Abstract
Minimally invasive therapeutic procedures have been applied for the management of degenerative joint disease in the temporomandibular joint (TMJ). This study describes a modified technique of arthrocentesis with concentric needle and cannula in the TMJ associated with viscosupplementation and/or orthobiologics. Its effects were evaluated based on clinical outcomes related to pain, mouth opening, and joint sound, along with longitudinal tomographic evaluation based on the Wilkes classification. A prospective study was conducted with 22 patients (44 TMJs) undergoing arthrocentesis complemented by ultrasonography. The technique allowed effective lavage followed by infiltration into both the upper and lower compartments, using therapeutic agents selected based on the stage of articular temporomandibular disorder (TMD) according to the Wilkes classification. Clinical and tomographic assessments were performed before and after treatment, with follow-up ranging from 12 to 14 months. Significant improvements in pain outcomes (p < 0.001) and mouth opening amplitude (p < 0.001) were observed in all patients. There were no significant changes in joint sound post-treatment. The Wilkes classification revealed a reduction in degenerative stages in both the right (p = 0.003) and the left (p = 0.007) TMJs. The modified arthrocentesis technique combined with viscosupplementation and/or orthobiologics (platelet-rich fibrin) has been shown to be effective in reducing pain and improving TMJ function, suggesting a minimally invasive and safe approach for managing advanced articular TMDs. Future studies are recommended to confirm its applicability in different populations and in individuals with vary stages of TMD.
Similar content being viewed by others
Introduction
Temporomandibular disorders (TMDs) are characterized by a set of conditions classified into two main categories, namely, muscular or articular disorders1,2. Among TMDs of articular origin, the most prevalent are disc displacement with or without reduction (19.1%) and degenerative joint disease (DJD) (9.8%)3.
There is an estimated high risk of DJD in patients with articular disc displacement with and without reduction4,5. This chronic degenerative disease affects the fibrocartilage covering the articular surfaces and the underlying subchondral bone, causing chondrocyte death, degradation of the extracellular matrix and bone remodeling6,7.
Painful conditions usually manifest in patients with more advanced stages of DJD, which makes early diagnosis difficult and highlights the importance of a detailed anamnesis and confirmatory complementary tests2,6 .On imaging exams, DJD presents as subchondral cysts, erosive lesions, osteophytes and/or generalized sclerosis. Subcortical flattening and sclerosis are not considered determinants for the occurrence of DJD but may be precursors1,6,8.
Therapeutic strategies that not only provide symptomatic relief and biomechanical gain but also aim to repair the joint structures degraded by DJD have been the subject of great interest5. From this perspective, treatment should stabilize the progression of the DJD, control painful conditions, restore joint biomechanics and, whenever possible, promote tissue regeneration or repair6,9. Based on the Wilkes classification, which is recommended for describing and classifying structural alterations in the joint environment, it is possible to establish an appropriate clinical rationale for the stage of tissue alterations, considering the level of pain and changes in biomechanics5.
Minimally invasive therapeutic procedures have been used to control DJD. These include arthrocentesis, which can be complemented by viscosupplementation, i.e., intra-articular application of hyaluronic acid solutions, or orthobiological agents such as platelet-rich plasma (PRP) and fibrin-rich plasma (PRF). When performed alone or in combination, these procedures have shown promising results7,8,10,11,12.
In this context, arthrocentesis, which aims to remove inflammatory mediators and free debris from the joint environment, breaks up joint adhesions and thus relieves painful symptoms and promotes mandibular mobility, plays a strategic role in minimally invasive therapies13. Arthrocentesis has been the primary choice for preparing the joint environment, sometimes in combination with viscosupplementation (VS) and/or orthobiologics (OB), enhancing the results for DJD control, pain reduction, improved mouth opening and structural gain7,10.
Although the classic double-puncture technique is widely used for the upper compartment, new methods have been proposed to increase efficacy, safety and patient comfort. In 201114, proposed a simplified and economical solution using concentric needles to perform irrigation and drainage in a single puncture. The authors15 evaluated a modification of the classic technique, replacing the needle with a cannula to reduce intra-articular trauma.
Therefore, this study aims to present an innovative minimally invasive arthrocentesis technique in which a single-access puncture is made for each joint compartment, through which a concentric needle and cannula are introduced. By reducing the number of access ports commonly used in the traditional technique, the aim is to increase the procedure’s predictability, simplify its execution, increase its safety and reduce morbidity and immediate postoperative discomfort without compromising the therapeutic objectives.
Arthrocentesis is carried out in the first part of the treatment cycle, prior to the first therapeutic infiltration of VS and/or OB. The sequential infiltrations will be carried out at monthly intervals (sequential protocol for the upper and lower compartments) according to the stage of degeneration. In addition, the aim of this study was to evaluate the tomographic effects using the Wilkes classification and the clinical effects related to pain, mouth opening and joint sound following use of this modified arthrocentesis technique complemented by VS and/or OB.
Results
Participant flow
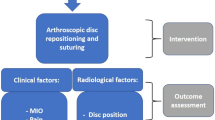
A total of 22 patients (20 women and 2 men) with indications for arthrocentesis were assessed, and all patients were eligible for the study, totaling 44 temporomandibular joints (TMJs). All participants signed an informed consent form and were allocated to receive the intervention according to the degree of degeneration of their TMJs. On the right side, 19 patients received VS and 3 received OB (PRF) in the upper compartment, whereas in the lower compartment, 10 received VS and 12 received OB (PRF). On the left side, 20 patients received VS and 2 received OB (PRF) in the upper compartment, whereas in the lower compartment, 11 received VS and 11 received OB (PRF) (Fig. 1).
All information on patient characteristics and treatment received can be found in (Tables 1 and 2).
Outcomes and estimation
Osseous changes - Wilkes classification based on tomographic evaluation
Table 3 presents the Wilkes classification for the right TMJ in the postoperative period compared with the preoperative classifications. A varied distribution among the Wilkes stages was observed, with significant changes (p = 0.003), as identified by the marginal homogeneity test for paired samples.
