Abstract
The aim of this study was to identify risk factors more comprehensively and develop the first nomogram for predicting tigecycline-associated drug induced liver injury (DILI) in a Chinese population. Patients who underwent tigecycline treatment from January 1, 2021, to July 31, 2024, at the Affiliated Hospital of Jining Medical University were included in this retrospective study. Candidate variables were selected using least absolute shrinkage and selection operator (Lasso) regression and support vector machine recursive feature elimination (SVM-RFE), followed by univariate and multivariate logistic regression to identify independent risk factors, which were visualized in a nomogram. Nomogram model performance was evaluated via the area under the receiver operating characteristic curve (AUC). A total of 357 patients were enrolled, including 73 patients (20.4%) diagnosed with DILI, and 284 patients (79.6%) without. Fourteen intersected variables were screened through Lasso regression and SVM-RFE method. Seven variables were identified as independent risk factors and were used to construct prediction nomogram model. The AUC values of 0.82 (95% CI: 0.76–0.88) in the training cohort and 0.80 (95% CI: 0.70–0.89) indicated the nomogram model had satisfactory prediction ability. Furthermore, decision curve analysis (DCA) revealed that the nomogram provided a significant net benefit in the identifying patients at high risk of tigecycline-associated DILI. This study was the first to identify patients treated with voriconazole, with a history of malignant tumors, in a state of septic shock, and with intra-abdominal infections were at a significantly elevated risk of developing tigecycline-associated DILI. The constructed nomogram demonstrated a high level of accuracy, showcasing substantial potential to aid clinicians in pinpointing risk factors and implementing preventive measures.
Similar content being viewed by others
Introduction
Tigecycline, the first glycylcycline-class semisynthetic antibiotic, was developed to treat polymicrobial multidrug-resistant infections1,2. Approved for indications such as complicated intra-abdominal infections (cIAI), complicated skin and skin structure infections (cSSSI), and community-acquired pneumonia (CAP)3, it also serves as a treatment for severe Clostridioides difficile infections4. Compared with tetracycline, tigecycline demonstrates superior antibacterial activity by overcoming resistance mechanisms such as efflux pumps and ribosome protection5. It further circumvents resistance pathways in other antibiotics, including enzymatic degradation, DNA gyrase mutations, and drug target modifications6, positioning it as a “last-resort” therapy for multidrug-resistant bacterial infections. However, its clinical safety—particularly hepatotoxicity—has emerged as a critical concern for clinicians.
Unpredictable DILI remains one of the most challenging liver disorders in clinical practice. Antibiotics are recognized as major contributors to idiosyncratic DILI7,8. While tigecycline’s most common adverse effects are gastrointestinal (e.g., nausea, vomiting), its product labeling warns of hepatotoxicity, manifested as elevations in total bilirubin (TB) and transaminases9. DILI associated with tigecycline can range from mild liver enzyme elevations to life-threatening liver failure, potentially requiring liver transplantation or leading to mortality10. Once the DILI occurs especially with the increase of transaminases ((aspartate/alanine transaminase ratio greater than five times the upper limit of normal) and/or jaundice, the culprit drug should be discontinued11. Consequently, identifying predictive factors and developing robust risk prediction models are imperative for guiding clinical decision-making and implementing preventive strategies against tigecycline-associated DILI.
To date, risk factors for tigecycline-associated DILI still remain controversial. Yu et al. reported that Intensive Care Unit (ICU) admissions, abnormal baseline alanine aminotransferase (ALT) levels and prolonged treatment duration were independent risk factors for tigecycline-associated DILI12. The study conducted by Shi et al. found that high maintenance dose, number of concomitant hepatotoxic drugs and prolonged duration is related to the tigecycline-associated DILI13. Additionally, low baseline albumin (ALB < 25 g/L) and treatment duration have been implicated as significant predictors14. The discrepancies in current research data underscore the urgent need for systematic and multi-level in-depth studies to comprehensively elucidate the risk factor spectrum of tigecycline-associated DILI, thereby providing evidence-based decision-making support for clinical practice.
