Abstract
Mounting evidence supports associations between air pollution and noise exposure and cardiovascular events; however, the relationships at low exposure levels and for stroke outcomes remain uncertain. The aim was to investigate the associations between environmental exposures over 1-year and 10-year periods and both stroke severity and stroke type in a registry-based cohort including people with stroke residing in a low-pollution area of Sweden. Patients with stroke admitted to the Sahlgrenska University Hospital from 2014 to 2019 were included. Stroke severity was assessed with the National Institutes of Health Stroke Scale and stroke types were ischemic and hemorrhagic. Annual residential environmental exposures (road traffic noise (LAeq,24h), inhalable particulate matter (PM10), and nitrogen oxides (NOx)) were assigned from high-resolution dispersion models to participants one year and for ten years prior to stroke, respectively. Of 4066 patients, 1965 (48.3%) were women. The mean (± SD) age was 73.6 (14.0) years. A total of 1563 (28%) had moderate to severe stroke, and 3603 (88.6%) had ischemic stroke. We did not find significant associations between environmental exposures (LAeq,24h, NOx, PM10) and stroke severity nor stroke type. The generally low levels of exposure and low variance of these environmental factors might explain the lack of observed associations.
Similar content being viewed by others
Introduction
Globally, one in four people are affected by stroke during their lifetime. This makes stroke the most common cause of long-term disability among adults with 18 million years lived with disability1. In Sweden, about 21 000 people are diagnosed with stroke yearly2. Together with World Health Organization (WHO), the European Stroke Organization (ESO) has launched an Action Plan with specific goals for stroke, to be attained by 20303. One goal is to reduce the number of strokes in Europe by 10%, which is anticipated to be attained by targeting lifestyle risk factors such as physical inactivity and by reducing environmental risk factors such as air pollution3. However, air pollution is not yet recognized as one of the major risk factors, although evidence is building concerning mechanisms and pathways for the negative effects of ambient particulate matter air pollution on vascular health4,5,6,7.
Ambient particulate matter (PM) air pollution is the major environmental cause of disease, contributing four million deaths per year, being the reason behind 17% of ischemic heart disease cases and 14% of stroke cases, and causing 24% of deaths in stroke worldwide8,9. Further, evidence on associations between air pollution and stroke incidence are building10,11. Short-term exposure to air pollution i.e. hours to days of exposure could act as a trigger for stroke and has been associated with incidence of stroke as well as stroke mortality12,13, associations being strongest for ischemic stroke type10,12. In line with this, long-term exposure to air pollution i.e. months to years, has also been associated with stroke incidence14,15. Positive associations between road traffic noise and stroke incidence have also been reported16,17,18.
Inhaled air pollutants initiate events that can lead to stroke, primarily through inducing systemic inflammation, autonomic nervous system dysfunction, and direct neurotoxicity10. The inflammatory pathway, triggered by inhaled particulates, releases pro-inflammatory markers and reactive oxygen species that can lead to coagulation, vascular dysfunction, and hypertension. Simultaneously, air pollutants may disrupt autonomic nervous system homeostasis, leading to increased sympathetic tone, vasoconstriction, elevated blood pressure, and cardiac arrhythmias10. Ultrafine particles can even breach the blood–brain barrier, potentially accumulating in areas of vascular inflammation and causing direct neurotoxicity and white matter injury. Chronic exposure to these pollutants exacerbates subclinical manifestations such as atherosclerosis, endothelial dysfunction, hypertension, and cardiac arrhythmias, further increasing the risk of stroke10. The mechanisms leading to ischemic and haemorrhagic strokes differ in their emphasis on these pathways. Ischemic strokes are more closely linked to atherosclerosis and cardio-embolism, where pollutants contribute to plaque instability and rupture, leading to vessel occlusion. Cardiac arrhythmias, particularly atrial fibrillation, induced by air pollution can also increase the risk of embolic strokes10. In contrast, haemorrhagic strokes are more associated with acute vasoconstriction and changes in vascular resistance resulting from autonomic nervous system dysfunction. Furthermore, chronic exposure to air pollution may lead to microvascular damage and cerebral microbleeds, predisposing individuals to haemorrhagic events10.