Table 4 shows the Wilkes classification for the left TMJ in the postoperative period compared with the preoperative classifications. A varied distribution was observed between the Wilkes stages, with significant changes (p = 0.007), as identified by the marginal homogeneity test for paired samples.
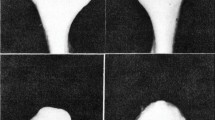
In the Fig. 2 the sagittal and coronal oblique computerized tomography (CB) scans demonstrate significant morphological changes in the mandibular head after the procedure. In the preoperative assessment (Wilkes Stage IV), bone resorption and the absence of cortical bone lining on the mandibular head surface are observed (red arrows). One year after treatment (Wilkes Stage I), a continuous cortical bone lining can be seen around the mandibular head (green arrows), indicating a process of bone remodeling and repair. These changes are evident in both sagittal and coronal oblique views, suggesting the effectiveness of the procedure in restoring the osseous integrity of the temporomandibular joint.
When the Wilkes classification was assessed continuously, there was a significant reduction in the score of the group assessed for both the right TMJ (p = 0.001) and the left TMJ (p = 0.002) (Table 5).
Mouth opening
Figure 3 shows the average variation in mouth opening in millimeters, with the standard deviation. There was a significant increase in mouth opening amplitude for all participants (p < 0.001).
Arthralgia
There were significant differences in the pre- and postoperative values for all participants (p < 0.001), with average pain scores of 2.2 (± 1.1) preoperatively and 0 (± 0.0) postoperatively. There were also significant differences between patients with right TMJ Stages IV (p = 0.011) and V (p = 0.010). There were significant differences in the left TMJ in the pre- and postoperative values for all participants (p < 0.001), with average pain scores of 2.0 (± 1.1) preoperatively and 0 (± 0.0) postoperatively. There were also significant differences between patients with left TMJ Stages IV (p = 0.011) and V (p = 0.010) according to Wilkes’ classification (Fig. 4).
Joint sound
The joint sounds observed in the patients were clinically characterized according to the research diagnostic criteria for TMD (RDC/TMD)2. The sounds showed characteristics compatible with articular disc displacement, both with and without reduction, whether or not they were associated with movement limitation. However, none of the patients presented with joint sound compatible with crepitus, which is characteristic of more advanced degenerative conditions.
No statistically significant differences were found with regard to the presence or absence of joint sound for either the right (p = 0.453) or left (p = 0.375) TMJ.
Adverse events
In this study, only 1 case of mild postoperative arthralgia was reported.
Discussion
Degenerative joint disease has a significant negative impact on patients’ quality of life since it is related to pain, impairment of mandibular function, and addiction to joint noise16. Its treatment is focused on stabilizing the progression of the disease, controlling pain, restoring joint biomechanics and promoting tissue repair6,9.
Minimally invasive therapies that promote pain relief, improve biomechanics (range of movement) and repair joint structures have been the subject of great scientific interest17. These techniques have gained ground as therapeutic options for the treatment of TMD, promoting significant improvements in the joint environment. Among these therapies, arthrocentesis and intra-articular application of VS and/or OB stand out as safe options with a low risk of complications18,19,20.
This study proposes an innovative arthrocentesis technique with a concentric needle and cannula, allowing effective access to both the upper and lower joint compartments, with a single puncture for each compartment. This approach reduces injuries to joint structures, minimizing postoperative morbidity and allowing rapid recovery of joint biomechanics21. The results confirmed expectations, showing improvements in joint pain, mouth opening amplitude and osseous changes.
All the patients in this study showed an improvement in joint pain, reaching a pain level of 0. Arthrocentesis provides a “washout” of the joint, which removes metabolites and inflammatory mediators present in the joint cavity, such as the proinflammatory cytokines IL-1β and TNF-α, known to be associated with chronic pain and inflammation22. This joint flushing mechanism can reduce the inflammatory effect and, consequently, the pain experienced by patients. In addition, studies suggest that the mechanical expansion of joint structures during the injection procedure and flushing of the joint environment can help restore mobility and reduce joint overload, as well as improve the range of motion by reducing adhesions and relieving intra-articular mechanical tension18,19,20. These findings reinforce the relevance of arthrocentesis in the management of TMD, providing patients with less pain and functional relief, which has a positive impact on their quality of life, functional capacity and treatment adherence.
The therapeutic strategy of applying arthrocentesis prior to the clinical rationale proved to be important in promoting improvements in the joint environment. In addition to providing relief from painful symptoms and increasing mandibular mobility, the breaking up of adhesions and removal of inflammatory mediators and free debris circulating in the joint environment allow for more effective direct action of the agents injected into the joint surface, be it sodium hyaluronate (SH) or blood products, especially PRF13,23. The washing of inflammatory mediators and free radicals contributes to the stability of the injected solutions used in VS and OB, resulting in an extended intra-articular residence time and, consequently, enhanced effects.
Current studies suggest that minimally invasive therapies be instituted as early as possible, especially when patients do not respond well to conservative treatment. This clinical approach has been increasingly used, as early-stage DJD has a better prognosis24,25.
SH injections have shown significant promise in the treatment of TMD. Research highlights the efficacy and safety of SH for managing various TMDs, including disc displacement, osteoarthritis, and degenerative joint disease26. Intra-articular SH injections have demonstrated substantial improvements in pain, joint sounds, and clinical dysfunction in patients with reduced disc displacement, surpassing placebo treatments27. Compared with conventional bite-plane therapy, SH injections offer comparable long-term outcomes with better patient tolerability28. Additionally, a long-term study comparing SH injections to corticosteroid injections revealed that both treatments effectively alleviate symptoms and enhance bite force in patients with chronic TMD-related arthritis, with SH emerging as a potentially preferable option due to its favorable side effect profile29. The structural improvements observed in Wilkes stages I, II, and III, which are characterized by initial lesions where the drug’s target site is the fibrocartilage, are consistent with findings reported in the literature and underscore the potential of SH as a safe and effective therapeutic option for a range of TMDs.
