Abstract
Both anti-thymocyte globulin (ATG) and post-transplant cyclophosphamide (PTCy) have shown prophylactic effects on graft-versus-host disease (GVHD) in multiple phase III studies. We conducted a comparative study of for low dose ATG (thymoglobulin) versus PTCy for GVHD prophylaxis in peripheral blood stem cell transplantation (PBSCT). The ATG (n = 67) and PTCy (n = 40) groups included patients enrolled in multicenter phase II studies (JSCT-ATG15 and JSCT-PTCY19, respectively). The probability of GVHD-free and relapse-free survival at 2 years as the primary endpoint was not significantly different between these two groups (57.9% for ATG vs. 67.8% for PTCy, P = 0.49). Both neutrophil and platelet engraftments were both significantly shorter in the ATG group than in the PTCy group (neutrophils: median 13 days vs. 15 days, P = 0.007; platelets: median 20 days vs. 27 days, P = 0.007). The cumulative incidences of acute and chronic GVHD, relapse, non-relapse mortality, and off-immunosuppressant use were similar between these two groups. The probabilities of overall and progression-free survival were 83.4% and 70.0% in the ATG group and 76.5% and 75.2% in the PTCy group, respectively, with no significant differences. These data indicate that low dose ATG and PTCy are equivalent for GVHD prophylaxis for PBSCT.
Similar content being viewed by others
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is an established curative treatment for patients with severe hematological malignancies. Patients who received HSCT are prepared with a high-dose of chemotherapy and/or total body irradiation, followed by intravenous infusion of hematopoietic stem cells1. After infusion, hematopoietic stem cells will leave circulation and engraft in the bone marrow2. Graft-versus-host disease (GVHD) is one of the most severe complications, and its prophylaxis is essential for successful HSCT. Although calcineurin inhibitor and methotrexate has been used as conventional GVHD prophylaxis, more intensive GVHD prophylaxis is needed for HSCT associated with increased risk of GVHD, including peripheral blood stem cell transplantation (PBSCT)3. Anti-thymocyte globulin (ATG) has shown the GVHD prophylactic effects in a series of phase III randomized control trials4,5,6,7,8,9, and post-transplant cyclophosphamide (PTCy) has also provided remarkable GVHD prophylactic effects on HLA haploidentical HSCT10,11 and has been increasingly used for other types of HSCT. Our study group previously reported two prospective, multicenter, phase II studies, JSCT-ATG15 and JSCT-PTCY19, demonstrating that both low dose ATG and PTCy effectively prevented acute and chronic GVHD in PBSCT12,13. However, the position of the low dose ATG and the PTCy as GVHD prophylaxis in PBSCT other than haploidentical HSCT has not been elucidated.
Materials and methods
Patients and study design
We conducted a comparative study to compare the clinical outcomes of patients with hematological malignancies (acute myeloid leukemia, acute lymphoblastic leukemia, myelodysplastic syndrome, and malignant lymphoma) who underwent PBSCT with low dose rabbit ATG (thymoglobulin) or PTCy as GVHD prophylaxis. Patients with “other leukemia” or “adult T-cell leukemia/lymphoma” were excluded. The ATG group included patients who were enrolled in the multicenter single-arm phase II study (JSCT-ATG15, jRCTs011180012), wherein a total of 2 mg/kg of thymoglobulin was administered on day − 2 and − 1 (1 mg/kg/day) in combination with calcineurin inhibitor (cyclosporine or tacrolimus) and short-term methotrexate for HLA-matched PBSCT using myeloablative conditioning (MAC)12. The PTCy group included patients enrolled in the multicenter single-arm phase II study (JSCT-PTCY19, jRCTs011190009), wherein 50 mg/kg of cyclophosphamide was administered on days 3 and 4 in combination with tacrolimus and mycophenolate mofetil for HLA-matched or HLA 1–2 allele mismatched PBSCT using MAC or reduced intensity conditioning (RIC)13. The brief summaries of both protocols were shown in the supplemental Table 1. The time intervals of patient’s inclusion were from January 2016 to October 2018 in the JSCT-ATG15 study and from March 2020 to July 2021 in the JSCT-PTCY19 study, respectively.