Carbapenem-resistant Acinetobacter baumannii (CRAB) is reported to be one of the most common causative pathogens of hospital-acquired infections in China. Guidelines from the China Bacterial Resistance Surveillance Network recommend tigecycline-based regimens, often combined with polymyxin15. Due to its cost-effectiveness, tigecycline is frequently employed in clinical practice, although its heteroresistance profile limits its utility as monotherapy16. A common strategy involves combining tigecycline with cefoperazone/sulbactam for CRAB infections17, despite cefoperazone/sulbactam’s documented hepatic adverse effects, including elevations in ALT, aspartate aminotransferase (AST), alkaline phosphatase (ALP), and bilirubin. Furthermore, tigecycline is often administered to patients with multidrug-resistant bacterial infections who require concomitant voriconazole for fungal prophylaxis or treatment. Voriconazole is a well-established cause of acute DILI18, raising questions about whether these combinations exacerbate hepatotoxicity risks. However, the impact of cefoperazone/sulbactam or voriconazole co-use on tigecycline-associated DILI remains unclear.
Nomograms, as visual predictive models, offer clinicians tools for individualized risk assessment and proactive intervention. Despite their utility in other medical fields, no nomogram has been developed to predict tigecycline-associated DILI. This study aims to address this gap by developing a precision nomogram for Chinese patients based on machine learning and logistic regression analyses, while validating associations between clinical variables and DILI risk.
Results
Characteristics of the study population.
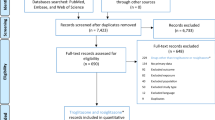
A total of 833 patients treated with tigecycline from January 1, 2021, to July 31, 2024 were identified from the medical records(Fig. 1). 302 patients were excluded own to the lack of laboratory data (36.2%), treatment duration less than three days(122, 14.6%), and ages less than 18 years (52, 6.24%). Ultimately, 357 patients were enrolled, including 73 patients diagnosed with DILI, and 284 patients without.
Optimization of variables.
The risk factors of tigecycline-associated DILI.
The results of univariate logistic regression analysis for the 14 variables were presented in Fig. 4. The results revealed that variables such as combination therapy with voriconazole, maintenance dose, treatment duration, malignant tumor, sepsis shock, ICU admission, intra abdomen infection and baseline platelet were more likely to associate with an increased likelihood of tigecycline-associated DILI. Subsequently, multivariate logistic regression analysis indicated that combination therapy with voriconazole (OR 2.09, 95% CI 1.11–3.92), maintenance dose(OR 3.44, 95% CI 1.84–6.14), treatment duration(OR 1.13, 95% CI 1.06–1.21), malignant tumor(OR 3.86, 95% CI 1.68–8.86), sepsis shock(OR 2.71, 95% CI 1.41–5.23), Baseline platelet(OR 1.00, 95% CI 0.99-1.00) and intra abdomen infection(OR 2.90, 95% CI 1.18–7.12) were independent risk factors for tigecycline-associated DILI. Notably, the baseline platelet factor was excluded owning to the OR value was 1, indicating a lack of significant association with the development of DILI.
Development and validation of tigecycline-associated DILI predicting nomogram.
To develop a predictive model for tigecycline-associated DILI, the patients were randomly allocated into training and validation cohorts at a 7:3 ratio. Candidate variables identified through univariate logistic regression were subjected to multivariate logistic regression analysis in each cohort, and a nomogram was constructed as the final predictive model. The logistic regression equation was: logit(P) = − 4.803 + (Voriconazole × 0.983) + (Maintenance dose × 1.311) + (Treatment duration × 0.099) + (Malignant tumor × 1.849) + (Sepsis shock × 0.841) + (ICU admission × 0.987) + (Intra-abdominal infection × 0.999).
Of these, 245 patients were assigned into the training cohort and 112 into the validation cohort. The DILI occurred in 43 patients (17.5%) in the training cohort and 30 patients (26.7%) in the validation cohort. No significant differences were found among these 7 independent risk factors between the two cohorts (P > 0.05) (Table 2), confirming reasonable and random grouping.
