Abstract
To analyze the predictive value of serum Golgi protein 73 (GP73) and IL-6 for 90-day prognosis in patients with hepatitis B virus-related acute-on-chronic liver failure (HBV-ACLF). A total of 289 patients with hepatitis B virus infection who attended the Infection Department of the 910th Hospital of the PLA Logistics Support Force from February 2022 to April 2024 were included in this study. A total of 149 patients with HBV-ACLF were followed up for 3 months after diagnosis, and their outcomes were recorded and assessed. Serum GP73 and IL-6 levels were determined via an enzyme-linked immunosorbent assay and an automatic electrochemical luminescence immunity analyzer, respectively. Multivariate Cox regression, piecewise linear regression analysis, threshold effect and receiver operating characteristic curves were used to evaluate the predictive value of serum Golgi protein 73 (GP73) and IL-6 for 90-day prognosis in patients with HBV-ACLF. Our results revealed that the serum GP73 and IL-6 levels in patients with HBV-ACLF were significantly higher than in chronic hepatitis B group (all P values < 0.001). The serum levels of GP73 and IL-6 in patients with HBV-ACLF who survived after 90 days were lower than those in the nonsurvival group (all P values < 0.001). In addition, the highest serum levels of GP73 and IL-6 were associated with a greater risk of death in HBV-ACLF patients after adjusting for potential confounders (P = 0.0094, 0.0377). Additionally, a nonlinear relationship was observed between GP73 and the risk of 90-day mortality, with an inflection point at 298.99 ng/mL (P = 0.003). A positive linear correlation between IL-6 and the risk of 90-day death was observed in patients with serum IL-6 levels less than 98.78 pg/mL (P = 0.0368). Furthermore, the accuracy of classical prognostic scores, including the model for end-stage liver disease (MELD) score and model for end-stage liver disease-sodium (MELD-Na) score, was significantly improved after combining GP73 and IL-6 in predicting the 90-day prognosis of patients with HBV-ACLF. Serum GP73 and IL-6 levels were significant predictors of short-term prognosis in patients with HBV-ACLF. The combination of GP73 and IL-6 significantly improved the predictive value of classical prognostic scores.
Similar content being viewed by others
Introduction
Acute-on-chronic liver failure (ACLF) is a clinical syndrome characterized by rapid deterioration of liver function due to cirrhosis or chronic liver disease. It may eventually develop into multiple organ failure, with a short-term mortality rate ranging from 30 to 90%1. This remains one of the most formidable challenges to overcome in the field of liver disease. Accurately assessing the severity and prognosis of patients with ACLF is critical for enhancing their chances of survival.
Several classical prognostic models, such as the Child‒Turcotte‒Pugh (CTP) score, model for end-stage liver disease (MELD) score and model for end-stage liver disease-sodium (MELD-Na) score2,3,4,5, have been used for assessing the condition and prognosis of liver failure. However, owing to several types of ACLF, with HBV infection being the major form of ACLF in Asians and alcohol or hepatitis C virus infection being the major form of ACLF in Europe6,7, the sensitivity and specificity of these classical prognostic models for ACLF are suboptimal.
Persistent excessive inflammatory responses in the early stages of ACLF play a critical role in the pathogenesis and outcome of ACLF. Golgi membrane protein 73 (GP73), is a novel Golgi type II membrane protein with unknown function discovered in 20008. GP73 is hardly expressed in normal liver tissues, but it is expressed in almost all liver cells in liver diseases caused by various reasons9. Owing to its high expression in hepatocellular carcinoma patients, it was considered a potential hepatocellular carcinoma biomarker in initial studies10,11,12. However, the expression of GP73 is more closely associated with advanced liver inflammation in patients with HBV infection compared with hepatocellular carcinoma in recent studies13,14. Several studies have reported that GP73 may serve as an independent risk factor for short-term prognosis in patients with not only alcohol-associated ACLF but also HBV-related ACLF15,16,17. It is evident that serum GP73 levels are higher in ACLF patients than in healthy people15,16,17. However, further research is necessary to confirm the role of GP73 in patients with HBV-ACLF. Moreover, inflammatory factors, which are overexpressed during excessive inflammatory responses in ACLF and contribute significantly to the progression of liver failure, should also be noted. Interleukin 6 (IL-6), a key proinflammatory cytokine, is associated with the severity of hepatic inflammation. In our previous study, we reported a gradual increase in serum IL-6 levels along with liver disease progression in patients with chronic HBV infection18. Several studies have reported that it is an independent predictor of short-term prognosis in patients with ACLF19,20. However, the specificity of the prognostic value is limited21,22.
