Abstract
This research aims to summarize the ultrasound features and pregnancy outcomes of closure of ductus venosus, providing a basis for prenatal consultation and clinical management. A retrospective cohort study was conducted at the Hunan Provincial Maternal and Child Health Care Hospital in China, involving pregnant patients diagnosed with ductus venosus closure between January 2020 and December 2023. Data on maternal age, gestational age, ultrasound findings, timing and method of pregnancy termination, and pregnancy outcomes were collected. Twenty-five pregnant women were diagnosed with ductus venosus closure during the study period. Among them, 12 cases (48%, 12/25) were associated with other abnormalities. Of these, 4 cases (33.33%, 4/12) resulted in live births, while 8 cases (66.67%, 8/12) led to induced labor due to major abnormalities. The remaining 13 cases (52%, 13/25) involved isolated ductus venosus closure, with 1 case (7.69%, 1/13) of intrauterine fetal death and 12 cases (92.31%, 12/13) of successful delivery. The closure of the ductus venosus was primarily characterized by the tramline sign (52%, 13/25) and the cord sign (48%, 12/25) on two-dimensional ultrasound, with no detectable blood flow on Doppler ultrasound imaging. Ductus venosus closure can occur as an isolated finding (52%) or in conjunction with other abnormalities (48%), with cardiac anomalies being the most common. The closure of ductus venosus can occur during the second and third trimesters of pregnancy. The two-dimensional ultrasound showing tramline sign or cord sign, along with the absence of blood flow on Doppler ultrasound imaging, should raise suspicion of closure of ductus venosus.
Similar content being viewed by others
Introduction
The ductus venosus is a crucial blood vessel in fetal circulation, allowing oxygenated blood from the placenta to bypass the liver and preferentially flow through the right atrium and foramen ovale to the left atrium. Structurally, the ductus venosus has an hourglass shape due to the narrow isthmus near its entrance and its connection to the inferior vena cava (IVC) distally, with an internal diameter of only 1–2 mm1. Its relatively fixed position makes it suitable for standardized ultrasound examination, where it is best visualized in the sagittal section of the fetus or on a transverse section of the fetal abdomen.
Postnatally, the ductus venosus gradually closes and becomes the ligamentum venosum. Intrauterine closure of the ductus venosus is exceedingly rare and scarcely documented in the literature, particularly concerning prenatal ultrasound characteristics2. Given its rarity, the pathogenesis and prognosis of ductus venosus closure remain unclear. This retrospective study aims to summarize the prenatal sonographic features and outcomes of closure of ductus venosus, providing insights for prenatal diagnosis and counseling.
Materials and methods
Subjects
We conducted a retrospective analysis of all cases diagnosed with prenatal ductus venosus closure at the Hunan Provincial Maternal and Child Health Care Hospital between January 2020 and December 2023. All cases in this study were accidentally discovered during routine systematic screening. Data on maternal age, gestational age, prenatal sonographic features, timing and method of pregnancy termination, and outcomes were reviewed.
Prenatal ultrasound examination
Standardized fetal ultrasound examinations were performed by experienced sonographers using GE Voluson E6, E8, E10 (GE Healthcare, Milwaukee, WI, USA) and Samsung HERA W10 (Samsung Healthcare, Korea) machines. Ultrasonic evaluation of the ductus venosus was included in routine screening for both low-risk and high-risk patients. Ductus venosus closure was diagnosed based on the absence of flow on color Doppler ultrasound or the appearance of the ductus venosus as closed on standard two-dimensional views.
Statistical analysis
Numerical data were presented as mean ± standard deviation (SD). Fisher’s exact test was performed to compare pregnancy outcomes between isolated closure of ductus venosus and closure of ductus venosus with other abnormalities. P < 0.05 was considered statistically significant.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Hunan Provincial Maternal and Child Health Care Hospital (consent number: 2024-S051). The committee granted an exemption from informed consent for this retrospective study. All procedures involving human participants followed the ethical standards of the institutional and/or national research committee and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Results
Subject information
Between January 2020 and December 2023, 25 fetuses were diagnosed with ductus venosus closure at the Department of Ultrasound, Hunan Provincial Maternal and Child Health Care Hospital. The average maternal age was 30 ± 5 years, and the average gestational age at diagnosis was 29.18 ± 4.93 weeks. Among these cases, one involved a twin pregnancy, while the others were singleton pregnancies.
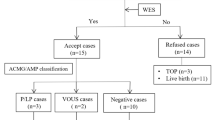
Of the 25 cases, 12 (48%, 12/25) were associated with other abnormalities, with 4 cases (33.33%, 4/12) resulting in live births and 8 cases (66.67%, 8/12) leading to induced labor due to major abnormalities. The 13 cases (52%, 13/25) of isolated ductus venosus closure included 1 case (7.69%, 1/13) of intrauterine fetal death and 12 cases (92.31%, 12/13) of live births. Among the 16 deliveries, 10 were by cesarean section, and 6 were vaginal deliveries, with an average gestational age of 38.29 ± 2.13 weeks and a mean birth weight of 2981.25 ± 566.83 g. Figure 1 shows the diagnosis and pregnancy outcomes of closure of ductus venosus in 25 included cases.