The primary endpoint was the probability of GVHD-free and relapse-free survival (GRFS) at 2 years. The study was performed in accordance with the institutional ethical guidelines, including the World Medical Association Declaration of Helsinki, and was approved by the institutional review board of Hokkaido University (No. 024–0191). Informed consent was obtained from each patient for participation in the study. For patients who could not obtain informed consent, we disclosed the information about this clinical study on the website of our institution and guarantee the opportunity for refusal (opt-out). Since this study is a retrospective study, opt-out disclosure eliminates the need for patient consent.
Definitions
Neutrophil engraftment was defined as an absolute neutrophil count > 0.5 × 109/L on the first three consecutive days, and platelet engraftment was defined as an absolute platelet count > 2.0 × 1010/L without transfusion support on the first seven preceding days. Acute GVHD was graded according to the consensus criteria14, chronic GVHD was graded according to the criteria of the National Institutes of Health Consensus Development Project15. The refined disease risk index (DRI) was determined according to the scoring system as previously described16. Non-relapse mortality (NRM) was defined as death caused by any cause other than relapse. Relapse and causes of death were determined at the discretion of the clinician. Overall survival (OS) was calculated from the day of PBSCT, with patients alive at the time of the last follow-up censored. Progression-free survival (PFS) was calculated from the date of PBSCT until the date of disease recurrence, death from any cause, or the last follow-up for patients without these events being censored. GRFS was defined as the absence of grade III - IV acute or chronic GVHD requiring systemic therapy, relapse, or death17.
Statistical analysis
Statistical analysis was performed using Fisher’s exact test for categorical variables; Mann–Whitney U-test for continuous variables; Kaplan-Meier method and log-rank test for OS, PFS, and GRFS; and Gray’s test for engraftment, acute and chronic GVHD, relapse, NRM, and off-immunosuppressants. We included age, sex, disease, donor, HLA compatibility, conditioning, performance status, DRI, disease status at transplant, and number of CD34 + cells were included as variables in univariate analysis for relapse, NRM, OS, PFS, and GRFS. P < 0.05 was used to determine statistical significance. All analyses were performed with EZR version 1.61 (Jichi Medical University, Saitama Medical Center; http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmedEN.html)18, a graphical user interface for R (The R Foundation for Statistical Computing; http://www.r-project.org) that extends the functionality of R Commander by adding statistical functions, and analyses were conducted using R version 4.3.1 and R Commander version 2.9-1.
Results
Patients and transplant characteristics
A total of 67 patients who were enrolled in the JSCT-ATG15 study were assigned to the ATG group, and 41 patients who were enrolled in the JSCT-PTCY19 study were assigned to the PTCy group (Supplemental Fig. 1). The median patient age was 46 years, ranging from 19 to 65 years. The PTCy group had higher numbers of DRI-high patients, unrelated donors, and higher number of CD34+ cells than the ATG group. Patients who underwent RIC and HLA-mismatched transplantation were observed only in the PTCy group because of differences in the study protocol. Other factors did not differ between the groups (Table 1).
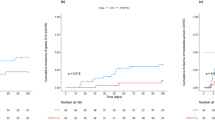
Engraftments
Neutrophil and platelet engraftments were both significantly higher and shorter, respectively, in the ATG group than in the PTCy group. Neutrophil engraftment was achieved in 100% and 97.6% of the ATG and PTCy groups, respectively (P = 0.007; Fig. 1a). The median time of platelet engraftment was 13 days, ranging from 12 to 27 days in the ATG group, and 15 days, ranging from 13 to 43 days in the PTCy group (P < 0.001; Fig. 1b). Platelet engraftment was achieved in 98.5% and 92.7% of the patients in the ATG and PTCy groups, respectively (P = 0.007, Fig. 1c). The median time of neutrophil engraftment was 20 days, ranging from 11 to 58 days, in the ATG group and 27 days, ranging from 11 to 117 days, in the PTCy group (P = 0.003, Fig. 1d).
