Abstract
Detachable coils grant controlled deployment, retrieval, and repositioning until desired placement is achieved for complex visceral artery aneurysms (VAAs), but a detailed investigation is needed for its clinical application. Between June 2018 and September 2020, 28 patients with 31 complex VAAs successfully treated with detachable coils in two hospitals were retrospectively analyzed. The technical success rate reached 100%. Then, 96.8% (30/31) of the afferent arteries and 94.9% (75/79) of the efferent branches were patent without occlusion after the procedure. At the last follow-up, 77.4% and 12.9% of aneurysms were graded as class I and class IIIa, respectively, according to the Modified Raymond-Roy Occlusion Classification. Compared to immediately after the procedure, the number of aneurysms decreased in classes II, IIIa, and IIIb, whereas the number of class I aneurysms significantly increased from 18 to 24 at the last follow-up. Bleeding was not identified in any patients, but three patients (two with abdominal pain and one asymptomatic) developed ischemic complications of either splenic or renal infarction. Overall, transarterial embolization with detachable coils was safe and effective for treating complex VAAs, and the procedure should be performed with caution to avoid ischemic complications.
Similar content being viewed by others
Introduction
Visceral artery aneurysm (VAA) is a rare vascular disease with an average prevalence of 0.1–2%1. Complex VAAs located at the bifurcation of the tortuous visceral artery, in the hilum of distal organs, or with multiple vessels involved are even rarer. In general, VAAs are asymptomatic and incidentally identified for other unrelated clinical indications. The rupture rate of VAAs ranges from 3.1–20%2,3, with a high mortality rate of 20–100% if left untreated3,4.
As per the main therapeutic intention, to exclude the aneurysm while ensuring perfusion of the distal organs, various treatment approaches have been proposed. However, conservative treatment carries a substantial risk of rupture and bleeding, and surgery produces a higher morbidity rate of up to 9% and a mortality rate of up to 1.3% though suitable for complex aneurysms5. Considering its minimal invasiveness and rapid recovery, endovascular therapy has been increasingly preferred for VAAs, particularly when comorbidities coexist6,7. New neurointerventional devices and techniques, such as stenting and flow-diverting stent and balloon-/stent-assisted embolization, have been attempted to treat complex VAAs, but their applications are restricted by hemorrhagic and ischaemic complications8,9,10. Among them, transarterial embolization (TAE) with coils is commonly used for treating VAAs given its lower risk of bleeding compared to other endovascular approaches. Nonetheless, embolizing complex VAAs with coils alone is technically challenging due to potential risks of ischemic complications.
Unlike conventional coils, detachable coils possess the advantages of controlled deployment, retrieval, and repositioning until desired placement is achieved11. However, embolizing complex VAAs using detachable coils is scarcely reported, necessitating a detailed investigation for further exploring its application in the clinical setting. Therefore, this study aimed to evaluate the safety and efficacy of TAE with detachable coils for treating complex VAAs concerning technical success, recurrence, and complications.
Materials and methods
Patients and study design
The study protocol was approved by the Institutional Review Board for Clinical Research at each participating institution in compliance with the recommendations of the Declaration of Helsinki. Written informed consent from patients was waived due to the retrospective nature of the study. From June 2018 to September 2020, medical records and imaging data of consecutive patients with complex VAAs who were successfully treated with TAE using detachable coils in two hospitals were retrospectively analyzed. VAAs primarily affected the splenic artery (SA), superior mesenteric artery (SMA), renal artery (RA), and their branches. Complex VAAs were diagnosed based on multidetector computed tomography (CT) angiography (CTA). Patients who were lost to follow-up or with incomplete imaging data were excluded from further analyses.
Coil embolization
All procedures were performed under local anesthesia by experienced interventional radiologists using a right transfemoral approach. Digital subtraction angiography (DSA) was performed using a 5 Fr RH catheter (Boston Scientific, Natick, USA) to confirm the size and location of the aneurysm, afferent artery/efferent branch, and arterial tortuosity. The catheter was replaced with a 5 Fr Cobra catheter (Cook Medical, Bloomington, USA) in cases of difficult catheterization. Then, a 5 Fr RH or Cobra catheter was placed at the origin of the involved artery for embolization. Detachable coils, including interlock coils (Boston Scientific, Natick, USA) and ev3 coils (ev3, Irvine, USA), were inserted through a 5 Fr catheter or microcatheter when appropriate. For extremely tortuous arteries or catheter springback, a 6 Fr guiding catheter (Boston Scientific, Natick, USA) was inserted to provide adequate strength. All patients were closely monitored after the procedure for serious complications, such as bleeding and target organ infarction.
