Abstract
Due to various factors such as anesthesia, the core body temperature of perioperative patients often fluctuates significantly. Ideal core temperature measurements are particularly needed during the perioperative period for early identification of hypothermia and malignant hyperthermia, and even to guide intraoperative temperature protection. This study aimed to evaluate the consistency of the optimized Zero-Heat-Flux (ZHF) thermometer with esophageal temperature monitoring under general anesthesia. Adult patients, classified as American Society of Anesthesiologists (ASA) I–III, who are scheduled for elective surgery will be enrolled in this study. Both esophageal and ZHF core temperature monitoring were measured simultaneously. The consistency and correlation between the two measurements were evaluated using Bland–Altman analysis, linear regression methods, and the percentage of differences within ± 0.5 °C. The sensitivity and specificity of the ZHF temperature in identifying hypothermia were further validated. Ninety patients with a total of 1035 pairs of measurements were analyzed. Bland–Altman analysis revealed a mean difference between ZHF temperature and esophageal temperature of 0.06 ± 0.26 °C, with 95% limits of agreement ranging from − 0.57 to 0.46 °C. 96.0% of the measurement differences were within ± 0.5 °C. The consistency correlation coefficient was 0.89 (95% CI 0.88–0.90). The sensitivity and specificity of ZHF temperature monitoring in diagnosing hypothermia were 0.86 and 0.91 respectively. The modified ZHF core temperature monitoring system demonstrates good accuracy and consistency with esophageal temperature monitoring during general anesthesia for surgery. ZHF temperature monitoring is highly reliable for diagnosing hypothermia, though further research is needed to evaluate its accuracy.
Similar content being viewed by others
Introduction
Hypothermia is a common thermoregulatory disturbance in surgical patients, with an incidence ranging from 4 to 90%1,2,3. Anesthesia interferes with the regulation and defense response of the hypothalamus and periphery to hypothermia. The operating room environment, surgical disinfection, and related procedures, as well as patient factors, exacerbate the occurrence of hypothermia4. Previous studies have confirmed that perioperative hypothermia can lead to a series of adverse complications, including cardiovascular dysfunction, wound infection, delayed anesthesia recovery, and extended hospital stays5,6. Accurate and convenient continuous core temperature monitoring is crucial for preventing and managing perioperative hypothermia.
The ideal method for core temperature monitoring should be highly accurate, cost-effective, minimally invasive, and capable of dynamically and continuously reflecting the patient’s core temperature7,8. Currently, core temperature monitoring is primarily conducted at the pulmonary artery, tympanic membrane, distal esophagus, and nasopharynx. A non-invasive core temperature measurement was developed based on the “Zero-Heat-Flux (ZHF)” principle9. Compared to other monitoring methods, it is more suitable for perioperative patients, especially for achieving continuous non-invasive monitoring of the entire perioperative period10. The system comprises two temperature sensors separated by an insulating device and covered by a servo-controlled heater. Under normal conditions, a heat gradient exists from the body’s core to the skin, with most heat transferring towards the skin. In the case of a zero-heat-flux thermometer, the heat flow to the skin cannot escape through the insulating system and accumulates in the area of the temperature sensors. Theoretically, after a few minutes of equilibrium, the temperature at the zero-heat-flux thermometer site will match the core temperature as the gradient from the core to the forehead skin surface is maintained.
To achieve optimal perioperative temperature monitoring, foreign scholars have compared the consistency of zero-heat-flux core temperature monitoring with other methods and sites11,12. However, there is controversy over the device’s performance monitoring core temperature13,14. This study aims to improve zero-heat-flux core temperature monitoring implementation and compare its accuracy and consistency with esophageal temperature measurement under general anesthesia in non-cardiac surgery
Methods
Subjects
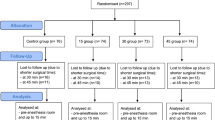
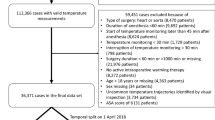
This study received ethics approval from the Institutional Review Board of Baoding No. 1 Central Hospital (Ethics Approval No. [2021]158), which was then registered with the Chinese Clinical Trial Registry (ChiCTR2200057548). Written informed consent was obtained from all participants, and the Declaration of Helsinki followed all methods. We enrolled adult patients undergoing elective major non-cardiac surgery at Baoding No. 1 Central Hospital between January and December 2022, with inclusion criteria of an expected anesthesia duration exceeding 120 min and a preoperative body temperature between 36.0 and 37.5 °C. Exclusion criteria included patients with an American Society of Anesthesiologists (ASA) physical status classification over Grade IV and those with conditions that could interfere with standard temperature measurement or lead to inaccurate core temperature readings. Such conditions included brain diseases, thermoregulatory disorders, and a history of thyroid dysfunction (either hypothyroidism or hyperthyroidism).