Beyond incidence of stroke, associations between air pollution and stroke severity have been investigated, showing inconclusive results. In Barcelona, a study of more than 2700 patients with stroke found that traffic noise was associated with a more severe stroke in the acute phase, but no association between PM2.5 and initial stroke severity19. In line with this finding, a study of approximately 2500 patients with stroke in London found no association between PM10 or NO2 and initial stroke severity20. Another study, including more than 3000 patients with ischemic stroke in the city of Corpus Christi, Texas, found that PM2.5 was associated with stroke severity, but only in socially disadvantaged areas21.
Air pollution levels differ geographically, being higher in Asian countries than in Europe and North America22, also reflected in findings of stronger association between air pollution and stroke in more polluted regions in the world10,13. In Sweden, air pollution levels are generally low, and have improved even further during the recent years23. In a Swedish study on traffic related air pollution and stroke incidence with longitudinal data, no clear associations were found, possibly reflecting relatively low levels of pollutants24. In another Swedish study with low levels of air pollution, associations with stroke incidence were only found for black carbon, but neither for PM10 or PM2.525. In yet another Swedish study, associations were found between long-term exposure to NOx, risk factors for stroke, and stroke incidence26.
There is thus evidence of associations between both air pollution and noise exposure and cardiovascular events, including stroke. However, the relationships at low exposure levels and for admission stroke severity or type of stroke remain uncertain. Therefore, this study aims to analyse possible associations between environmental exposures the year before stroke on admission stroke severity.
Also, to investigate possible associations between environmental exposures over the decade preceding hospital admission on the severity of stroke and stroke type.
Methods
We adhered to the guidelines outlined by the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) for reporting of this study.
Study design and study sample
This registry-based cohort study utilized data compiled from multiple registries and sources. Väststroke, Gothenburg’s local stroke registry, records information on patients admitted to stroke units at Sahlgrenska University Hospital (SU), which operates three stroke units. One of these units provides thrombolysis services for Gothenburg’s urban and rural populations, and thrombectomy services for the Västra Götaland County.
Data on stroke outcomes were obtained from Riksstroke, Sweden’s national quality registry for stroke care27. We collected data on stroke patients admitted to SU’s stroke units between 2014 and 2019. Environmental and climate data were modelled by the Swedish Meteorological and Hydrological Institute (SMHI). Additionally, socio-economic data were retrieved from Statistics Sweden’s Longitudinal Integrated Database for Health Insurance and Labour Market Studies (LISA), which contains comprehensive information on Swedish citizens28. Patients were included if they were 18 years or older at the time of the stroke, had a clinically confirmed index stroke, and a diagnosis consistent with the International Classification of Diseases, 10th Revision (ICD-10), specifically codes I61 (hemorrhagic stroke) and I63 (Ischemic Stroke). Furthermore, information on stroke severity upon hospital admission was necessary for inclusion. We excluded patients with incomplete data on environmental exposure variables, and a history of previous stroke (Table 1).
Procedure
Data sources were merged by the registry holders using unique Swedish personal identification numbers, and the final dataset was pseudonymized to protect participant privacy. Multiple registries and datasets were used to capture the diverse range of information needed for the study. Väststroke provided data on stroke severity and type, while Riksstroke contributed information on reperfusion treatments, medications, comorbidities, and living conditions. Geographic Information Systems (GIS) enabled the assignment of yearly mean exposure levels at participants’ residential addresses based on these data sets. LISA contributed data on education and income levels28. Healthcare professionals at stroke units recorded the data in Väststroke and Riksstroke, whereas governmental agencies entered the data for SMHI and LISA.
Variables and definitions
Outcomes
The primary outcome of this study was stroke severity at admission, assessed using the National Institute of Health Stroke Scale (NIHSS)29. The NIHSS total score ranges from 0 (no stroke symptoms) to 42 (severe stroke with multiple symptoms). If NIHSS data were missing from the registry, one author supplemented the information by reviewing patients’ medical records30. In this study, an outcome category moderate/severe stroke was defined as an NIHSS score ≥ 6, while a mild stroke was defined as an NIHSS score ≤ 531.
