Abstract
This study investigated the effects of corneal and lens characteristics, including refractive power, thickness, and curvature, on peripheral defocus and their impact on different regions. A cross-sectional study was conducted involving 296 patients with myopia using data from the right eye. Peripheral retinal defocus was measured using a novel device, a multispectral refractive topographer, which can assess peripheral defocus. Retinal images were sequentially captured using single-wavelength monochromatic light at varying wavelengths to determine the refractive status of the fundus. Select relevant data at the corneal diameters of 4 mm, 6 mm, and 8 mm (superior, inferior, nasal and temporal). The refractive power of the superior cornea negatively correlated with peripheral defocus in inferior regions. Specifically, cornea refractive power at the 4 mm position below the cornea negatively correlated with peripheral defocus in inferior regions (r = -0.130, P < 0.05; r = -0.141, P < 0.05). Temporal corneal refractive power was negatively correlated with peripheral defocus in certain inferior regions. Nasal corneal refractive power negatively correlated with peripheral defocus in inferior regions and positively correlated with peripheral defocus in superior regions. Lens refractive power was positively correlated with peripheral defocus in superior regions and negatively correlated with peripheral defocus in inferior regions. Refractive media such as the cornea and lens are strongly associated with peripheral defocus in different regions. Among these, corneal refractive power exerts the most significant influence. Inferior peripheral defocus exhibits significant correlations with superior, temporal, and nasal corneal refractive powers. Temporal and inferior hyperopic peripheral defocus demonstrate a stronger association with myopia compared to other regions.
Similar content being viewed by others
Introduction
Peripheral defocus may be an important factor that influences myopia progression. Previous animal studies have shown that, during refractive development, hyperopic peripheral defocus leads to posterior movement of the retina, ultimately resulting in axial elongation1. However, previous studies have often focused on the overall state of peripheral defocus, lacking regional analysis. Currently, there is limited research on the impact of corneal and lens refractive characteristics on peripheral defocus.
Some studies have indicated that the cornea can affect peripheral defocus. For example, wearing orthokeratology lenses can alter the corneal shape, causing a myopic shift in peripheral defocus and thereby controlling the onset and progression of myopia2,3. However, the specific correlations remain unclear, and the range, magnitude, and extent of the influence of different corneal regions on retinal peripheral defocus remain unknown.
Other studies have suggested that the lens may also contribute to the generation of peripheral defocus4. Walker and Lundström et al. found that under accommodative stimulation, hyperopic shifts in peripheral defocus occur in the nasal retina5,6. Conversely, Whatham et al.7 observed a myopic shift in peripheral defocus upon measurement. Additionally, some studies have reported that peripheral defocus does not significantly change with accommodation8. These conflicting findings highlight the need for further research to clarify these relationships.
Therefore, the current study systematically partitioned the refractive states of the cornea and lens alongside the peripheral defocus state of the retina. This study aims to explore the range, magnitude, and extent of influence of different corneal and lens regions on peripheral retinal defocus. Furthermore, this study sought to associate these factors with the onset and progression of myopia, thereby investigating the changes that occur during its development.
Methods and materials
Study population
From January to March 2024, 296 patients with myopic who underwent preoperative examinations at the Refractive Surgery Center of Tianjin Ophthalmology Hospital, Tianjin Medical University, were recruited. The cohort included 141 males and 155 females, aged between 18 and 40 years (25.7 ± 6.4 years). Data from the right eyes were used in this study.
The study was conducted in accordance with the principles of the Declaration of Helsinki. All participants voluntarily participated in the study and signed an informed consent form. The study protocol was approved by the Medical Ethics Committee of Tianjin Ophthalmology Hospital (KY-2024020).
Inclusion criteria
-
Age ≥ 18 years.
-
Refractive error stable for at least 2 years.
-
Transparent cornea without opacities or scars.
-
Normal corneal morphology without tendencies toward keratoconus.
-
Best-corrected visual acuity ≥ 0.8.
