Abstract
The current study integrated static (sFNC) and dynamic (dFNC) functional network connectivity to investigate the neurobiological mechanisms underlying alterations in static and dynamic functional network connectivity in subcortical vascular cognitive impairment (SVCI). We recruited 80 patients with SVCI (39 males, 41 females) and 83 healthy controls (32 males, 51 females). Clinical and imaging data, including clinical history, neuropsychological assessments, and Magnetic Resonance Imaging (MRI) scans, were collected. We extracted network independent components for sFNC and dFNC using independent component analysis with resting-state functional MRI data. Firstly, changes in sFNC in SVCI were comparatively analyzed. Subsequently, dynamic connectivity was examined using the sliding time window technique and cluster analysis to assess brain functional activity states and temporal properties. Differences in dFNC temporal properties (fractional occupancy, mean dwell time, and number of transitions) and functional connectivity across different time domains between groups were assessed with two sample t-tests. Spearman correlation analyses were performed to explore relationships between sFNC and dFNC changes and cognitive function. In the sFNC analysis, the SVCI group showed significantly decreased interactions between the sensorimotor network and lateral visual network, which was negatively associated with executive function (r = − 0.248, p = 0.027). In the dFNC analysis, brain functional activity was grouped into four highly structured functional connection states. The results revealed one connected state dominated by an increased connectivity pattern, two moderately connected states primarily characterized by increased connectivity with moderate decreases, and one weakly connected state exhibiting a modular connectivity pattern. These findings illustrate the progression in SVCI from connectivity disruption to compensation, eventually leading to a diminished compensatory response. Fractional occupancy and mean dwell time of states were correlated with cognitive function (all p < 0.05). SVCI patients exhibit impairments in both sFNC and dFNC, linked to cognitive decline. Connectivity dynamics reflect the brain’s adaptive capacity in response to cognitive impairment.
Similar content being viewed by others
Introduction
Vascular cognitive impairment (VCI) is the second most common cause of dementia after Alzheimer disease1 and is a huge burden on families and society. Cerebral small vessel disease (CSVD), which is common with aging, is characterized by asymptomatic lacunar infarcts, white matter hyperintensities (WMH), and other features visible on routine magnetic resonance imaging (MRI)2. It can manifest as stroke, cognitive decline, neurobehavioural symptoms, or functional impairment. When CSVD is accompanied by cognitive decline, it is defined as subcortical vascular cognitive impairment (SVCI)3. SVCI represents a continuum of cognitive impairment associated with CSVD4,5,6, accounting for more than 50% of VCI and associated with a higher dementia risk7,8. However, due to the diverse clinical presentations, the underlying pathogenesis of SVCI remains poorly understood, and no effective drugs are currently available for its prevention and treatment.
Magnetic resonance imaging (MRI) is the primary diagnostic method for detecting and evaluating the degenerative pathological process of CSVD due to its higher sensitivity and specificity compared to CT9. The imaging surrogate markers of CSVD, including recent small subcortical infarcts, white matter hyperintensities (WMH), cerebral lacunae, cerebral microbleeds, enlarged perivascular space, and brain atrophy, are associated with SVCI10. Among these, WMH is a typical feature of CSVD11, which is a significant contributor to dementia worldwide. However, there are some limitations to the relationship between the above brain imaging markers and cognitive impairment such as whether a threshold effect or anatomical distribution (strictly lobar vs deep vs mixed) is relevant12, and CSVD brain imaging markers are not consistent with the clinical manifestations of patients13,14.
Studies have shown that SVCI is a pathophysiological process that disrupts whole-brain network connectivity15. As a non-invasive imaging method, resting state-functional MRI (rs-fMRI) allows ease of data collection and can fully demonstrate the changes in the brain functional network connectivity at voxel, brain region, and large-scale levels. It has become the primary imaging method for investigating alterations in brain functional networks associated with SVCI. A brain network is an interconnected system of brain regions that integrates local and distant areas through densely connected pathways to facilitate cognition, behavior, and complex brain functions16. The brain connections support the latent mechanisms that determine the function of the brain and cognition as we know it17. The brain network is constructed to pay more attention to the integration of whole-brain information caused by changes in different structures and functions, which is of great significance for understanding the occurrence and development mechanism of SVCI.
In recent years, rs-fMRI has been used to study the brain functional network of patients with SVCI. It has been found that the underlying pathogenic mechanism of SVCI involves network disruption18. A large-scale static functional network connectivity (sFNC) analysis has found that the disruption of the functional network is closely related to SVCI; for example, increased within-network connectivity of the frontoparietal network (FPN) and reduced negative connectivity between the FPN and the default mode network (DMN) have been correlated with SVCI19. However, the large-scale sFNC analysis assumed that brain activity remained relatively stable during the whole rs-fMRI scanning (> 5 min), and the time-dependent relationship between signals in different brain regions were explored by averaging the whole time period to obtain the sFNC. Experimentally controllable mental states cannot be achieved by individuals in reality20. Different temporal scales have been found to considerably affect sFNC21,22,23. As a result of spontaneous changes in the underlying networks, time-varying characteristics may reveal neuronal mechanisms that cannot be discovered by sFNC alone24. Dynamic FNC (dFNC) is a widely used method that can comprehensively reveal changes in brain functional network connections by making full use of information in the collected data. There are limited studies on changes in dFNC connectivity in patients with SVCI25,26,27. Chen et al.26 and Huang et al.27 explored the changes in dFNC related to cognitive functions in patients with CSVD, without integrating sFNC and without separately comparing the SVCI group. Li et al.25 compared the sFNC and dFNC in CSVD patients with Alzheimer’s Disease (AD), focusing only on the three common networks—DMN, salience network (SN), and executive control network (ECN)—and not on mild cognitive impairment. Mild cognitive impairment is a transition phase between normal cognition and dementia. By combining sFNC and dFNC, we present a comprehensive framework for investigating the cognitive impairment in SVCI patients, revealing new insights into the disease’s mechanisms.