Then, using the 7 independent risk factors, the quantitative and convenient nomogram model was provided in the training cohort (Fig. 5). The respective values of each factor were on the variable axis and its corresponding score was defined as the vertical line from the value to the points. These 7 scores were summed and located on the total points. The risk of the tigecycline-associated DILI was defined as the vertical line from the total points to the risk. The performance of this nomogram was evaluated by AUC. In the training cohort, the AUC was 0.82 (C-index: 0.819, 95% CI: 0.76–0.88), and in the validation cohort, it was 0.80 (C-index: 0.795, 95% CI: 0.70–0.89) (Fig. 6a and b), indicating satisfactory predictive ability. Calibration curves (Fig. 6c and d) showed that the tigecycline-associated DILI probabilities predicted by the nomogram matches well with the actual situation. In addition, the decision curve analysis (DCA) revealed that this model showed a positive net benefit from the risk of DILI (Fig. 7), indicating its great clinical practical application in predicting tigecycline-associated DILI.
Discussion
Carbapenem-resistant A. baumannii (CRAB) has emerged as worldwide public threat. Its infection ranks the fourth in terms of antibiotic resistance19. Tigecycline, polymyxin and sulbactam were the most commonly used agents. As polymyxin was associated with great toxicity and side effects, its use was restricted20. In China, the combination therapy of tigecycline and sulbactam was generally recommended21. A multicenter retrospective study reported a 10.3% incidence of tigecycline-associated DILI12, highlighting the urgent need for risk stratification tools. This study addresses this gap by developing the first predictive nomogram for tigecycline-associated DILI, enabling clinicians to implement early clinical interventions.
Patients receiving tigecycline are often immunocompromised, increasing susceptibility to aspergillosis and necessitating combination therapy with voriconazole. Voriconazole is strongly associated with asymptomatic serum aminotransferase elevations and acute liver injury22. Our study is the first to demonstrate that voriconazole co-administration significantly increases DILI risk (OR = 2.09, 95% CI = 1.11–3.92), underscoring the need for intensified liver function monitoring in such patients.
In addition, our analysis also firstly revealed that malignant tumors, sepsis shock, and intra abdomen infection are independent risks for tigecycline-associated DILI. Two possible factors contribute in malignant tumors patients. On the one hand, the liver was the second most frequently influenced organ through metastasis, even without function or homeostasis change23. On the other hand, the chemotherapeutic therapys combined with radiation and other medications were significant cause of DILI24. The liver is one of the most frequently affected target from sepsis injury, including inducing hypoxic hepatitis, cholestasis, and hepatocellular injury25. Generally, sepsis shock indicated that the patients were under life-threatening dysfunction. Therefore, patients under sepsis shock state should be monitored closely about the liver function when using the tigecycline treatment. Intra-abdominal infection might result in liver damage through bacterial overgrowth and its translocation towards the liver via the portal vein26. Thus, clinicians should be more cautious about the safety when the intra-abdominal infection patient used tigecycline for treatment.
The association between treatment duration, maintenance dose, and DILI aligns with findings by Shi et al..¹³ but contrasts with a multicenter study by Yu et al..¹², highlighting ongoing controversies. Some data reported with increased risk27,28 while some were oppsoited29. Our study indicated a dose-dependent risk (OR = 3.44, 95% CI = 1.84–6.14), emphasizing the need to balance therapeutic efficacy with safety when optimizing dosing regimens. Notably, cefoperazone/sulbactam—frequently co-administered for CRAB—was not associated with DILI, possibly due to its dual hepatorenal clearance pathway27. However, larger studies are needed to confirm this finding.
The nomogram constructed in the present study was the first one and may have significant implications at aiding the clinicians evaluating the possibilities of DILI. Although this nomogram performed well, some limitations should not be ignored. Firstly, this was a retrospective study, some bias and confounders seem inevitable. Secondly, our sample was small and single-center. Though this nomogram was proved useful, larger samples in multi-center were needed for confirmation to use in clinical.