To date, information regarding GP73 and IL-6 in patients with HBV-ACLF is limited. The prognostic value of GP73 and IL-6 for HBV-ACLF patients remains to be further clarified in the literature. In this study, we individually assessed the associations between serum GP73 and IL-6 levels and the risk of mortality at 90 days in patients with HBV-ACLF. Moreover, the prognostic value of the combination of GP73 and IL-6 was also explored.
Results
Serum GP73 and IL-6 levels between patients with chronic hepatitis B and HBV-ACLF
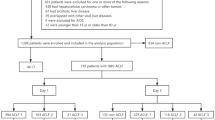
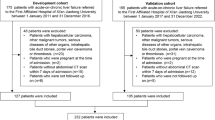
A total of 140 patients with chronic hepatitis B (CHB) and 149 patients with HBV-ACLF were included in the study. The serum levels of GP73 and IL-6 in the HBV-ACLF group were significantly higher than in chronic hepatitis B group (all P values < 0.001) (Fig. 1). Meanwhile, there were significant differences in age, serum levels of ALT and AST between the two groups (all P values < 0.001) (Table 1).
Baseline characteristics of patients with HBV-ACLF
Table 2 summarizes the demographic and clinical characteristics of 149 patients with HBV-ACLF, classified according to 90-day mortality. Patients who survived were younger than those who died (P = 0.009). The serum GP73 and IL-6 levels in the survival group were lower than those in the nonsurvival group (P < 0.001). In addition, several parameters, including laboratory test indicators (ALT, AST, TBil, Cr, Na and the international normalized ratio [INR]), incidence of complications (ascites, hepatic encephalopathy and pulmonary infection), and scores (MELD and MELD-Na), differed significantly between the two groups (P < 0.05) (Table 2).
Associations between the serum levels of GP73 or IL-6 and 90-day mortality in patients with HBV-ACLF
The cumulative survival rates during the 90-day follow-up period were analyzed via Kaplan‒Meier curves based on the serum GP73 and IL-6 tertiles. The cumulative survival rates of each group were 88.0% (T1), 57.1% (T2), and 38.0% (T3) in the GP73 cohort and 80.0% (T1), 65.3% (T2), and 38.0% (T3) in the IL-6 cohort. Figure 2 shows that the cumulative survival rate was the lowest in patients within the highest tertiles of GP73 (T3) and IL-6 (T3) (Fig. 2).
K‒M curves showing the short-term probability of 90-day survival among patients with HBV-ACLF stratified into tertiles according to the serum GP73 (A) or IL-6 (B) levels. *Versus the serum levels of GP73 or IL-6 in the T1 group as a control. #Versus the serum levels of GP73 or IL-6 in the T2 group as a control.
The associations among GP73, IL-6 and 90-day mortality were evaluated by a univariate linear regression model. As continuous variables, the serum levels of GP73 and IL-6 were positively correlated with mortality at 90 days in the unadjusted model (Model 1) (HR 1.01 [1.00–1.01], P < 0.001; HR 1.01 [1.00, 1.01], P = 0.001). The same trends are observed in Model 2 and Model 3 (Table 3). Moreover, the serum levels of GP73 and IL-6 were handled as categorical variables (Tertiles), but the same trend was observed in the GP73 tertile cohort only (P values for trends were < 0.0001, 0.0033, and 0.0235 in Models 1, 2, and 3, respectively). We did not detect a connection in Model 3 in the IL-6 tertile cohort (P for trend was 0.0780).
