Abstract
Despite advances in metastatic breast cancer (MBC) management, leptomeningeal disease (LMD) prognosis remains poor. This study evaluates clinicopathological and treatment factors influencing outcomes of MBC patients with LMD treated with radiotherapy (RT). We conducted a retrospective analysis of patients with MBC treated with RT for brain metastases (BrM) between 2005 and 2019. LMD diagnosis was made via magnetic resonance imaging (MRI). Multivariable analysis (MVA) identified variables associated with brain-specific progression-free survival (bsPFS) and overall survival (OS). Among 691 MBC patients treated with RT for BrM, 161 (23%) had LMD, either at initial presentation (50/161) or after BrM treatment. Patients with LMD were younger, more likely to have ER + disease, more likely to have undergone surgery for BrM, and less likely to have received prior whole-brain RT. HER2+ LMD was associated with longer bsPFS (HR 0.47, 95% CI: 0.25–0.86, p = 0.01) and OS (HR 0.38, 95% CI: 0.2–0.75, p = 0.002). Median OS for triple-negative breast cancer was 3.7 months, 5.1 months for HR+/HER2 − and 15.4 months for HER2 + MBC. HER2-targeted therapy, either at or after LMD diagnosis, improved long-term survival (> 2 years) (Fisher’s test, p < 0.05). Low Karnofsky Performance Status (KPS < 60) was linked to shorter bsPFS (HR 2.91, 95% CI: 1.49–5.69, p < 0.01) and OS (HR 3.37, 95% CI: 1.78–6.41, p < 0.001). These findings highlight the need for effective CNS-penetrating systemic therapies for HER2-negative breast cancer.
Similar content being viewed by others
Introduction
Leptomeningeal disease (LMD) is a devastating complication of metastatic breast cancer (MBC) characterized by the infiltration of cancer cells into the leptomeninges of the brain and/or spinal cord, generally resulting in severe morbidity and short survival1. Approximately 5–15% of patients with MBC develop LMD and those with HER2-positive disease are at particularly high risk2. Recent advances in anti-HER2 therapies with the ability to penetrate the blood brain barrier, including T-DM1, Trastuzumab Deruxtecan, and Tucatinib, have significantly improved survival for patients with HER2 + MBC and brain metastases (BrM)3,4,5. These improvements in prognosis, however, have led to a prolongation of survival, during which patients may develop complications such as LMD6.
The development of LMD in a breast cancer patient typically presents a poor prognosis, with a median survival of 3–6 months7,8,9. However, there is substantial variation in survival outcomes influenced by specific factors, including molecular and histological subtype, performance status, extracranial control, and number of parenchymal BrM10,11,12. Available treatment options include radiotherapy (whole brain radiotherapy [WBRT] and/or craniospinal irradiation [CSI], ) intrathecal chemotherapy, brain-penetrating systemic chemotherapy, and/or targeted agents13,14). Recently, proton CSI has also emerged as a novel therapeutic option with a median CNS progression-free survival rate of 7 months in 21 patients with a variety of malignancies including 3 with breast cancer15.
Although both BrM and LMD are manifestations of CNS involvement, they differ in terms of spread, treatment response, and survival impact. LMD often arises as a progression from BrM, so understanding the link between the two could help identify patients at higher risk for LMD as well as the factors that influence outcomes. This understanding could improve prognostication, guide treatment decisions, and support more personalized strategies for managing high-risk patients. In the largest retrospective cohort to date, we report on the survival outcomes and risk factors associated with LMD development in MBC patients with BrM treated with RT.
Methods
Patient population
This study was approved by the Research Ethics Board (REB) at Sunnybrook Hospital and conducted in accordance with the Declaration of Helsinki. We retrospectively reviewed all MBC patients with BrM and/or LMD treated with stereotactic radiosurgery (SRS) and/or whole-brain radiotherapy (WBRT) at our center between 2005 and 2019. Informed consent was obtained from all study participants. Data were compiled from the electronic patient and treatment records, detailing demographic and clinical characteristics, and treatment modalities, including age and stage at diagnosis of initial breast cancer, breast cancer subtype, breast cancer treatments delivered (surgery, systemic therapy, radiation), age at BrM diagnosis and LMD diagnosis, number of BrM upon initial referral for radiation, size and location of largest BrM, BrM and LMD treatments delivered (surgery, WBRT, SRS, fractionated stereotactic radiotherapy (FSRT), palliative spine RT), type and location of LMD diagnosed.