Incidence of engraftment in the ATG and PTCy groups. The cumulative incidence of neutrophil engraftment in the ATG (solid lines) and PTCy (dashed lines) groups (a), and the median neutrophil engraftment days from the day of HSCT in the ATG and PTCy groups (b). The cumulative incidence of platelet engraftment in the ATG (solid lines) and PTCy (dashed lines) groups (c), and the median platelet engraftment days from the day of HSCT in the ATG and PTCy groups (d). The ends of the center box indicate the upper and lower quartile of the data, the line inside the rectangle indicates the median, the whiskers indicate the maximum and minimum values, and the dots outside the rectangle indicate outliers.
GVHD
The cumulative incidences of grade II to IV acute GVHD on day 200 were 19.4% and 14.6% (P = 0.54, Fig. 2a), and those of grade III to IV acute GVHD on day 200 were 0.0% and 2.4% in the ATG and PTCy groups, respectively (P = 0.201, Fig. 2b). The cumulative incidence of all-grade chronic GVHD at 2 years was 21.0% and 14.6% (P = 0.453, Fig. 2c), and that of moderate to severe chronic GVHD at 2 years was 10.6% and 4.9% in the ATG and PTCy groups, respectively (P = 0.356, Fig. 2d), with no significant difference.
Relapse, NRM, off-immunosuppressants, and causes of death
The cumulative incidences of relapse and NRM at 2 years were 25.4% and 4.5% in the ATG group, and 17.7% and 7.3% in the PTCy group, respectively, with no significant differences (Fig. 3a, b). The cumulative incidence of immunosuppressant discontinuation without relapse at 2 years was 61.9% in the ATG group and 74.0% in the PTCy group (P = 0.15; Fig. 3c). The causes of death were similar between groups (Supplemental Table 2).
Incidences of relapse, NRM, and off-immunosuppressants, and probabilities of OS, PFS and GRFS in the ATG and PTCy groups. The cumulative incidences of relapse (a), NRM (b), and off-immunosuppressants (c), and the probabilities of OS (d), PFS (e), and GRFS (f) in the ATG (solid lines) and non-ATG (dashed lines) groups.
Survival outcomes
With a median follow-up of 721 days, the probability of OS at 2 year was 83.4% (95% CI, 72.0–90.4%) in the ATG group and 76.5% (95% CI, 59.1–87.2%) in the PTCy group (P = 0.48, Fig. 3d), PFS at 2 year was 70.0% (95% CI, 57.4–79.5%) in the ATG group and 75.2% (95% CI, 58.7–85.8%) in the PTCy group (P = 0.66, Fig. 3e), and GRFS at 2 year was 57.9% (95% CI, 45.2–68.7%) in the ATG group and 67.8% (95% CI, 51.0–79.9%) in PTCY group (P = 0.48, Fig. 3f), all with no significant difference.
Univariate analysis for relapse, NRM, OS, PFS and GRFS in pre-transplant parameters identified age (< 45 years) (P = 0.040) as a risk for relapse, disease status (not in CR) (P = 0.012) and CD34+ cells (< 3.65 × 106/kg) (P = 0.010) as risks for NRM, DRI (high) as a risk for OS (P = 0.020), and performance status (≥ 1) as a risk for PFS (P = 0.038), respectively (Supplemental Table 3).