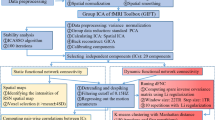
In our study we hypothesized that sFNC analysis can partly reflect changes in brain networks and dFNC analysis can show the changes in brain networks in patients with SVCI more comprehensively. In this study, network independent components for both sFNC and dFNC were extracted using independent component analysis in SVCI patients. Then, the sliding time window and cluster analysis were employed to obtain the temporal properties of dFNC. We comparatively analyzed changes in both sFNC and dFNC in SVCI to explore the underlying neurobiological mechanisms of SVCI.
Results
Demographic and clinical characteristics
Eighty SVCI patients [39 males, 41 females, mean age (65.89 ± 6.59) years] were prospectively included in the discovery cohort. During the same period, 83 healthy controls (HCs), matched for sex, age, and education level with the SVCI group, were included. Demographic details and cognitive performance of the study participants are given in Table 1. There were no significant differences in age, sex, education, and history of hypertension, diabetes, or hyperlipidemia between the SVCI and HCs. There were significant differences in the cognitive assessment between the two groups.
Networks of interests
Through multiple ICASSO clustering analyses and a spatial correlation analysis between the ICA spatial maps and a widely used resting-state network (RSN) template28, a total of 34 independent components (ICs) were identified, from which 12 meaningful functional network independent components were selected. Spatial correlation analysis demonstrated that the ICA-derived components closely matched established functional brain networks. These included the auditory network (AN, IC 3, r = 0.770), default mode network (DMN, ICs 22 and 29, r = 0.320 and 0.319, respectively), dorsal attention network (DAN, IC 17, r = 0.430), sensorimotor network (SMN, IC 4, r = 0.687), left frontoparietal network (lFPN, IC 8, r = 0.460), right frontoparietal network (rFPN, IC 31, r = 0.440), ventral attention network (VAN, IC 19, r = 0.368), salience network (SN, IC 1, r = 0.725), lateral visual network (lVN, ICs 10 and 16, r = 0.630 and 0.378, respectively), and medial visual network (mVN, IC 14, r = 0.835) (Supplementary Fig. 1 and Supplementary Fig. 2).
Differences between groups in sFNC
A static FNC was then estimated via the Pearson correlation coefficients of the entire time course of the functional networks for each group, resulting in a symmetric static FNC matrix with 12 × 12 dimensions, encompassing the entire scanning period for each subject, constructed using the 12 meaningful network components. Pairwise comparisons were then performed between different network components, resulting in 12*11/2 comparisons, which could increase the false positive rate. To reduce the false positive rate, p values were corrected using the False Discovery Rate (FDR) method, with a corrected threshold set at 0.05. A corrected p value of less than 0.05 was considered statistically significant. For the sFNC analysis, it was found that the SVCI group exhibited significantly decreased interactions between the SMN (IC 4) and lVN (IC 10) (SVCI: − 0.0108 ± 0.3522; HC: 0.1973 ± 0.3314; t = − 3.8856, FDR-adjusted p values = 0.0001, Fig. 1), when compared to the HCs. Supplementary Fig. 3 presents the FDR-adjusted p values for comparisons among all network components.
Static functional network connectivity. The image is a connectogram graph which shows decreased interactions of SMN (IC 4) and lVN (IC 10) (SVCI: − 0.0108 ± 0.3522; HC: 0.1973 ± 0.3314; t = − 3.8856, FDR-adjusted p values = 0.0001) in the internetwork of sFNC in SVCI compared to HC group. The image was generated using GroupICATv4.0b (https://github.com/trendscenter/gift).
Differences in dFNC between groups
In dynamic functional network connectivity analysis, a state indicates the frequency and structure of recurrent patterns in functional network connectivity29. These states are characterized by distinct and statistically significant configurations of brain activity that recur over time. Fractional occupancy (FO) is the number of windows in each state relative to the total number of windows, mean dwell time (MDT) is defined as the number of contiguous windows belonging to a state, and the number of transitions is defined as the number of transitions between states, indicating the reliability of each state. Using the k-means clustering approach repeated three times, we consistently found the optimal number of clusters to be k = 4. Therefore, we selected k = 4 as the optimal number of clusters (Supplementary Fig. 4). This analysis yielded four distinct and highly structured functional connectivity states, along with their respective cluster centroids (Fig. 2).
Matrices and connectograms of four highly structured functional connection states and corresponding cluster centers. States 1 (21%) and 2 (31%) were moderately connected, primarily characterized by increased connectivity with moderate decreases (A–D). State 3, the most frequent (36%), showed predominantly weak connectivity, but with a modular pattern—marked by enhanced connectivity within the DMN and mVN (E and F). State 4, the least frequent (13%), exhibited strong connectivity patterns (G and H).
After discarding the first 10 time points during preprocessing, 290 time points per subject were retained for analysis. Using a sliding window approach with a window length of 30 TRs, 260 windows were generated for each subject, resulting in a total of 42,380 windows across all 163 participants. Among these, 8973 windows were assigned to state 1, accounting for 21% of the total. The remaining windows were distributed across state 2 (31%), state 3 (36%), and state 4 (13%), respectively. Specifically, State 4, the least frequent (13%), exhibited strong connectivity patterns (Fig. 2G and H). States 1 (21%) and 2 (31%) were moderately connected, primarily characterized by increased connectivity with moderate decreases (Fig. 2A to D). State 3, the most frequent (36%), showed predominantly weak connectivity, but with a modular pattern—marked by enhanced connectivity within the DMN and mVN (Fig. 2E and F). The results demonstrated that the occurrence rate for each group across the four states was notably high, ranging from 56.25% to 98.80%. These rates represent the proportion of time that the brain remains in each state during the observation period, illustrating the dynamic stability and transitions of brain activity.
