Abstract
To investigate whether preoperative chlorhexidine mouthwash can reduce the risk of postoperative pulmonary complications(PPCs) in elderly patients with tracheal intubation under general anesthesia. 78 elderly patients undergoing elective surgery under general anesthesia and endotracheal intubation were randomly divided into the chlorhexidine group (CH group, n = 39) and the normal saline group (NS group, n = 39). Nurses instructed patients to gargle with 15 ml saline or compound chlorhexidine mouthwash the night before surgery, on the morning of surgery, and upon entering the operating room. The primary outcome was lung ultrasound score (LUS) on postoperative day 1 (D1). The secondary outcome was LUS on the preoperative day (D0) and postoperative day 3 (D3), bacterial colony count at the tip of the endotracheal tube, inflammatory markers (IL-1β, IL-6, TNF-α), and the incidence of postoperative fever, pneumonia, cough severity and sputum production. The CH group had significantly lower D1LUS compared to the NS group, whereas there was no significant difference in D3LUS between the groups. Within three postoperative days, there were no significant differences between the groups in cough severity, sputum production, fever, inflammatory markers, or pneumonia incidence. Bacterial colony counts on the endotracheal tube at extubation were lower in the CH group than in the NS group. Post hoc sensitivity analysis revealed that in patients with oral frailty, the number of colonies cultured at D1LUS, D3LUS, and the catheter tip in the CH group was lower than that in the NS group. However, there was no significant difference between the two groups in terms of the incidence of pneumonia and other aspects. Exploratory subgroup analysis showed that chlorhexidine mouthwash significantly reduced postoperative LUS in patients with oral frailty, while there were no significant differences in gender, smoking and age subgroups. Preoperative chlorhexidine mouthwash improved early postoperative LUS in elderly patients by reducing oropharyngeal bacterial colonization, particularly in those with oral weakness, though clinical outcomes like pneumonia showed no significant differences. Chinese clinical trial registration number: ChiCTR2400089898.
Similar content being viewed by others
Introduction
With the global aging population, the number of elderly patients with hip fractures continues to rise1. It is estimated that approximately 10 million hip fractures occur worldwide each year2. Due to underlying comorbidities, reduced cardiopulmonary reserve, and weakened immune function, elderly patients experience a significantly high rate of postoperative complications, reaching up to 53%3,4. PPCs, including postoperative pneumonia, atelectasis, airway secretion accumulation and respiratory insufficiency, are one of the unavoidable problems in elderly patients undergoing hip replacement5. These complications are one of the main reasons for the increased risk of death in patients with hip fracture, resulting in prolonged hospital stay, waste of medical resources, and a possible increase in postoperative mortality6.
In recent years, more studies have focused on the potential link between oral microbiota and pulmonary infections7,8. Oral pathogens spread to the lower respiratory tract, causing lung infections9. Oral health problems often occur in elderly patients, among which oral frailty is particularly prominent and is closely related to the rehabilitation effect10,11,12. These factors increase the number of pathogenic bacteria in the oral cavity and the risk of bacterial colonization, making pulmonary infections and related complications more likely. Studies have shown that preoperative mouth rinsing can reduce the number of pathogens13, and poor oral hygiene is associated with an increase in obligate anaerobic bacteria in the lungs of pneumonia patients14. Additionally, pathogenic microorganisms in the oral microbiome are linked to an increased incidence of aspiration pneumonia in hospitalized elderly patients. Furthermore, brushing teeth one week before surgery has been shown to reduce the incidence of postoperative pneumonia from 32 to 9%15. Studies also indicate that chlorhexidine mouthwash can improve oral cleanliness in intubated patients, reduce the colony count of Candida in orthodontic patients, and lower the incidence of ventilator-associated pneumonia in ICU patients16.
In summary, investigating the effect of preoperative chlorhexidine mouthwash on PPCs in elderly patients undergoing general anesthesia and endotracheal intubation is crucial to reducing the incidence of postoperative complications and improving postoperative recovery quality. This research will also provide clinical decision-making evidence for perioperative oral care and preventive interventions, thereby opening new directions for the prevention of PPCs.