We also evaluated the association of donor (related or unrelated), HLA compatibility (matched or mismatched), and conditioning intensity (MAC or RIC) with survival outcomes between ATG and PTCy and found no significant difference in OS between all subgroups. The probabilities of OS at 2 years were 86.8%, 76.2%, 76.9%, and 76.0% (P = 0.67) in patients who received HSCT from related and unrelated donors in the ATG group and related and unrelated donors in the PTCy group (Fig. 4a); 83.4%, 78.5%, and 75.6% (P = 0.77) in the ATG group (all patients received from HLA-matched donor) and patients who received HSCT from HLA-matched and mismatched donors in the PTCy group (Fig. 4b); and 83.4%, 72.2%, and 85.7% (P = 0.33) in the ATG group (all patients received MAC) and patients who received MAC and RIC in the PTCy group (Fig. 4c), respectively. The probabilities of PFS (Supplemental Fig. 2a–c) and GRFS (Supplemental Fig. 2d–f) were also similar.
Probability of OS in the ATG and PTCy groups according to donor, HLA compatibility, and conditioning intensity. The probability of OS in the ATG and non-ATG groups according to donor (a), HLA compatibility (b), and conditioning intensity (c). (a); related donor (black line) and unrelated donor (red line) in the ATG group, and related donor (green line) and unrelated donor (blue line) in the PTCy group, (b); HLA-matched donor (black line) in the ATG group, and HLA-matched donor (red line) and HLA-mismatched donor (green line) in the PTCy group, (c); MAC (black line) in the ATG group, and MAC (red line) and RIC (green line) in the PTCy group.
Discussion
The latest EBMT recommendation for GVHD prophylaxis states that ATG or PTCy should be preferred to prophylaxis with neither ATG nor PTCy for HSCT from HLA-matched unrelated donor, whereas PTCy should not be generally preferred to ATG HSCT from HLA-matched related donor because of the lack of high-quality evidence of direct comparative evidence19. Comparative studies of ATG and PTCy is increasing based on retrospective analysis except one prospective phase II study reported from Europe to evaluate the efficacy of 50 mg/kg for 2 days of PTCy or 2.5 mg/kg for 2 days of ATG for HLA-matched PBSCT after RIC. This study showed the comparable outcome of the primary endpoint, probability of GRFS at 2 years between the groups, except that the median time to neutrophil and platelet engraftment were significantly longer in the PTCy group than in the ATG group, which is consistent with the prospective phase II study20. Other transplant outcomes including NRM, relapse, PFS, and OS were also comparable between the groups, whereas detailed evaluation of these outcomes is difficult because of the diversity of primary diseases and disease states at transplant. Other retrospective studies almost showed the comparable transplant outcomes between ATG and PTCy for HLA-matched HSCT21,22,23,24, whereas a recent study indicates the favorable transplant outcomes in the PTCy group compared to that in the ATG group25.
In our study, PTCy had comparable efficacy for GVHD prevention to low dose ATG, although the patient backgrounds of JSCT-PTCY19, wherein an HLA-mismatched donor or RIC as a conditioning was included, were heterogeneous compared to those of JSCT-ATG15. Notably, patients who received HSCT from an HLA-mismatched donor or RIC as conditioning in the PTCy group had similar outcomes to the others. Almost all phase III trials that demonstrated the efficacy of ATG used MAC4,5,6,7,8,9, whereas phase III trials that demonstrated the efficacy of PYCy used RIC10,11, suggesting that conditioning intensity may affect the transplant outcomes between ATG and PTCy. A previous matched-pair analysis between ATG and PTCy in HLA-mismatched HSCT showed that the incidence of grade III-IV acute GVHD was significantly lower in patients with PTCy than in those with ATG, and leukemia-free survival, OS, GRFS, and NRM were favorable outcomes in the PTCy group26. Other studies on HSCT from HLA-mismatched unrelated donors also reported favorable outcomes for PTCy compared to those for ATG27,28,29,30,31.