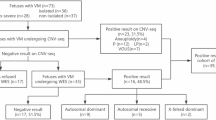
Reviewing electronic medical records and follow-up phone calls, no abnormalities were detected in the ductus venosus during the first trimester routine screening in any cases. Eleven cases (44%, 11/25) were identified during the second trimester screening, while the remaining 14 cases (56%, 14/25) were detected in the third trimester.
Prenatal ultrasonic characteristics
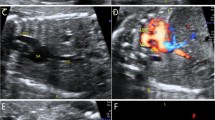
There were two main ultrasonic characteristics of closure of ductus venosus in this study. First, the ductus venosus of 13 fetuses (52%, 13/25) was slightly narrow, with an inner diameter of less than 1 mm, showing two parallel linear high-echo, similar to track, so we call it tramline sign. In addition, no blood flow signal was detected in both color and pulse Doppler ultrasound, as shown in Fig. 2. The second ultrasonic feature was the complete occlusion of ductus venosus, and it was manifested as a cord-like high-echo structure, which is called the cord sign. Similarly, no blood flow signal was detected, as shown in Fig. 3. The cord sign was identified in 12 cases (48%, 12/25). No abnormal intrahepatic or extrahepatic drainage was found in all cases.
Ultrasound images of tramline sign of closure of ductus venosus. (A) and (B) are ultrasound images of case 4 and case 20, respectively. (C) and (D) are two-dimensional and color Doppler ultrasound images of case 9, respectively. The white arrow shows the tramline sign. DV ductus venosus, IVC inferior vena cava, UV umbilical vein.
Prenatal associated features and pregnancy outcome in fetal closure of ductus
In our study, 12 cases of closure of ductus venosus had associated anomalies. Additional findings were only cardiac abnormalities (20%, 5/25) and isolated extracardiac anomalies (8%, 2/25). 5 fetuses (20%, 5/25) showed multiple system abnormalities. Cardiac anomalies were the most common, appearing in 10 cases, including aberrant right subclavian artery (ARSA), persistent left superior vena cava (PLSVC), ventricular septal defect (VSD), atrioventricular septal defect (AVSD) and arrhythmia, etc. Other extracardiac anomalies include intracranial abnormalities, facial deformities, and congenital urogenital abnormalities. Among the 8 induced fetuses, all pregnant women refused to undergo autopsy, and in one case the CNV-seq of aborted tissue was negative. For the case of fetal death in utero, the pregnant woman also refused to undergo autopsy, so it was unknown whether the fetal death was directly related to closure of ductus venosus. In 16 cases of childbirth, closure of ductus venosus was confirmed after the fetuses were delivered, and the overall postnatal survival rate was 100%. The pregnancy outcome of isolated closure of ductus venosus better than that of closure of ductus venosus combined with other abnormalities, and the difference was statistically significant (P < 0.05). Table 1 shows the ultrasound characteristics and pregnancy outcomes of 25 cases of closure of ductus venosus.
Discussion
The ductus venosus is a vital vessel during fetal development, playing a significant role in regulating blood circulation. Over recent decades, ultrasound examination of the fetal ductus venosus has become an area of increasing interest. As awareness among sonographers grows, more cases of fetal ductus venosus anomalies, such as agenesis, are being reported3,4,5,6. However, intrauterine closure of the ductus venosus remains exceedingly rare and underreported, particularly regarding prenatal ultrasound diagnosis2. To the best of our knowledge, this is the first retrospective study to include such a large number of patients and provide detailed accounts of prenatal ultrasound diagnostic experience and pregnancy outcomes associated with ductus venosus closure.
While closure of ductus venosus typically occurs postnatally, our study demonstrates that it can also occur during the second and third trimesters of pregnancy. It is well known that fetal circulation depends on three physiological shunts: the ductus venosus, foramen ovale, and ductus arteriosus. These shunts ensure that highly oxygenated blood travels from the placenta to the brain and heart of the fetus, bypassing the liver and lung circulation. The ductus venosus regulates its flow by adjusting the pressure gradient between the umbilical vein and the heart. Therefore, an ultrasonic evaluation of the fetal ductus venosus is crucial. Diagnosing closure of ductus venosus requires distinguishing it from ductus venosus agenesis, a congenital anomaly characterized by the absence of the ductus venosus during routine morphological screening. In this study, all pregnant women showed no ductus venosus abnormalities during the nuchal translucency (NT) examination at 11–13+ 6 weeks, making it possible to differentiate ductus venosus closure from agenesis.
Differed from that of other veins, the ductus venosus showed narrowing at its origin and progressive dilatation towards the subdiaphragmatic vestibulum, giving the lumen an hourglass appearance1. Previous studies have shown that peak systolic velocities in the ductus venosus are in the range of 40–80 cm / second, and the ductus venosus flow velocity is approximately three times higher than flow velocity in the umbilical vein or IVC7,8,9. Color Doppler is often applied to identify the isthmus of the ductus venosus, which is often apparent by its high forward velocities or aliasing, in a mid-sagittal or abdominal transverse plane10. Therefore, if color Doppler ultrasound shows no blood flow in the ductus venosus, and the possibility of closure of ductus venosus should be considered. In our study, closure of ductus venosus was mainly manifested as two major ultrasonic signs on two-dimensional ultrasound: tramline sign and cord sign. Meanwhile, it had no detectable flow by Doppler ultrasound imaging. Based on our diagnostic experience, we believe that both two-dimensional and Doppler ultrasound features are indispensable for the diagnosis of closure of ductus venosus.