Radiation treatment
Radiation treatments were delivered using either SRS via the Gamma Knife® Icon™ (Elekta AB, Stockholm, Sweden), FSRT with a 4–5 mm multi-leaf collimator linear accelerator (Linac) system equipped with cone beam CT guidance and 6 degree of freedom couch rotation, or WBRT. SRS and FSRT were used solely for the treatment of BrM and not LMD. The immobilization and planning target volume varied depending on the platform used and has been previously described by our group16. WBRT was delivered, most commonly, with 20 Gy in 5 fractions. Symptomatic areas of spinal LMD were treated with conventional external beam RT, with doses ranging between 8 Gy in 1 to 20 Gy in 5 fractions. Details of RT treatments are presented in supplementary Table 1.
Study outcomes
We identified LMD through a review of MRI findings, as CSF cytology was not routinely performed at our institution. When scan images were unavailable, the diagnosis was based on MRI reports. LMD cases were classified as classical, nodular or mixed as previously described16. Overall survival (OS) was defined from the time of diagnosis of LMD until the date of death or last follow-up. Brain specific progression-free survival (bsPFS) was defined from the time of LMD diagnosis to the date of radiographic or symptomatic disease progression in the CNS, including both BrM and LMD progression. Standard imaging follow-ups were scheduled every 2–4 months per our institutional protocol and additional imaging was done based on patient symptoms. Alongside determining clinical outcomes, we also aimed to identify predictors of LMD development in MBC patients with BrM.
Statistical analysis
Clinical and treatment characteristics are described with median and interquartile range (IQR) for continuous variables, or frequencies and percentages for categorical variables. Logistic regression was used to investigate potential predictors of LMD. Kaplan-Meier (KM) methods generated estimates of OS and bsPFS, and p-values were calculated using the log-rank (Mantel-Cox) test. Cox proportional hazards regression was used to estimate hazard ratios (HR) and identify predictors of OS and bsPFS. Univariable analyses (UVA) were performed for all covariates. Multivariable analysis (MVA) excluded treatment covariates as clinical characteristics form the basis for decisions about therapy. Bayesian Information Criteria (BIC) determined best models from all subsets of covariates. Logistic regression model fit was assessed with the Hosmer-Lemeshow fit statistic. The proportional-hazards assumption was appraised by visually inspecting graphs of Schoenfeld residuals and testing their independence over time. All analyses were performed using R* software version 4.3.217. All p-values were two-sided and statistical significance was determined using the traditional p-value of < 0.05.
Results
Patient characteristics
Out of 691 MBC patients referred for radiation to BrM and/or LMD, 161 cases of LMD were identified with a median follow-up of 5.5 months (interquartile range [IQR] 1.4–16.8) for the entire cohort. Among patients who developed LMD, the median time from BrM to LMD was 14.7 weeks (IQR 4.3–56.7), while the median LMD-free survival for the full cohort was 24.2 months (95% CI 19–35) (Supp Fig. 1).The BC subtypes of patients with LMD were as follows: 51% HR + HER2-, 25% HER2+, and 24% triple-negative breast cancer (TNBC). Median ages at the time of initial breast cancer and LMD diagnoses were 48 years (IQR 40–57) and 54 years (IQR 45–63), respectively. The primary sites of extracranial metastases were bone (75%, 121/161), liver (55%, 88/161), and lung (47%, 76/161). LMD presentation varied; about one-third (50/161) had isolated LMD without concurrent BrM, whereas late LMD, over > 1 year post-BrM, was less common (15%, 25/161). Nodular LMD was the most common subtype (53%, 86/161), followed by classical (36%, 58/161) and mixed LMD (6%, 9/161). Brain-only LMD occurred in 58% of patients, combined brain and spinal LMD in 35%, and spine-only LMD was less common (representing 7% of our cohort). Among patients with LMD, 83% with brain-only involvement received WBRT, while 73% with spine-only disease received spine RT. For those with combined brain and spine LMD, 64% received RT to both areas. The most common regimens for WBRT were 20 Gy/5 (59%), and 30 Gy/10 (15%), while spine RT was most often delivered using 20 Gy/5 (48%) and 8 Gy/1 (10%) (Supp Table 1). No patients in our cohort received SRS or FSRT for the treatment of LMD. Detailed baseline clinical and treatment characteristics for the overall and LMD subgroups are presented in Table 1 and Supplementary Table 2, respectively.