Angiographic outcomes and follow-up
All patients underwent follow-up CTA or DSA 1–3 months after the procedure and at the last follow-up in December 2022. Visceral arterial tortuosity was divided into three types according to DSA or CTA findings: type I, mild tortuosity with no large bend in the visceral artery; type II, moderate tortuosity with one large bend; and type III, severe tortuosity with two or more large bends. A bend at the origin of the visceral artery was considered physiological and not counted.
Based on the Modified Raymond-Roy Occlusion Classification (MRRC)12, aneurysm occlusion can be categorized into four classes: class I, complete obliteration; class II, residual neck; class IIIa, residual aneurysm with contrast within coil interstices; and class IIIb, residual aneurysm with contrast along the aneurysmal wall. DSA or CTA was also performed to evaluate the patency of the afferent artery/efferent branch. Complications were recorded whenever identified.
Statistical analysis
All quantitative data are expressed as mean ± standard deviation. Dichotomous and categorical data are reported as numbers and percentages. All statistical analyses were performed using SPSS (version 22.0, SPSS, Chicago, USA).
Results
Patient and aneurysm characteristics
The baseline characteristics of the patients and aneurysms are shown in Table 1. A total of 28 patients (7 males and 21 females) at a mean age of 62 ± 11 years (range, 36–81 years) were included. Of the 31 aneurysms whose mean size was 21.8 ± 5.7 mm (range, 13–33 mm), 24 (77.4%) were splenic artery aneurysms (SAAs), 2 (6.5%) were superior mesenteric artery aneurysms (SMAAs), and 5 (16.1%) were renal artery aneurysms (RAAs). Besides, 25 patients (89.3%) had a single aneurysm, while three patients (10.7%) had multiple VAAs. Two patients developed two tandem SAAs, and one patient developed an SAA and an SMAA. All VAAs were saccular aneurysms in terms of morphology. Of the 26 tortuous visceral arteries, 23 (88.5%) were categorized as severely tortuous, 1 (3.8%) as moderately tortuous, and 2 (7.7%) as mildly tortuous (Fig. 1). Three patients were admitted due to pain, with two having mild abdominal pain and one having sudden right lumbar pain.
Embolization of the aneurysms
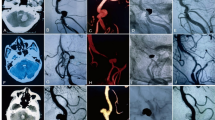
All aneurysms were successfully embolized using detachable coils alone, reaching a technical success rate of 100% (31/31). At the last follow-up, 24 (77.4%) aneurysms were completely occluded, and 28 (90.3%) achieved excellent clinical prognosis. No class I aneurysm deteriorated, but one class II aneurysm deteriorated to class IIIa. One class II aneurysm improved to class I; five class IIIa aneurysms improved to class I aneurysms; and one class IIIb aneurysm improved to class II. As summarized in Table 2, more class I aneurysms were identified at the last follow-up than immediately after embolization, and class IIIa aneurysms at the last follow-up became significantly fewer. No significant difference was noticed in either class II or IIIb aneurysms. In this study, a ruptured class II right RAA, determined on post-procedural angiogram, was embolized in an emergency setting (Fig. 2), whereas all other VAAs were embolized during elective procedures. Unfortunately, the ruptured RAA recurred after 2 years and after recoiling, it deteriorated to class IIIa at the last follow-up. Reintervention or recurrence was not found in any other cases.
Emergency embolization of a ruptured renal artery aneurysm (RAA). (A) Renal arteriogram demonstrated the ruptured RAA (arrow) with four efferent branches (arrowheads). (B) Renal arteriogram after coil embolization showed occlusion of the aneurysm with patent branches, and the classification of occlusion was classified as class II as per the Modified Raymond-Roy Classification (MRRC). (C) Two years later, recurrence of the aneurysm and increased contrast filling in the aneurysmal neck was detected on digital subtraction angiography (DSA). (D) DSA after re-embolization showed complete embolization of the aneurysm and classified as MRRC class I.