The network connectivity differences between two groups across various states were analyzed using a two-sample t-test, with FDR correction, the adjusted p value threshold was set at 0.05. The results of the altered connection strength among the four states in SVCI patients and HCs were shown in Fig. 3. The color bar indicates signed -log10(p value), derived from the direction of group differences (HCs minus SVCI). Positive values reflect significantly higher connectivity in the SVCI group, whereas negative values indicate reduced connectivity relative to HCs. Values within the boxes represent FDR-corrected p values.
Differences in dFNC between SVCI and HCs of four highly structured functional connection states. (A) In State 1, the SVCI group showed reduced connectivity between the mVN and the VAN, while the overall pattern demonstrated a relatively greater increase in global connectivity. (B) In State 2, reduced connectivity was observed primarily among the DMN, FPN, and SN, while connectivity between the VN and other networks was enhanced. (C) In State 3, decreased connectivity was mainly observed between the FPN and other networks, accompanied by increased connectivity between the VN and several other networks. (D) In State 4, the SVCI group demonstrated reduced connectivity between the SN and SMN compared to the HC group.
The group differences in dFNC across the four states exhibit distinct patterns. Overall, the SVCI group showed a general trend of decreased connectivity, particularly in inter-network connections, while the HCs maintained stronger network integration.
In State 1 (Fig. 3A), the SVCI group exhibited a relatively greater increase in overall connectivity, although connectivity between the mVN and the VAN was reduced, potentially reflecting a compensatory mechanism. In States 2 and 3, the SVCI group showed a combination of increased and decreased connectivity across multiple networks. Specifically, in State 2, reduced connectivity was observed primarily among the DMN, FPN, and SN, while connectivity between the VN and other networks was enhanced (Figs. 3B). In State 3, decreased connectivity was mainly observed between the FPN and other networks, accompanied by increased connectivity between the VN and several other networks (Fig. 3C). In State 4 (Fig. 3D), the SVCI group demonstrated reduced connectivity between the SN and SMN compared to the HC group. Detailed results of network connectivity changes across the four states are provided in the supplementary materials.
Temporal properties of dFNC states
We analyzed group-level dFNC states to examine the temporal dynamics of functional connectivity between groups. The differences in the temporal properties of the FNC states between the two groups are shown in Fig. 4. The results indicated significant group differences in the mean dwell time in state 2. The FO (SVCI: 0.408 ± 0.274; HCs: 0.305 ± 0.250, p = 0.012) and MDT (SVCI: 37.663 ± 42.948; HCs: 25.616 ± 25.021, p = 0.029) of the SVCI group was longer than that of the HCs group in state 3. However, no significant group differences were observed in the number of state transitions (p > 0.05).
Comparison of fractional occupancy, mean dwell time and number of transitions between the two groups for each state. (A) Fractional occupancy in dynamic states of SVCI group was longer than HCs group in state 3. (B) Mean dwell time of SVCI group was longer than HCs group in state 3. (C) Number of transitions in dynamic state had no group difference.
Correlation results and mediation effects
The relationship between FNC attributes and cognitive performance in the SVCI group was examined to explore their association with cognitive impairments. In the SVCI group, the correlations of decreased interactions of SMN-lVN in the internetwork with the cognitive performance of SVCI group were further analyzed. The results showed that the interactions of SMN-lVN in the internetwork were negatively associated with executive function (r = − 0.248, p = 0.027, Fig. 5A). In dFNC, the correlation of the temporal properties of FNC states, including FO, MDT, and number of transitions of four highly structured functional connection states, with cognitive performance of the SVCI group were further analyzed. The results revealed that FO of state 2 was positively associated with global cognitive function (r = 0.232 and 0.270, p = 0.038 and 0.017, respectively), while the FO of state 3 was negatively associated with global cognition (r = − 0.232, p = 0.038). In contrast, the FO of state 4 also showed a positive correlation with global cognitive function (r = 0.235, p = 0.038) (Fig. 5B). Additionally, the MDT of state 1 was negatively associated with attention (r = − 0.276, p = 0.013), whereas the MDT of state 4 was positively correlated with global cognition (r = 0.249, p = 0.028) (Fig. 5C). No significant associations were found between the number of state transitions and any cognitive domain, suggesting that the temporal properties of dynamic states may be more relevant to cognitive function than the frequency of switching.
The correlation between functional connectivity and cognitive function in SVCI. (A) The correlations of decreased interactions with cognitive performance of SVCI group in sFNC. (B) The correlation of the fractional occupancy in four highly structured functional connection states, with cognitive performance of SVCI group. (C) The correlation of the mean dwell time in four highly structured functional connection states, with cognitive performance of SVCI group. * indicates p < 0.05, indicating statistical significance of the correlation.
STRIVE-2 was developed as an update to STRIVE-1 to incorporate new findings on SVD markers, advanced MRI techniques, and emerging imaging biomarkers, aiming to better assess vascular changes in aging and neurodegeneration. The STRIVE-2 criteria define a summary CSVD score as a composite measure that combines accepted SVD markers into a single index, score, or unified construct2. We also examined the correlation between the summary CSVD score and patients’ cognitive function and further explored whether functional connectivity mediates the relationship between the CSVD summary score and cognitive function. Our findings indicate that the summary CSVD score is significantly associated with cognitive function in SVCI. However, further mediation analysis revealed that functional connectivity does not mediate the effect of the summary CSVD score on cognitive function (Supplementary Fig. 5).
Discussion
The present study combined sFNC analysis with dFNC analyses to investigate the whole-brain features of SVCI, focusing on the correlation between cognitive function and abnormal interactions of sFNC, as well as the temporal properties in the dFNC states on large-scale functional network connectivity. The results revealed that the altered sFNC and dFNC features are associated with cognitive performance in the SVCI group, which may provide insights into additional relevant information on the disease and help map the full picture of connectivity abnormalities.