The secondary outcome was stroke type. Ischemic stroke (ICD-10 code I63) was an outcome category and defined as a stroke caused by a reduction in blood flow to a part of the brain, typically due to an obstruction in the arteries supplying blood to the brain32. Intracerebral hemorrhage (ICD-10 code I61) was a reference category and defined as non-traumatic bleeding within the brain tissue, distinct from bleeding in the ventricles or subarachnoid space32.
Environmental exposures
There were three primary explanatory variables in this study: the mean annual A-weighted 24-h equivalent sound pressure level (LAeq,24h), the mean annual concentrations of nitrogen oxides (NOx), and the mean annual concentrations of particulate matter with a diameter of 10 µm or less (PM10). Data on all primary explanatory variables were collected for the ten years preceding the stroke. Exposures were averaged across all previous addresses for participants who moved during the study period. For the main analyses, exposure data from one year before the stroke were used. In sensitivity analyses, we calculated the mean exposure levels over the entire 10-year period.
Concentrations of PM10 and nitrogen oxides (NOx) were modeled at a dynamic resolution of up to 50 × 50 m2, using methods detailed elsewhere23. In brief, emission inventories were compiled for the years 2000, 2011, and 2018, incorporating data on both local sources and long-range transport. Concentrations for intermediary years were interpolated and adjusted for meteorological variations. Local emissions were modeled using dispersion models, while long-range transport emissions were estimated with a bias-corrected chemical transport model. The modeled particle levels were validated by comparing them with data from quality-controlled monitoring stations. Illustrative maps and Geo files can be accessed through the Swedish National Data Service33,34. Illustrative maps of mean NOx and mean PM10 concentrations, as well as mean levels of LAeq,24h in the study area for the year 2018 are presented in Fig. 1.
Maps of the greater Gothenburg area, Sweden, with the levels of PM10 (µg/m3), NOx (µg/m3) and road traffic noise (dB) for the model year 2018, retrieved from Molnár and Ögren33,34. Air pollution and noise maps for SCAPIS environment (Version 1) [Data set]. University of Gothenburg. The maps were created in QGIS 3.22 (https://qgis.org/) by importing the geo-tiff files created using high resolution Gaussian dispersion models as described elsewhere https://doi.org/10.5878/btxv-v69823,35. The conversion for Lden is: Lden = LAEq,24h + 3.1.
Residential exposure to road traffic noise levels was based on traffic intensity data for the years 2000, 2011, and 2018, modeled using previously described techniques35. In brief, the 24-h A-weighted equivalent sound pressure level (LAeq,24h) from road traffic was estimated at the most exposed façade of each residence, using a dynamic grid with resolutions up to 25 m.
Yearly average exposure levels were assigned to all study participants using QGIS software (version 3.22, QGIS Development Team), based on their individual address history obtained from Statistics Sweden. The addresses were automatically geocoded and then manually checked and corrected for accuracy.
Variables and covariates
The following covariates were analyzed: sex (male or female) and age (as a continuous variable). Income was based on disposable income during the year before the stroke, expressed in thousands of Swedish Krona (SEK) (average exchange rates for 2020 provided by the Swedish Riksbank (10.5 SEK = 1 EUR, 11.8 SEK = 1 GBP). Education was categorized into three levels: primary school (≤ 9 years), secondary school (10–12 years), and university education (≥ 13 years). Living circumstances were classified as either living alone or living with someone else. The need for assistance was defined as requiring help with daily activities or not. Accommodation was categorized as living in one’s own home, with or without community assistance, or residing elsewhere, including nursing homes. Reperfusion treatment was defined as either thrombolysis or thrombectomy. The length of hospital stay was measured as the number of days from admission to discharge. Additionally, data from Riksstroke were analyzed to include the following risk factors and comorbidities as covariates in multivariable regression models: diabetes, atrial fibrillation, and transient ischemic attack (TIA). For descriptive statistics, we included data on the use of thrombolysis and thrombectomy, as well as the length of hospital stay (in days).