Arterial patency
In this study, 31 afferent arteries and 79 efferent branches were involved, and each aneurysm had one afferent artery and an average of 2.6 ± 0.7 (range, 2–4) efferent branches (Table 3). The patency rate of the afferent artery and the efferent branch was 96.8% (30/31) and 94.9% (75/79), respectively; in other words, one afferent artery and four efferent branches were completely obstructed. More particularly, only one SAA and involved arteries (i.e., one afferent artery and two efferent branches) were completely embolized, and the remaining two occluded efferent branches belonged to two different aneurysms.
Complications
Complications are listed in Table 4. During a mean follow-up of 43.3 ± 7.7 months (range, 27–54 months), bleeding did not occur in any patients. Ischemic complications developed in three patients, including two splenic infarctions and one renal infarction, resulting in a complication rate of 10.7%. In more detail, two cases of splenic infarction were accompanied by abdominal pain, which was spontaneously resolved a few days later. Pain developed immediately after TAE in one patient as the parent artery was completely occluded and one month after TAE since one of the two efferent branches was occluded. Asymptomatic renal infarction was detected in one patient at the 1-month follow-up without afferent/efferent branch obstruction. None of the infarctions required surgical resection of the target organ, and the three patients were continuously monitored.
Discussion
The most important finding was that having a technical success rate of 100% (31/31), TAE with detachable coils was safe and effective for treating complex VAAs. Compared to conservative treatment and surgery, the approach demonstrated in this study could help to reduce the risk of rupture and subsequent bleeding and potentially decrease the morbidity and mortality rates throughout a mean follow-up of 43.3 ± 7.7 months. These were thought to benefit from the precise deployment of the coils where the coils could be repositioned before being detached to ensure desired placement. With respect to arterial tortuosity, TAE with detachable coils was effective for all complex VAAs in this study regardless of their arterial tortuosity being mild, moderate, or severe though most patients (88.5%) were diagnosed with severe arterial tortuosity. Also, TAE with detachable coils was performed through a minimally invasive approach, which was considered safer and more tolerable for patients with a relatively high age, given that the mean age of the group was 62 years in this study.
The common indications for treatment of VAAs are aneurysms larger than 2 cm in SAAs and larger than 1 cm in RAAs, the presence of progressive enlargement over time, and symptoms attributable to the aneurysm3,13. Other recommended indications for treatment include women of childbearing age in the peripartum period and liver transplant recipients3,13,14,15. There is no optimal treatment for complex VAAs, though both surgical and endovascular approaches are feasible16. Although endovascular therapy represents a safe and effective alternative to conventional surgery given its lower procedure-related morbidity and mortality but high technical success rates17,18, it faces great challenges (e.g., bleeding and ischemic complications) in the cases of complex VAAs. Stent implantation and stent-/balloon-assisted embolization are technically difficult in severely distorted visceral arteries and may increase the risk of complications. Neck control failure is up to 22.2% in such applications, and insufficient stent expansion, intraprocedural vessel injury, and subsequent distal thromboembolic complications have also been reported19. Furthermore, stent-/balloon-assisted procedures for complex VAAs require intraprocedural heparinization or post-procedural long-term antiplatelet therapy to prevent thrombosis, boosting the risk for intra- and post-procedural bleeding8,9. However, for coil embolization alone, pre-procedural antiplatelet preparation or intra-procedural heparinization was not required, and intra- or post-procedural bleeding was not discovered in this study.
The tortuosity of the visceral artery is categorized into three types and affects the positioning and stability of the catheter, which is critical for successful TAE with detachable coils. Of the three types, type III accounted for 88.5% of the patients in this study, making catheter placement more challenging. In this scenario, a 6 Fr guiding catheter was used to provide sufficient support to hold the microcatheter in place and maintain sufficient stability during embolization. In addition, the microcatheter was shaped before insertion to better allow the end to pass through the bends for a more stable embolization. As a result, a 100% technical success rate was achieved in this study, which was consistent with previous publications (90–100%)20, realizing higher aneurysm occlusion and visceral artery patency rates.
For complex VAAs, complete embolization of the aneurysm and the parent artery may prevent aneurysm recurrence but carries a higher risk of target organ infarction. Rather than complete embolization of the aneurysm and parent artery5,21, simple embolization of the aneurysm can reduce the complication of organ infarction by maintaining visceral artery patent. In this study, the parent artery was preserved as much as possible given the benefits of detachable coils – safer, more effective, and more easily manipulated than conventional coils11. As a result, the parent arteries were effectively preserved after embolization, with 96.8% of the afferent arteries and 94.9% of the efferent branches patent.