Anesthesia method
After the patient entered the operating room, the nurse confirmed the patient’s identity and established intravenous infusion. Essential vital signs, including pulse oximetry, electrocardiography, and blood pressure measurement, were initiated. During the induction phase, the following medications were administered: etomidate, sufentanil, and cisatracurium; endotracheal intubation was performed using a video laryngoscope. Anesthesia was maintained with sevoflurane to keep the bispectral index (BIS) between 40 and 60 and continuous infusion of remifentanil and cisatracurium to achieve adequate analgesia and muscle relaxation.
Core body temperature monitoring
After the patient arrived in the operating room, a disposable non-invasive ZHF sensor (3M Company, St Paul, MN, USA) was applied to the right forehead and connected to a designated monitor. After 3–5 min for the temperature to stabilize, the core temperature from the forehead is recorded. To reduce the interference of heat flow from the surrounding areas during forehead temperature monitoring, the patient wears a disposable surgical cap covering the temperature sensor and the skin on the forehead. The esophageal temperature monitoring is performed after the patient completes anesthesia induction, with the assistance of a visual laryngoscope. The esophageal temperature probe (Philips Medical Systems Model 21,075 A, Andover, MA) is placed through the patient’s nostril to the distal esophagus, with the placement depth determined based on the Mekjavic formula15 calculated by height. The patient’s core temperature is recorded every 15 min using both measurements. The ZHF and esophageal temperature measurements were performed by anesthesiologists who had received standardized training for the respective equipment. ZHF temperature monitoring continues until the end of anesthesia, after which the esophageal temperature probe is removed, and the monitoring is terminated before the patient awakens from anesthesia. The continuous temperature data from the forehead and esophagus measurements are downloaded from the monitor storage system by a designated person using a double-check data entry method, thereby avoiding data entry by the doctors performing the temperature measurements.
Observation indicators
The primary outcome measures were the ZHF core temperature (Tzhf) agreement with the esophageal core temperature (Teso). The secondary outcome measures were the performance of ZHF core temperature monitoring in intraoperative detection of hypothermia and hyperthermia.
Sample size estimation
This study was designed as a single-sample diagnostic trial to evaluate the consistency and accuracy of the ZHF core temperature monitoring compared to the esophageal core temperature. A single-arm, one-tailed t-test assessed whether the upper Limits of Agreement (LoA) were statistically below 0.5 °C, with an anticipated LoA of 0.3 °C and a standard deviation (SD) of 0.5 °C. The analysis controlled the Type I error rate at α = 2.5% and achieved 94% statistical power, requiring a cohort of 81 participants. According to previous studies16,17, the final sample size is 90 cases.
Statistical processing
Statistical analysis was performed using MedCalc software (version 20.111) and GraphPad Prism software (version 9.0). A difference of ≤ 0.5 °C between the ZHF and esophageal temperatures at the same time point was considered clinically acceptable. The ZHF thermometer’s agreement was assessed using a random effects model of Bland–Altman analysis, which included the proportion of deviations within the range of 0.5 °C compared to the esophageal core temperature. The Bland–Altman method for repeated measurements was constructed with patients, baseline measurements, and collection times as random factors, and variance was estimated after adjusting for multiple variables. From the same model, the mean difference, standard deviation (SD), limits of agreement (LOA), and 95% confidence interval (CI) of the deviations between the two were calculated as measures of accuracy. The correlation between Tzhf and Teso was evaluated using Lin’s concordance correlation coefficient (CCC). The performance of the ZHF thermometer in diagnosing hypothermia was assessed as a secondary outcome measure by calculating sensitivity, specificity, and predictive values. Following the previous literature18, hypothermia was defined as T < 36.0 °C and hyperthermia as T ≥ 37.5 °C. The characteristics of ZHF monitoring in diagnosing hypothermia and hyperthermia, including sensitivity, specificity, and positive and negative predictive values, were calculated. A difference with p < 0.05 was considered statistically significant.