Intra-articular injections of PRF have also shown promising results in improving pain and jaw function in patients with intra-articular TMJ disorders. Studies, including those by Albilia et al.30, Yuce et al.31 and Torul et al.32, have shown that compared with arthrocentesis alone or arthrocentesis with SH, PRF significantly reduces pain and improves jaw movement. The long-term benefits were highlighted in the follow-ups carried out by Karadayi et al.10 and Ghoneim et al.33, with sustained improvements in pain and function up to 12 months after treatment. The structural improvements observed in patients classified as Wilkes stages IV and V, who presented with more extensive lesions involving the medullary bone, indicate the effectiveness of this drug’s reparative potential.
The decision to apply VS (sodium hyaluronate) or OB (PRF) to each joint compartment (upper and lower) was based on the stage of the disease, as assessed by tomography and Wilkes classification5. Although the original classification is based on magnetic resonance imaging (MRI) and computed tomography scans, cone-beam computed tomography (CBCT) is considered the appropriate test for determining the stage of the disease, as it allows clearer and more detailed visualization of the condition of the articular bone structures, such as the cortical and medullary bone of the head of the mandible and temporal components. The detailed identification of the lesions, considering their exact location and extent, allowed for the development of an individualized treatment plan for each patient, tailoring the most appropriate therapy for each compartment according to the type of lesion present. The comparative analysis of pre- and posttreatment CBCT images confirmed the ability of this technique to assess the progression of the disease and the therapeutic results, revealing signs of tissue repair, including the medular bone aspect.
The safety and ease allowed by the proposed technique are based on clinical demarcation of the access points to the upper and lower joint compartments, based on the use of clinically identifiable points, with local anesthesia, which enables it to be performed on an outpatient basis21. In addition to accurately checking the condition of the articular surfaces, prior assessment and planning using a high-resolution CBCT scan make it possible to carry out safety measures to control the depth of needle penetration, preventing the capsule from being trepanned medially in the parapharyngeal space34 and further enhancing patient safety care.
Notably, it is an easy procedure performed under local anesthesia with low morbidity, as demonstrated by the absence of postoperative edema and pain reported by the treated patients, and can be performed in a clinical setting without the need for sedation or general anesthesia. These aspects promote a positive effect of increasing patient adherence to treatment, which is highly important, especially when the clinical rationale requires a sequence of infiltrations21.
An aspect of great relevance regarding the marking of the access ports, observed during the in vivo stage, is that in cases of anatomical variation in the positioning of the ear, when the positioning of the tragus does not coincide with the preauricular depression, point 1 of the technique described here should be marked considering the uppermost region of the articular fossa in order to compensate for this variation in the facial phenotype. The correction of this marking can be verified using ultrasound to locate the lateral pole of the mandibular head in relation to point 4. This adaptation should be considered in all situations of facial phenotype variation.
The use of a concentric needle and cannula in arthrocentesis allows precise checking of the location of the instruments in the articular compartments, particularly when accessing the lower compartment, where “double-checking” of lateral bone contact is carried out to ensure safe positioning. The blunt tip of the cannula helps avoid injury to the articular structures while offering an additional tactile check for ultrasound guidance, increasing precision and reducing risks during the procedure14,21.
The prior knowledge of the lateromedial dimension of the mandibular condyle provided by CBCT, in addition to the ultrasonographic measurement of the soft tissue thickness adjacent to the lateral pole of the condyle, enabled precise control of instrument depth, establishing a safety margin that prevents medial perforation of the joint into the parapharyngeal region. The 70 mm cannula with a blunt tip has a lateral irrigation hole and markings every 10 mm, which allow the operator to adjust the positioning according to prior planning, promoting lateral or depth-controlled movements within the intra-articular space. This versatile design allows for greater predictability and safety, optimizing the control and effectiveness of arthrocentesis for safer and more precise clinical results. These technical features contribute to a lower morbidity, minimally invasive intervention with greater therapeutic benefit, in line with the demand for safe and effective procedures in patients with TMD14,21.
The results of tomographic evaluation revealed a pattern of regression in the degenerative condition of the right TMJ during the postoperative period. There was progressive repair of the cortex at the sites of the initial lesions, characterized as open lesions, as well as an increase in cortical density and improvement in the sclerosis of the medullary bone and its trabeculae, suggesting a positive response to the procedure performed. There were some cases in which, after the procedure, there was no regression of the Wilkes classification; however, it is possible to see a reduction in the lesions, which is why we decided to carry out an evaluation using continuous data, where the results significantly improved, reinforcing the importance of using both categorical and continuous classification methods to capture nuances in the therapeutic response. This approach offers a more detailed view of the effects on the recovery of the treated temporomandibular joints, allowing for a more comprehensive and accurate assessment of therapeutic success.
With respect to joint sound, the effectiveness of arthrocentesis varies across studies, with some reporting significant improvements35,36 and others reporting no significant changes37. Polat & Yanik, 202036 reported that arthrocentesis significantly reduced joint sound in the short term, suggesting that the procedure favors the elimination of adhesions and the normalization of synovial fluid viscosity, reducing friction between joint surfaces. On the other hand, Alpaslan & Alpaslan35 reported that, in addition to conventional arthrocentesis, the injection of hyaluronic acid intensified the reduction in joint sound, especially in patients with joint locking, due to the lubricating and protective properties of hyaluronic acid on the articular cartilage.
Although the technique has been effective in various aspects of TMD management, no difference was found regarding joint sound after treatment, indicating that it may not be sufficient to eliminate joint noise. This finding suggests that disc displacement and/or changes in joint surfaces are not directly resolved by arthrocentesis. Notably, in the majority of patients, joint noise is related to disc displacement but not crepitus, which is more related to degenerative processes of the TMJ. Arthrocentesis can help release adhesions between the articular disc and the mandibular fossa, which can improve mobility and the circulation of synovial fluid but does not guarantee the total elimination of joint sounds.
Another important highlight of this study was the use of ultrasonography to verify the correct position of the needle tip in the lateral pole of the mandibular head in images with good resolution that were generated in real time. In addition, the use of ultrasound was also important for planning procedures, as it enabled vascular mapping, measurement of the thickness of the soft tissues to be punctured and measurement of the thickness of the joint capsule21,38. During the transoperative period, ultrasonography made it possible to validate the correct positioning of the instruments, especially in the access port to the lower compartment, which made the procedure more reassuring and assertive. Although the procedure was highly reproducible, with easy clinical identification of the anatomical reference points for accessing the joint compartments, ultrasonography provided greater security21,38,39.