Conclusion
In conclusion, concomitant voriconazole use, treatment duration, maintenance dose, malignant tumor, sepsis shock and intra abdomen infection were firstly found as independent risk factors for tigecycline-associated DILI. A highly accurate nomogram was constructed to predict the risk of tigecycline-associated DILI which makes it an valuable tool for clinicians to individually manage tigecycline-associated side effects.
Materials and methods
Study design and Ethical considerations.
This single-center, case-control, and retrospective study was performed in the Affiliated Hospital of Jining Medical University. The objective was to develop an accurate prediction model for the tigecycline-associated DILI. The enrolled patients were from January 1, 2021, to July 31, 2024 treatment with tigecycline in the Affiliated Hospital of Jining Medical University, Jining Medical University.
This study was approved by the Ethics Committee of the Affiliated Hospital of Jining Medical University. Due to its retrospective design, the required informed consent was waived. The study was carried out in accordance with the Declaration of Helsinki and the Ethical Guidelines for Medical and Health Research Involving Human Subjects.
The inclusion and exclusion definition.
Patients met the criteria were included: (1) ages ≥ 18 years; (2) the treatment duration ≥ 3 days. Patients were excluded with the criteria followed: (1) the pregnant woman; (2) woman under breastfeeding; (3) the incomplete data of liver function during the treatment.
The criterion for judgement tigecycline-associated DILI.
Guided by the National Cancer Institute Common Terminology Criteria for Adverse Events version 5.0 grading system30the patients met the following criteria during tigecycline treatment were defined as possibly tigecycline-associated DILI: (1) ALT ≥ 3×upper limit of normal (ULN), (2) AST ≥ 3×ULN, (3) ALP ≥ 2.5×ULN, (4) TB ≥ 1.5×ULN. For patients with abnormal above biochemical indicators, the ULN should be replaced by them.
Date collection.
The basic laboratory values including indicators of liver function and inflammation were defined as the data obtained within 7 days prior to the onset day of tigecycline used. DILI-related liver function values were defined as data collected from the onset of tigecycline treatment up to 3 days after initiation. The combination therapy was defined as simultaneous use for more than 3 days. All data were collected from the electronic medical records.
The standard data collection format was applicable to all patients, with a total of 50 variables included: demographics (age, gender, body weight, history of smoking or drinking), medical history (diabetes mellitus, solid organ cancer, hematologic malignancy, malignant tumor, cardiovascular disease, nephropathy, liver disease, ICU admission, sepsis shock, CRRT, mechanical ventilation), infection site (pulmonary, intra-abdomen, skin and soft tissue, and other or undefined), maintenance dose, treatment duration, combination therapies (voriconazole, cefoperazone sulbactam, sulfamethoxazole, linezolid, quinolones, macrolide, sodium valproate, ciclosporin or tacrolimus, nonsteroidal anti-inflammatory drugs and statins), number of hepatotoxic drugs used concomitantly, baseline Child-Pugh class, clinical parameters (baseline ALT, AST, ALP, GGT, TBil, DBil, albumin, prothrombin time, APTT, fibrinogen, platelet, creatinine, WBC, C-reactive protein, PCT), and time to onset of hepatotoxicity.
Statistics.
Firstly, the raw data were preprocessed with R software (version 4.3.1). VIM 6.2.2 and mice 3.15.0 packages were used to address the missing data and conduct five times imputations. Subsequent analyses were applied to filter the candidate variables among 50 collected variables through Lasso regression and SVM-RFE selection method. Lasso regression was conducted though a ten-fold cross-validation procedure and the least absolute shrinkage with the glmnet 4.1.6 package. SVM-RFE was through nonlinear kernels using the e1071 package to eliminate the least important variables.
Univariate and multivariate logistic regression analyses were then conducted to select independent risk factors for nomogram construction with p value < 0.05. The discrimination ability of the prediction nomogram model was validated by AUC. Calibration curves were performed by a visual calibration plot to compare the predicted and actual probability of tigecycline DILI. Decision curve analysis (DCA) was performed to calculate the individual net benefits as to validate the clinical benefits of this prediction model. P < 0.05 was considered as statistically significant.