Similar to previous reports2, ischemic complications occurred in three (10.7%) patients, including two patients suffering from abdominal pain and one asymptomatic patient. Of the two patients suffering from painful splenic infarction, one’s pain was thought to rise from complete embolization of the splenic artery (i.e., one afferent artery and two efferent branches), and detached thrombi was thought to cause the symptoms in the other patient, causing inadequate collateral circulation. Asymptomatic renal infarction without afferent/efferent artery obstruction was detected at 1-month follow-up in the third patient, which was likely related to peripheral small vessel embolism caused by thrombosis and shedding. As illustrated in a retrospective study, complete embolization of the splenic artery is safe and feasible for patients with SAAs and normal spleen; however, severe complications may occur when the collateral circulation is insufficient or not consummate5. Taken together, this study further demonstrated the great significance of maintaining parent artery patent while embolizing complex VAAs.
Considering TAE may result in incomplete occlusion and require reintervention22, MRRC was established to grade the occlusion of endovascularly treated intracranial aneurysms and predict prognosis12,23. Despite that classes II and IIIb aneurysms tend to produce higher rupture and reintervention rates12, a ruptured RAA in this study was graded as class II after the procedure and required reintervention though rupture did not recur after treatment. In addition, class IIIa aneurysms showed a higher rate of improvement to class I than class II aneurysms, which was consistent with Mascitelli et al.’s study on intracranial study12. Besides, 90.3% of complex VAAs had a satisfying prognosis in this study. Therefore, it is believed that MRRC can also be applied to evaluate the occlusion status of complex VAAs9. Compared to immediately after the procedure, the number of aneurysms decreased in classes II, IIIa, and IIIb, whereas the number of class I aneurysms significantly increased from 18 to 24 at the last follow-up. Following MRRC during embolization of complex VAAs may help avoid recanalization of the aneurysms and lower the risk of vascular occlusion. Also, post-procedural MRRC evaluation of complex VAAs is critical for making follow-up strategies, which may reduce patient costs as well as X-ray exposure without minimally invasive angiographic examinations.
There are some limitations in this study. First, as a retrospective study with a small sample size, inherent bias may exist to hinder the generalizability of the outcomes. Larger case series or prospective multicenter studies are needed to further validate the findings of this study. Second, defining arterial tortuosity by the number of vascular curvatures may not be appropriate, though it is helpful for selecting treatment options based on the patient’s condition. Third, VAAs embolized in this study were mainly unruptured saccular true aneurysms, which had an advantage in the first framing detachable coil embolization. Lastly, intestinal gas and bowel movement may affect MRRC grading.
Conclusion
Embolization of complex VAAs with detachable coils was safe and reliable with a lower risk of aneurysm recurrence or reintervention while maintaining the patency of the parent artery. Subsequent prospective clinical trials with larger sample sizes and extended follow-ups are warranted to further validate this technique.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Belli, A. M., Markose, G. & Morgan, R. The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc. Interv. Radiol. 35, 234–243 (2012).
Pitton, M. B. et al. Visceral artery aneurysms: incidence, management, and outcome analysis in a tertiary care center over one decade. Eur. Radiol. 25, 2004–2014 (2015).
Kok, H. K., Asadi, H., Sheehan, M., Given, M. F. & Lee, M. J. Systematic review and single-center experience for endovascular management of visceral and renal artery aneurysms. J. Vascular Interventional Radiology: JVIR. 27, 1630–1641 (2016).
Pasha, S. F., Gloviczki, P., Stanson, A. W. & Kamath, P. S. Splanchnic artery aneurysms. Mayo Clin. Proc. 82, 472–479 (2007).
Li, E. S. et al. Total Splenic artery embolization for Splenic artery aneurysms in patients with normal spleen. World J. Gastroenterol. 20, 555–560 (2014).
Ruhnke, H. & Kroncke, T. J. Visceral artery aneurysms and pseudoaneurysms: retrospective analysis of interventional endovascular therapy of 43 aneurysms. RoFo: Fortschr. Auf Dem Gebiete Der Rontgenstrahlen Und Der Nuklearmedizin. 189, 632–639 (2017).
Venturini, M. et al. Endovascular repair of 40 visceral artery aneurysms and pseudoaneurysms with the viabahn stent-graft: technical aspects, clinical outcome and mid-term patency. Cardiovasc. Interv. Radiol. 41, 385–397 (2018).