Materials and methods
Ethical considerations
This study was approved by the ethics committee of the hospital and registered at the Chinese Clinical Trials.gov (ChiCTR2400089898, 19/09/2024). Elderly patients undergoing elective hip replacement surgery under general anesthesia from September 25, 2024 to December 20, 2025 are the study subjects. Written informed consent was obtained from the patients and their families. This study followed the Consolidated Standards of Reporting Trials (CONSORT) reporting guidelines. The study was performed in accordance with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Study population
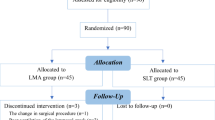
The inclusion and exclusion criteria are as follows: Inclusion criteria:① ASA I-III.② Age > 65 years.③ Undergoing hip replacement surgery with endotracheal intubation under general anesthesia. Exclusion criteria:① Preoperative respiratory infections. ② Combined with other lung diseases, tumors, etc. ③ Oral diseases (completely edentulous, history of oral surgery, oral ulcers, etc.). ④ Use of antibiotics within the past 2 weeks. ⑤ Use of chlorhexidine mouthwash within the past month. ⑥ Refusal to participate in this study. Among the initial 96 patients, 18 were excluded due to the following reasons: 10 cases with emphysema, 4 cases with a history of lobectomy, 3 cases with preoperative respiratory tract infection, and 1 case with a history of oral surgery. Ultimately, 78 patients were randomly assigned into the chlorhexidine group (CH group, n = 39) and the normal saline group (NS group, n = 39) using a random number table method(Fig. 1).
Randomization and blinding
This study employed a randomized, double-blind design. After obtaining written informed consent, eligible patients were randomly assigned in a 1:1 ratio to either CH group or NS group using a random number table method. A unique identification number was assigned to each participant, and the randomization process was carried out by an independent researcher to ensure allocation concealment. The allocation sequence was kept in sealed, opaque envelopes, and neither the patients nor the clinical researchers (nurses, anesthesiologists, and statisticians) were aware of the group assignments. The study nurses, who were not involved in patient care or data collection, provided the assigned mouthwash (either chlorhexidine or saline) to the patients and ensured that the procedure was correctly followed. The mouthwash was prepared and dispensed in identical bottles to maintain blinding.
Intervention
Routine preoperative preparation was carried out for elderly patients undergoing hip replacement surgery. First, any oral diseases or mouthwash contraindications were excluded. Patients in CH group were instructed to rinse their mouths with 15 ml of compound chlorhexidine mouthwash, while patients in NS group used 15 ml of saline solution. The nurse guided the patients to rinse their mouths the evening before the surgery, on the morning of the surgery, and after entering the operating room. The mouthwash procedure involved using 15 ml of mouthwash to rinse the mouth 8 to 10 times, followed by tilting the head back to gargle, holding the mouthwash in the throat for 15 to 20 s before spitting it out. This process was repeated three times.
Bacterial colony count at catheter tip
During extubation, tissue fluid or surface samples from the endotracheal tube tip were collected using sterile cotton swabs or sterile Bijou tubes and placed in 1 ml of sterile normal saline for homogenization. Subsequently, the diluted samples were uniformly inoculated onto nutrient agar plates using the spread plate method and incubated at 37 °C for 24 h. After incubation, colony-forming units (CFU) at the catheter tip were quantified. To ensure detection accuracy, each batch of cultures included positive and negative controls, and strict aseptic techniques were rigorously followed. Finally, statistical analysis was conducted to compare CFU counts between the CH and NS groups, thereby evaluating the effect of compound chlorhexidine gargle on the microbial flora at the catheter tip.
Oral frailty screening scale for the elderly
The Oral Frailty Screening scale for the Elderly included five dimensions: denture use, swallowing function, social participation, oral health-related behaviors and oral swallowing ability. The total score ranged from 0 to 11, with higher scores indicating worse oral condition. Oral frailty was defined as a score ≥ 417.