Results
General Information
We included 90 patients aged between 18 and 80 years. The demographic characteristics are presented in Table 1, with a mean age of (56.3 ± 11.5) years and a mean body mass index (BMI) of (24.5 ± 3.8). 55.6% of the patients were male. Among the selected patients, 25 (27.8%) underwent thoracic surgery, 24 (26.7%) underwent orthopedic surgery, and 19 (21.1%) underwent urological surgery. 22 patients (24.4%) underwent gastrointestinal surgery. 35 patients (38.9%) used forced-air warming systems for thermal protection.
Evaluation of consistency between two temperature monitoring methods
A total of 1035 pairs of esophageal and forehead temperatures were measured simultaneously in the study. The temperature measurement process was safe for all patients, and no adverse events related to temperature measurement occurred. The Bland–Altman analysis showed in Table 2, a − 0.06 ± 0.26 °C bias with a 95% CI of − 0.07 to − 0.04 °C. The 95% limits of agreement (LoA) for the bias between the two measurements were relatively narrow, at − 0.57–0.46 °C, with a 95% CI for the calculated consistency limit of − 0.60–0.49 °C. As shown in Fig. 1, the Bland–Altman plot between Tzhf and Teso did not show significant fluctuations with temperature change. The proportion of differences within 0.5℃ between Tzhf and Teso was 96.0% (95% CI 94.7–97.1%). The concordance correlation coefficient was 0.89 (95% CI 0.88–0.90), indicating a strong correlation between them (Fig. 2).
Performance in diagnosing hypothermia
Using esophageal temperature as the reference, the ZHF thermometer had a sensitivity of 0.86(95% CI 0.81–0.89) and a specificity of 0.91 (95% CI 0.89–0.93) in identifying hypothermia. Its positive predictive value (PPV) was 0.82(95% CI 0.77–0.86), and its negative predictive value (NPV) was 0.93(95% CI 0.91–0.95).
Discussion
This study validated the performance of zero-heat flux (ZHF) core temperature monitoring during non-cardiac surgeries under general anesthesia. It used esophageal temperature as a reference and confirmed its consistency with esophageal temperature. The comparison between ZHF temperature monitoring and esophageal temperature probes was conducted using multiple perspectives and statistical methods. The widely accepted standard for core temperature monitoring, proposed by Sessler16, stipulates that the device’s error should not exceed ± 0.5 °C compared to the actual core temperature. This study found that 96.0% of ZHF temperatures differed within the range of ± 0.5 °C from esophageal temperatures. The Bland–Altman analysis showed a bias of 0.06 °C for ZHF compared to esophageal temperature, with 95% limits of agreement (LoA) of − 0.57–0.46 °C. The consistency correlation coefficient was 0.89, indicating a good consistency between ZHF temperature monitoring and esophageal temperature probes. The ZHF measurement performed well in diagnosing hypothermia with a sensitivity of 0.86, specificity of 0.91, PPV of 0.82, and NPV of 0.93.
Intraoperative hypothermia in patients can lead to a series of adverse outcomes. Accurate temperature monitoring is crucial for the early identification of hypothermia and malignant hyperthermia and serves as a key basis for standard thermal protection and regulation. However, the lack of an accurate and patient-tolerable core temperature measurement is a recognized obstacle to perioperative thermal management. Guidelines and expert consensus recommend choosing the same approach and method for temperature monitoring before and after surgery, with measurements taken every 15–30 min after anesthesia until leaving the PACU4,19. The core temperature monitoring methods currently used during the perioperative period have varying degrees of limitations regarding non-invasiveness, patient tolerance, infection risk, and operational convenience20,21,22. Zero-heat-flux core temperature monitoring can provide non-invasive, continuous, and suitable monitoring for awake and conscious patients, aligning it with the ideal core temperature monitoring standard.
Some studies in Europe and the United States have raised certain controversies regarding the accuracy of zero-heat-flux core temperature monitoring. These studies mainly consider the potential impact of lateral heat convection from peripheral blood flow on the zero-heat-flux channel established from the body core to the skin surface, making it challenging to fully satisfy the assumptions of zero-heat-flux temperature measurement2. To reduce the impact of external ambient temperature, Hanzi Lu et al. improved the design of the ZHF system with the Peltier module, which developed the application for a high-temperature environment23. Based on previous experience, this study has improved zero-heat-flux temperature monitoring to reduce differences in lateral heat gradients in the measurement area and the interference of low-temperature air convection in the operating room on the ZHF channel. Patients were provided with disposable medical surgical caps to cover the forehead skin and the measurement area, and the application and effectiveness of this measure have not been reported previously.