Data analyses
Differences between included and excluded patients were assessed using the Chi-squared test for sex and stroke type, and the Mann–Whitney U test for age and stroke severity. Descriptive statistics for the sample were presented as frequencies with valid percentages (%), means with standard deviations (SD), and medians with interquartile ranges (IQR).
Crude associations between admission stroke severity groups and covariates were examined using binary logistic regression, with results reported as odds ratios (OR) and 95% confidence intervals (95% CI). Group differences in the primary independent variables, admission stroke severity categories, and stroke types were analyzed using independent sample t-tests.
The primary outcome variable was stroke severity at admission, defined as moderate to severe stroke (NIHSS ≥ 6) and the reference category was a mild stroke (NIHSS ≤ 5)31. We performed individual multivariable logistic regression analyses with NOx, PM10, and LAeq,24h as the main explanatory variables. The models were adjusted for covariates, including sex, age, education, country of birth, individual income in the year before the stroke, atrial fibrillation, previous transient ischemic attack, diabetes, accommodation type, and cohabitation status. Smoking was not included in the multivariable models due to the high proportion of missing values (13%). These variables were chosen based on authors’ clinical reasoning and previous studies36,37,38. Results were presented as OR with 95% CI. A similar regression analysis approach was applied to the secondary outcome, which was stroke type. In this analysis, hemorrhagic stroke served as the reference category, while ischemic stroke was the studied category. For sensitivity analyses, we calculated the mean levels of NOx, PM10, and LAeq,24h over the 10 years preceding the index stroke.
Ethics approval and consent to participate
Ethical approval has been granted by the Swedish Ethical Review Authority for the project in 2016-05-02 (346-16) with approved amendment 2020-06-15 (2020-02793). Collected data were protected by confidentiality regulations for Public Access to Information. Secrecy Act (2009:400), Chapter 24. The data were handled in accordance with the European Union (EU) General Data Protection Regulation (GDPR) and Swedish law (2018:218), which supplemented the GDPR. The Declaration of Helsinki was not relevant to this project, which was based on data generated in public registries. Informed consent: According to the Swedish Ethical Review Authority, quality registers are exempt to the general rule of patient consent according to the Personal Data Act (Swedish law No. SFS 1998:204).
Results
We included 4066 patients with a first-ever stroke in the study (Fig. 2). There were no significant differences between included (n = 4066) and excluded patients (n = 2425) in terms of sex (p = 0.06), stroke type (p = 0.13), or age (p = 0.13). However, included patients had significantly more severe strokes compared to excluded patients (p < 0.01), with mean (± SD) NIHSS scores of 5.6 (6.7) and 6.3 (7.3), respectively.
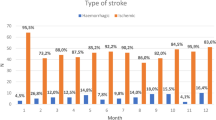
Sociodemographic, stroke-related characteristics, and environmental exposures
Of the 4066 included patients, 1965 (48.3%) were women, and the mean age was 73.6 years (± 14.0). A total of 3603 patients (88.6%) had ischemic strokes. Detailed information on the study sample, stratified by stroke severity, is presented in Table 1.
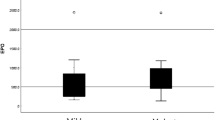
The average environmental exposures one year before stroke were 55.05 dB for LAeq,24h, 15.30 µg/m3 for NOx, and 14.39 µg/m3 for PM₁₀. The average environmental exposures over the 10-year period prior to stroke were 54.78 dB for LAeq,24h, 16.41 µg/m3 for NOx, and 15.09 µg/m3 for PM₁₀ (Table 2).
Environmental exposures and admission stroke severity
There were no significant associations between LAeq,24h (p = 0.29), NOx (p = 0.88), or PM10 (p = 0.08), and admission stroke severity. In multivariable binary logistic regression models, none of the environmental exposure variables significantly explained moderate to severe stroke at admission (Table 3). The complete multivariable models are presented in eTable 1, eTable 2, and eTable 3.