Lung ultrasound examination and scoring
All patients underwent lung ultrasound examinations during preoperative visits. A single experienced ultrasound physician performed the examinations using a color Doppler ultrasound diagnostic device equipped with a high-frequency linear array probe. The lung was scanned transversely and longitudinally to obtain dynamic images, using the 12-zone method: dividing the lungs into six regions per side based on the parasternal line, anterior axillary line, posterior axillary line, and the inter-nipple line, resulting in a total of 12 regions for both lungs. Lung evaluation was based on the pleural line and lung surface condition. Irregular, blurred, or even absent pleural lines were indicative of lung inflammation. The Lung Ultrasound Score (LUS) was used to assess the extent of lesions in the 12 lung regions, with a total score of 36. The scoring criteria were as follows:0 points: Normal lung aeration. 1 point: Moderate reduction in lung aeration, characterized by the presence of more than three independent B-lines or vertical coalescent lines. 2 points: Diffuse coalescent B-lines or localized areas of lung consolidation. 3 points: Complete loss of lung aeration, with or without bronchial air sign. A higher score indicated more severe pulmonary lesions5.
Outcome measures
Primary Outcome: Postoperative Day 1 Lung Ultrasound Score (D1LUS). Secondary Outcomes: Preoperative day 1 LUS (D0LUS) and postoperative day 3 LUS (D3LUS). Endotracheal Tube Bacterial Colony Count. Levels of IL-1α, IL-1β, TNF-α. The incidence of fever and pneumonia18, cough severity (I: no cough; II: occasional short cough; III: frequent cough, mildly affecting daily life; IV: severe cough, affecting daily life), and sputum production within 3 days postoperatively. Any adverse reactions associated with chlorhexidine mouthwash.
Sample size and statistical analysis
This study used PASS 15.0 to calculate the sample size. Based on preliminary experimental results, the D1LUS for the CH group was 4.8, and for the NS group, it was 7.4, with a variance of 3.1. With an α of 0.05 and a power of 0.9, 31 patients per group were required. Considering a dropout rate of 20%, 39 patients were planned for each group, totaling 78 patients. Data analyses were performed in December 2024. Because missing data for all secondary outcomes were less than 5%, no imputation was performed for missing data. All analyses were performed according to the intention-to-treat principle. Statistical analysis and graphing were performed using SPSS 26.0 and GraphPad Prism 9.0. Kolmogorov-Smirnov tests were used to assess the normality of the data distribution, and Levene’s test was used for homogeneity of variance. For normally distributed continuous variables, the mean ± standard deviation (x ± s) was used, and intergroup comparisons were performed using the independent-samples t-test. For non-normally distributed continuous variables, the median (M) and interquartile range (IQR) were used, and intergroup comparisons were performed using the Mann-Whitney U test. Categorical data were expressed as proportions and compared using the chi-square test or Fisher’s exact probability method. Ordinal data were compared using the rank sum test. The generalized estimating equation (GEE) was used to compare D1LUS and D3LUS between the two groups, with D0LUS as a covariate. A post hoc sensitivity analysis was conducted based on the presence or absence of oral frailty to evaluate the potential beneficial effects of the intervention in patients with oral frailty. Post hoc subgroup analyses of the primary outcome measures were conducted based on gender, smoking, oral frailty and age(≥ 70). P < 0.05 was considered statistically significant.
Results
Patient demographics in the two groups
A total of 78 patients were included in this study, with an average age of 69.2 ± 3.7 years and an average BMI of 21.9 ± 3.0 kg/m². The distribution of ASA classifications was as follows: ASA I, 19 cases (24.4%); ASA II, 38 cases (48.7%); and ASA III, 21 cases (26.9%). Comorbidities included 22 cases of diabetes mellitus (28.2%) and 23 cases of hypertension (29.5%). Ten patients (12.8%) had a history of cardiovascular or cerebrovascular diseases, and 23 participants (29.5%) were current smokers. The overall oral frailty score was 3.3 ± 1.9, with 31 patients (39.7%) identified as having oral frailty. There were no statistically significant differences between the two groups in terms of age, sex, BMI, ASA classification, oral frailty score, presence of oral frailty, or intubation duration (all P > 0.05, Table 1).