Analyzing changes in large-scale functional network connectivity provides valuable insights into the dynamic interactions between brain regions that underline cognitive functions. This method allows us to identify specific network alterations associated with disease pathology, such as disrupted connectivity patterns in memory or executive function networks, which are commonly observed in neurological and psychiatric conditions. CSVD has been proven as a slowly progressing disease that destroys subcortical networks, leading to various symptoms, especially cognitive impairment8, which is clinically referred to as SVCI. Although an increasing number of studies have reported alterations in brain structural or neuronal functional activity exhibited in patients with SVCI, it is still unclear which alterations are reliable.
Proposed by the Scaffolding Theory of Aging and Cognition (STAC)30, the maintenance of functional performance in older age may be related to the flexible and adaptive allocation of limited neural resources. The brain network connectome utilizes graph theory to analyze brain lesions from both an integrated and a segregated perspective. Consistent with our initial hypothesis, in sFNC analysis of the present study, the results showed relatively little network change. Consistent with findings of previous studies on other neurological and psychiatric disorders31,32, the results of the present study showed that the abnormal interactions of sFNC were related to cognitive function. Specifically, abnormal interactions of SMN-lVN in the internetwork negatively correlated with executive function. According to previous study, altered cortico-striatal circuitry is associated with SVCI33. Visual networks, from occipital, temporal, and parietal cortices and also from cortical regions in the ventral and dorsal stream, have been shown to be related to cognitive dysfunction34, especially visuospatial function35, which is consistent with the results of the present study. Connectivity changes in the sensorimotor network, indicating impaired cortico-striatal loops35, have also been proven to be associated with cognitive impairment35. The result of sFNC indicated that the damage of the brain functional network in SVCI patients may indicate the disruption of cortico-striatal circuitry.
dFNC assumes that whole brain connectivity sequentially iterates through a finite set of connectivity patterns known as dFNC states. In the present study, brain functional activity was grouped into four highly structured functional connection states in dFNC. Then, by comparing the network connection changes in different states of the two groups, we found that the network connection changes in different states have certain characteristics. State 3, characterized as a strongly connected state dominated by reduced connectivity, may represent an early stage of the disease, where connectivity reductions begin to emerge but are not yet extensively widespread or irreversible. In state 4, although the connectivity between the mVN and the VAN was reduced, the overall pattern exhibited a relatively greater increase in global connectivity, potentially reflecting a compensatory mechanism. States 1 and 2 were characterized by moderately reduced connectivity accompanied by localized increases, whereas state 3 showed a marked decrease in connectivity with only minimal enhancement in specific regions, possibly indicating a progressive stage of network decompensation. State 3 represents a weakly connected state, in which increased intra-network connectivity within the DMN and VN suggests localized functional organization despite diminished global network integration. Prolonged FO and MDT in network connection changed state (state 3) suggest inefficient functional integration and flexibility in the brain36. These disruptions may hinder the brain’s capacity to adapt to dynamic cognitive demands. Overall, these findings suggest that the brain’s connectivity dynamics vary significantly across states, highlighting the brain’s flexible and adaptive nature in managing its neural resources to meet varying demands and conditions.
Consistent with our initial hypothesis, compared with sFNC, the change in network connections in dFNC were more comprehensive and complex, but somewhat overlapping. In addition to SMN and VN found by sFNC, DMN, SN, FPN, AN, and DAN network connections in SVCI patients were also obviously altered by dFNC analysis. This indicates that dFNC reflects more comprehensive information about brain functional activity, consistent with a previous study37. Some scholars have explored the relationship between FNC and cognitive impairment, and found that DMN, SN, and FPN have the most important relationship with cognition38, DMN is mainly related to attention, FPN is primarily related to executive function, SN is a dynamic converter between the DMN and the FPN, reflecting the switch of human brain in the state of memory and executive function39, and the integration and separation of these three networks is the key to maintaining cognition and the key mechanism in causing cognitive impairment40. This study found that in state 2, connectivity within the DMN and between the DMN and both the FPN and SN was reduced, consistent with previous findings. Meanwhile, increased connectivity between the VN and other networks suggests a compensatory mechanism during the progression of SVCI. In dFNC, brain network connection changes are more widespread, which indicated that the dynamic properties of brain networks may be a more reliable biomarker of cognitive change which needs to be validated with larger data volumes.
The CSVD score is significantly associated with cognitive function, and dFNC attributes are also related to cognitive function. However, mediation analysis shows that functional connectivity does not mediate the effect of the CSVD score on cognitive function. Study has found that whether WMH matches cognitive function is associated with dFNC connectivity patterns in CSVD41, suggests that CSVD markers, dFNC attributes, and cognitive function may not have a simple mediating relationship. Further research, including advanced connectivity analyses and longitudinal studies, may help to disentangle these relationships more fully.
This study has some limitations which must be discussed. First, patients with CSVD without cognitive impairment were not included in this study. Although we performed further analysis to confirm the correlation between network connection changes and cognitive function, patients with CSVD without cognitive impairment should be included in future studies. Second, this study included a small sample of SVCI patients. To ensure the stability of the results, multiple ICASSO clustering analyses were performed, and the similarity and stability of the components were further validated by assessing the correlation between components from two independent runs, thereby enhancing the accuracy and reliability of the findings. The sample size should be increased to further test the reliability of the results. Third, there was no analysis of external data to evaluate the stability of the results. Finally, we did not conduct a longitudinal study, and the current analysis can only demonstrate the association between brain network connectivity changes and cognitive function in SVCI patients, without establishing a causal relationship. Our center has initiated follow-up studies aimed at exploring changes in network connectivity in patients with SVCI. In the future, we intend to perform FNC validation analysis and other in-depth network analysis using multi-center data with a larger sample size to ensure the reliability and stability of the results.