This innovative modified concentric needle-and-cannula arthrocentesis technique offers significant advantages, including low morbidity, minimal or no facial edema after the procedure, rapid postoperative recovery, improved joint function and reduction in painful symptoms, and it is easily complemented by other minimally invasive techniques, such as viscosupplementation with HA and OB (PRF), making it a good therapeutic option among minimally invasive interventions for treating patients with TMDs.
As a highly relevant aspect of the study, this technique is innovative, as it introduces a modified arthrocentesis technique with a concentric needle and cannula that simplifies the procedure and potentially increases its safety and efficacy, providing its comprehensive methodology and demonstrating that its use with ultrasonography guidance increases the accuracy and safety of the procedure. Some limitations of the study should also be mentioned, such as the sample size, which may limit the generalizability of the results, and the lack of a control group.
Conclusion
The modified arthrocentesis technique with concentric needle and cannula for the treatment of articular TMD has proven to be a promising and minimally invasive alternative, with clear benefits in pain reduction and improved joint function. Complementation by viscosupplementation and/or orthobiologics, adjusted to the stage of joint degeneration, enhanced the therapeutic effects, especially in patients with advanced degeneration, as evidenced by improvements in Wilkes classification and mouth opening amplitude. The use of ultrasonography during the procedure, combined with the marking of access ports, made it possible to use only one access port for the procedure for each compartment, which added safety and precision, increased the effectiveness of the treatment and minimized morbidity. The results of this study are very promising, even with a relatively small sample, suggesting the need for further research to validate the technique in different contexts and populations and to assess its long-term effectiveness.
Methods
Participants
A prospective clinical study was conducted with 12 to 14 months of follow-up. The report of this study follows the TREND statement40 (Appendix 1). The study was approved by the ethics committees of the Federal University of Minas Gerais (CAAE: 53014921.5.0000.5149) and Mater Dei Hospital (CAAE: 86451425.6.0000.5128). This study followed the Declaration of Helsinki, and all methods were carried out in accordance with the relevant guidelines and regulations. All patients provided written informed consent after being oriented to the procedure.
The technical procedures for accessing the upper and lower compartments of the TMJs were based on the technique recommended by21. The referred study was carried out on 20 TMJs from 10 fresh-frozen cadaver heads made available by the Morphology Department of the Institute of Biological Sciences at the Federal University of Minas Gerais. Additionally, in the same study, the technique was applied to 10 patients (20 temporomandibular joints), and the location of the lower and upper compartments was confirmed via ultrasound.
In the present study, the procedures were performed on 22 patients (44 TMJs) seen at the School Clinic of the Mater Dei Private Hospital in Minas Gerais, Belo Horizonte, Brazil, between May and June 2023. The sample size is consistent with current literature41. Patients were selected according to the following inclusion and exclusion criteria:
Inclusion criteria: volunteer patients aged 18 years or older with a diagnosis of DJD according to the DC/TMD criteria2, with clinical and imaging indications for arthrocentesis with complementary VS and/or OB application. All patients underwent MRI and CBCT for the classification of TMJ conditions according to the Wilkes staging system. The MRI was also employed to ensure the absence of communication between the articular compartments, which could result from disc perforation or ligamentous injury. Only patients presenting with a clear separation between the superior and inferior joint compartments were included in the study.
The classic Wilkes classification takes into account computed tomography and magnetic resonance imaging assessments. In this study, the tomographic classification was used for the choice of treatment and evaluating the progression of degenerative joint lesions. Treatment planning was undertaken based on the Wilkes classification in the following stages: I, II, III, IV or V. Cone beam computed tomography scans of each patient were used to verify the anatomical conditions of the articular structures, confirm the clinical diagnosis of DJD, and measure the lateromedial extension of the mandibular heads. The scans were carried out on a cone beam computed tomography scanner (Morita Veraview X800® J. Morita. Kyoto/Japan; 7.9 mA, 101 kV; Voxel size 0.8 mm: FOV: 40 mm × 40 mm).
Patients with Wilkes Stages I, II and III, which present integrity of the cortical bone of the mandibular head, or even loss of bone density, promoting a “smokiness” of this articular component, as well as the mandibular fossa (component of the temporal bone), were selected to receive VS with sodium hyaluronate as a treatment associated with arthrocentesis.
Patients with Wilkes Stages IV and V, which show loss of integrity of the cortical bone of the mandibular head and/or the cortical bone of the articular fossa, with exposure of the medullary bone, were selected to receive OB (PRF) as a treatment associated with arthrocentesis. Intra-articular infiltration of OB has been used to control DJD. In this case, the use of leukocytes and PRF stands out. PRF acts as a temporary structuring framework with high adhesiveness, which allows it to protect growth factors from concentrated platelets. It also helps to restore joint rheology, normalize endogenous HA synthesis and induce osteochondral regeneration, combined with anti-inflammatory, analgesic and antibacterial properties33,42,43.
The infiltration of exogenous hyaluronic acid (sodium hyaluronate) directly into the intra-articular space aims to restore the properties of the synovial fluid26,44. In addition, depending on the characteristics of the viscosupplement used, it can stimulate the secretion of endogenous hyaluronic acid (viscoinduction)26,44 and have anti-inflammatory26,45, analgesic26,44 and chondroprotective46,47 effects, although demonstrating the magnitude of this effect specifically for the temporomandibular joint requires clinical studies dedicated to this purpose.
Exclusion criteria
Autoimmune disease, benign or malignant lesions in the TMJ, neurological disorders, blood dyscrasias, pregnancy, or a history including having recently undergone similar techniques.
Interventions
All injections were carried out by the same professional (E.J.). The technique for accessing the upper and lower compartments was previously described by Januzzi et al. (2022)21. The procedures for performing concentric needle-and-cannula arthrocentesis were carried out according to the following steps (Fig. 5):
-
1.
1. Marking the access ports: The entry points for access to the joint compartments were identified (Fig. 5a).
-
2.