The LUS and complications were compared between the two groups
Analysis using the GEE revealed that the LUS on D0, D1, and D3 showed a statistically significant reduction in the LUS on D1 in the CH group compared to the NS group (P = 0.001). However, no significant differences were observed between the two groups on D3 (P > 0.05, Fig. 2). Additionally, there were no statistically significant differences between the two groups in terms of cough severity, sputum production, fever, or the incidence of pneumonia within 3 days postoperatively (all P > 0.05). Furthermore, bacterial colony counts on the tip of the endotracheal tube upon extubation were significantly lower in the CH group compared to the NS group (P = 0.007). Details are presented in Table 2; Fig. 3.
The inflammatory factors were compared between the two groups
To further investigate whether chlorhexidine mouthwash affects the systemic inflammatory response, plasma levels of IL-1β, IL-6, and TNF-α were measured on D0, D1, and D3. The results showed no significant differences in plasma IL-1β, IL-6, or TNF-α levels between the two groups on D1 and D3 (P > 0.05). Details are presented in Fig. 4.
Subgroup analysis
Post hoc sensitivity analysis was conducted to evaluate the presence of oral frailty among elderly patients, identifying 31 individuals with oral frailty (12 in the NS group and 19 in the CH group). Among elderly patients without oral frailty (n = 47), the LUS on D0, D1, and D3 were 2.8 ± 1.3, 4.7 ± 2.4, and 2.8 ± 1.8 in the NS group, respectively, compared to 2.4 ± 1.5, 4.0 ± 1.2, and 3.0 ± 1.2 in the CH group, respectively. There were no statistically significant differences in LUS between the two groups on D0, D1, and D3 (all P > 0.05). Additionally, the bacterial colony counts at the catheter tip were 4 (2,5) CFU/ml in the NS group and 3 (0,4) CFU/ml in the CH group, with no significant difference observed (P = 0.097). In elderly patients with oral frailty (n = 31), the NS group exhibited LUS scores of 2.0 ± 1.0 on D0, 11.1 ± 2.8 on D1, and 3.8 ± 2.9 on D3, whereas the CH group showed LUS scores of 2.7 ± 1.5 on D0, 5.8 ± 2.7 on D1, and 2.0 ± 1.8 on D3. Significant differences in LUS were observed between the CH and NS groups on D1 (P < 0.001) and D3 (P = 0.035), with the CH group demonstrating significantly lower LUS scores compared to the NS group (Fig. 5). Furthermore, the bacterial colony counts at the catheter tip were significantly lower in the CH group (2 (0,3.5) CFU/ml) compared to the NS group (4 (2,8.25) CFU/ml; P = 0.043). Regardless of oral frailty status, there were no significant differences between the NS and CH groups in the incidence of pneumonia, fever, cough severity, or sputum production (all P > 0.05, Table 3). Post hoc subgroup analysis based on gender, smoking, oral frailty and age revealed that in the oral frailty subgroup, chlorhexidine mouthwash significantly reduced postoperative LUS(-5.29, 95%CI, -7.25 ~ -3.34, P < 0.001), while there were no significant differences in gender, smoking and age (Fig. 6).
Changes in LUS over time in patients with and without oral frailty. (A) Line chart showing changes in LUS on D0, D1, and D3 for NS and CH groups in patients with oral frailty. (B) Line chart showing changes in LUS on D0, D1, and D3 for NS and CH groups in patients without oral frailty. (C) Bar chart showing changes in LUS on D0, D1, and D3 for NS and CH groups in patients with oral frailty. (D) Bar chart showing changes in LUS on D0, D1, and D3 for NS and CH groups in patients without oral frailty. Compared to the NS group, *P < 0.05; ***P < 0.001.