Environmental exposures and ischemic stroke
There were no significant associations between LAeq,24h (p = 0.54), NOx (p = 0.58), or PM10 (p = 0.38) and stroke types. The multivariable logistic regression analysis revealed that none of the environmental exposure variables were significant predictors of ischemic stroke (Table 4).The complete multivariable models are provided in eTable 4, eTable 5, and eTable 6.
Sensitivity analyses mean of 10 y exposure
In multivariable binary logistic regression analyses, higher PM10 levels were significantly associated with marginally lower odds of experiencing a moderate to severe stroke (OR = 0.82; p = 0.04; eTable 7). No significant associations were observed for LAeq,24h, or NOx exposures, eTable 8 and eTable 9, respectively. Additionally, ischemic stroke was not significantly associated with any of the environmental exposure variables (eTable 10, eTable 11, eTable 12).
Discussion
In this registry-based cohort study, no positive associations were found between long-term environmental exposures to air pollution and road traffic noise with initial stroke severity or stroke subtype in 4,066 patients with acute stroke. The levels of particulate matter air pollution and noise were, however, relatively low across all tested exposures and subgroups.
Similar to prior studies, initial stroke severity was not associated with long-term exposure to particulate matter air pollution19,20. Further, there were no associations between noise and initial stroke severity, which is contradictory to the previous findings on this topic, showing an association between road traffic noise and initial stroke severity among residents in Barcelona19. However, in that study noise levels were somewhat higher, and the associations were significant only regarding the highest quartile of noise levels, which may complicate comparison with the present study. However, in sensitivity analyses an association was found between higher exposure to PM10 and less severe stroke. This could possibly be due to multiple statistical testing, or perhaps the low exposure level and limited variability in the PM10 variable. However, we could not speculate further on this finding.
One aspect to keep in mind when interpreting our results is that the levels of air pollution were quite low compared with other studies14,20. Also, levels of noise were at the lower end compared to studies in the field17. The mean levels of PM10 in our study corresponded to the WHO 2021 air quality guidelines level of 15 µg/m3 as an annual average22.
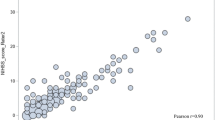
There are several strengths and limitations of this study. An observational design cannot establish causal relationships between environmental exposures and stroke outcomes. The reliance on registry data may also introduce potential biases due to missing or incomplete data, which could affect the accuracy of the analyses. The low levels of exposure and low exposure contrast may have contributed to the lack of significant associations observed in our study. Another aspect that could influence our results is that we were not able to assign PM2.5 in our data, but only had access to PM10. This is a limitation since the evidence on air pollution affecting stroke incidence is strongest regarding PM2.54,5,6,10. Long-term levels of PM10 and PM2.5 are however highly correlated (r = 0.85) in this setting39. Moreover, the assessment of environmental exposures was based on residential address data and did not account for individual variations in time spent outdoors or occupational exposures. We did, however, follow participants residential history and assign exposure from high-resolution models of good quality. Confounding factors, such as socioeconomic status and pre-existing health conditions, were considered, but residual confounding may still influence the results. Moreover, we did not include smoking in the multivariable models due to the high proportion of missing values, which may influence the results.
As a conclusion, the environmental exposures such as noise levels, nitrogen oxides, and particulate matter did not significantly influence stroke severity or type. Considered that the levels of air pollution were quite low, there are several clinical, and scientific implications of the study. First, these findings suggest that factors beyond environmental exposures should be considered when assessing stroke outcomes. While environmental factors are known to be associated with stroke incidence, this study indicates they may not play a critical role in determining stroke severity or type when hit by stroke in areas with low level of pollution. Second, from a public health perspective, while reducing environmental pollutants is crucial for overall health, these findings suggest that such interventions might not directly reduce the severity of strokes, and perhaps stoke severity is determined by other stronger predictors as age, sex, pre-morbid conditions, etc. However, in return, pre-morbid conditions, such as high blood pressure, is related to high levels of environmental exposures, associations which could be present in our data but not investigated in this study. Third, the results underscore the complexity of stroke aetiology and highlight the need for further research into other potential determinants of stroke outcomes. This could include genetic factors, social determinants of health, or other environmental exposures not covered in this study.