Data availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
References
Greer, N. D. Tigecycline (Tygacil): the first in the Glycylcycline class of antibiotics. Proc. (Bayl Univ. Med. Cent). 19 (2), 155–161. https://doi.org/10.1080/08998280.2006.11928154 (2006).
Garrison, M. W., Neumiller, J. J. & Setter, S. M. Tigecycline: an investigational Glycylcycline antimicrobial with activity against resistant gram-positive organisms. Clin. Ther. 27 (1), 12–22. https://doi.org/10.1016/j.clinthera.2005.01.007 (2005).
Heizmann, W. R. et al. Clinical efficacy of Tigecycline used as monotherapy or in combination regimens for complicated infections with documented involvement of multiresistant bacteria. Infection 43 (1), 37–43. https://doi.org/10.1007/s15010-014-0691-4 (2015).
Kechagias, K. S., Chorepsima, S., Triarides, N. A. & Falagas, M. E. Tigecycline for the treatment of patients with Clostridium difficile infection: an update of the clinical evidence. Eur. J. Clin. Microbiol. Infect. Dis. 39 (6), 1053–1058. https://doi.org/10.1007/s10096-019-03756-z (2020).
Jenner, L. et al. Structural basis for potent inhibitory activity of the antibiotic Tigecycline during protein synthesis. Proc. Natl. Acad. Sci. U S A. 110 (10), 3812–3816. https://doi.org/10.1073/pnas.1216691110 (2013).
Seputiene, V. et al. Tigecycline - how powerful is it in the fight against antibiotic-resistant bacteria? Med. (Kaunas). 46 (4), 240–248 (2010).
Chalasani, N. et al. Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the united States. Gastroenterology 135 (6), 1924–1934. https://doi.org/10.1053/j.gastro.2008.09.011 (2008).
Chalasani, N. et al. Features and outcomes of 899 patients with Drug-Induced liver injury: the DILIN prospective study. Gastroenterology 148 (7), 1340–52e7. 10.1053/ j.gastro.2015.03.006 (2015).
Shi, X., Lao, D., Xu, Q., Li, X. & Lv, Q. A case report of drug-induced liver injury after Tigecycline administration: histopathological evidence and a probable causality grading as assessed by the updated RUCAM diagnostic scale. BMC Infect. Dis. 22 (1), 368. https://doi.org/10.1186/s12879-022-07258-w (2022).
Björnsson, H. K. & Björnsson, E. S. Drug-induced liver injury: pathogenesis, epidemiology, clinical features, and practical management. Eur. J. Intern. Med. 97, 26–31. https://doi.org/10.1016/j.ejim.2021.10.035 (2022).
Katarey, D. & Verma, S. Drug-induced liver injury. Clin. Med. (Lond). 16 (Suppl 6), s104–s109. https://doi.org/10.7861/clinmedicine.16-6-s104 (2016).
Yu, Z. et al. Prevalence and risk factors of tigecycline-associated liver injury: A multicenter retrospective study. Int. J. Infect. Dis. 120, 59–64. https://doi.org/10.1016/j.ijid.2022.04.024 (2022).
Shi, X. et al. Real-World data of Tigecycline-Associated Drug-Induced liver injury among patients in china: A 3-year retrospective study as assessed by the updated RUCAM. Front. Pharmacol. 12, 761167. https://doi.org/10.3389/fphar.2021.761167 (2021).
Jiang, T. et al. Risk factors for Tigecycline-Associated hepatotoxicity in patients in the intensive care units of 2 tertiary hospitals: A retrospective study. J. Clin. Pharmacol. 62 (11), 1426–1434. https://doi.org/10.1002/jcph.2099 (2022).
Paul, M. et al. European society of clinical microbiology and infectious diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin. Microbiol. Infect. 28 (4), 521–547. https://doi.org/10.1016/j.cmi.2021.11.025 (2022).
Liu, H. et al. Detection and characterization of Tigecycline heteroresistance in E. cloacae: clinical and Microbiological findings. Emerg. Microbes Infect. 8 (1), 564–574. https://doi.org/10.1080/22221751.2019.1601031 (2019).