Analysis of the dose‒response relationship and threshold effect
The dose–response relationships between serum GP73 and IL-6 levels and the risk of 90-day mortality in patients with HBV-ACLF were analyzed by smoothing function analysis (Fig. 3). As shown in Fig. 3A–C, the relationship between GP73 and the risk of 90-day mortality was nonlinear both in the adjusted and unadjusted models. To further explore the dose–response relationship, likelihood ratio test was used to compare the goodness of fit of two models (one-line liner regression model or two-piecewise liner regression model) in Table 4. Moreover, the inflection point at 298.99 ng/mL was determined via a two-piecewise linear regression model (Table 4). On the left of the inflection point, the hazard ratio (HR) was 1.02 (95% CI 1.01–1.03) (P = 0.0013). There was a significant positive linear regression relationship between GP73 and the risk of 90-day mortality after adjusting potential confounders among patients with serum levels of GP73 less than 298.99 ng/mL. However, when serum levels of GP73 more than 298.99 ng/mL, the linear regression correlation was no significant (P = 0.2190) (Table 4). The two-piecewise linear regression model had more goodness of fit than the one-line linear regression model in the dose–response relationship between the serum levels of GP73 and the risk of 90-day mortality, as determined by the log-likelihood ratio test (P = 0.003) (Table 4).
The risk of mortality at 90 days was associated with the serum levels of GP73 (A–C) and IL-6 (D–F). The red line indicates the estimated mortality risk, and the blue lines represent the pointwise 95% CI. (A) and (D) were not adjusted. (B) and (E) were adjusted for age, ALT, AST, TBil, Cr, INR and Na. (C) and (F) were adjusted for age; ALT, AST, TBil, Cr, INR, and Na; and presence of complications (ascites, HE, and PI).
Figure 3D–Fshows the dose–response relationship between the IL-6 concentration and the risk of 90-day mortality. A positive linear correlation between them was observed both in unadjusted model or model adjusted only for age, ALT, AST, TBil, INR and Na (Fig. 3D,E). The inflection point at 98.78 pg/mL was calculated via a two-piecewise linear regression model (Table 4). On the right of the inflection point, the risk of 90-day mortality decreased when the presence of complications was added to the potential confounders (Fig. 3F). Meanwhile, this segment did not reach statistical significance (P = 0.1676) (Table 4). On the left of the inflection point, there was a significant positive linear regression relationship between them (P = 0.0368). The log likelihood ratio test showed that the one-line linear regression model had more goodness of fit than the two-piecewise linear regression model in the dose–response relationship between the serum levels of IL-6 and the risk of 90-day mortality, as P value was 0.086 (Table 4). However, the statistical test showed that the one-line linear regression relationship was not significant (P = 0.2732) when the presence of complications was added to the potential confounders (Table 4).
Analysis of the prognostic value of GP73 combined with IL-6 for 90-day mortality in patients with HBV-ACLF
GP73 and IL-6 were compared with the MELD and MELD-Na scores, which are classical prognostic scores (Fig. 4). As single indices, the prognostic value of GP73 and IL-6 was comparable to that of classical prognostic scores (GP73 vs. MELD yielded 0.769 vs. 0.778 [P = 0.880], GP73 vs. MELD-Na yielded 0.769 vs. 0.771 [P = 0.977]; IL-6 vs. MELD yielded 0.715 vs. 0.778 [P = 0.220], and IL-6 vs. MELD-Na yielded 0.715 vs. 0.771 [P = 0.287]). Moreover, after combining GP73, the predictive value of the MELD and MELD-Na scores improved significantly (GP73 + MELD vs. MELD yielded 0.861 vs. 0.778 [P = 0.006], and GP73 + MELD-Na vs. MELD-Na yielded 0.864 vs. 0.771 [P = 0.002]). Most notably, after combining GP73 and IL-6, the predictive efficacy of the MELD score was significantly better than that of the MELD and MELD-Na scores (GP73 + IL-6 + MELD vs. MELD yielded 0.875 vs. 0.778 [P = 0.002], and GP73 + IL-6 + MELD vs. MELD-Na yielded 0.875 vs. 0.771 [P = 0.008]) (Table 5).