In conclusion, this study comprehensively demonstrated distinct patterns of FNC alterations in individuals with SVCI. SVCI neuropathology is associated with significant changes in static FNC, while exhibiting more pronounced dynamic FNC alterations closely linked to cognitive function. These findings suggest that dFNC not only validates but also expands upon the results of sFNC, providing reliable insights into the FNC changes associated with SVCI. Dynamic connectivity analysis reveals the brain’s adaptive capacity to cognitive impairment and suggests potential clinical applications, including early detection of cognitive decline, monitoring disease progression, and designing personalized interventions. Additionally, dynamic metrics offer a non-invasive means to evaluate therapeutic efficacy and optimize SVCI management.
Methods
Participants
The discovery cohort comprised individuals with SVCI (n = 80) and age-, sex-, and education-matched HCs (n = 83), recruited between December 2022 and September 2023. The replication cohort included individuals with SVCI (n = 36) and age-, sex-, and education-matched HCs (n = 36), recruited from October 2023 to November 2024. Inclusion criteria were, age between 50 and 80 years; education level above primary school; right-handed; imaging findings consistent with neuroimaging criteria for CSVD42 [(WMH Fazekas scale 2 or greater43, lacunar infarction, or cerebral microbleed (≥ 1)]; no history of malignant tumor, craniocerebral operation, massive cerebral infarction or cerebral hemorrhage; any other serious systemic disorders; mental illness; and any contraindications for MRI examination. Exclusion criteria included other causes of cognitive impairment (e.g., AD), clinical cerebrovascular disorders with large intracranial vascular lesions, and MRI images with artifacts that affected the observation. All healthy control group patients had normal nervous system examination (including neuropsychological assessments and MRI examination), with no history of mental disorders, and serious heart, lung, liver, and kidney diseases.
The study protocol was approved by the Ethics Committee of the Wuxi People’s Hospital (Institutional Review Board approval number: KY22080). The study was conducted after obtaining informed written consent from all the participants. All study methods were performed in accordance with the Declaration of Helsinki and local regulations.
Neuropsychological assessment
Each patient underwent a comprehensive and standardized neuropsychological assessment that has been used in other large epidemiological studies, including tests of global cognition and four cognitive domain tests. Global cognition was tested using the Mini-mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA). The four cognitive domain tests were as follows: (i) Executive functions: Trail Making Test B (TMT-B) and Stroop Color and Word Test (Stroop-C); (ii) Attention: Trail Making Test A (TMT-A) and Stroop Color and Word Test (Stroop-A, Stroop-B); (iii) Memory: Auditory Verbal Learning Test (AVLT-IR, Auditory Verbal Learning Test-immediate recall; AVLT-DR, Auditory Verbal Learning Test-20-min delayed recall); (iv) Visuospatial functions: Clock Drawing Test (CDT).
In all the neuropsychological tests, cognitive impairment was defined as a score below 1.5 standard deviations of the normative mean44. MCI was diagnosed by the respective mild neurocognitive disorder criteria of the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)45. The neuropsychological test scores of the healthy control group were all within the normal range.
MRI data acquisition
MRI scans were obtained using a 3.0-Tesla MR system (Prisma, Siemens Medical Solutions, Inc., Germany) with a 64-channel head coil. Foam padding was used to minimize motion of the head, and earplugs were used to dampen the scanner noise. All patients were instructed to relax, stay as still as possible, keep their eyes closed, think of nothing, and not fall asleep during the scanning process.
The scan sequences included T2WI, T2WI-FLAIR, SWI, 3D_TOF, 3D-T1WI, and resting-state functional MRI. T2WI was acquired with repetition time (TR) = 4960 ms, echo time (TE) = 109 ms and slice thickness = 5 mm; T2WI-FLAIR was acquired with TR = 8000 ms, TE = 84 ms and slice thickness = 5 mm; SWI was acquired with TR = 28 ms, TE = 20 ms and slice thickness = 2.5 mm; 3D_TOF was acquired with TR = 21 ms, TE = 3.3 ms and slice thickness = 0.7 mm. 3D T1-weighted structural images were acquired with the following parameters: TR = 2000 ms; TE = 2.49 ms; flip angle (FA) = 9; field of view (FOV) = 256 mm × 256 mm; matrix size = 256 × 256; slice thickness = 1 mm, no gap; 192 sagittal slices. Resting-state functional MRI data were acquired using a gradient-echo-planar imaging (GRE-EPI) sequence using a simultaneous multislice technique with the following parameters: TR = 1500 ms; TE = 31 ms; FA = 70; FOV = 211 mm × 211 mm; matrix size = 88 × 88; slice thickness = 2.4 mm, no gap; 60 interleaved axial slices; with a total acquisition duration of 7 min and 40 s.
Three senior radiologists (experience in radio diagnosis were five, eight and 12 years respectively) were assigned to diagnose the disease and rule out other brain lesions.
fMRI data processing
Image preprocessing
Resting-state BOLD data were preprocessed using the resting-state fMRI toolbox (RESTplus v 1.25, http://restfmri.net/forum/RESTplus). Each participant’s first 10 volumes were discarded to allow the signal to reach equilibrium and for the patients to adapt to the scanning noise. For the remaining volumes, the timing differences in slice acquisition were corrected46. Realignment was then performed between the time points to correct the motion. Spatial normalization was done by the diffeomorphic anatomical registration through the exponentiated Lie algebra (DARTEL) technique47. The specific steps were as follows: first step was to co-register individual structural images with the mean functional image, then DARTEL was used to segment and normalize the transformed structural images to the Montreal Neurological Institute (MNI) space. Using the deformation parameters estimated during the above step, each filtered functional volume was normalized to the MNI space and finally resampled into a 3-mm cube. The functional datasets were band-pass filtered in a frequency range of 0.01–0.1 Hz. The functional datasets underwent band-pass filtering with a frequency range between 0.01 and 0.08 Hz. A Gaussian kernel of 6 × 6 × 6 mm3 full width at half maximum was used to smooth all datasets following spatial normalization. During fMRI preprocessing, we also excluded images with excessive head motion during the scan (i.e., translational or rotational motion greater than 3 mm or 3°)48,49 and those with poor spatial normalization.