-
Soft contact lenses were discontinued for ≥ 2 weeks, and rigid contact lenses were discontinued for ≥ 4 weeks.
Exclusion criteria
-
Other ocular diseases, such as keratoconus, keratitis, glaucoma, and severe dry eye.
-
History of ocular surgery or trauma.
-
Systemic immune-related diseases, connective tissue diseases, diabetes, etc.
-
Pregnant or breastfeeding women.
Examination
All patients underwent comprehensive examinations, including subjective and objective refraction, uncorrected visual acuity, intraocular pressure, and anterior segment examination. The Pentacam (Pentacam HR, Oculus, Wetzlar, Germany) anterior segment imaging analyzer was used to measure the total corneal refractive power, steep keratometry (K2), flat keratometry (K1), and mean keratometry (Km). LenStar (LS-900; Haag-Streit AG, Switzerland) optical biometry device (Haag-Streit AG, Switzerland) was used to measure central corneal thickness (CCT) and axial length (AL). CASIA2 anterior segment OCT (Tomey Corporation, Nagoya, Japan) was used to measure the average radius of curvature of the anterior and posterior surfaces of the lens, anterior chamber depth (ACD), steepest curvature radius, flattest curvature radius, and Lens Thickness (LT).
Peripheral defocus examination
A multispectral refractive topographer (MRT; MSI C2000, Shenzhen Shengda Tongze), whose accuracy has been validated9,10. is a novel device capable of measuring retinal peripheral defocus. It involves sequentially capturing fundus images using single-wavelength monochromatic light at different wavelengths. By compensating for the movement of the lens, a large number of fundus images are taken continuously. Using advanced computer algorithms, a comparative analysis of multispectral images is performed after lens compensation to calculate and compile the actual refractive values of each pixel. Imaging primarily uses infrared light, interspersed with other spectral lights to identify retinal details and distinguish clarity at different focal lengths at the chromatic aberration level. It can measure peripheral defocus within a 53° range centered on the macula fovea. MRT is more accurate than the previous measurement method and has a larger measurement range.
Examination procedure
Patients were seated with their chin resting on the chin rest and their forehead pressed against the forehead rest. After being instructed to blink several times and open their eyes wide to gaze at a fixed red fixation target, the examiner adjusted the joystick until the image was centered and vertically aligned. After pressing the examination button, the machine automatically identified and captured the image, obtaining peripheral defocus data. Each eye was measured three times, and the average of the results with a system confidence level greater than 90% was used for analysis. All examinations were performed by the same ophthalmologist to ensure consistency.
Data analysis and statistical methods
Analyze the effects of corneal thickness and corneal refractive power on different areas of peripheral defocus. Additionally, the effects of parameters such as the lens and cornea on peripheral defocus were also analyzed.
Selection of corneal thickness and corneal refractive power
Select relevant data at the corneal diameters of 4 mm, 6 mm, and 8 mm (superior, inferior, nasal and temporal). Corneal thickness:
-
Superior corneal thickness: CCTS4, CCTS6, CCTS8.
-
Inferior corneal thickness: CCTI4, CCTI6, CCTI8.
-
Nasal corneal thickness: CCTN4, CCTN6, CCTN8.
-
Temporal corneal thickness: CCTT4, CCTT6, CCTT8.
Corneal refractive power:
-
Superior corneal refractive power: FS4, FS6, FS8.
-
Inferior corneal refractive power: FI4, FI6, FI8.
-
Nasal corneal refractive power: FN4, FN6, FN8.
-
Temporal corneal refractive power: FT4, FT6, FT8.
Division of peripheral defocus into different regions
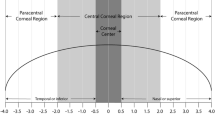
After excluding the peripheral defocus within a 15° range centered on the macula, retinal defocus was equally divided into four regions: superior, inferior, nasal, and temporal, denoted as RDVS, RDVI, RDVN, and RDVT, respectively. Subsequently, based on a 30° circular range centered on the macula, horizontal and vertical axes, 45°−225° axis, and 135°−315° axis, each region was further divided into four sub-regions denoted as S1-S4, I1-I4, T1-T4, and N1-N4 (Fig. 1).