Discussion
HBV-associated acute-on-chronic liver failure (ACLF) is the major form of ACLF in China. The accuracy of classical prognostic models in predicting the mortality risk of patients with HBV-ACLF is lacking. This study explored the predictive value of GP73 and IL-6 for 90-day prognosis in patients with HBV-ACLF from multiple perspectives.
This study found that the serum levels of GP73 and IL-6 were greater in patients with HBV-ACLF than in those with chronic hepatitis B, especially in the death group at 90 days among patients with HBV-ACLF. High levels of serum GP73 and IL-6 indicate severe liver disease and increased mortality risk in patients with HBV-ACLF. A positive correlation between serum GP73 levels and 90-day mortality in patients with HBV-ACLF was confirmed, whether as a continuous variable or categorized into three tertiles, via both adjusted and unadjusted models. Threshold effect analysis revelated that the risk of 90-day mortality among HBV-ACLF patients exhibited a progressive dose–response escalation with increasing serum levels of GP73. Beyond the inflection point at 298.99 ng/mL, the linear correlation dissipated, whereas the mortality rate within this hyper-risk cohort remained persistently high (Among the 59 cases with serum levels of GP73 exceeding 298.99 ng/mL, 36 mortality events were documented, yielding a crude mortality rate of 61.02%). GP73 as a high-risk factor for short term in patients with HBV-related ACLF should be paid more attention in clinical. As previously mentioned, GP73 levels in serum and liver tissue are closely associated with the severity of chronic liver disease and that the diagnostic value for early hepatocellular carcinoma is limited12,13. Indeed, serum GP73 has been deemed an effective and reliable marker for the diagnosis of liver inflammation and hepatic damage23,24. Unlike alanine aminotransferase (ALT), which is present in the cytoplasm of liver cells, GP73 is located in the Golgi apparatus. This means that GP73 is released into the bloodstream due to destruction of internal organelles, which is caused by severe damage to the liver. Moreover, ACLF is characterized by short-term massive liver cell necrosis resulting from chronic liver injury. The high serum levels of GP73 in patients with HBV-ACLF observed in this study might be associated in part with severe liver inflammation and hepatocyte damage, which can lead to poor survival outcomes.
Unlike GP73, a positive dose–response association between serum IL-6 and 90-day mortality in patients with HBV-ACLF was substantially attenuated after adjusting for potential confounders of complications, with this confounding effect being most pronounced in individuals with serum levels of IL-6 exceeding the inflection point at 98.78 pg/mL. The observed association between serum levels of IL-6 and mortality in this subgroup (IL-6 > 98.78 pg/mL, n = 20) should be interpreted with caution due to insufficient statistical power, necessitating further validation through large-scale studies with expanded datasets. Nevertheless, IL-6 still had a good predictive value, nearly similar to classical prognostic scores in ROC analysis. Notably, after combining GP73 and IL-6, the predictive efficacy of the MELD score had the best accuracy among all the models. IL-6 as a proinflammatory cytokine, was produced in large quantities when acute inflammatory reactions occur, causing extensive necrosis of liver cells and leading to severe hepatitis25,26. Some studies reported that serum IL-6 levels were higher in ACLF patients than in other patients with chronic hepatitis B, which was consistent with our findings19,20,21. Several studies have shown that IL-6 can predict 90-day mortality and is comparable to the MELD-Na model in end-stage liver disease patients22,27. However, when confounding factors include other clinical indicators, the predictive value of IL-6 is weakened22. Whether IL6 could be used as a high-risk factor for short-term prognosis in patients with HBV-related ACLF needs further study.