Predictors of OS
The median OS of patients with LMD was 5.5 months (Supp Fig. 2). Patients with HER2-positive disease demonstrated markedly longer OS compared to those with HR + HER2- and triple negative MBC (HR 0.38, 95% CI: 0.2–0.75, p = 0.002). The median OS of patients with HER2 + LMD was 15.4 months (2.6, not reached) as compared to 5.1 months (2.5, 8.7) in patients with HR + HER2- and 3.7 months (1.8, NR) in those with TNBC (Fig. 1). Long-term survival, defined as an OS of over two years, was strongly associated with receipt of HER2 + systemic treatment both at the time and following LMD diagnosis (Fisher’s test both p < 0.05). The median OS of patients with HER2 + LMD receiving HER2-directed therapy was 23 months, compared to 3.1 months for those who did not receive HER2-directed therapy (p = 0.2) (Supp Fig. 3). Conversely, both low Karnofsky Performance Status (KPS) score (< 60) (HR 4.07, 95% CI: 2.09–7.93, p < 0.01) and longer time from BrM to LMD (HR 1.01, 95% CI: 1.003–1.02, p < 0.05) were associated with shorter OS (Supp Fig. 4). Neither the type nor location of LMD was associated with overall survival. Given potential changes in systemic therapies over time, we also assessed the impact of period of LMD diagnosis (2013–2019 vs. 2005–2012) and found no difference in OS. UVA and MVA results are summarized in Table 2.
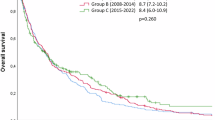
Predictors of brain-specific PFS
The overall bsPFS in our study was 4.1 months (2.6–6.1) (Supp Fig. 5). In MVA, patients with HER2 + LMD had significantly longer bsPFS (HR 0.47, 95% CI: 0.25–0.86, p < 0.05) as compared to patients with HR+/HER2- and triple negative MBC (Table 3). The median bsPFS of patients with HER2 + LMD was 6.7 months (2.4, 25.1) as compared to 4.9 months (3, 6.3) and 2 months (1.7–6.4) in patients with HR + HER2- or TNBC (Fig. 2). In contrast, both low KPS score (< 60) (HR 3.41, 95% CI: 1.71–6.8, p < 0.01) and longer time from BrM to LMD (HR 1.01, 95% CI: 1.003–1.02, p < 0.05) were associated with shorter bsPFS (Supp Fig. 6). There was no association between LMD subtype, or time period of LMD diagnosis and risk of bsPFS.
Impact of RT dose on LMD outcomes
To evaluate whether radiotherapy dose influenced survival after LMD, we calculated the biologically effective dose (BED) at the time of treatment using an α/β ratio of 10. In the subgroup of patients with brain-only LMD who received WBRT (n = 78), a higher BED (≥ 30 Gy) was significantly associated with longer overall survival (HR 0.25, 95% CI: 0.08–0.73, p < 0.05) on multivariable analysis, alongside HER2-positive status and KPS ≥ 60 (Supp Table 3). The most common fractionation schedule in the < 30 Gy group was 20 Gy in 5 fractions, while 30 Gy in 10 fractions was most common among those receiving ≥ 30 Gy. BED was not associated with bsPFS. We restricted this analysis to brain-only patients to minimize confounding from spinal LMD cases, which were few in number and treated heterogeneously.
Factors associated with the development of LMD
In the overall cohort of MBC patients with BrM treated with RT, patients with LMD were more likely to be younger at breast cancer diagnosis (OR 1.31, 95% CI: 1.11–1.54, p = 0.001), have ER + tumors (OR 1.63, 95% CI: 1.10–2.40, p = 0.01), a history of surgical intervention for brain metastases (OR 3.04, 95% CI: 1.68–5.52, p = 0.0002) and less likely to have received prior WBRT (OR 0.27, 95% CI: 0.15–0.47, p < 0.0001). Among patients who underwent surgery, which in our cohort consisted exclusively of craniotomy with tumor resection, the nodular form of LMD was predominant, accounting for 65% of cases in this group. The type of systemic treatment administered at or soon after the diagnosis of BrM was not associated with the risk of LMD development (Supp Table 4).