Data availability
The datasets generated and analysed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author on reasonable request.
References
Cieza, A. et al. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10267), 2006–2017 (2020).
registry. TR-tSs. Stroke och TIA, Riksstrokes årsrapport 2017 (2019).
Norrving, B. et al. Action plan for stroke in Europe 2018–2030. Eur. Stroke J. 3(4), 309–336 (2018).
Bevan, G. H., Al-Kindi, S. G., Brook, R. D., Münzel, T. & Rajagopalan, S. Ambient air pollution and atherosclerosis: Insights into dose, time, and mechanisms. Arterioscler. Thromb. Vasc. Biol. 41(2), 628–637 (2021).
Ding, R., Huang, L., Yan, K., Sun, Z. & Duan, J. New insight into air pollution-related cardiovascular disease: an adverse outcome pathway framework of PM2.5-associated vascular calcification. Cardiovasc. Res. 120(7), 699–707 (2024).
Kilbo Edlund, K. et al. Long-term ambient air pollution and coronary atherosclerosis: Results from the Swedish SCAPIS study. Atherosclerosis. 117576 (2024).
Brook, R. D. et al. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation 121(21), 2331–2378 (2010).
Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990–2021: A systematic analysis for the Global Burden of Disease Study 2021. Lancet. 403(10440), 2162–203 (2024).
Cohen, A. J. et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the Global Burden of Diseases Study 2015. Lancet 389(10082), 1907–1918 (2017).
Kulick, E. R., Kaufman, J. D. & Sack, C. Ambient air pollution and stroke: An updated review. Stroke 54(3), 882–893 (2023).
Lee, K. K., Miller, M. R. & Shah, A. S. V. Air pollution and stroke. J. Stroke 20(1), 2–11 (2018).
Toubasi, A. & Al-Sayegh, T. N. Short-term exposure to air pollution and ischemic stroke: A systematic review and meta-analysis. Neurology 101(19), e1922–e1932 (2023).
Lin, W., Pan, J., Li, J., Zhou, X. & Liu, X. Short-term exposure to air pollution and the incidence and mortality of stroke: A meta-analysis. Neurologist 29(3), 179–187 (2024).
Stafoggia, M. et al. Long-term exposure to ambient air pollution and incidence of cerebrovascular events: Results from 11 European cohorts within the ESCAPE project. Environ. Health Perspect. 122(9), 919–925 (2014).
de Bont, J. et al. Mixtures of long-term exposure to ambient air pollution, built environment and temperature and stroke incidence across Europe. Environ. Int. 179, 108136 (2023).
Yankoty, L. I. et al. Relationships between long-term residential exposure to total environmental noise and stroke incidence. Noise Health 24(113), 33–39 (2022).
Fu, W. et al. The association of noise exposure with stroke incidence and mortality: A systematic review and dose-response meta-analysis of cohort studies. Environ. Res. 215(Pt 1), 114249 (2022).
Münzel, T. et al. Transportation noise pollution and cardiovascular health. Circ. Res. 134(9), 1113–1135 (2024).
Vivanco-Hidalgo, R. M. et al. Association of residential air pollution, noise, and greenspace with initial ischemic stroke severity. Environ. Res. 179(Pt A), 108725 (2019).
Maheswaran, R., Pearson, T., Beevers, S. D., Campbell, M. J. & Wolfe, C. D. Outdoor air pollution, subtypes and severity of ischemic stroke—a small-area level ecological study. Int. J. Health Geogr. 13, 23 (2014).
Wing, J. J. et al. Synergism of short-term air pollution exposures and neighborhood disadvantage on initial stroke severity. Stroke 48(11), 3126–3129 (2017).