Calculation of Lens refractive power (PL)
The Bennett formula11 was used for calculation, c1 and c2 were the estimated parameters by the Gullstrand-Emsley eye model. c₁ = 0.596, c₂ = −0.358. ACD: anterior chamber depth, CCT: central corneal thickness, LT lens thickness, V: vitreous depth, K: corneal power, Rm, a: anterior corneal curvature radius, Rm, p: posterior corneal curvature radius, and the corneal refractive index (nc =1.376), as well as the refractive index of aqueous and vitreous humors (n = 1.333). Scv was the spherical refraction at the corneal vertex. Refraction was measured using an autorefractor (Topcon KR-800, Topcon Co. Tokyo, Japan). SE was calculated as follows: SE = spherical power + 0.5 × cylindrical power.
Statistical analyses were performed using SPSS (version 22; IBM Corporation). All collected data were first subjected to the Kolmogorov-Smirnov test for normality. Pearson’s correlation analysis was performed when data followed a normal distribution. Spearman’s correlation analysis was used for non-normally distributed data. Statistical significance was set at p < 0.05.
Results
Distribution characteristics of corneal refractive power and retinal peripheral defocus
The average corneal refractive power gradually increased from the center to the periphery, with the nasal corneal refractive power being the lowest (Fig. 2). Retinal peripheral defocus exhibited asymmetry, with the strongest hyperopic peripheral defocus observed in regions T4 and I3 and the strongest myopic the peripheral defocus in regions S2 and S4 (Fig. 3).
Distribution of average corneal refractive power. The sample size was 296 patients’ right eyes. FS1-FS4 denote the mean corneal refractive power at the 4 mm, 6 mm, and 8 mm superior corneal locations. FI1-FI4 denote the mean corneal refractive power at the 4 mm, 6 mm, and 8 mm inferior corneal locations. FT1-FT4 represent the average corneal refractive powers at the 4, 6, and 8 mm positions on the temporal side of the cornea. FN1-FN4 represent the average corneal refractive power at the 4, 6, and 8 mm positions on the nasal side of the cornea.
Distribution of retinal peripheral defocus. OD: right eye, Red (positive values) represents hyperopic defocus, and blue (negative values) represents myopic peripheral defocus. Sample size: 296 right eyes, S1-S4: The four superior zones of peripheral defocus, I1-I4: The four inferior zones of peripheral defocus, T1-T4: The four temporal zones of peripheral defocus, N1-N4: The four nasal zones of peripheral defocus.
Correlation analysis between corneal refractive power and peripheral defocus
The refractive power of the superior cornea was negatively correlated with the peripheral defocus in regions I2 and I4 (both P < 0.05). Specifically, corneal refractive power measured at 4 and 6 mm positions above the cornea was negatively correlated with the peripheral defocus in region I1 (r = −0.123, P < 0.04; r = −0.118, P < 0.048). Corneal refractive power measured at the 4 mm position below the cornea was negatively correlated with the peripheral defocus in I2 and I4 regions (r = −0.130, P < 0.05; r = −0.141, P < 0.05) as well as in region N4 (r = −0.139, P < 0.05). Temporal corneal refractive power was negatively correlated with the peripheral defocus in regions I2 and I4. Additionally, corneal refractive power measured at the 8 mm position on the temporal side of the cornea was negatively correlated with the peripheral defocus in region N4 (r = −0.122, P < 0.05). Nasal corneal refractive power was negatively correlated with the peripheral defocus in region I4 but positively correlated with the peripheral defocus in regionS2. Furthermore, corneal refractive power at 4 mm position on the nasal side of the cornea was negatively correlated with the peripheral defocus in region I2 (r = −0.118, P < 0.05).
No significant correlations were found between the corneal refractive power in other regions and retinal peripheral defocus (all P > 0.05) (Fig. 4).