Discussion
In this study, we demonstrate that patients with HER2 + metastatic breast cancer and leptomeningeal disease had improved clinical outcomes compared to those with HER2 − disease, with a median OS of 15.4 months and less than 6 months respectively. Furthermore, within the HER2 + cohort, those receiving HER2-directed therapy had a longer median OS of 23 months compared to 3.1 months for those who did not receive such treatment. These findings underscore the efficacy of HER2 + directed agents in patients with HER2 + MBC complicated by LMD, and highlights the need to integrate these therapies into standard of care through further prospective studies. While we did not collect data on the specific HER2-directed therapies administered, the standard of care during the study period (2005–2019) would have included Trastuzumab (Herceptin) with or without Pertuzumab and/or T-DM1 (Trastuzumab emtansine), which were considered standard therapies for HER2 + metastatic breast cancer. The lack of survival differences between time periods may reflect the comparable efficacy of these agents. Newer therapies with improved CNS activity, such as Trastuzumab deruxtecan (T-DXd), were not yet available and thus not represented in this cohort.
The introduction of novel HER2-targeted therapies capable of crossing the blood-brain barrier have revolutionized the management of MBC patients with intracranial disease, but their role in LMD remains unclear. Since the completion of our study, T-DXd has emerged as a new standard of care for patients with metastatic HER2 + breast cancer, demonstrating significantly improved intracranial activity and encouraging results in early studies specifically evaluating patients with LMD18. The systemic treatment landscape for HER2 + LMD has been recently reviewed by Bartsch et al.14. A recent case series by Alder et al. showed that all eight heavily pre-treated patients with HER2 + MBC who had progressing LMD experienced clinical benefit with T-DXd, and half achieved a clinical objective response with a median OS of 10.5 months19. The efficacy of T-DXd in patients with HER2 + LMD is further supported by results of the multi-centre retrospective “ROSET-BM” cohort study; the 12-month PFS and 12-month OS among 19 patients treated with T-DXd for HER2 + LMD were 60.7% and 87.1%, respectively20. Cohort 5 of the DEBBRAH trial plans to enroll a total of 7 patients with HER2 + or HER2-low MBC and LMD21. Recent investigations have also indicated that combining Neratinib and Capecitabine may have efficacy among patients with HER2 + LMD, alongside intrathecal Trastuzumab administration22,23. Furthermore, ongoing prospective clinical trials such as NCT06016387 are assessing the combination of Tucatinib with brain and/or spinal RT in patients with HER2 + LMD. Such studies are beginning to address the historical lack of inclusion of LMD patients in clinical trials24.
The poor survival outcomes observed in patients with HER2-ve MBC in our study confirms the critical need for effective CNS-penetrating therapeutic agents for this cohort. Current research is actively investigating potential treatments that can effectively penetrate the blood-brain barrier in both HR + and TNBC subtypes. Single-agent Abemaciclib demonstrated intracranial activity in a non-randomized phase 2 study, with a reduction in the volume of target BrM observed in 38% of 58 patients with HR+/HER2- MBC25. Notably, the trial included a small cohort of 10 patients with MBC and LMD, among whom one patient achieved a confirmed complete clinical response. Although the ASCENT study established the efficacy of Sacituzumab Govitecan (SG) in patients with metastatic TNBC, it excluded patients with BrM from its primary endpoints26. However, a post-hoc analysis of patients who had stable BrM for > 4 weeks revealed that the use of SG was association with a slightly longer PFS but numerically shorter OS compared to the use of standard chemotherapy27. In a retrospective real world analysis of SG’s efficacy among 33 patients with MBC and CNS metastases, the real-world CNS-specific PFS and OS were 12.7 weeks and 29.1 weeks, respectively. Among 8/33 (24%) patients with LMD treated with SG, the CNS-specific response rate was 14.3% and the median OS was 15.8 weeks28. Immunotherapy with the PD-L1 inhibitor Pembrolizumab has also shown promise, demonstrating intracranial activity in 57 patients with BrM from various cancers, including 35 with MBC, achieving an intracranial benefit rate of 42.1%29. Additionally, a single-arm Phase II study combining Pembrolizumab with Ipilimumab (a CTLA-4 inhibitor) in 18 patients with LMD from various histologies (44% with MBC, n = 8) found the combination to be safe and associated with a 3-month OS rate of 44%30.