Forest plot of the subgroup analysis for the primary outcome. A post hoc subgroup analysis was performed based on gender, smoking status, oral frailty, and age. To evaluate the effect of the intervention within each specific subgroup, the results were presented separately as relative risks (RRs) with 95% confidence intervals (CIs). The interaction term is a test of whether the effect of the experimental intervention is statistically different in significance between subgroups.
Discussion
This study is a randomized controlled clinical trial that included 78 elderly patients. The primary results showed that the CH group had significantly lower D1LUS compared to the NS group, and the bacterial colony count at the tip of the endotracheal tube was also significantly lower at extubation. This indicates that the antibacterial effect of chlorhexidine plays a role in reducing oropharyngeal colonization and the risk of pulmonary complications. Notably, Exploratory subgroup analysis revealed that these benefits were particularly pronounced in patients with oral frailty, with significantly lower D1LUS and D3LUS scores in the CH group. However, regardless of oral frailty status, no significant differences were found between the CH and NS groups in terms of cough severity, sputum production, fever, or pneumonia incidence within the first three days post-surgery. No chlorhexidine related adverse events were observed in this study.
The results of this study align with existing literature and further support the crucial role of oral hygiene in reducing PPCs15,19. Previous studies have shown that preoperative oral care can significantly reduce the incidence of postoperative pneumonia. For instance, performing oral care for 5 days prior to surgery reduced the incidence of postoperative pneumonia in esophageal cancer patients from 32–9%15. Additionally, chlorhexidine mouthwash has been shown to reduce the incidence of ventilator-associated pneumonia (VAP) in intensive care units by decreasing oropharyngeal bacterial colonization16. Our findings validate these observations, showing a significant reduction in bacterial colony count at the tip of the endotracheal tube in the CH group, suggesting that chlorhexidine’s antimicrobial effect plays a role in reducing pulmonary infection sources. This antimicrobial effect was especially pronounced in patients with oral frailty, with significantly lower D1LUS and D3LUS in the CH group. Furthermore, in patients with oral frailty, the bacterial colony count at the tip of the endotracheal tube was also significantly lower in the CH group, which may be attributed to the poorer oral health status of these patients, making them more prone to bacterial colonization. Thus, chlorhexidine’s antimicrobial efficacy is more apparent in these patients20.
Although this study demonstrated a clear advantage of the CH group in early postoperative pulmonary recovery, no significant difference in LUS between the two groups was observed on D3.This might be due to the fact that the initial effect of chlorhexidine weakens over time or as the lung disease naturally recovers. In addition, the routine postoperative nursing intervention may have weakened the sustained effect of chlorhexidine. Furthermore, the small sample size of the study might have reduced the statistical power on the third day. This might suggest that short-term chlorhexidine mouthwash before surgery may be more suitable for short-term reduction of the risk of oral infection, while long-term prevention requires a combination of multimodal oral care strategies (such as continuous oral care after surgery, etc.). Furthermore, there were no significant differences between the two groups in the incidence of postoperative adverse reactions such as pneumonia, fever, cough severity, or pneumonia incidence, and neither group experienced severe pulmonary complications such as atelectasis or pleural effusion. We speculate that this result may be related to the exclusion of patients with preoperative high-risk pulmonary infections12, which may have led to a false negative result. On the other hand, this may also be attributed to the relatively small sample size of the present study. Future research with a larger sample size is warranted to validate these findings.