Correlation between peripheral defocus and total corneal refractive power. FS4, FS6, and FS8 represent corneal refractive power at the 4 mm, 6 mm, and 8 mm superior corneal locations, FI4, FI6, and FI8 represent corneal refractive power at the 4 mm, 6 mm, and 8 mm inferior corneal locations, FT4, FT6, and FT8 represent corneal refractive power at 4, 6, and 8 mm positions on the temporal side of the cornea, FN4, FN6, and FN8 represent corneal refractive power at 4, 6, and 8 mm positions on the nasal side of the cornea, S1-S4: The four superior zones of peripheral defocus, I1-I4: The four inferior zones of peripheral defocus. T1-T4: The four temporal zones of peripheral defocus, N1-N4: The four nasal zones of peripheral defocus. *: P < 0.05; **: P < 0.01.
Correlation analysis between corneal thickness and peripheral defocus
Corneal thickness at the 8 mm position above the cornea was positively correlated with the peripheral defocus in regions I4 and N2 (r = 0.141, P < 0.05; r = 0.119, P < 0.05) but negatively correlated with the peripheral defocus in region T1 (r = −0.140, P < 0.05). Corneal thickness at the 8 mm position below the cornea was negatively correlated with the peripheral defocus in region T1 (r = −0.121, P < 0.05). Corneal thickness at 8 mm position on the temporal side of the cornea was positively correlated with the peripheral defocus in region N1 (r = 0.118, P < 0.05). Corneal thickness at 6 mm and 8 mm positions on the nasal side of the cornea was negatively correlated with the peripheral defocus in region T1 (r = −0.122, P < 0.05; r = −0.154, P < 0.01).
No significant correlations were found between corneal thickness in other regions and peripheral defocus (all P > 0.05) (Fig. 5).
Correlation between peripheral defocus and corneal thickness. CCTS4, CCTS6, and CCTS8 represent corneal thicknesses at the 4 mm, 6 mm, and 8 mm superior corneal locations, CCTI4, CCTI6, and CCTI8 represent corneal thicknesses at the 4 mm, 6 mm, and 8 mm inferior corneal locations. CCTT4, CCTT6, and CCTT8 represent corneal thicknesses at 4, 6, and 8 mm positions on the temporal side of the cornea. and CCTN4, CCTN6, and CCTN8 represent corneal thicknesses at the 4, 6, and 8 mm positions on the nasal side of the cornea. S1-S4: The four superior zones of peripheral defocus, I1-I4: The four inferior zones of peripheral defocus. T1-T4: The four temporal zones of peripheral defocus, N1-N4: The four nasal zones of peripheral defocus. *: P < 0.05, **: P < 0.01.
Correlation analysis between corneal curvature, anterior chamber depth, and peripheral defocus
K1 was negatively correlated with the peripheral defocus in region I4 (r = −0.178, P < 0.01). K2 was negatively correlated with the peripheral defocus in regions I2 and I4 (r = −0.134, P < 0.05; r = −0.144, P < 0.05). Km was negatively correlated with the peripheral defocus in regions I2 and I4 (r = −0.131, P < 0.05; r = −0.167, P < 0.01). ACD was positively correlated with the peripheral defocus in regions I1, T2, and T4 (r = 0.137, P < 0.05; r = 0.158, P < 0.05; r = 0.150, P < 0.05, respectively) (Fig. 6).
Correlation between peripheral defocus and other refractive factors. K1: Flat keratometry; K2: Steep keratometry; Km: Mean keratometry; ACD: Anterior Chamber Depth; R-F (lens): radius of curvature of the anterior surface of the lens, R-B (lens): radius of curvature of the posterior surface of the lens, LT: Lens thickness, PL: Lens refractive power. S1-S4: The four superior zones of peripheral defocus, I1-I4: The four inferior zones of peripheral defocus. T1-T4: The four temporal zones of peripheral defocus, N1-N4: The four nasal zones of peripheral defocus. *: P < 0.05; **: P < 0.01.