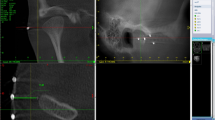
2. Prior ultrasonography assessment: A portable ultrasound with a linear transducer (Dominus®; 12.5–20 MHz; Alfamed Sistemas Médicos, Lagoa Santa, Brazil) was used to map the vascularization of the region in order to avoid vascular complications, followed by measurement of the thickness of the soft tissues (from the skin to the PLCM) and measurement of the thickness of the joint capsule (Fig. 5b).
-
3.
3. Tomographic measurement: The lateral–medial extension of the mandibular heads was evaluated by tomography (Fig. 5c).
-
4.
4. Antisepsis: The preauricular area was cleaned with 2% chlorhexidine digluconate solution (Riohex® - Indústria Farmacêutica Rioquímica LTDA - São José do Rio Preto - SP) (Fig. 5d).
-
5.
5. Anesthesia of the auriculotemporal nerve: With the patient’s mouth closed, anesthetic was administered using a vasoconstrictor (Alphacaine 2% 1:100,000 - DFL). When necessary, complementary intra-articular anesthesia was performed (Fig. 5e).
-
6.
6. Positioning of the safety cursor: An 18G needle with a cursor was used to limit the penetration depth, preventing the needle from advancing too far (lower compartment) (Fig. 5f).
-
7.
7. Needle insertion: An 18G needle was inserted into the access door to the lower compartment (Point 4) with the bevel facing the skin, in an inferosuperior direction, at 45° to the skin surface until it met resistance corresponding to the needle tip touching the lateral pole of the head of the mandible. At this point, the correct positioning of the needle was checked by ultrasound in the longitudinal protocol (Fig. 5g).
-
8.
8. Positioning the cannula: A 25G/70 mm cannula was inserted inside the 18G needle positioned next to the lateral pole of the head of the mandible until resistance was met (double-checking bone contact). Importantly, the red marking on the cannula barrel faced the skin in the same direction as the needle bevel so that the cannula exit hole was free and not obliterated by the closed portion of the needle tip, allowing good circulation of the irrigation fluid and effective washing of the joint environment (Fig. 5h, 5i).
-
9.
9. Connecting a syringe and starting the lavage: A 20 ml disposable sterile syringe (Luer Lock 20 ml - BD) was connected to the concentric needle and cannula set, with the aid of a PVC extender (Extensionfix 20 cm - Braun), loaded with saline solution, followed by certification that the saline solution was effectively circulated in the circuit in order to start the lavage of the joint environment (Fig. 5i).
-
10.
10. Adjusting the depth of penetration of the needle and cannula: A delicate maneuver was performed to pull back the bevel of the needle to allow it to be introduced into the posterior recess of the lower compartment of the TMJ, next to the posterior surface of the mandibular head. The depth of penetration must comply with the previous limitation of the cursor (a safety measure) so that the concentric cannula and needle assembly can reach half of the lateral-medial extension of the mandibular head, with the tip of the cannula introduced no more than 5 to 10 mm beyond the tip of the needle bevel maximum. Notably, the total penetration of the concentric needle and cannula set, with the tip of the cannula extending beyond the tip of the needle, was determined beforehand by measuring the thickness of the soft tissue to be punctured, plus half the measurement of the lateral-medial extension of the head of the mandible (measurement taken by the initial computed tomography scan prior examination). This limitation of the cursor prevented the capsule from being trepanned medially in the parapharyngeal space, which is a safety measure (determined in Items 2 and 3). Tactile certification of the correct position of the needle ensured that it was not in contact with the lateral pole of the head of the mandible (Fig. 5j, k) (Appendix 2).
-
11.
11. Irrigation of the lower compartment: A physiological solution circulation was established to wash the lower joint environment, starting with gentle irrigation and observation of the skin surface to ensure that there was no increase in volume in the preauricular region, indicating extracapsular injection. This was followed by a gradual increase in pressure to circulate 40 ml48 of saline solution throughout the joint environment, promoting effective lysis of possible adhesions, as well as effective washing of the lower joint space, removing debris and inflammatory mediators (Fig. 5l).
-
12.
12. Removal of the cannula and aspiration: After washing, the cannula was removed, and the saline solution that remained inside the needle was gently aspirated (Fig. 5m).
-
13.
13. Therapeutic application according to the stage of the disease in each joint compartment: Articular surfaces in patients with Wilkes Stages I, II and III received VS with sodium hyaluronate (Osteonil Mini® and/or Polireumin® - TRB Pharma) (in a sequential protocol, with one infiltration every 4 weeks, according to the clinical rationale initially established) (Tables 1 and 2). Articular surfaces in patients with Stages IV and V, with loss of cortical integrity, received PRF infiltration. In patients receiving OB, PRF was applied and obtained following the protocol described by Albilia et al.42 (in a sequential protocol, with one infiltration every 4 weeks, according to the initial clinical rationale) (Fig. 5n).
-
14.
14. Procedure in the upper compartment: The safety measure was set by positioning the cursor at 20 mm. The 18G needle was inserted at point 01, in a cranial-caudal direction, at angles between 30 and 45 degrees to the medial side, until the tactile sensation of passing through the joint capsule was felt. At this point, the cannula was inserted gently, taking care not to go deeper than the safety measure and avoiding trauma to the retrodiscal tissue (Fig. 5o).
-
15.
15. Washing the upper compartment: Washing was performed with gentle irrigation, and the pressure was gradually increased so that adequate circulation of 60 ml49 the physiological solution throughout the joint environment was established (Fig. 5p).
-
16.
16. Final application of the therapeutic agent: As with the arthrocentesis of the lower compartment, this was followed by removal of the cannula, aspiration of the remaining serum and infiltration of the agent indicated for the case, either viscosupplementation or orthobiologics (Fig. 5q).
-
17.
17. Postoperative measurement: Immediate ultrasound assessment of the thickness of the joint capsule was doe.
Patients with Wilkes Stages I, II and III received VS with sodium hyaluronate (Osteonil Mini® and/or Polireumin® - TRB Pharma) (in a sequential protocol, with one infiltration every 4 weeks, according to the clinical rationale initially established) (Tables 1 and 2). Articular surfaces in patients with Stages IV and V, with loss of cortical integrity, received PRF infiltration (in a sequential protocol, with one infiltration every 4 weeks, according to the initial clinical rationale) (Tables 1 and 2).