Finally, it should be noted that this study has inherent limitations as a single-center retrospective analysis without study without external validation cohorts. The associations between serum levels of GP73 and IL6 exceeding the inflection points (GP73 was 298.99 ng/mL and IL-6 was 98.78 pg/mL) and mortality risk did not reach statistical significance, necessitating further validation through expanded datasets to elucidate. In addition, the association between GP73 and IL-6 is currently unclear, which need further research. Few studies have reported that GP73 might be involved in the expression of cytokines including IL-6, but the effect is very contradictory in different studies28,29,30. In summary, the inflammatory status especially the serum levels of GP73 of HBV-ACLF patients should be paid more attention in clinical practice.
Materials and methods
Patient population
From February 2022 to April 2024, 149 patients with HBV-ACLF and 140 patients with chronic hepatitis B, were included in this retrospective study conducted in the Infection Department of the 910th Hospital of the PLA Logistics Support Force (Quanzhou, China). Patients were eligible for enrollment if they met the clinical diagnostic criteria for chronic hepatitis B or ACLF. The enrollment criteria for patients with HBV-ACLF were as follows: (1) a positive HBsAg test for more than 6 months; (2) an international normalized ratio (INR) of ≥ 1.5 or prothrombin activity of less than 40%; and (3) a total bilirubin (TBil) level of ≥ 10 times the upper limit of normal. The exclusion criteria for patients with HBV-ACLF were as follows: (1) infection with hepatitis A, C, D, or E virus; (2) autoimmune liver disease; (3) alcoholic liver disease; (4) drug-induced liver disease; (5) Wilson’s disease; (6) obstructive jaundice; (7) malignancy, including HBV-related hepatocellular carcinoma; and (8) history of liver transplantation and anticoagulant use1,18. The survival status of 149 patients with HBV-ACLF was followed up for 3 months after diagnosis. This study was approved by the Ethics Committee of the 910th Hospital of the PLA Logistics Support Force. The ethics committee waived the requirement of patient consent due to data were analyzed anonymously and the retrospective nature of the study did not compromise the health, safety, and privacy of the patients. The study was conducted in accordance with the tenets of the 2013 Helsinki Declaration.
Laboratory tests and data collection
The clinical data of patients with HBV-ACLF, which included demographic characteristics, and laboratory markers [e.g., alanine aminotransferase (ALT), aspartate aminotransferase (AST), albumin, total bile acid (TBA), total bilirubin (TBil), cholinesterase, blood urea nitrogen (BUN), creatinine (Cr), blood platelet count (PLT), blood neutrophil count, blood lymphocyte count, INR, sodium, serum HBV surface antigen (HBsAg) level and serum HBV DNA quantification], were collected at enrollment. The complications of patients with HBV-ACLF, which included ascites, hepatic encephalopathy (HE), pulmonary infection (PI) and gastrointestinal hemorrhage (GH), were also evaluated.
Serum GP73 were detected via an enzyme-linked immunosorbent assay and when the serum level of GP73 reaches 150 ng/mL or above, the sensitivity for diagnosing hepatocellular carcinoma stands at 70.2%, with a specificity of 88% (Hotgen Biotechnology, China). Serum IL-6 levels were detected via an automatic electrochemical luminescence immunity analyzer and the detection range of undiluted serum samples is 1.5–5000 pg/mL (Roche Diagnostics, Germany). HBsAg was detected via the Cobas e601 system and the detection range of undiluted serum samples is 0.05–130 IU/mL (Roche Diagnostics, Germany). The extraction of serum HBV DNA was performed via the Natch S system using superparamagnetic nanomagnetic bead (Sansure Biotech Inc., China). The quantification of HBV DNA was performed via the Mx3000P system using real-time PCR (Agilent Technologies, Santa Clara, CA, USA), with an HBV detection limit of 20 IU/L.