Correlation analysis between radius of curvature of the lens, thickness, refractive power, and peripheral defocus
The average radius of curvature of the anterior surface of the lens was negatively correlated with the peripheral defocus in regions S1, S2, S3, and S4 (r = −0.152, P < 0.05; r = −0.150, P < 0.05; r = −0.175, P < 0.01; r = −0.163, P < 0.01, respectively). LT was positively correlated with the peripheral defocus in regions S1, S2, S3, and S4 (r = 0.272, P < 0.01; r = 0.183, P < 0.01; r = 0.269, P < 0.01; r = 0.183, P < 0.01, respectively) and negatively correlated with the peripheral defocus in regions I2 and I4 (r = −0.198, P < 0.01; r = −0.166, P < 0.05, respectively). Lens refractive power was positively correlated with the peripheral defocus in regions S1 and S4 (r = 0.166, P < 0.05; r = 0.140, P < 0.05) and negatively correlated with the peripheral defocus in region I1 (r = −0.146, P < 0.05). The average radius of curvature of the posterior surface of the lens showed no significant correlation with peripheral defocus in any region (all P > 0.05) (Fig. 6).
Correlation analysis between peripheral defocus in different regions and spherical equivalent and AL
Peripheral defocus in the superior regions was negatively correlated with spherical equivalents (all P > 0.05). The peripheral defocus in regions I3 and I4 was negatively correlated with the spherical equivalent (all P > 0.05), and the peripheral defocus in the temporal regions was negatively correlated with the spherical equivalent (all P < 0.01). These results indicate that greater hyperopic peripheral defocus is associated with higher spherical equivalent values.
The peripheral defocus in regions I1-I3 was positively correlated with AL (all P > 0.05), indicating that greater hyperopic peripheral defocus is associated with longer ALs (Table 1).
Discussion
Although research on the relationship between peripheral defocus and myopia has been conducted for many years, the specific characteristics and underlying mechanisms in localized regions remain unclear. This study is the first to perform a regional analysis of peripheral defocus in myopic eyes, examining the relationship between the morphological characteristics of the ocular surface, cornea, and lens with peripheral defocus. The study findings revealed that the refractive power of the inferior cornea was the highest among all corneal regions. Additionally, corneal refractive power increased progressively from the center to the periphery, with nasal corneal refractive power being lower than that in other regions (Fig. 2). However, in conventional measurements, corneal refractive power progressively decreases from the central to peripheral regions. Because the data we used comes from the “Total Corneal Refractive Power” in Pentacam. This model accounts for both the anterior and posterior corneal surfaces and the true refractive index, while also incorporating the influence of corneal thickness and asphericity on corneal refractive power. Conventional measurements of corneal refractive power are often based solely on the curvature of the anterior surface. Therefore, conventional measurements differ from our results. Regarding retinal peripheral defocus, hyperopic defocus was the strongest in the inferior and temporal regions, whereas myopic defocus was the strongest in the superior regions (Fig. 3).
Corneal refractive power is a significant factor influencing peripheral defocus12. Our results indicate that inferior peripheral defocus is closely related to the refractive power of the superior, nasal, and temporal corneal regions. Similarly, peripheral defocus in region S2 was influenced by nasal corneal refractive power, and peripheral defocus in region N4 was affected by I4 and T8 corneal refractive powers (Fig. 4). This correlation may be related to the projection of light within the fundus, especially with respect to inferior peripheral defocus. Furthermore, our results revealed that the impact of the cornea on peripheral defocus was not strictly one-to-one. For example, inferior peripheral defocus is simultaneously influenced by the superior, nasal, and temporal regions of the cornea. This may be due to the fact that in natural conditions, the direction of light is non-uniform, where peripheral defocus in a specific region can be affected by light from adjacent areas. In addition, the eye is a non-concentric eccentric optical element, and peripheral retinal defocus may also be affected by this, which may also be related to the above phenomenon. Although we did many correlation analyses, some of the correlation results are meaningless for the reasons mentioned above. However, we believe that the correlation between the corneal refractive power in the superior, nasal, and temporal directions and the peripheral defocus in the inferior part is the most important and meaningful. This is because the hyperopic peripheral defocus in the inferior and temporal regions is the strongest. However, these conjectures require further research for validation.