World Health O. WHO global air quality guidelines: particulate matter (PM2.5 and PM10), ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. (World Health Organization, 2021).
Kilbo Edlund, K. et al. High-resolution dispersion modelling of PM2.5, PM10, NOx and NO2 exposure in metropolitan areas in Sweden 2000‒2018–large health gains due to decreased population exposure. Air Qual. Atmos. Health. 1–15 (2024).
Korek, M. J. et al. Traffic-related air pollution exposure and incidence of stroke in four cohorts from Stockholm. J. Eposure Sci. Environ. Epidemiol. 25(5), 517–523 (2015).
Ljungman, P. L. S. et al. Long-term exposure to particulate air pollution, black carbon, and their source components in relation to ischemic heart disease and stroke. Environ. Health Perspect. 127(10), 107012 (2019).
Oudin, A. et al. Hospital admissions for ischemic stroke: Does long-term exposure to air pollution interact with major risk factors?. Cerebrovasc. Dis. 31(3), 284–293 (2011).
Asplund, K. et al. The Riks-Stroke Story: Building a sustainable national register for quality assessment of stroke care. Int. J. Stroke. 6, 99–108 (2011).
Ludvigsson, J. F., Svedberg, P., Olén, O., Bruze, G. & Neovius, M. The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur. J. Epidemiol. 34(4), 423–437 (2019).
Kwah, L. K. & Diong, J. National Institutes of Health Stroke Scale (NIHSS). J. Physiother. 60, 61 (2014).
Kasner, S. E. et al. Reliability and validity of estimating the NIH stroke scale score from medical records. Stroke 30, 1534–1537 (1999).
Spokoyny, I. et al. Defining mild stroke: Outcomes analysis of treated and untreated mild stroke patients. J. Stroke Cerebrovasc. Dis. 24(6), 1276–1281 (2015).
Sacco, R. L. et al. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44(7), 2064–2089 (2013).
Molnár, P. & Ögren, M. Air pollution and noise maps for SCAPIS environment (2024).
Molnár, P. & Ögren, M. Air pollution and noise GeoTIFF files for SCAPIS environment (2024).
Andersson, E. M. et al. Road traffic noise, air pollution and cardiovascular events in a Swedish cohort. Environ. Res. 185, 109446 (2020).
Vivanco-Hidalgo, R. M., Ribera, A. & Abilleira, S. Association of socioeconomic status with ischemic stroke survival. Stroke 50(12), 3400–3407 (2019).
Marshall, I. J. et al. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 14(12), 1206–1218 (2015).
Darehed, D., Reinholdsson, M., Viktorisson, A., Abzhandadze, T. & Sunnerhagen, K. S. Death and ADL dependency after scoring zero on the NIHSS: A Swedish retrospective registry-based study. Neurol. Clin. Pract. 13(5), e200186 (2023).
Kilbo Edlund, K. et al. Long-term ambient air pollution exposure and renal function and biomarkers of renal disease. Environ. Health. 23(1), 67 (2024).
Funding
Open access funding provided by University of Gothenburg. The study was financed by grants from the Swedish state under the agreement between the Swedish government and the county councils, the ALF agreement (ALFGBG-983906, ALFGBG-965653, ALFGBG-877961, ALFGBG-872511) and from the Swedish Stroke Association. The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Adam Viktorisson: Conceptualization, Investigation, Methodology, Writing – review & editing. Annie Palstam: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing – original draft, Writing – review & editing. Katharina Stibrant Sunnerhagen: Funding acquisition, Resources, Writing – review & editing. Leonard Stockfelt: Methodology, Resources, Writing – review & editing. Mikael Ögren: Data curation, Resources, Visualization, Writing – review & editing. Peter Molnár: Data curation, Resources, Visualization, Writing – review & editing. Tamar Abzhandadze: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abzhandadze, T., Molnar, P., Viktorisson, A. et al. No associations between environmental exposures and stroke severity in a low pollution area in Sweden. Sci Rep 15, 20218 (2025). https://doi.org/10.1038/s41598-025-06639-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-06639-w