Statistical analysis
Continuous variables and categorical variables are expressed as medians (interquartile ranges) and numbers (percentages), respectively. The serum GP73 and IL-6 levels were divided into three tertiles in ascending order. In the three tertile groups, the GP73 and IL-6 levels were analyzed as continuous variables. The Kruskal‒Wallis rank sum test was used for continuous variables to compare the differences between groups. The chi-square test was used for categorical variables. Kaplan‒Meier survival curves were used to analyze the cumulative survival rate among the three tertile groups (GP73 or IL-6). The log-rank test was used to compare significant differences. Hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of mortality at 90 days were assessed via multivariate Cox proportional hazard models. Some indicators that were significantly different between the survival and nonsurvival groups at 90 days in patients with HBV-ACLF were included as potential confounders in the Cox regression models. A test for linear trend was used with the median value of each tertile of GP73 or IL-6 as a continuous variable in the models. A smoothing function was used to analyze the relationship between the serum GP73 or IL-6 concentration and the risk of 90-day mortality in patients with HBV-ACLF. The log-likelihood ratio test was used to compare the significant differences between the one-line linear regression model and two-piecewise linear regression models. Receiver operating characteristic (ROC) curves were used to evaluate the predictive value of GP73 and IL-6 for 90-day prognostic in patients with HBV-ACLF. All the statistical tests were performed via GraphPad Prism version 5.0 (GraphPad Software Inc., La Jolla, CA, USA) and EmpowerStats (X&Y Solutions, Inc., Boston, MA, USA). A P value of < 0.05 for a two-sided test was considered statistically significant.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
References
Liver Failure and Artificial Liver Group, Chinese Society of Infectious Diseases, Chinese Medical Association, Severe Liver Disease and Artificial Liver Group, Chinese Society of Hepatology, Chinese Medical Association. Guideline for diagnosis and treatment of liver failure. Zhonghua Gan Zang Bing Za Zhi 27, 18–26 (2019).
Malinchoc, M. et al. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 31, 864–871 (2000).
Biggins, S. W. et al. Evidence-based incorporation of serum sodium concentration into MELD. Gastroenterology 130, 1652–1660 (2006).
O’Grady, J. G., Alexander, G. J., Hayllar, K. M. & Williams, R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology 97, 439–445 (1989).
Pugh, R. N., Murray-Lyon, I. M., Dawson, J. L., Pietroni, M. C. & Williams, R. Transection of the oesophagus for bleeding oesophageal varices. Br. J. Surg. 60, 646–649 (1973).
Sarin, S. K. et al. Correction to: Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): An update. Hepatol. Int. 13, 826–828 (2019).
Jalan, R. et al. Toward an improved definition of acute-on-chronic liver failure. Gastroenterology 147, 4–10 (2014).
Brown, A. J. et al. Cholesterol, statins and cancer. Clin. Exp. Pharmacol. Physiol. 34(3), 135–141 (2007).
Ba, M. C., Long, H., Tang, Y. Q. & Cui, S. Z. GP73 expression and its significance in the diagnosis of hepatocellular carcinoma: A review. Int. J. Clin. Exp. Pathol. 5, 874–881 (2012).
Marrero, J. A. et al. GP73, a resident Golgi glycoprotein, is a novel serum marker for hepatocellular carcinoma. J. Hepatol. 43, 1007–1012 (2005).
Mao, Y. et al. Golgi protein 73 (GOLPH2) is a valuable serum marker for hepatocellular carcinoma. Gut 59, 1687–1693 (2010).
Liu, T. et al. Serum Golgi protein 73 is not a suitable diagnostic marker for hepatocellular carcinoma. Oncotarget 8, 16498–16506 (2017).
Xu, Z. et al. Predictive value of serum Golgi protein 73 for prominent hepatic necroinflammation in chronic HBV infection. J. Med. Virol. 90, 1053–1062 (2018).
Wei, M. et al. Serum GP73—An additional biochemical marker for liver inflammation in chronic HBV infected patients with normal or slightly raised ALT. Sci. Rep. 9, 1170. https://doi.org/10.1038/s41598-018-36480-3 (2019).
Ye, Q. X. et al. Short-term prognostic factors for hepatitis B virus-related acute-on-chronic liver failure. World J. Clin. Cases 10, 8186–8195 (2022).
Tong, J. et al. Relationship between the level of serum Golgi protein 73 and the risk of short-term death in patients with ALD-ACLF. J. Clin. Transl. Hepatol. 10, 449–457 (2022).