Our study revealed that the four inferior zones of peripheral defocus exhibited stronger correlations with corneal refractive power, while peripheral defocus in other regions showed only limited associations. Additionally, the inferior region is one of the most pronounced areas of hyperopic peripheral defocus, and this distinctive phenomenon has prompted further investigation. Previous studies have demonstrated that in emmetropic eyes, the inferior region of the retinal nerve fiber layer (RNFL) exhibits a greater average thickness compared to other regions13. This may be related to the higher density of motion-related visual signals that the inferior retina is required to process. However, in myopic eyes, the inferior RNFL is thinner. This morphological alteration suggests that the inferior retina may be more susceptible to changes during myopic progression14. This may account for the higher prevalence of positive outcomes observed in inferior peripheral defocus compared to other regions in our results. Further research is needed to validate this hypothesis.
The lens, a vital component of the intraocular refractive system, plays a significant role in peripheral defocus. This study found a positive correlation between LT and peripheral hyperopic defocus, which is consistent with the findings of Mutti et al.15 Additionally, this study discovered that LT was strongly and positively correlated with superior peripheral defocus (P < 0.01) and negatively correlated with the peripheral defocus in regions I2 and I4. The refractive power of the lens is positively correlated with the peripheral defocus in regions S1 and S4 and negatively correlated with the peripheral defocus in region I2, which is generally consistent with the aforementioned correlation between LT and peripheral defocus. This phenomenon may be related to the shape and degree of tilt of the lens. There are no direct studies on the effects of lens shape and tilt on peripheral defocus. However, through a literature we hypothesized that the lens shape and degree of tilt may have an effect on peripheral retinal defocus16. Since this experiment did not accurately measure the lens shape and degree of tilt, we will further explore this in future studies.
There is an interplay among the cornea, lens, and peripheral retinal defocus. Our study found that because the refractive power of the inferior cornea and lens was greater than that of other regions, refracted light forms a myopic peripheral defocus above the retina. The refractive power of the nasal cornea and lens is weaker than that of other regions; therefore, after light passes through it, a hyperopic peripheral defocus forms in the temporal and inferior retina (I3, T4). Additionally, the internal and external rotation of the eyeball during the near- and far-viewing processes, as well as the tilt of the lens, may have some impact on the final projection, causing hyperopic defocus to occur in the temporal and inferior region rather than on the temporal side. Although we did not measure the refractive power of the lens in different regions, Pearson correlation analysis showed a negative correlation between the refractive power of the lens and the inferior retinal regions, indirectly supporting our results.
Peripheral defocus is closely associated with the onset and progression of myopia. We divided the peripheral defocus of the retina into 16 regions, some of which have correlations with the axial length and spherical equivalent, while others do not. We believe that this phenomenon may be due to the varying degrees of peripheral defocus in different regions affecting myopia. Previous studies by Faria-Ribeiro and Radhakrishnan have shown that peripheral defocus in the nasal area may be associated with the progression of myopia17,18. However, the study by Lin19 suggests that peripheral defocus in the superior region is an indicator of myopia development. Our research found that the strongest hyperopic peripheral defocus occurred in the temporal and inferior regions (I3, T4), and there was a strong correlation with spherical refractive error (P < 0.01) (Table 1). Therefore, we believe that this area may be an important region affecting the occurrence and development of myopia. During the onset and development of myopia in children, prolonged near work with a downward gaze causes the eyeball to rotate downward and inward, partially occluding the inferior cornea. Light is refracted by the superior cornea and lens and projected below the retina, forming a strong hyperopic peripheral defocus20, which may further contribute to the onset and progression of myopia.