Exploratory subgroup analysis further highlighted that the improvement was more pronounced in the oral frailty patient group, suggesting that elderly patients with oral frailty may benefit more from oral hygiene interventions. Considering that elderly patients often have reduced immunity and slower pulmonary recovery. Poor oral health may be a marker of the onset of frailty21. A study of community-dwelling older adults showed that accumulated poor oral health strongly predicted the occurrence of adverse health outcomes22,23. Therefore, improving oral function and reducing the impact of oral frailty may improve nutritional and functional status in the elderly and may be associated with a reduction in pulmonary complications and other adverse health outcomes24. However, given the small sample size of this subgroup, these findings should be interpreted as hypothesis-generating rather than confirmatory. Additionally, no significant differences were observed in systemic inflammatory markers (IL-1β, IL-6, TNF-α) between the CH and NS groups, indicating that while chlorhexidine effectively reduced local bacterial colonization, it may not significantly influence broader systemic inflammatory responses in the short term. Future large-scale randomized trials are needed to validate these exploratory findings and elucidate the mechanisms underlying oral frailty-specific responses to perioperative oral care.
This study underscores the potential benefits of incorporating chlorhexidine mouthwash into the preoperative care plan for elderly patients, particularly those with oral frailty. As a simple, cost-effective, and non-invasive intervention, chlorhexidine can effectively reduce oropharyngeal bacterial colonization, thereby decreasing the risk of early pulmonary inflammation and complications. This intervention is especially important for elderly patients with weakened immune systems and poor pulmonary recovery. The method does not rely on complex equipment or costly medications, making it a feasible addition to standard preoperative care in resource-limited clinical settings. However, despite positive results in reducing LUS scores and bacterial counts, the clinical impact of chlorhexidine on the prevention of pulmonary complications, such as pneumonia, remains to be further explored25.
Chlorhexidine mouthwash, due to its low cost and wide availability, represents a highly cost-effective oral care measure. Compared to other pharmacological interventions aimed at preventing PPCs, chlorhexidine mouthwash does not require additional medical resources and is easy to implement in routine preoperative care. This economic advantage is particularly crucial in settings with limited medical resources or when patients face financial constraints26,27,28.
There are some limitations to this study. Firstly, the sample size was small. Post hoc power analysis showed a power of 64.8%, but the primary endpoint still indicated a statistically significant difference. Larger-scale studies are needed in the future to confirm these findings with higher statistical power. In addition, the proportion of elderly patients with oral frailty is relatively low, which may affect the statistical power of subgroup analysis. Additionally, this study excluded patients with preoperative respiratory infections, which may have led to the loss of high-risk patient data, potentially resulting in false negatives. Future research could consider including more high-risk patients, such as those from community elderly populations, to assess the effects of oral hygiene interventions in different risk groups. Another limitation is the short postoperative follow-up period of only 3 days, which may overlook the long-term lung prognosis and complications. Therefore, future studies should extend the follow-up period to evaluate the long-term effect, or further extend the intervention time and assess the impact of oral hygiene intervention on hospital stay and recovery time etc. Moreover, this study did not comprehensively account for all potential confounders, such as patient mobility and postoperative rehabilitation adherence, which may influence PPCs. Future studies should aim to design more comprehensive protocols to control for additional confounding variables and improve the accuracy and generalizability of the findings.
Future research should focus on standardizing preoperative oral care protocols, including the optimal timing and frequency of chlorhexidine mouthwash use. Additionally, studies comparing the effectiveness of different antimicrobial mouthwashes could help identify the best oral care regimen. Another important avenue for research is to explore the synergistic effects of oral hygiene interventions with other measures to prevent PPCs, such as respiratory rehabilitation and nutritional support, to further reduce the incidence of postoperative pulmonary complications.
Conclusions
This study indicates that the use of preoperative chlorhexidine mouthwash positively influences postoperative pulmonary recovery in elderly patients, particularly those exhibiting oral frailty. Consequently, implementing perioperative oral care may be regarded as a viable strategy to mitigate the potential risks associated with postoperative pulmonary complications and enhance overall recovery outcomes in this demographic.
Data availability
The data are contained within the article, please contact the corresponding author.
References
Gadgaard, N. R. et al. Comorbidity and risk of infection among patients with hip fracture: a Danish population-based cohort study. Osteoporos. Int. 34, 1739–1749. https://doi.org/10.1007/s00198-023-06823-6 (2023).
