zoster-associated neuralgia who underwent interventional pain management [J]. Front. Mol. Neurosci. 17(0), 1393219 (2024).
Liu, L. et al. Propensity score matching comparing short-term nerve electrical stimulation to pulsed radiofrequency for herpes zoster-associated pain: A retrospective study [J]. Front. Mol. Neurosci. 15(0), 1069058 (2022).
Jiabin, H. et al. Early Treatment with Temporary Spinal Cord Stimulation Effectively Prevents Development of Postherpetic Neuralgia [J]. Pain Physician 23(2), E219 (2020).
Harsha, S. et al. Evidence-based consensus guidelines on patient selection and trial stimulation for spinal cord stimulation therapy for chronic non-cancer pain [J]. Reg. Anesth. Pain Med. 48(6), 273–287 (2023).
Yang, L. et al. Clinical outcome of Pulsed-Radiofrequency combined with transforaminal epidural steroid injection for lumbosacral radicular pain caused by distinct etiology [J]. Front. NeuroSci. 15, 683298 (2021).
Wu, C. et al. Efficacy of pulsed radiofrequency in herpetic neuralgia: A Meta-Analysis of randomized controlled trials [J]. Clin. J. Pain 36(11), 887–895 (2020).
Min, R. et al. Effect of CT-Guided Repeated Pulsed Radiofrequency on Controlling Acute/Subacute Zoster-Associated Pain: A Retrospective Cohort Study [J]. Pain Ther. 13(1), (2023).
Lu, C. et al. Interventions for zoster-associated pain: A retrospective study based on the clinical database [J]. Front. Neurol. 13(0), 1056171 (2022).
Francisco, R.-N. et al. Effect of non-invasive spinal cord stimulation in unmedicated adults with major depressive disorder: a pilot randomized controlled trial and induced current flow pattern [J]. Mol. Psychiatry, (2023).
Xuelian, L. et al. A central and peripheral dual neuromodulation strategy in pain management of zoster-associated pain [J]. Sci. Rep. 14(1), 24672 (2024).
Wuping, S. et al. Short-term spinal cord stimulation is an effective therapeutic approach for herpetic-related neuralgia-A Chinese nationwide expert consensus [J]. Front. Aging Neurosci. 14(0), 939432 (2022).
Acknowledgements
Thanks to Affiliated Hospital of Southwest Medical University for its support of this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Feng: Conceptualization, Methodology, Software. Long: Data curation, Writing- Original draft preparation. Qiu: prepared Figs. 1, 2, 3 and 4. Zhang: prepared Table 1, and 2.Ren: Writing- Reviewing. Ou: Visualization, Investigation. Fu: Supervision, Software, Validation, Writing- Reviewing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Feng, F., Long, Z., Qiu, L. et al. Comparative efficacy and safety of pulsed radiofrequency versus spinal cord stimulation in thoracic herpes zoster pain: a retrospective study. Sci Rep 15, 23280 (2025). https://doi.org/10.1038/s41598-025-06289-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-06289-y