Garnacho-Montero, J. et al. Task force on management and prevention of Acinetobacter baumannii infections in the ICU. Intensive Care Med. 41 (12), 2057–2075. https://doi.org/10.1007/s00134-015-4079-4 (2015).
Kyriakidis, I., Tragiannidis, A., Munchen, S. & Groll, A. H. Clinical hepatotoxicity associated with antifungal agents. Expert Opin. Drug Saf. 16 (2), 149–165. https://doi.org/10.1080/14740338.2017.1270264 (2017).
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet 399 (10325), 629–655. https://doi.org/10.1016/S0140-6736(21)02724-0 (2022).
Piperaki, E. T., Tzouvelekis, L. S., Miriagou, V. & Daikos, G. L. Carbapenem-resistant Acinetobacter baumannii: in pursuit of an effective treatment. Clin. Microbiol. Infect. 25 (8), 951–957. https://doi.org/10.1016/j.cmi.2019.03.014 (2019).
Chinese, X. D. R. & Consensus Working Group. Laboratory diagnosis, clinical management and infection control of the infections caused by extensively drug-resistant Gram-negative bacilli: a Chinese consensus statement. Clin. Microbiol. Infect. 22 (Suppl 1), S15–25. https://doi.org/10.1016/j.cmi.2015.11.004 (2016).
Pata, R., Dolkar, T., Patel, M. & Nway, N. Voriconazole-Induced acute liver injury: A case report. Cureus 13 (12), e20115. https://doi.org/10.7759/cureus.20115 (2021).
Clark, A. M., Ma, B., Taylor, D. L., Griffith, L. & Wells, A. Liver metastases: microenvironments and ex-vivo models. Exp. Biol. Med. (Maywood). 241 (15), 1639–1652. https://doi.org/10.1177/1535370216658144 (2016).
Bahirwani, R. & Reddy, K. R. Drug-induced liver injury due to cancer chemotherapeutic agents. Semin Liver Dis. 34 (2), 162–171. https://doi.org/10.1055/s-0034-1375957 (2014).
Strnad, P., Tacke, F., Koch, A. & Trautwein, C. Liver - guardian, modifier and target of sepsis. Nat. Rev. Gastroenterol. Hepatol. 14 (1), 55–66. https://doi.org/10.1038/nrgastro.2016.168 (2017).
Kobashi, H., Toshimori, J. & Yamamoto, K. Sepsis-associated liver injury: incidence, classification and the clinical significance. Hepatol. Res. 43 (3), 255–266. https://doi.org/10.1111/j.1872-034X.2012.01069.x (2013).
Gong, J. et al. Efficacy and safety of high-dose Tigecycline for the treatment of infectious diseases: A metaanalysis. Med. (Baltim). 98, e17091. https://doi.org/10.1097/MD.0000000000017091 (2019).
Zha, L. et al. Effectiveness and safety of high dose Tigecycline for the treatment of severe infections: A systematic review and Meta-Analysis. Adv. Ther. 37, 1049–1064. https://doi.org/10.1007/s12325-020-01235-y (2020).
Garnacho-Montero, J. & Ferrándiz-Millón, C. High dose of Tigecycline for extremely resistant Gram-negative pneumonia: yes, we can. Crit. Care. 18, 157. https://doi.org/10.1186/cc13942 (2014).
National Cancer Institute, National Institutes of Health, US Department of Health and Human Services. Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. (2017). https://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_8.5x11.pdf.Published Accessed September 19, 2024.
Author information
Authors and Affiliations
Contributions
X.Z. and H. H. conceived and designed the study. X. Z. and L. L. collected the data. C. Z.performed the analysis and interpreted the results. X.Z. drafted the manuscript. H. Z. revised the manuscript. X. Z. and H. H.supervised the study and manuscript submission. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, X., Li, L., Zhang, C. et al. A nomogram for predicting the risk of tigecycline-associated drug-induced liver injury in a Chinese population. Sci Rep 15, 22593 (2025). https://doi.org/10.1038/s41598-025-07116-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-07116-0