Objectives – hypotheses
To evaluate the tomographic effects of the modified arthrocentesis technique complemented by viscosupplementation or orthobiologics in the TMJ using the Wilkes classification and the clinical effects in relation to pain, mouth opening and joint sound after follow-up.
H0: There are no tomographic changes or differences in pain, mouth opening or joint sound levels between the pre- and postoperative periods 12 to 14 months after the procedure.
H1: There is a regression of tomographic changes and positive differences in pain levels, mouth opening and joint sound between the pre- and postoperative periods 12 to 14 months after the procedure.
Outcomes
Primary outcome
Tomographic changes - Wilkes classification
The tomographic evaluation to determine the stages of joint degeneration according to Wilkes’ classification was performed using cone-beam computed tomography (CBCT) of the TMJs. The images were obtained in customized sagittal and coronal slices, with a slice thickness of 1 mm, allowing detailed visualization of the bony structures of the mandibular head and the articular fossa. The images were analyzed by an experienced radiologist, who classified the TMJs according to Wilkes’ five stages, ranging from initial changes, such as mild bone remodeling, to advanced stages with significant erosion and joint collapse. This classification process followed standardized criteria, including the assessment of aspects such as the shape of the mandibular head, the presence of osteophytes, erosions, and changes in the integrity of the bone cortex. The accuracy and reliability of the diagnosis were enhanced by the use of three-dimensional reconstructions when necessary, providing a comprehensive analysis of the extent of joint degeneration.
New CT images were taken at least 6 to 8 months after the last infiltration cycle.
Arthralgia
The diagnosis of arthralgia was made according to the DC/TMD. It was based on a history of pain in the jaw, temple, ear, or front of the ear and pain modified by jaw movement, function, or parafunction. The physical examination had to meet both of the following criteria: confirmation of pain location in the TMJ(s) area and a report of familiar pain in the TMJ with at least one of the following provocation tests: (a) palpation of the lateral pole or around the lateral pole or (b) maximum unassisted or assisted opening, right or left lateral movements, or protrusive movement(s). Pain levels were measured on a scale from 0 to 3, with 0 indicating no pain and 3 indicating the maximum level of pain.
Secondary outcomes
Maximum mouth opening (MMO)
A single examiner performed all MMO measurements, thus avoiding interexaminer variability. Patients rested their heads against a firm surface in an upright position on the chair and were instructed to open their mouths as wide as possible. The MMO was measured as the distance between the edges of the upper and lower incisor teeth using a digital caliper. Measurements were taken in millimeters before the procedure and during the final follow-up.
Joint sound
The evaluation of TMJ joint sound was performed clinically. Sound, including mouth opening and closing, protrusion, and right and left lateral movements, was recorded during standardized mandibular movements. Each movement was repeated three times to ensure data consistency, and sound was captured in a quiet environment to minimize external interference. Joint sound was classified according to the literature into distinct types (clicks, crepitus, and pops).
Sample size
A convenience sample was obtained from individuals who met the inclusion criteria, agreed to participate in the study, and were available during the data collection period.
Assignment method
Participants were allocated to intervention groups using the Wilkes classification. In the presence of cortical discontinuity, patients were assigned to the PRF group. In the absence of cortical discontinuity, patients were allocated to the VS intervention group using computer-generated simple randomization.
Blinding (masking)
The study was double-blinded, with participants and evaluators blinded to group allocation. Treatments were administered by an independent researcher who was not involved in data collection. An independent researcher, oral and maxillofacial radiologist with 20 years of experience performed the images exams.
Unit of analysis
The unit of analysis proposed in this study was the TMJ, which was categorized as right or left.
Statistical methods
The data are presented as the means and standard deviations (SDs) or absolute (n) and relative (%) frequencies. Data normality was tested using the Shapiro-Wilk test. Paired t tests and Wilcoxon tests were used to compare the mouth opening measurements and Wilkes classification pre- and postoperatively for parametric and nonparametric data, respectively. The McNemar-Bowker and McNemar tests were used to compare changes in the proportions of Wilkes classification and joint sound (present/absent), respectively, before and after the procedure. A statistical significance level of 5% (p < 0.05) was adopted. Statistical analysis was performed using IBM SPSS Statistics software (version 26).
Data availability
Data is provided within the manuscript.
References
De Leeuw, R. & Klasser, G. D. Orofacial pain: guidelines for assessment, diagnosis, and management. Am. J. Orthod. Dentofac. Orthop. 134, 171 (2008).
Schiffman, E. et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J. Oral Facial Pain Headache. 28, 6 (2014).
Valesan, L. F. et al. Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin. Oral Invest. 25, 441–453. https://doi.org/10.1007/s00784-020-03710-w (2021).
Fan, P. et al. Risk Estimation of degenerative joint disease in temporomandibular disorder patients with different types of sagittal and coronal disc displacements: MRI and CBCT analysis. J. Oral Rehabilitation. 50, 12–23. https://doi.org/10.1111/joor.13385 (2023).
Wilkes, C. H. Internal derangements of the temporomandibular joint: pathological variations. Archives Otolaryngology–Head Neck Surg. 115, 469–477 (1989).
Alstergren, P., Pigg, M. & Kopp, S. Clinical diagnosis of temporomandibular joint arthritis. J. Oral Rehabilitation. 45, 269–281. https://doi.org/10.1111/joor.12611 (2018).
Sillmann, Y. M. et al. Intra-articular injection of orthobiologics for temporomandibular joint osteoarthritis: a systematic review of randomized controlled trials. Int. J. Oral Maxillofac. Surg. S0901502725000086. https://doi.org/10.1016/j.ijom.2025.01.008 (2025).
Derwich, M., Mitus-Kenig, M. & Pawlowska, E. Mechanisms of action and efficacy of hyaluronic acid, corticosteroids and platelet-rich plasma in the treatment of temporomandibular joint osteoarthritis—a systematic review. Int. J. Mol. Sci. 22, 7405 (2021).