Many studies have shown that absence of ductus venosus was often accompanied by intrahepatic or extrahepatic drainage of the umbilical vein4,5,6,11,12,13. In the 25 cases of this study, no intrahepatic or extrahepatic drainage of the umbilical vein was detected, the reason for which is currently unknown. We speculate that it may be related to the closure time of the ductus venosus in the second and third trimester of pregnancy.
Our study showed that the prognosis of closure of ductus venosus depends on the combination of abnormalities. In this study, closure of ductus venosus can be isolated (52%) or associated with other abnormalities (48%), of which cardiac abnormalities were the most common. In pregnancies with apparently isolated closure of ductus venosus, the prognosis is good. In our series of 13 such cases, there were 12 healthy live births and only one intrauterine death occurred. For 12 cases accompanied by other abnormalities, especially in the 8 cases (66.67%) with major abnormalities, considering the possibility of poor prognosis after birth and heavy economic burden, these pregnant women chose to terminate their pregnancies. In 4 cases with minor abnormalities, the prognosis is good with the live birth of grown normal babies.
Conclusions
In summary, closure of ductus venosus can occur in second and third trimester of pregnancy. The two-dimensional ultrasound showing tramline sign or cord sign, and Doppler ultrasound not detecting blood flow, should be highly suspected of closure of ductus venosus.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Mavrides, E., Moscoso, G., Carvalho, J. S., Campbell, S. & Thilaganathan, B. The human ductus venosus between 13 and 17 weeks of gestation: histological and morphometric studies. Ultrasound Obstet. Gynecol. 19, 39–46 (2002).
Achiron, R. et al. Abnormalities of the fetal central veins and umbilico-portal system: prenatal ultrasonographic diagnosis and proposed classification. Ultrasound Obstet. Gynecol. 16, 539–548 (2000).
Sau, A., Sharland, G. & Simpson, J. Agenesis of the ductus venosus associated with direct umbilical venous return into the heart–case series and review of literature. Prenat Diagn. 24, 418–423 (2004).
Iliescu, D. G. et al. Agenesis of ductus venosus in sequential first and second trimester screening. Prenat Diagn. 34, 1099–1105 (2014).
Strizek, B. et al. Prenatal diagnosis of agenesis of ductus venosus: A retrospective study of anatomic variants, associated anomalies and impact on postnatal outcome. Ultraschall Med. 40 (3), 333–339 (2019).
Nagy, R. D. et al. Ductus venosus agenesis and portal system Anomalies-Association and outcome. Biology 11, 548 (2022).
Kiserud, T., Eik-Nes, S. H., Blaas, H. G. & Hellevik, L. R. Ultrasonographic velocimetry of the fetal ductus venosus. Lancet 338, 1412–1414 (1991).
Huisman, T. W., Stewart, P. A. & Wladimiroff, J. W. Ductus venosus blood flow velocity waveforms in the human fetus–a doppler study. Ultrasound Med. Biol. 18, 33–37 (1992).
Sherer, D. M., Fromberg, R. A. & Divon, M. Y. Prenatal ultrasonographic assessment of the ductus venosus: a review. Obstet. Gynecol. 88 (4 Pt 1), 626–632 (1996).
Seravalli, V., Miller, J. L., Block-Abraham, D. & Baschat, A. A. Ductus venosus doppler in the assessment of fetal cardiovascular health: an updated practical approach. Acta Obstet. Gynecol. Scand. 95 (6), 635–644 (2016).
Contratti, G. et al. Absence of the ductus venosus: report of 10 new cases and review of the literature. Ultrasound Obstet. Gynecol. 18, 605–609 (2001).
Garcia-Delgado, R. et al. Echographic features and perinatal outcomes in fetuses with congenital absence of ductus venosus. Acta Obstet. Gynecol. Scand. 96, 1205–1213 (2017).
Chaoui, R., Heling, K. S. & Karl, K. Ultrasound of the fetal veins part 1: the intrahepatic venous system. Ultraschall Med. 35, 208–228 (2014).
Funding
The study was supported by the grant from The Hunan Provincial Hospital of Maternal and Child Health Care’s High-Level Talent Development Scheme.
Author information
Authors and Affiliations
Contributions
M.X.Z. designed and wrote the article; S.Z and M.H.L. were responsible for the data collection. Y.C.L. contributed to study design. All authors contributed to and approved of the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, M., Zhang, S., Liu, M. et al. Prenatal ultrasound diagnosis and pregnancy outcomes of closure of ductus venosus: a single‑center retrospective study. Sci Rep 15, 23453 (2025). https://doi.org/10.1038/s41598-025-07239-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-07239-4