Group independent component analysis
After data preprocessing, group independent component (IC) analysis of fMRI Toolbox (GIFT version 4.0b; https://trendscenter.org/software/gift/) was used to extract meaningful functional networks from the two groups and calculate the FNC between networks50. The minimum description length (MDL) criteria were used to estimate the number of independent components (N = 34). Two data reduction steps and the infomax algorithm were used to decompose the spatial ICA data into linear mixtures of spatially independent components. The Infomax algorithm was repeated 100 times in ICASSO (http://cis.legacy.ics.tkk.fi/projects/ica/icasso/) to ensure estimation stability. ICASSO enhances the reliability of ICA components by performing multiple ICA runs with different random initialization seeds, followed by clustering analysis. In this study, two separate ICASSO clustering analyses were conducted, each with 100 repetitions, to assess the reproducibility and consistency of the ICA-derived component maps. The component maps from each ICA run were vectorized, and pairwise Pearson correlation coefficients (r) were computed to quantify the similarity and stability of the components. Components with a Pearson r greater than 0.9 were considered stable and retained for further analysis, whereas less stable components were excluded. Maps of participants’ specific spatial distributions and time courses were produced using GICA back-reconstruction, and the components were scaled using Z-scores.
Before sFNC and dFNC calculation, the following additional postprocessing steps were performed on the selected time courses of functional networks to remove physiological and scanner noise: (1) detrending linear, quadratic, and cubic trends; (2) despiking detected outliers; (3) lowpass filtering with a high-frequency cut-off of 0.15 Hz.
Identification of network components
To objectively identify and label the functionally relevant ICs derived from group-level ICA, we performed a voxel-wise spatial correlation analysis between the ICA spatial maps and RSN template. Prior to correlation, all images were resampled to a common resolution to ensure voxel-wise comparability. The analysis was conducted using the fslcc function from the FMRIB Software Library (FSL), which computes voxel-wise spatial Pearson correlations between input volumes. ICs showing moderate to high spatial similarity with canonical RSNs (defined as Pearson’s r > 0.3) were assigned to the corresponding functional networks. This data-driven approach ensured objective and reproducible component labeling.
To further validate the accuracy of the ICs derived from the ICA analysis, two independent reviewers identified functional network-independent components based on criteria including peak activation in the GM, minimal spatial overlap with known vascular, ventricular, motion, and susceptibility artifacts, and dominance in low-frequency power51. Subsequently, based on previous research findings52,53, we compared the spatial maps of each IC with the spatial distribution of known functional areas. Any discrepancies among the reviewers were resolved through discussion until a consensus was reached.
Static FNC analysis
A static functional network connectivity (FNC) matrix was computed by calculating the Pearson correlation coefficients across the entire time course of the functional network ICs for each group, resulting in a symmetric matrix that encompassed the entire scanning period for each subject. To assess differences within the sFNC matrix, we applied the MANCOVAN approach for pairwise comparisons of its elements. The statistical p values from these pairwise comparisons were corrected for multiple comparisons using the False Discovery Rate (FDR) method54, with a correction threshold set at p = 0.05 to minimize the risk of false positives.
Dynamic FNC analyses
We estimated the dFNC matrices of each patient using the sliding window approach, as reported in previous studies55. We used a window size of 30 repetition times (TR, 45 s) in steps of 1 TR (1.5 s), a sliding step as 1 TR, and obtained T = 260 windows for each patient. The rectangular window was convolved with a Gaussian (Alpha = 3TR) to obtain a tapered window, which was used to acquire dynamic information as described in a previous study56. We then applied the k-means clustering algorithm to explore recurring dFNC patterns across patients25.
The dFNC windows were clustered into distinct states using k-means clustering with squared Euclidean distance, employing 1000 iterations and 1000 repetitions to enhance robustness. The optimal number of mental states was determined using the elbow criterion, defined as the ratio of within-cluster to between-cluster distances. To ensure result stability, the k-means clustering procedure was repeated three times, and the average outcome across these runs was used for subsequent analyses.
Group differences in dFNC and temporal properties
We evaluated the group-level dFNC states to check the characteristics of dFNC states between groups. In each optimal state, differences in dynamic temporal properties (fractional occupancy and mean dwell time in each state, and the number of transitions) between groups (SVCI and HCs) in dFNC were investigated using two-sample t-tests, and the results were corrected for multiple comparisons using the FDR to reduce the false positive rate. We analyzed the temporal properties of the dFNC states by computing the fractional occupancy and mean dwell time in each state, as well as the number of transitions between states. A two-sample t-test was used to analyze the significance of the fractional occupancy, mean dwell time, and number of transitions of each state in the SVCI group and the HCs group.
Correlation between FNC attributes and cognitive performance
The correlation between FNC attributes and cognitive performance in the SVCI group was further analyzed. Since the cognitive assessment scores did not follow a normal distribution, spearman correlation analysis was used to analyze the correlation between changed internetwork connectivities in sFNC and cognitive assessments (including MMSE, MoCA, AVLT-IR, AVLT-DR, TMB-A, TMT-B, Stroop-A, Stroop-B, Stroop-C, and CDT scores) , and dynamic temporal properties (fractional occupancy and mean dwell time in each state, and the number of transitions) and cognitive assessments; controlling for age, gender, and education. SPSS 26.0 was used for statistical analysis with p < 0.05 as the threshold. The Chi-squared (χ2) test was used for categorical data, while the two-sample t-test was employed for comparisons between continuous variables. The processing flowchart is shown in Fig. 6.