Bianchi, J. et al. Quantitative bone imaging biomarkers to diagnose temporomandibular joint osteoarthritis. Int. J. Oral Maxillofac. Surg. 50, 227–235 (2021).
Karadayi, U. & Gursoytrak, B. Randomised controlled trial of arthrocentesis with or without PRF for internal derangement of the TMJ. J. Cranio-Maxillofacial Surg. 49, 362–367 (2021).
Nagori, S. A., Gopalakrishnan, V., Rangarajan, H., Kulkarni, V. & Roychoudhury, A. Does intra-articular injection of platelet-rich plasma/platelet-rich fibrin improve outcomes after temporomandibular joint arthrocentesis? A systematic review and meta-analysis. British Journal of Oral and Maxillofacial Surgery (accessed 12 November 2024); https://www.sciencedirect.com/science/article/pii/S0266435624001694?casa_token=L4fSfv3GL5YAAAAA:5YsNNX2zQT0Kfcl4ZpCbK4VbaDNTpD0GInPHoV_GuqiDjY9HTpRLC1rWX9m8hthuY9OFScQuVZOf
Xu, J. et al. Comparative effectiveness of hyaluronic acid, platelet-rich plasma, and platelet-rich fibrin in treating temporomandibular disorders: a systematic review and network meta-analysis. Head Face Med. 19, 39. https://doi.org/10.1186/s13005-023-00369-y (2023).
Machon, V., Hirjak, D. & Lukas, J. Therapy of the osteoarthritis of the temporomandibular joint. J. Cranio-Maxillofacial Surg. 39, 127–130 (2011).
Öreroğlu, A. R., Özkaya, Ö., Öztürk, M. B., Bingöl, D. & Akan, M. Concentric-Needle cannula method for Single-Puncture arthrocentesis in temporomandibular joint disease: an inexpensive and feasible technique. J. Oral Maxillofac. Surg. 69, 2334–2338. https://doi.org/10.1016/j.joms.2011.03.004 (2011).
Grossmann, E. & Poluha, R. L. Comparative study of arthrocentesis with concentric-needle cannula with classic concentric needle: A randomized single-blind controlled clinical trial, Journal of Cranio-Maxillofacial Surgery (accessed 29 January 29 2025); https://www.sciencedirect.com/science/article/pii/S1010518224001586?casa_token=wn1B-FKLz3oAAAAA:U_ME3x16okhDaOkL8_KZqEwHa44yEaFBf_bm5hsWIQxFNQ_8pMXPopp4dMu0e_USTpfHI22tbcA
Bitiniene, D. et al. Quality of life in patients with temporomandibular disorders. Syst. Rev., 20 (2018).
Talaat, W. M., Hamdoon, Z. & Ghoneim, M. M. Minimally invasive surgeries for the treatment of temporomandibular disorders: prognostic indicators and persistence of treatment outcomes over a 5-year follow-up. Adv. Biomedical Health Sci. 1, 34–44. https://doi.org/10.4103/abhs.abhs_14_21 (2022).
De Riu, G. et al. Arthrocentesis and temporomandibular joint disorders: clinical and radiological results of a prospective study. Int. J. Dent. 2013, 1–8. https://doi.org/10.1155/2013/790648 (2013).
Kim, S., Park, Y. & Kim, S. T. Combined effects of botulinum toxin injection and oral appliance therapy on sleep bruxism: A randomized controlled trial. J. Sleep. Res. 31 https://doi.org/10.1111/jsr.13740 (2022).
Nitzan, D. W., Dolwick, M. F. & Martinez, G. A. Temporomandibular joint arthrocentesis: a simplified treatment for severe, limited mouth opening. J. Oral Maxillofac. Surg. 49, 1163–1167 (1991).
Januzzi, E. et al. Viscosupplementation in the upper and lower compartments of the temporomandibular joint checked by ultrasonography in an ex vivo and in vivo study. Sci. Rep. 12, 17976 (2022).
Emshoff, R., Puffer, P., Strobl, H. & Gassner, R. Effect of temporomandibular joint arthrocentesis on synovial fluid mediator level of tumor necrosis factor-alpha: implications for treatment outcome. Int. J. Oral Maxillofac. Surg. 29, 176–182. https://doi.org/10.1034/j.1399-0020.2000.290304.x (2000).
Tatli, U., Benlidayi, M. E., Ekren, O. & Salimov, F. Comparison of the effectiveness of three different treatment methods for temporomandibular joint disc displacement without reduction. Int. J. Oral Maxillofac. Surg. 46, 603–609 (2017).
De Nordenflycht, D., Ayala, A., Orellana, L. & Tesch, R. D. S. Intra-articular injections in the TMJ inferior joint space: A scoping review. J. Oral Rehabilitation. 50, 1316–1329. https://doi.org/10.1111/joor.13542 (2023).
Li, D. T. S., Wong, N. S. M., Li, S. K. Y., McGrath, C. P. & Leung, Y. Y. Timing of arthrocentesis in the management of temporomandibular disorders: an integrative review and meta-analysis. Int. J. Oral Maxillofac. Surg. 50, 1078–1088 (2021).
Grossmann, E., Januzzi, E. & Iwaki Filho, L. O Uso do hialuronato de Sódio no Tratamento Das disfunções temporomandibulares articulares. Revista Dor. 14, 301–306 (2013).
Hepguler, S. et al. The efficacy of intra-articular sodium hyaluronate in patients with reducing displaced disc of the temporomandibular joint. J. Oral Rehabilitation. 29, 80–86. https://doi.org/10.1046/j.1365-2842.2002.00807.x (2002).
Guarda-Nardini, L. et al. Efficacy of botulinum toxin in treating myofascial pain in bruxers: A controlled placebo pilot study. Cranio J. Craniomandib. Prac. 26, 126–135. https://doi.org/10.1179/crn.2008.017 (2008).
Kopp, S., Carlsson, G. E., Haraldson, T. & Wenneberg, B. Long-term effect of intra-articular injections of sodium hyaluronate and corticosteriod on temporomandibular joint arthritis. J. Oral Maxillofac. Surg. 45, 929–935 (1987).