Another notable complication with PTCy is cardiac toxicity32,33. In the PTCy group, one patient died of cardiomyopathy. Although adverse effects were not evaluated in this study, both phase II studies investigated grade 3–4 non-hematologic toxicity within 100 days after HSCT. Major grade 3–4 adverse effects within 30 days after HSCT were as follows: lung: 3%, nervous system: 1%, liver: 6%, SOS: 3%, renal and urinary: 5%, and infection: 13% in JSCT-ATG15; cardiac: 4%, lung: 2%, liver: 2%, SOS: 2%, renal and urinary: 5%, and infection: 19% in JSCT-PTCY19, and from 30 to 100 days after HSCT were as follows: lung: 1%, liver: 5%, renal and urinary: 4%, and infection: 13% in JSCT-ATG15; cardiac: 3%, lung: 6%, liver: 3%, and infection: 12% in JSCT-PTCY19, with no significant difference between the studies, although cardiac complication was prominent in JSCT-PTCY19. A recent study evaluating early cardiac toxicity also showed that the incidence of cardiac toxicity until day 180 after HSCT was significantly higher in patients with PTCy than in those without PTCy, and total body irradiation and pre-transplant cardiac morbidity were identified as risk factors for early cardiac toxicity33. Detailed evaluation of pre-transplant cardiac function and risk assessment may be essential for using PTCy.
Our study is the first to compare the clinical outcomes of fixed low dose ATG and PTCy for PBSCT. Recent studies tend to adopt lower dose of ATG because higher dose of ATG is a risk for relapse or infection related mortality34,35,36,37,38. EBMT recommendation also states that the recommended dose of ATG ranges from 2.5 to 5 mg/kg in HSCT from HLA-matched related donor to 4.5–6 mg/kg in HSCT from HLA-matched unrelated donor with the caution that higher doses are associated with a higher risk of infectious complications39. Our previous pilot study showed that only a total of 2 mg/kg of ATG can reduce naïve T cells at day 28 after PBSCT40, leading to the evidence of JSCT-ATG15 study12.
Our study has some limitations, particularly for the evaluation of OS or PFS, that should be considered when reviewing the results, including its retrospective design, the comparison of two prospective studies with a limited number of patients, and diversity of primary disease and disease status at transplant. Nevertheless, our data indicated the efficacy and safety of GVHD prophylaxis using both ATG and PTCy. Larger prospective studies are needed to establish the roles of ATG and PTCy in GVHD prophylaxis.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Socié, G. et al. Long-term survival and late deaths after allogeneic bone marrow transplantation. Late effects working committee of the international bone marrow transplant registry. N Engl. J. Med. 341, 14–21 (1999).
Lanzkron, S. M., Collector, M. I. & Sharkis, S. J. Homing of long-term and short-term engrafting cells in vivo. Ann. N Y Acad. Sci. 872, 48–54 (1999). discussion 54–56.
Anasetti, C. et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl. J. Med. 367, 1487–1496 (2012).
Bacigalupo, A. et al. Antithymocyte Globulin for graft-versus-host disease prophylaxis in transplants from unrelated donors: 2 randomized studies from gruppo Italiano Trapianti Midollo Osseo (GITMO). Blood 98, 2942–2947 (2001).
Finke, J. et al. Standard graft-versus-host disease prophylaxis with or without anti-T-cell Globulin in Haematopoietic cell transplantation from matched unrelated donors: a randomised, open-label, multicentre phase 3 trial. Lancet Oncol. 10, 855–864 (2009).
Kröger, N. et al. Antilymphocyte Globulin for prevention of chronic Graft-versus-Host disease. N Engl. J. Med. 374, 43–53 (2016).
Walker, I., Panzarella, T. & Couban, S. Pretreatment with anti-thymocyte Globulin versus no anti-thymocyte Globulin in patients with haematological malignancies undergoing Haemopoietic cell transplantation from unrelated donors: a randomised, controlled, open-label, phase 3, multicentre trial. Lancet Oncol. 17, 164–173 (2016).
Soiffer, R. J. et al. Prospective, randomized, Double-Blind, phase III clinical trial of Anti-T-Lymphocyte Globulin to assess impact on chronic Graft-Versus-Host Disease-Free survival in patients undergoing HLA-Matched unrelated myeloablative hematopoietic cell transplantation. J. Clin. Oncol. 35, 4003–4011 (2017).