After wearing orthokeratology lenses during myopia correction, the central corneal curvature becomes flatter, while the mid-periphery becomes steeper. Simultaneously, peripheral defocus shifts from hyperopic to myopic. However, the group wearing single-vision glasses did not experience this change21. This indicates that the morphology of peripheral defocus is closely related to the refractive power of the cornea. However, previous studies have typically analyzed the cornea as a whole in relation to the peripheral defocus of the fundus, and peripheral defocus measurements were often limited to the axial line. This research method does not clearly reflect the impact of different corneal regions on peripheral defocus. Therefore, in our study, relevant parameters were selected from different regions of the cornea at 4, 6, and 8 mm positions in the superior, inferior, nasal, and temporal directions, representing the central, paracentral, and peripheral corneal regions, respectively.
Because of the asymmetry of peripheral defocus, the peripheral area was further subdivided in this study. After removing the retinal defocus within a 15° range centered on the macula, the retinal defocus was equally divided into four regions: superior, inferior, nasal, and temporal. Subsequently, based on a 30° circular range centered on the macula along the horizontal, vertical, 45°−225°, and 135°−315° axes, each region was further divided into four sub-regions, totaling 16 regions, labeled as S1-S4, I1-I4, T1-T4, and N1-N4 (Fig. 1). This subdivision allowed for a more precise and targeted analysis.
This study has some limitations. Although we analyzed the impact of factors, such as the cornea and lens, on peripheral defocus in different regions, the optical principle behind it is not yet known. We plan to pursue more comprehensive investigations into this subject in future studies.
In conclusion, refractive factors, such as the cornea and lens, influence peripheral defocus in different regions. Our results indicate that corneal refractive power is the main factor affecting retinal peripheral defocus, whereas other factors, such as the lens, have a limited impact. Specifically, the temporal and inferior regions of retinal peripheral defocus form significant hyperopic defocus and are strongly correlated with the degree of myopia. We believe that this phenomenon may be related to prolonged near work, in which light entering the eye is refracted by the cornea and lens, resulting in hyperopic defocus in the temporal and inferior retina, thereby contributing to the onset and progression of myopia. This study provides new insights for further research into the mechanisms of myopia and offers new approaches for more effective myopia correction. For example, designing frame glasses or orthokeratology lenses that target inferior peripheral defocus may offer more effective prevention and control of myopia.
Data availability
All data used in the statistical analyses are available upon request from the corresponding author.
References
Smith, E. L. 3rd et al. Effects of optical defocus on refractive development in monkeys: evidence for local, regionally selective mechanisms. Investigative ophthalmology & visual science 51, 3864–3873, (2010). https://doi.org/10.1167/iovs.09-4969
Wang, J. et al. Anisomyopia and orthokeratology for myopia control - Axial elongation and relative peripheral refraction. Ophthalmic Physiol. Opt. 44, 1261–1269. https://doi.org/10.1111/opo.13365 (2024).
Yang, X., Li, Z. & Zeng, J. A. Review of the potential factors influencing myopia progression in children using orthokeratology. Asia Pac. J. Ophthalmol. (Phila). 5, 429–433. https://doi.org/10.1097/apo.0000000000000242 (2016).
Yu, J. & Zhou, Y. Effect of Lens deviation on peripheral defocus and optic quality in adolescents with moderate and severe myopia. Eye Contact Lens. 50, 375–383. https://doi.org/10.1097/icl.0000000000001104 (2024).
Walker, T. W. & Mutti, D. O. The effect of accommodation on ocular shape. Optom. Vis. Sci. 79, 424–430. https://doi.org/10.1097/00006324-200207000-00010 (2002).
Lundström, L., Mira-Agudelo, A. & Artal, P. Peripheral optical errors and their change with accommodation differ between emmetropic and myopic eyes. J Vis 9 (11-11) https://doi.org/10.1167/9.6.17 (2009).
Whatham, A. et al. Influence of accommodation on off-axis refractive errors in myopic eyes. J. Vis. 9, 14.11–13. https://doi.org/10.1167/9.3.14 (2009).
Calver, R., Radhakrishnan, H., Osuobeni, E. & O’Leary, D. Peripheral refraction for distance and near vision in emmetropes and myopes. Ophthalmic Physiol. Opt. 27, 584–593. https://doi.org/10.1111/j.1475-1313.2007.00518.x (2007).