Sing, C. W. et al. Global epidemiology of hip fractures: secular trends in incidence rate, Post-Fracture treatment, and All-Cause mortality. J. Bone Min. Res. 38, 1064–1075. https://doi.org/10.1002/jbmr.4821 (2023).
Fleisher, L. A. Improving perioperative outcomes: my journey into risk, patient preferences, guidelines, and performance measures: ninth honorary FAER research lecture. Anesthesiology 112, 794–801. https://doi.org/10.1097/ALN.0b013e3181d41988 (2010).
Kain, Z. N., Fitch, J. C., Kirsch, J. R., Mets, B. & Pearl, R. G. Future of anesthesiology is perioperative medicine: a call for action. Anesthesiology 122, 1192–1195. https://doi.org/10.1097/ALN.0000000000000680 (2015).
Vetrugno, L. et al. Active ageing interdisciplinary, accuracy of preoperative lung ultrasound score for the prediction of major adverse cardiac events in elderly patients undergoing HIP surgery under spinal anesthesia: the LUSHIP multicenter observational prospective study. Anaesth. Crit. Care Pain Med. 43, 101432. https://doi.org/10.1016/j.accpm.2024.101432 (2024).
Chen, X. et al. Risk factors for postoperative mortality at 30 days in elderly Chinese patients with hip fractures. Osteoporos. Int. 33, 1109–1116. https://doi.org/10.1007/s00198-021-06257-y (2022).
He, J. et al. Association between oral Microbiome and five types of respiratory infections: a two-sample Mendelian randomization study in East Asian population. Front. Microbiol. 15, 1392473. https://doi.org/10.3389/fmicb.2024.1392473 (2024).
Dong, J. et al. Relationships between oral microecosystem and respiratory diseases. Front. Mol. Biosci. 8, 718222. https://doi.org/10.3389/fmolb.2021.718222 (2021).
Gregorczyk-Maga, I. et al. Correction: Impact of tooth brushing on oral bacteriota and health care-associated infections among ventilated COVID-19 patients: an intervention study. Antimicrob. Resist. Infect. Control. 12, 51. https://doi.org/10.1186/s13756-023-01256-6 (2023).
Nagatani, M. et al. Oral frailty as a risk factor for mild cognitive impairment in community-dwelling older adults: Kashiwa study. Exp. Gerontol. 172, 112075. https://doi.org/10.1016/j.exger.2022.112075 (2023).
Patel, R. et al. Refocusing dental care: A risk-based preventative oral health programme for dentate older people in UK care homes. Gerodontology 39, 131–138. https://doi.org/10.1111/ger.12543 (2022).
Molina, A., Huck, O., Herrera, D. & Montero, E. The association between respiratory diseases and periodontitis: A systematic review and meta-analysis. J. Clin. Periodontol. 50, 842–887. https://doi.org/10.1111/jcpe.13767 (2023).
Yaghmoor, W. et al. Effect of preoperative chlorhexidine, essential oil, and cetylpyridinium chloride mouthwashes on bacterial contamination during dental implant surgery: A randomized controlled clinical trial. Saudi Dent. J. 36, 492–497. https://doi.org/10.1016/j.sdentj.2023.12.011 (2024).
Hata, R. et al. Poor oral hygiene is associated with the detection of obligate anaerobes in pneumonia. J. Periodontol. 91, 65–73. https://doi.org/10.1002/JPER.19-0043 (2020).
Akutsu, Y. et al. Pre-operative dental brushing can reduce the risk of postoperative pneumonia in esophageal cancer patients. Surgery 147, 497–502. https://doi.org/10.1016/j.surg.2009.10.048 (2010).
Klompas, M., Speck, K., Howell, M. D., Greene, L. R. & Berenholtz, S. M. Reappraisal of routine oral care with chlorhexidine gluconate for patients receiving mechanical ventilation: systematic review and meta-analysis. JAMA Intern. Med. 174, 751–761. https://doi.org/10.1001/jamainternmed.2014.359 (2014).