Chang, Y. J. et al. Antithymocyte Globulin for matched sibling donor transplantation in patients with hematologic malignancies: A multicenter, Open-Label, randomized controlled study. J. Clin. Oncol. 38, 3367–3376 (2020).
Broers, A. E. C. et al. Posttransplant cyclophosphamide for prevention of graft-versus-host disease: results of the prospective randomized HOVON-96 trial. Blood Adv. 6, 3378–3385 (2022).
Bolaños-Meade, J. et al. Post-Transplantation Cyclophosphamide-Based Graft-versus-Host disease prophylaxis. N Engl. J. Med. 388, 2338–2348 (2023).
Shiratori, S. et al. Low-dose anti-thymocyte Globulin for GVHD prophylaxis in HLA-matched allogeneic peripheral blood stem cell transplantation. Bone Marrow Transpl. 56, 129–136 (2021).
Sugita, J. et al. Posttransplant cyclophosphamide in unrelated and related peripheral blood stem cell transplantation from HLA-matched and 1 allele mismatched donor. Bone Marrow Transpl. 59, 344–349 (2024).
Harris, A. C. et al. International, multicenter standardization of acute Graft-versus-Host disease clinical data collection: A report from the Mount Sinai acute GVHD international consortium. Biol. Blood Marrow Transpl. 22, 4–10 (2016).
Filipovich, A. H. et al. National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol. Blood Marrow Transpl. 11, 945–956 (2005).
Armand, P. et al. Validation and refinement of the disease risk index for allogeneic stem cell transplantation. Blood 123, 3664–3671 (2014).
Holtan, S. G. et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood 125, 1333–1338 (2015).
Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 48, 452–458 (2013).
Penack, O. et al. Prophylaxis and management of graft versus host disease after Stem-Cell transplantation for haematological malignancies: updated consensus recommendations of the European society for blood and marrow transplantation. Lancet Haematol. 11, e147–e159 (2024).
Brissot, E. et al. Post-transplant cyclophosphamide versus anti-thymocyte Globulin after reduced intensity peripheral blood allogeneic cell transplantation in recipients of matched sibling or 10/10 HLA matched unrelated donors: final analysis of a randomized, open-label, multicenter, phase 2 trial. Blood Cancer J. 14, 31 (2024).
Brissot, E. et al. Post-transplant cyclophosphamide versus antithymocyte Globulin in patients with acute myeloid leukemia in first complete remission undergoing allogeneic stem cell transplantation from 10/10 HLA-matched unrelated donors. J. Hematol. Oncol. 13, 87 (2020).
Lee, M. W. et al. A comparison of post-transplantation cyclophosphamide versus antithymocyte-globulin in patients with hematological malignancies undergoing HLA-matched unrelated donor transplantation. Med. (Baltim). 99, e21571 (2020).
Battipaglia, G. et al. Post-transplantation cyclophosphamide versus antithymocyte Globulin in patients with acute myeloid leukemia undergoing allogeneic stem cell transplantation from HLA-identical sibling donors: A retrospective analysis from the acute leukemia working party of the European society for blood and marrow transplantation. Cancer 127, 209–218 (2021).
Aydin, M., de Leeuw, D. C. & Rutten, C. E. ATG versus PTCy in matched unrelated donor Haematopoietic stem cell transplantations with non-myeloablative conditioning. Br. J. Haematol. 203, 439–445 (2023).
Penack, O. et al. ATG or post-transplant cyclophosphamide to prevent GVHD in matched unrelated stem cell transplantation? Leukemia 38, 1156–1163 (2024).
Battipaglia, G. et al. Posttransplant cyclophosphamide vs antithymocyte Globulin in HLA-mismatched unrelated donor transplantation. Blood 134, 892–899 (2019).
Mehta, R. S. et al. Post-transplantation cyclophosphamide versus conventional graft-versus-host disease prophylaxis in mismatched unrelated donor Haematopoietic cell transplantation. Br. J. Haematol. 173, 444–455 (2016).