The processing flowchart of functional MRI data analysis. (A) All patient data are concatenated in time and ICA analysis is done to identify Resting-State Networks (RSN) spatial maps. Patient-specific time courses of each RSN are estimated using dual regression (image generated using GroupICATv4.0b, GitHub: https://github.com/trendscenter/gift). (B) sFNC analysis done by calculating the correlation between each pair of RSNs using the entire time course. (C) dFNC was analyzed using sliding window approach and K-means clustering. (D) Correlation analysis of dFNC properties and clinical variables was done by linear regression.
Data availability
The datasets produced and/or analyzed in this study are accessible through the corresponding author. Access is restricted to academic purposes and requires a data transfer agreement as well as approval from the Ethics Committee.
References
Hosoki, S. et al. Molecular biomarkers for vascular cognitive impairment and dementia. Nat. Rev. Neurol. 19, 737–753 (2023).
Duering, M. et al. Neuroimaging standards for research into small vessel disease-advances since 2013. Lancet Neurol. 22, 602–618 (2023).
Kim, J. et al. Distinct spatiotemporal patterns of cortical thinning in Alzheimer’s disease-type cognitive impairment and subcortical vascular cognitive impairment. Commun. Biol. 7, 198 (2024).
Román, G. C., Erkinjuntti, T., Wallin, A., Pantoni, L. & Chui, H. C. Subcortical ischaemic vascular dementia. Lancet Neurol. 1, 426–436 (2002).
Kang, S. H. et al. Independent effects of amyloid and vascular markers on long-term functional outcomes: An 8-year longitudinal study of subcortical vascular cognitive impairment. Eur. J. Neurol. 29, 413–421 (2022).
Lee, J.-Y. et al. Optical coherence tomography angiography as a potential screening tool for cerebral small vessel diseases. Alzheimers Res. Ther. 12, 73 (2020).
Kalaria, R. N. & Erkinjuntti, T. Small vessel disease and subcortical vascular dementia. J. Clin. Neurol. 2, 1 (2006).
Du, J. & Xu, Q. Neuroimaging studies on cognitive impairment due to cerebral small vessel disease. Stroke Vasc. Neurol. 4, 99 (2019).
Wardlaw, J. M. et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 12, 822–838 (2013).
Jokinen, H. et al. Early-stage white matter lesions detected by multispectral MRI segmentation predict progressive cognitive decline. Front. Neurosci. 9, 455 (2015).
Schmidt, R. et al. White matter lesion progression in LADIS: Frequency, clinical effects, and sample size calculations. Stroke 43, 2643–2647 (2012).
Banerjee, G., Wilson, D., Jäger, H. R. & Werring, D. J. Novel imaging techniques in cerebral small vessel diseases and vascular cognitive impairment. Biochim. Biophys. Acta. 1862, 926–938 (2016).
da Silva, P. H. R. et al. Contrast agent-free state-of-the-art magnetic resonance imaging on cerebral small vessel disease—Part 2: Diffusion tensor imaging and functional magnetic resonance imaging. NMR Biomed. 35, e4743 (2022).
Pasi, M., van Uden, I. W. M., Tuladhar, A. M., de Leeuw, F.-E. & Pantoni, L. White matter microstructural damage on diffusion tensor imaging in cerebral small vessel disease: Clinical consequences. Stroke 47, 1679–1684 (2016).
Petersen, M. et al. Network localisation of white matter damage in cerebral small vessel disease. Sci. Rep. 10, 9210 (2020).
de Schotten Thiebaut, M. & Forkel, S. J. The emergent properties of the connected brain. Science 378, 505–510 (2022).
Passingham, R. E., Stephan, K. E. & Kötter, R. The anatomical basis of functional localization in the cortex. Nat. Rev. Neurosci. 3, 606–616 (2002).
Papma, J. M. et al. The influence of cerebral small vessel disease on default mode network deactivation in mild cognitive impairment. Neuroimage Clin. 2, 33–42 (2012).
Liu, R. et al. Distinctive and pervasive alterations of functional brain networks in cerebral small vessel disease with and without cognitive impairment. Dement. Geriatr. Cogn. Disord. 47, 55–67 (2019).
Delamillieure, P. et al. The resting state questionnaire: An introspective questionnaire for evaluation of inner experience during the conscious resting state. Brain Res. Bull. 81, 565–573 (2010).
Kucyi, A. & Davis, K. D. Dynamic functional connectivity of the default mode network tracks daydreaming. Neuroimage 100, 471–480 (2014).
Hutchison, R. M. et al. Dynamic functional connectivity: Promise, issues, and interpretations. Neuroimage 80, 360–378 (2013).
Damaraju, E. et al. Dynamic functional connectivity analysis reveals transient states of dysconnectivity in schizophrenia. Neuroimage Clin. 5, 298–308 (2014).
Tu, Y. et al. Abnormal thalamocortical network dynamics in migraine. Neurology 92, e2706–e2716 (2019).
Li, K. et al. The influence of cerebral small vessel disease on static and dynamic functional network connectivity in subjects along Alzheimer’s disease continuum. Brain Connect. 11, 189–200 (2021).
Chen, F. et al. Alterations in dynamic functional connectivity in patients with cerebral small vessel disease. Transl. Stroke Res. 15, 580–590 (2024).
Huang, C. et al. Altered dynamic functional network connectivity and topological organization variance in patients with white matter hyperintensities. J. Neurosci. Res. 101, 1711–1727 (2023).
Damoiseaux, J. S. et al. Consistent resting-state networks across healthy subjects. Proc. Natl. Acad. Sci. U. S. A. 103, 13848–13853 (2006).
Qu, J. et al. Aberrant dynamic functional network connectivity in progressive supranuclear palsy. Neurobiol. Dis. 195, 106493 (2024).