Albilia, J., Herrera-Vizcaíno, C., Weisleder, H., Choukroun, J. & Ghanaati, S. Liquid platelet-rich fibrin injections as a treatment adjunct for painful temporomandibular joints: preliminary results. CRANIO® 38, 292–304. https://doi.org/10.1080/08869634.2018.1516183 (2020).
Yuce, E. & Komerik, N. Comparison of the efficiacy of intra-articular injection of liquid platelet-rich fibrin and hyaluronic acid after in conjunction with arthrocentesis for the treatment of internal temporomandibular joint derangements. J. Craniofac. Surg. 31, 1870–1874 (2020).
Torul, D., Cezairli, B. & Kahveci, K. The efficacy of intra-articular injectable platelet-rich fibrin application in the management of Wilkes stage III temporomandibular joint internal derangement. Int. J. Oral Maxillofac. Surg. 50, 1485–1490 (2021).
Ghoneim, N. I., Mansour, N. A., Elmaghraby, S. A. & Abdelsameaa, S. E. Treatment of temporomandibular joint disc displacement using arthrocentesis combined with injectable platelet rich fibrin versus arthrocentesis alone. J. Dent. Sci. 17, 468–475 (2022).
Torres-Gaya, J. et al. Temporomandibular joint arthrocentesis guided by ultrasonography: an anatomical study. J. Stomatology Oral Maxillofacial Surg. 122, e27–e31. https://doi.org/10.1016/j.jormas.2021.03.002 (2021).
Alpaslan, G. H. & Alpaslan, C. Efficacy of temporomandibular joint arthrocentesis with and without injection of sodium hyaluronate in treatment of internal derangements. J. Oral Maxillofac. Surg. 59, 613–618 (2001).
Polat, M. E. & Yanik, S. Efficiency of arthrocentesis treatment for different temporomandibular joint disorders. Int. J. Oral Maxillofac. Surg. 49, 621–627 (2020).
Bergstrand, S., Ingstad, H. K., Møystad, A. & Bjørnland, T. Long-term effectiveness of arthrocentesis with and without hyaluronic acid injection for treatment of temporomandibular joint osteoarthritis. J. Oral Sci. 61, 82–88 (2019).
Champs, B., Corre, P., Hamel, A., Laffite, C. D. & Le Goff, B. US-guided temporomandibular joint injection: validation of an in-plane longitudinal approach. J. Stomatology Oral Maxillofacial Surg. 120, 67–70. https://doi.org/10.1016/j.jormas.2018.10.008 (2019).
Orhan, K. & Rozylo-Kalinowska, I. Ultrasonography-guided invasive procedures of the temporomandibular joint. Clin. Dent. Rev. 5, 3. https://doi.org/10.1007/s41894-020-00091-x (2021).
Des Jarlais, D. C., Lyles, C., Crepaz, N. & Group, T. R. E. N. D. The improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. Am. J. Public Health 94, 361–366 https://doi.org/10.2105/AJPH.94.3.361 (2004).
Chaulagain, R. S. et al. Does combining arthrocentesis with injectable platelet-rich fibrin outperform arthrocentesis or injectable platelet-rich fibrin alone in alleviating pain and improving function in temporomandibular joint dysfunction?? J. Oral Maxillofac. Surg. (2025).
Albilia, J. B., Weisleder, H. & Wolford, L. M. Treatment of posterior dislocation of the mandibular condyle with the double Mitek mini anchor technique: a case report. J. Oral Maxillofac. Surg. 76, 396–e1 (2018).
Hegab, A. F., Ali, H. E., Elmasry, M. & Khallaf, M. G. Platelet-rich plasma injection as an effective treatment for temporomandibular joint osteoarthritis. J. Oral Maxillofac. Surg. 73, 1706–1713 (2015).
Fonseca, R. M. D. F. B. et al. Effectiveness of sequential viscosupplementation in temporomandibular joint internal derangements and symptomatology: A case series. Pain Res. Manage. 2018, 1–9. https://doi.org/10.1155/2018/5392538 (2018).
Tamer, T. M. Hyaluronan and synovial joint: function, distribution and healing. Interdisciplinary Toxicol. 6, 111–125. https://doi.org/10.2478/intox-2013-0019 (2013).
Gallagher, B. et al. Chondroprotection and the prevention of osteoarthritis progression of the knee: A systematic review of treatment agents. Am. J. Sports Med. 43, 734–744. https://doi.org/10.1177/0363546514533777 (2015).
Grishko, V. et al. Effects of hyaluronic acid on mitochondrial function and mitochondria-driven apoptosis following oxidative stress in human chondrocytes. J. Biol. Chem. 284, 9132–9139 (2009).
Kalbande, B. S., Vishnani, R. & Malaviya, R. Rev. Techniques TMJ Arthrocentesis, 12 (2022).
Dıraçoğlu, D. et al. Arthrocentesis versus nonsurgical methods in the treatment of temporomandibular disc displacement without reduction, oral surgery, oral medicine, oral pathology. Oral Radiol. Endodontol. 108, 3–8. https://doi.org/10.1016/j.tripleo.2009.01.005 (2009).
Author information
Authors and Affiliations
Contributions
The authors E.J. and M.A.A.d.C. contributed to developing the concept for the work; acquiring, analyzing, and interpreting the data; drafting the article; and revising it critically for important intellectual content. They also granted final approval to the version to be published, and they agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work were appropriately investigated and resolved. The authors P.P., T.C.A.C., G.S., M.K.I., M.P., J.F., A.R.P., A.L.N.C., B.D.M.d.S., A.S.B.D., M.R.S.Z., I.H., S.P., and P.G.d.O. contributed to the acquisition and interpretation of data and critically revised the article for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 2
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Januzzi, E., Pauletto, P., Cunha, T.C.A. et al. Outcomes of modified arthrocentesis using concentric needle and cannula technique with sequential viscosupplementation and orthobiologics in both TMJ compartments. Sci Rep 15, 27465 (2025). https://doi.org/10.1038/s41598-025-06715-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06715-1