Soltermann, Y. et al. Reduced dose of post-transplantation cyclophosphamide compared to ATG for graft-versus-host disease prophylaxis in recipients of mismatched unrelated donor hematopoietic cell transplantation: a single-center study. Ann. Hematol. 98, 1485–1493 (2019).
Nykolyszyn, C. et al. Posttransplantation cyclophosphamide vs. antithymocyte Globulin as GVHD prophylaxis for mismatched unrelated hematopoietic stem cell transplantation. Bone Marrow Transpl. 55, 349–355 (2020).
Modi, D. et al. Post-transplant cyclophosphamide versus thymoglobulin in HLA-Mismatched unrelated donor transplant for acute myelogenous leukemia and myelodysplastic syndrome. Transpl. Cell. Ther. 27, 760–767 (2021).
Penack, O. et al. PTCy versus ATG as graft-versus-host disease prophylaxis in mismatched unrelated stem cell transplantation. Blood Cancer J. 14, 45 (2024).
Duléry, R., Mohty, R. & Labopin, M. Early cardiac toxicity associated with Post-Transplant cyclophosphamide in allogeneic stem cell transplantation. JACC CardioOncol. 3, 250–259 (2021).
Pérez-Valencia, A. I. et al. Incidence, risk factors, and impact of early cardiac toxicity after allogeneic hematopoietic cell transplant. Blood Adv. 7, 2018–2031 (2023).
Ayuk, F. et al. Comparison of two doses of antithymocyte Globulin in patients undergoing matched unrelated donor allogeneic stem cell transplantation. Biol. Blood Marrow Transpl. 14, 913–919 (2008).
Hamadani, M. et al. Improved nonrelapse mortality and infection rate with lower dose of antithymocyte Globulin in patients undergoing reduced-intensity conditioning allogeneic transplantation for hematologic malignancies. Biol. Blood Marrow Transpl. 15, 1422–1430 (2009).
Devillier, R. et al. Impact of antithymocyte Globulin doses in reduced intensity conditioning before allogeneic transplantation from matched sibling donor for patients with acute myeloid leukemia: a report from the acute leukemia working party of European group of bone marrow transplantation. Bone Marrow Transpl. 53, 431–437 (2018).
Boga, C. et al. Effects of two doses of anti-T lymphocyte globulin-Fresenius given after full-match sibling stem cell transplantation in acute myeloblastic leukemia patients who underwent myeloablative fludarabine/busulfan conditioning. Hematol. Oncol. Stem Cell. Ther. 11, 149–157 (2018).
Butera, S. et al. Impact of anti-thymocyte Globulin dose for graft-versus-host disease prophylaxis in allogeneic hematopoietic cell transplantation from matched unrelated donors: a multicenter experience. Ann. Hematol. 100, 1837–1847 (2021).
Penack Ol, Marchetti, M. et al. Prophylaxis and management of graft versus host disease after Stem-Cell transplantation for haematological malignancies: updated consensus recommendations of the European society for blood and marrow transplantation. Lancet Haematol. 7, e157–e167 (2020).
Shiratori, S. et al. T-cell depletion effects of low-dose antithymocyte Globulin for GVHD prophylaxis in HLA-matched allogeneic peripheral blood stem cell transplantation. Transpl. Immunol. 46, 21–22 (2018).
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
No funding was received to conduct this study.
Author information
Authors and Affiliations
Contributions
SS, JS and TT designed the study, and SS analyzed data and wrote the manuscript. JI, TK, YM, TE, SK, and KF included patients. TT revised the manuscript. MH managed the Research Group (Japan Study Group for Cell Therapy and Transplantation). All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
TT reports grants from Sanofi and donations from SHIONOGI, during the conduct of the study. All the remaining authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shiratori, S., Sugita, J., Ishikawa, J. et al. A comparative study of GVHD prophylaxis using low dose ATG versus PTCy for PBSCT based on two independent prospective cohorts. Sci Rep 15, 20677 (2025). https://doi.org/10.1038/s41598-025-07263-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07263-4