Tanaka, T., Hirano, H., Ohara, Y., Nishimoto, M. & Iijima, K. Oral frailty Index-8 in the risk assessment of new-onset oral frailty and functional disability among community-dwelling older adults. Arch. Gerontol. Geriatr. 94, 104340. https://doi.org/10.1016/j.archger.2021.104340 (2021).
G.o.K.S.i.P.a.C.o.t.F.C.o.H.I.C.B.o.C.P.M. Association. Expert consensus on prevention and control of postoperative pneumonia. Chin. J. Clin. Infect. Dis. 11, 11–19. https://doi.org/10.3760/cma.j.issn.1674-2397.2018.01.003 (2018).
Bergan, E. H., Tura, B. R. & Lamas, C. C. Impact of improvement in preoperative oral health on nosocomial pneumonia in a group of cardiac surgery patients: a single arm prospective intervention study. Intensive Care Med. 40, 23–31. https://doi.org/10.1007/s00134-013-3049-y (2014).
Khadka, S. et al. Poor oral hygiene, oral microorganisms and aspiration pneumonia risk in older people in residential aged care: a systematic review. Age Ageing. 50, 81–87. https://doi.org/10.1093/ageing/afaa102 (2021).
de Sire, A. et al. Sarcopenic dysphagia, malnutrition, and oral frailty in elderly: A comprehensive review. Nutrients 14. https://doi.org/10.3390/nu14050982 (2022).
Tanaka, T. et al. Oral frailty as a risk factor for physical frailty and mortality in Community-Dwelling elderly. J. Gerontol. Biol. Sci. Med. Sci. 73, 1661–1667. https://doi.org/10.1093/gerona/glx225 (2018).
Dibello, V. et al. Oral frailty indicators to target major adverse health-related outcomes in older age: a systematic review. Geroscience 45, 663–706. https://doi.org/10.1007/s11357-022-00663-8 (2023).
Dibello, V. et al. Oral frailty and its determinants in older age: a systematic review. Lancet Healthy Longev. 2, e507–e520. https://doi.org/10.1016/S2666-7568(21)00143-4 (2021).
Iwata, E. et al. Effects of perioperative oral care on prevention of postoperative pneumonia after lung resection: multicenter retrospective study with propensity score matching analysis. Surgery 165, 1003–1007. https://doi.org/10.1016/j.surg.2018.11.020 (2019).
Tan, C., Tang, C. Z., Chen, X. S. & Luo, Y. J. Association between medical resources and the proportion of oldest-old in the Chinese population. Mil Med. Res. 8, 14. https://doi.org/10.1186/s40779-021-00307-6 (2021).
Qiao, Z., Ding, Y., Zhu, Y. & Qin, S. The matching relationship and driving mechanism of elderly medical care resources and elderly population in China: A study based on provincial perspective. Medicine 103. https://doi.org/10.1097/MD.0000000000040882 (2024).
Kanchanachitra, C. et al. J.F. Dela rosa, human resources for health in Southeast asia: shortages, distributional challenges, and international trade in health services. Lancet 377, 769–781. https://doi.org/10.1016/S0140-6736(10)62035-1 (2011).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
My.W: Formal Analysis, Software, Validation, Visualization. Fy.M: Formal Analysis, Methodology, Software, Validation, Visualization. P.P: Data curation, Investigation. Ch.G: Methodology, Writing – review & editing. T.L: Writing – original draft, Writing – review & editing. L.L: Conceptualization, Project administration, Resources, Supervision. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, M., Ma, F., Peng, P. et al. Preoperative chlorhexidine mouthwash can reduce the risk of postoperative pulmonary complications in elderly patients undergoing general anesthesia with endotracheal intubation. Sci Rep 15, 22932 (2025). https://doi.org/10.1038/s41598-025-06417-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06417-8