Gao, W. et al. Comparison of serum GP73 and p62 measurement to predict short-term prognosis in patients with HBV-related acute-on-chronic liver failure. Zhonghua Gan Zang Bing Za Zhi 29, 855–860 (2021).
Zhang, X. M. et al. Pattern of serum α-fetal protein, intereleukin-6 and Golgi protein 73 expressed in liver diseases and their diagnostic value on hepatocellular carcinoma. Chin. J. Exp. Clin. Infect. Dis. (Electron. Ed.) 11, 339–344 (2017).
Wu, Z. B. et al. Plasma interleukin-6 level: A potential prognostic indicator of emergent HBV-associated ACLF. Can. J. Gastroenterol. Hepatol. 2021, 5545181. https://doi.org/10.1155/2021/5545181 (2021).
Zhou, C. et al. High levels of serum interleukin-6 increase mortality of hepatitis B virus-associated acute-on-chronic liver failure. World J. Gastroenterol. 26, 4479–4488 (2020).
Zhu, H. J. et al. The early warning value of WBC, IL-6 and NLR in patients with acute-on-chronic liver failure. Chin. Hepatol. 24, 1076–1078 (2019).
Zhu, B. et al. Serum cytokine and chemokine profiles and disease prognosis in hepatitis B virus-related acute-on-chronic liver failure. Front. Immunol. 14, 1133656. https://doi.org/10.3389/fimmu.2023.1133656 (2023).
Xu, Z. J. et al. Effects of microwave ablation on serum Golgi protein 73 in patients with primary liver cancer. World J. Gastroenterol. 28, 3971–3980 (2022).
Yao, M. et al. Serum GP73 combined AST and GGT reflects moderate to severe liver inflammation in chronic hepatitis B. Clin. Chim. Acta 493, 92–97 (2019).
Moreau, R. The inflammatory response and immune function. Semin. Liver Dis. 36, 133–140 (2016).
Giuli, L., Maestri, M., Santopaolo, F., Pompili, M. & Ponziani, F. R. Gut microbiota and neuroinflammation in acute liver failure and chronic liver disease. Metabolites 13, 772. https://doi.org/10.3390/metabo13060772 (2023).
Wang, Y. et al. Value of interleukin-6 combined with model for end-stage liver disease score in predicting the prognosis of hepatitis B virus-related acute-on-chronic liver failure. J. Clin. Hepatol. 38, 1774–1779 (2022).
Frans, M. T., Kuipers, E. M., Bianchi, F. & van den Bogaart, G. Unveiling the impact of GOLM1/GP73 on cytokine production in cancer and infectious disease. Immunol. Cell Biol. 101, 727–734 (2023).
Li, Y. et al. Inter-individual variability and genetic influences on cytokine responses to bacteria and fungi. Nat. Med. 22, 952–960 (2016).
Yao, M. et al. Diagnostic value of serum Golgi protein 73 for liver inflammation in patients with autoimmune hepatitis and primary biliary cholangitis. Dis. Mark. https://doi.org/10.1155/2022/4253566 (2022).
Acknowledgements
The present study was supported by the financial grants of Quanzhou High Level Talent Innovation and Entrepreneurship Project (2023C020YR) and Scientific Research Funds of Quanzhou Medical College (XJY2415).
Author information
Authors and Affiliations
Contributions
Zhengju Xu participated in the clinical case enrollment and design of experimental work. Xiaoman Zhang participated in the study design, data collection, analysis of data and drafted the manuscript. Jingjing He participated in follow up work. Xiangping He participated in data collection and analysis of data. Caiting He carried out experimental work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Written informed consents have been obtained from each patient, including approval of the treatment, willingness to publish details of the case, and consent to use of blood samples for the tests involved in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, X., He, J., He, X. et al. Golgi protein 73 and IL-6 as strong predictors of short-term prognosis in patients with HBV-ACLF. Sci Rep 15, 22191 (2025). https://doi.org/10.1038/s41598-025-06472-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06472-1