Given the strong data supporting the intracranial efficacy of T-DXd among patients with HER2 + active brain metastases4,31 coupled with the efficacy of T-DXd among patients with HER2-low disease in the DESTINY-Breast04 trial18, the TUXEDO-4 trial is evaluating the efficacy of T-DXd among patients with active HER2-low brain metastases [NCT06048718]. The TUXEDO-3 clinical trial [NCT05865990i] is evaluating the efficacy of a novel HER3-targeted antibody-drug conjugate patritumab detuxtecan (HER3-Dxd) among patients with metastatic breast cancer or NSCLC with active brain metastases and/or LMD, irrespective of HER2-status. The results of these trials are eagerly awaited (supp Table 5).
While our study was not designed to identify predictors of LMD in patients with BrM referred for RT, it revealed that a history of surgical resection and younger age at diagnosis were associated with a higher risk of LMD. Surgical management of BrM could theoretically increase the risk of CSF seeding, with research indicating a higher incidence of LMD in patients treated with surgical resection compared to SRS alone. Nguyen et al. showed in his analysis of 235 patients with BrM that surgical cavities were at higher risk of LMD as compared to intact lesions16. Consistent with this observation, Johnson et al. revealed that patients who underwent surgery followed by SRS had a cumulative one-year LMD incidence of 16.9% compared to 5.2% in those treated without surgery32. The role of preoperative radiation in reducing LMD risk is also increasingly recognized with several trials designed to answer this question33. For instance, in a retrospective study of 180 patients treated with SRS, the rate of LMD in patients treated with preoperative SRS was 3.2% compared to 16.6% in those treated with post-operative SRS34. In parallel, our findings suggest that prior WBRT may reduce the risk of LMD, reinforcing the idea that early, comprehensive cranial irradiation could offer a protective effect. Critically, among patients with brain-only LMD, higher-dose RT (BED ≥ 30 Gy) was linked to significantly better survival, pointing to a potential dose–response relationship. Together, these data highlight the need to carefully consider not just when but how much cranial RT is delivered especially in high-risk patients.
One of the challenges in diagnosing LMD lies on the reliance of MRI and cerebrospinal fluid (CSF) is not routinely obtained. Early identification of patients with BrM at high risk for LMD may allow for earlier interventions and potentially improved outcomes. Traditionally, the diagnosis of LMD has relied on MRI imaging and CSF analysis for the presence of malignant cells. However, these tools can often result in false positives and negatives, leading to either delayed or unnecessary treatments35. Recently, the use of circulating tumor DNA (ctDNA) in CSF has been proposed as a potential tool for the early diagnosis of LMD, with some studies demonstrating higher sensitivity in detecting LMD compared to CSF cytology and MRI36. Future studies should also focus on identifying factors associated with the development of LMD, as these could be instrumental in screening programs aimed at early detection and treatment, provided this approach demonstrates a clear benefit in terms of survival or quality of life. Additionally, the potential role of proton CSI in high-risk patients should be explored, as early intervention with CSI before gross manifestations of LMD could potentially influence survival, although this remains a theoretical approach.
To our knowledge, this study represents the largest investigation into LMD in MBC. Despite its contributions, the study is subject to several limitations. Firstly, this study was limited by its retrospective nature and single-center analysis. Furthermore, our analysis relied primarily on MRI imaging for the diagnosis of LMD, without confirmatory CSF analysis, which may lead to overdiagnosis or misclassification in some cases. The study period (2005–2019) spans an era of evolving breast cancer therapies, including the subsequent approval of T-DX), which was not available to patients in our cohort. While most patients likely received Trastuzumab and/or T-DM1, we did not collect detailed data on specific HER2-directed agents, chemotherapy regimens, or endocrine therapies. This limits our ability to assess the differential impact of systemic treatments in use during the study period, or to evaluate the potential effects of newer agents on LMD risk and outcomes. The limited use of CSI among our cohort, similarly, restricts our ability to assess the full therapeutic impact of these advances. Additionally, we lacked data on extracranial disease progression or response, limiting assessment of its prognostic impact on survival. The study may also be influenced by survivorship bias, as the retrospective nature of our analysis is more likely to capture data from long-term survivors. Finally, the absence of genetic and molecular data in our dataset limits our ability to explore the role of specific biomarkers in predicting LMD risk and response to treatment. In addition, the lack of toxicity and quality-of-life data limits our understanding of treatment impact from the patient perspective, an area that is increasingly recognized as crucial for personalized cancer care.