Park, D. C. & Reuter-Lorenz, P. The adaptive brain: Aging and neurocognitive scaffolding. Annu. Rev. Psychol. 60, 173–196 (2009).
Wei, X. et al. Internetwork connectivity predicts cognitive decline in Parkinson’s and is altered by genetic variants. Front. Aging Neurosci. 14, 853029 (2022).
Jiang, L. et al. Multimodal covariance network reflects individual cognitive flexibility. Int. J. Neural Syst. 34, 2450018 (2024).
Li, Y. et al. Structural and functional alterations in cerebral small vessel disease: An ALE-based meta-analysis. Cereb. Cortex. 33, 5484 (2022).
Cooray, G. K., Sundgren, M. & Brismar, T. Mechanism of visual network dysfunction in relapsing-remitting multiple sclerosis and its relation to cognition. Clin. Neurophysiol. 131, 361–367 (2020).
Hou, Y. et al. Different resting-state network disruptions in newly diagnosed drug-naïve Parkinson’s disease patients with mild cognitive impairment. BMC Neurol. 21, 327 (2021).
Zhou, X. et al. Disrupted dynamic network attribution associated with gait disorder in cerebral small vessel disease. Brain Connect. 14, 327–339 (2024).
Li, F. et al. Altered static and dynamic functional network connectivity in post-traumatic headache. J. Headache Pain. 22, 137 (2021).
Schulz, M., Malherbe, C., Cheng, B., Thomalla, G. & Schlemm, E. Functional connectivity changes in cerebral small vessel disease—A systematic review of the resting-state MRI literature. BMC Med. 19, 103 (2021).
Menon, V. & Uddin, L. Q. Saliency, switching, attention and control: a network model of insula function. Brain Struct. Funct. 214, 655–667 (2010).
Greicius, M. D. & Kimmel, D. L. Neuroimaging insights into network-based neurodegeneration. Curr. Opin. Neurol. 25, 727–734 (2012).
Zeng, S. et al. Dynamic functional network connectivity in patients with a mismatch between white matter hyperintensity and cognitive function. Front. Aging Neurosci. 16, 1418173 (2024).
Kwon, H.-M. et al. Frequency, risk factors, and outcome of coexistent small vessel disease and intracranial arterial stenosis: Results from the stenting and aggressive medical management for preventing recurrent stroke in intracranial stenosis (SAMMPRIS) trial. JAMA Neurol. 73, 36–42 (2016).
Neumann-Haefelin, T. et al. Leukoaraiosis is a risk factor for symptomatic intracerebral hemorrhage after thrombolysis for acute stroke. Stroke 37, 2463–2466 (2006).
Du, J. et al. Structural brain network disruption at preclinical stage of cognitive impairment due to cerebral small vessel disease. Neuroscience 449, 99 (2020).
Sachdev, P. S. et al. Classifying neurocognitive disorders: The DSM-5 approach. Nat. Rev. Neurol. 10, 634–642 (2014).
Friston, K. J., Williams, S., Howard, R., Frackowiak, R. S. & Turner, R. Movement-related effects in fMRI time-series. Magn. Reson. Med. 35, 346–355 (1996).
Ashburner, J. A fast diffeomorphic image registration algorithm. Neuroimage 38, 95 (2007).
Cai, H. et al. Large-scale functional network connectivity mediate the associations of gut microbiota with sleep quality and executive functions. Hum. Brain Mapp. 42, 3088–3101 (2021).
Zhu, J. et al. Transcriptomic decoding of regional cortical vulnerability to major depressive disorder. Commun. Biol. 7, 960 (2024).
Du, Y. & Fan, Y. Group information guided ICA for fMRI data analysis. Neuroimage 69, 157–197 (2013).
Allen, E. A. et al. A baseline for the multivariate comparison of resting-state networks. Front. Syst. Neurosci. 5, 2 (2011).
Jung, J. et al. Alterations in functional brain networks in depressed patients with a suicide attempt history. Neuropsychopharmacology 45, 964–974 (2020).
Yao, W., Zhou, H., Zhang, X., Chen, H. & Bai, F. Inflammation affects dynamic functional network connectivity pattern changes via plasma NFL in cognitive impairment patients. CNS Neurosci. Ther. 30, e14391 (2024).
Glickman, M. E., Rao, S. R. & Schultz, M. R. False discovery rate control is a recommended alternative to Bonferroni-type adjustments in health studies. J. Clin. Epidemiol. 67, 850–857 (2014).
Allen, E. A. et al. Tracking whole-brain connectivity dynamics in the resting state. Cereb. Cortex. 24, 663–676 (2014).
Faghiri, A., Stephen, J. M., Wang, Y.-P., Wilson, T. W. & Calhoun, V. D. Changing brain connectivity dynamics: From early childhood to adulthood. Hum. Brain Mapp. 39, 1108–1117 (2018).
Acknowledgements
We thank all participants in the present study for their co-operation.
Funding
This study was funded by Wuxi Municipal Health Commission General Project (Grant No. M202421) and the Medical Expert Team Program of Wuxi Taihu Talent Plan 2021 (2021THRC-TF-YXYXK).
Author information
Authors and Affiliations
Contributions
HM: study concept, individual recruit, data analysis, statistics, and article writing. YS: article writing, evaluation of neuropsychological scale, and data analysis. QG: MRI imaging data analysis and evaluation of neuropsychological scale. MX: individual recruit and brain MRI imaging scanning. XH: individual recruit and CSVD markers reading. FW: study guidance. XF: study concept and guidance. All authors have reviewed and approved the submitted version of the manuscript. All authors have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mao, H., Shi, Y., Gao, Q. et al. Alterations in static and dynamic functional network connectivity in subcortical vascular cognitive impairment. Sci Rep 15, 22113 (2025). https://doi.org/10.1038/s41598-025-06640-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06640-3