Murray, T. E. et al. Treatment of visceral artery aneurysms using novel neurointerventional devices and techniques. J. Vascular Interventional Radiology: JVIR. 30, 1407–1417 (2019).
Secco, G. et al. Packing technique with or without remodeling for endovascular coil embolization of renal artery aneurysms: safety, efficacy and mid-term outcomes. J Clin Med. 10(2), 326. https://doi.org/10.3390/jcm10020326 (2021).
Ye, P. et al. Endovascular therapy for distal hilar renal artery aneurysm: A case report and literature review. J. Int. Med. Res. 50(1), 3000605211069282. https://doi.org/10.1177/03000605211069282 (2022).
Dudeck, O. et al. Embolization of the gastroduodenal artery before selective internal radiotherapy: A prospectively randomized trial comparing standard pushable coils with fibered interlock detachable coils. Cardiovasc. Interv. Radiol. 34, 74–80 (2011).
Mascitelli, J. R. et al. An update to the raymond-roy occlusion classification of intracranial aneurysms treated with coil embolization. J. Neurointerventional Surg. 7, 496–502 (2015).
Loffroy, R. et al. Endovascular management of visceral artery aneurysms: When to watch, when to intervene? World J Radiol. 7(7), 143–148. https://doi.org/10.4329/wjr.v7.i7.143 (2015).
Nosher, J. L., Chung, J., Brevetti, L. S., Graham, A. M. & Siegel, R. L. Visceral and renal artery aneurysms: A pictorial essay on endovascular therapy. Radiographics: Rev. Publication Radiological Soc. North. Am. Inc. 26, 1687–1704 (2006). quiz 1687.
Bracale, U. M. et al. Stent-assisted detachable coil embolization of wide-necked renal artery aneurysms. Diagn. Interv Radiol. 23, 77–80 (2017).
Martinelli, O. et al. Single-center experience in the treatment of visceral artery aneurysms. Ann. Vasc. Surg. 60, 447–454 (2019).
Chadha, M. & Ahuja, C. Visceral artery aneurysms: diagnosis and percutaneous management. Semin Intervent Radiol. 26, 196–206 (2009).
Hosn, M. A., Xu, J., Sharafuddin, M. & Corson, J. D. Visceral artery aneurysms: decision making and treatment options in the new era of minimally invasive and endovascular surgery. Int. J. Angiol. 28, 11–16 (2019).
Fischer, S. et al. Coiling of wide-necked carotid artery aneurysms assisted by a temporary bridging device (comaneci): preliminary experience. J. Neurointerventional Surg. 9, 1039–1097 (2017).
Wang, W. et al. Long-term outcomes of elective transcatheter dense coil embolization for Splenic artery aneurysms: A two-center experience. J. Int. Med. Res. 48, 300060519873256 (2020).
Loffroy, R. et al. Transcatheter arterial embolization of Splenic artery aneurysms and pseudoaneurysms: Short- and long-term results. Ann. Vasc. Surg. 22, 618–626 (2008).
Patel, A. et al. Single-center experience with elective transcatheter coil embolization of Splenic artery aneurysms: technique and midterm follow-up. J. Vascular Interventional Radiology: JVIR. 23, 893–899 (2012).
Funakoshi, Y. et al. Predictors of cerebral aneurysm rupture after coil embolization: Single-center experience with recanalized aneurysms. AJNR Am. J. Neuroradiol. 41, 828–835 (2020).
Acknowledgements
This study was supported by the Jiangsu Medical Association Interventional Medicine Research Fund Project [SYH-3201140-0048(2022005)].
Author information
Authors and Affiliations
Contributions
Study concepts and design: G.F.Z., G.D., and Y.L.Q. Literature research: G.F.Z., D.M., J.J.J., and Z.B.B. Manuscript preparation: G.F.Z., C.H.Z., D.M., and R.L. Manuscript editing: G.F.Z, C.H.Z., D.M., and Y.L.Q. Figure Preparation: G.F.Z and D.M. Final Manuscript Review: G.F.Z, C.H.Z., D.M., Y.L.Q, J.J.J, Z.B.B, R.L., and G.D.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, GF., Zeng, C., Man, D. et al. The safety and efficacy of transarterial embolization with detachable coils for complex visceral artery aneurysm. Sci Rep 15, 20786 (2025). https://doi.org/10.1038/s41598-025-06917-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06917-7