In summary, patients with HER2 + MBC and LMD had longer bsPFS and OS compared to those with HER2 − disease. In contrast, spinal LMD was associated with shorter bsPFS and poor performance status was associated with shorter OS. These results support the clinical efficacy of HER2 + directed therapies in patients with HER2 + LMD and highlight the need for more effective CNS-penetrating therapies for those with HER2- disease.
Data availability
The data generated and analyzed in this study are available upon reasonable request from the corresponding author.
References
Franzoi, M. A. & Hortobagyi, G. N. Leptomeningeal carcinomatosis in patients with breast cancer. Crit. Rev. Oncol. Hematol. 135, 85–94 (2019).
Lamba, N., Wen, P. Y. & Aizer, A. A. Epidemiology of brain metastases and leptomeningeal disease. Neuro-Oncol 23(9), 1447–1456 (2021).
Montemurro, F. et al. Trastuzumab emtansine (T-DM1) in patients with HER2-positive metastatic breast cancer and brain metastases: exploratory final analysis of cohort 1 from KAMILLA, a single-arm phase IIIb clinical trial. Ann. Oncol. 31(10), 1350–1358 (2020).
Bartsch, R. et al. Trastuzumab deruxtecan in HER2-positive breast cancer with brain metastases: a single-arm, phase 2 trial. Nat. Med. 28(9), 1840–1847 (2022).
Lin, N. U. et al. Tucatinib vs placebo, both in combination with trastuzumab and capecitabine, for previously treated ERBB2 (HER2)-positive metastatic breast cancer in patients with brain metastases: updated exploratory analysis of the HER2CLIMB randomized clinical trial. JAMA Oncol. 9(2), 197–205 (2023).
Kordbacheh, T., Law, W. Y. & Smith, I. E. Sanctuary site leptomeningeal metastases in HER2-positive breast cancer: a review in the era of trastuzumab. Breast 26, 54–58 (2016).
Znidaric, T. et al. Breast cancer patients with brain metastases or leptomeningeal disease: 10-year results of a National cohort with validation of prognostic indexes. Breast J. 25(6), 1117–1125 (2019).
Gauthier, H. et al. Survival of breast cancer patients with meningeal carcinomatosis. Ann. Oncol. 21(11), 2183–2187 (2010).
Scott, B. J., Oberheim-Bush, N. A. & Kesari, S. Leptomeningeal metastasis in breast cancer\u2014a systematic review. Oncotarget 7(4), 3740 (2016).
Abouharb, S. et al. Leptomeningeal disease and breast cancer: the importance of tumor subtype. Breast Cancer Res. Treat. 146, 477–486 (2014).
Niwińska, A., Rudnicka, H. & Murawska, M. Breast cancer leptomeningeal metastasis: propensity of breast cancer subtypes for leptomeninges and the analysis of factors influencing survival. Med. Oncol. 30, 1–8 (2013).
Huang, Z. et al. A nomogram for predicting survival in patients with breast cancer brain metastasis. Oncol. Lett. 15(5), 7090–7096 (2018).
Le Rhun, E., Preusser, M., van den Bent, M., Andratschke, N. & Weller, M. How we treat patients with leptomeningeal metastases. ESMO Open. 4, e000507 (2019).
Bartsch, R., Jerzak, K. J., Larrouquere, L., Muller, V. & Le Rhun, E. Pharmacotherapy for leptomeningeal disease in breast cancer. Cancer Treat. Rev. 102653. (2023).
Yang, T. J. et al. Clinical trial of proton craniospinal irradiation for leptomeningeal metastases. Neuro-Oncol 23(1), 134–143 (2021).
Nguyen, T. K. et al. Predictors of leptomeningeal disease following hypofractionated stereotactic radiotherapy for intact and resected brain metastases. Neuro-Oncol 22(1), 84–93 (2020).
R Core Team. R: A language and environment for statistical computing. https://www.R-project.org/ (R Foundation for Statistical Computing, 2023).
Hurvitz, S. A. et al. Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: updated results from DESTINY-Breast03, a randomized, open-label, phase 3 trial. Lancet 401(10371), 105–117 (2023).
Alder, L. et al. Durable responses in patients with HER2 + breast cancer and leptomeningeal metastases treated with trastuzumab deruxtecan. NPJ Breast Cancer. 9(1), 19 (2023).