Lu, W. et al. Agreement and repeatability of central and peripheral refraction by one novel Multispectral-Based refractor. Front. Med. (Lausanne). 8, 777685. https://doi.org/10.3389/fmed.2021.777685 (2021).
Liao, Y. et al. A quantitative comparison of multispectral refraction topography and autorefractometer in young adults. Front. Med. (Lausanne). 8, 715640. https://doi.org/10.3389/fmed.2021.715640 (2021).
Bennett, A. G. A method of determining the equivalent powers of the eye and its crystalline lens without resort to phakometry. Ophthalmic Physiol. Opt. 8, 53–59. https://doi.org/10.1016/0275-5408(88)90089-0 (1988).
Kang, P. & Swarbrick, H. Time course of the effects of orthokeratology on peripheral refraction and corneal topography. Ophthalmic Physiol. Opt. 33, 277–282. https://doi.org/10.1111/opo.12027 (2013).
Nousome, D. et al. Retinal nerve Fiber layer thickness in healthy eyes of black, chinese, and Latino americans: A Population-Based multiethnic study. Ophthalmology 128, 1005–1015. https://doi.org/10.1016/j.ophtha.2020.11.015 (2021).
Mu, Y. et al. Interocular comparison of peripapillary retinal nerve fiber layer thickness and vasculature in non-pathological myopia with anisometropia. Graefes Arch. Clin. Exp. Ophthalmol. https://doi.org/10.1007/s00417-025-06826-5 (2025).
Mutti, D. O., Sholtz, R. I., Friedman, N. E. & Zadnik, K. Peripheral refraction and ocular shape in children. Investig. Ophthalmol. Vis. Sci. 41, 1022–1030 (2000).
Natarajan, R. et al. Peripheral defocus of monofocal intraocular lenses. J. Cataract Refract. Surg. 50, 637–643. https://doi.org/10.1097/j.jcrs.0000000000001441 (2024).
Zadnik, K. et al. Ocular predictors of the onset of juvenile myopia. Invest. Ophthalmol. Vis. Sci. 40, 1936–1943 (1999).
Radhakrishnan, H. et al. Peripheral refractive changes associated with myopia progression. Invest. Ophthalmol. Vis. Sci. 54, 1573–1581. https://doi.org/10.1167/iovs.12-10278 (2013).
Lin, Z. et al. Relative myopic defocus in the superior retina as an Indicator of myopia development in children. Invest. Ophthalmol. Vis. Sci. 64, 16. https://doi.org/10.1167/iovs.64.4.16 (2023).
Charman, W. N. Myopia, posture and the visual environment. Ophthalmic Physiol. Opt. 31, 494–501. https://doi.org/10.1111/j.1475-1313.2011.00825.x (2011).
Huang, Y. et al. Orthokeratology reshapes eyes to be less prolate and more symmetric. Cont. Lens Anterior Eye. 45, 101532. https://doi.org/10.1016/j.clae.2021.101532 (2022).
Acknowledgements
The authors would like to thank all the participants of this study and Editage (www.editage.cn) for their assistance with English language editing.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82271118) and Tianjin Health Research Project (No. TJWJ2022XK036).
Author information
Authors and Affiliations
Contributions
S.Q. and F.S. contributed to the study’s conception and design. S.Q., F.S., S.B. and Y.L. organized the database. S.Q., L.C., and Y.T. analyzed and interpreted data. S.Q. wrote the first draft of the manuscript. S.Q. commented on previous versions of the manuscript. Y.W. provided administrative, technical, and material support, as well as supervision. All the authors contributed to the manuscript and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Commercial relationships disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qu, S., Song, F., Li, Y. et al. Analysis of the effects of corneal and lens characteristics on peripheral defocus of the retina and its relationship with myopia. Sci Rep 15, 22102 (2025). https://doi.org/10.1038/s41598-025-07126-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07126-y