Pellerino, A. et al. Neratinib and capecitabine for the treatment of leptomeningeal metastases from HER2-positive breast cancer: a series in the setting of a compassionate program. Cancers 14(5), 1192 (2022).
Niikura, N. et al. Treatment with trastuzumab deruxtecan in patients with HER2-positive breast cancer and brain metastases and/or leptomeningeal disease (ROSET-BM). NPJ Breast Cancer. 9(1), 82 (2023).
Perez-Garcia, J. M. et al. Trastuzumab deruxtecan in patients with central nervous system involvement from HER2-positive breast cancer: the DEBBRAH trial. Neuro-Oncol 25(1), 157–166 (2023).
Oberkampf, F. et al. Phase II study of intrathecal administration of trastuzumab in patients with HER2-positive breast cancer with leptomeningeal metastasis. Neuro-Oncol 25(2), 365–374 (2023).
Sharma, A. E. et al. Assessment of phase 3 randomized clinical trials including patients with leptomeningeal disease: a systematic review. JAMA Oncol. 9(4), 566–567 (2023).
Tolaney, S. M. et al. A phase II study of abemaciclib in patients with brain metastases secondary to hormone receptor-positive breast cancer. Clin. Cancer Res. 26(20), 5310–5319 (2020).
Bardia, A. et al. ASCENT: a randomized phase III study of sacituzumab Govitecan vs treatment of physician\u2019s choice in patients with previously treated metastatic triple-negative breast cancer. Ann. Oncol. 31, S1149–S1150 (2020).
Hurvitz, S. A. et al. Subgroup analyses from the phase 3 ASCENT study of sacituzumab Govitecan in metastatic triple-negative breast cancer. NPJ Breast Cancer. 10(1), 33 (2024).
Grinda, T. et al. Real-world outcomes with sacituzumab Govitecan among breast cancer patients with central nervous system metastases. Neuro-Oncol Adv. 6(Suppl 1), i24–i24 (2024).
Brastianos, P. K. et al. Pembrolizumab in brain metastases of diverse histologies: phase 2 trial results. Nat. Med. 29(7), 1728–1737 (2023).
Brastianos, P. K. et al. Phase II study of ipilimumab and nivolumab in leptomeningeal carcinomatosis. Nat. Commun. 12(1), 5954 (2021).
Harbeck, N. et al. Trastuzumab deruxtecan in HER2-positive advanced breast cancer with or without brain metastases: A phase 3b/4 trial. Nat. Med. 1–10 (2024).
Johnson, M. D. et al. Surgical resection of brain metastases and the risk of leptomeningeal recurrence in patients treated with stereotactic radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 94(3), 537–543 (2016).
Das, S. et al. A phase III multicenter randomized controlled trial of preoperative vs postoperative stereotactic radiosurgery for patients with surgically resectable brain metastases. BMC Cancer. 22(1), 1–8 (2022).
Patel, K. R. et al. Comparing preoperative with postoperative stereotactic radiosurgery for resectable brain metastases: a multi-institutional analysis. Neurosurgery 79(2), 279–285 (2016).
Glantz, M. J. et al. Cerebrospinal fluid cytology in patients with cancer: minimizing false-negative results. Cancer 82(4), 733–739 (1998).
White, M. D. et al. Detection of leptomeningeal disease using cell-free DNA from cerebrospinal fluid. JAMA Netw. Open. 4(8), e2120040 (2021).
Author information
Authors and Affiliations
Contributions
B.I, and K.J.J. contributed equally to study design, data collection, analysis, and manuscript preparation. V.M performed statistical analyses and assisted in data interpretation. H.C, E.W, S.M, C.L.T, J.D., D.D, C.H, A.S contributed to data collection/interpretation, and contributed to manuscript revisions and clinical input. A.S. H.S. supervised the study, contributed to data collection/interpretation, and critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics
This study was approved by the institutional review board of Sunnybrook Hospital and adhered to the principles outlined in the “World Medical Association Declaration of Helsinki: Research Involving Human Subjects.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Id Said, B., Jerzak, K.J., Chen, H. et al. Survival outcomes among patients with breast cancer and leptomeningeal disease. Sci Rep 15, 24170 (2025). https://doi.org/10.1038/s41598-025-07191-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07191-3
Keywords
This article is cited by
-
Clinical–pathological patterns and prognosis of young women with breast cancer brain metastases: a single-center retrospective study
Journal of Neuro-Oncology (2025)