The Bland–Altman consistency evaluation of ZHF temperature with esophageal temperature in our study is similar to that of Bo-Hyun Sang et al.12, who conducted a comparison in pediatric surgical settings and found a bias of 0.07 ± 0.17 °C, with 95% LoA of − 0.41–0.28 °C. The ESOSPOT study17 compared ZHF temperature with esophageal temperature in medium to large surgeries and found a bias of 0.005 °C, with 95% LoA of − 0.49–0.50 °C. Additionally, two other studies focusing on target temperature management in patients after cardiac arrest and stroke showed biases of 0.06 ± 0.45 °C and 0.06 ± 0.39 °C, respectively, when comparing the two monitoring approaches24,25. Conway et al.26 reported a mean bias of 0.03 °C after combined corrections in a meta-analysis study. In our study, credible interval estimation was performed while calculating the consistency limits, and the results slightly exceeded the predefined range of ± 0.5 °C, prompting further analysis.
This study calculated the proportion of measurement differences within the range of 0.5 °C, reaching 96.0%, and the consistency correlation coefficient between the two methods was 0.89. The ESOSOPT study17 reported a proportion of 97.89% and a consistency correlation coefficient of 0.89, slightly better than this study. A study involving 44 pediatric patients undergoing general anesthesia for surgery reported a proportion of differences within the 0.5 °C range as 89.5% and a consistency correlation coefficient of 0.8327, slightly lower than this study. The studies above concluded that ZHF temperature monitoring demonstrated clinically acceptable accuracy and precision for core temperature monitoring.
Different studies have discrepancies regarding the clinical acceptability of consistency between ZHF core and esophageal temperature monitoring. An observational study in 33 orthopedic patients reported that 75% of the differences were within the 0.5 °C range28. A comparison of core temperatures in 100 infants during surgery found ZHF to be 0.26 °C higher than esophageal temperature29. A qualified temperature monitoring device undoubtedly has sufficient theoretical support, and the differences in measurements are related to the personnel performing the measurements, such as the placement and depth of the esophageal temperature probe and the standardized installation of ZHF electrodes. Furthermore, the timing of temperature data collection by personnel may vary, and some studies, to reduce workload, compared temperature data by reading from different monitoring devices, which may introduce systematic bias28. Additionally, differences in blood perfusion and heat exchange may affect the correspondence of core temperatures in the forehead and esophagus to those in the brain and thorax.
ZHF core temperature monitoring has demonstrated high sensitivity, specificity, accuracy, and diagnostic value in identifying hypothermia in the study. As hypothermia is one of the most common thermal disturbances during the perioperative period2, ZHF core temperature monitoring provides continuous, non-invasive monitoring of core temperature, supporting the early identification of hypothermia and the implementation of multimodal temperature management strategies. Compared to esophageal temperature monitoring, which is only suitable for deeply sedated patients, ZHF core temperature monitoring is more widely accepted within clinically acceptable precision ranges29, making it more aligned with the ideal requirements for core temperature monitoring10.
However, this study has some limitations. Firstly, the study design did not employ blinding, and anesthesiologists could simultaneously observe the core temperatures of the forehead and esophagus during surgery and adjust accordingly, which may have influenced the results. Additionally, the surgeries included in the study were all non-cardiac surgeries. The range and degree of core temperature changes during cardiac surgeries are more pronounced, and the influencing factors are more complex30. Therefore, the accuracy of ZHF in cardiovascular surgeries requires further validation.
Furthermore, due to the low incidence of hyperthermia events during the perioperative period18, the sample size of febrile patients in the study was small. Thus, there were not enough samples to fully evaluate the performance of ZHF in febrile patients. The following study needs to include more cases of fever for further verification. The study failed to fully demonstrate its direct reduction of complications or medical costs, more comprehensive and adaptive clinical validation is required to address this gap. Finally, this study only compared the accuracy of one type of ZHF device, and other brands or models may perform differently.
In conclusion, improved ZHF core temperature monitoring has shown accuracy and consistency compared to esophageal temperature probes. It is suitable for clinical use in monitoring core body temperature in patients under general anesthesia. ZHF core temperature monitoring exhibits high reliability in diagnosing hypothermia, although further research is needed to understand its role in diagnosing hyperthermia.
Data availability
Data used during the current study is available from the corresponding author on reasonable request.
References
Sessler, D. I. Perioperative heat balance. Anesthesiology 92(2), 578–596 (2000).
Sessler, D. I. Perioperative temperature monitoring. Anesthesiology 134(1), 111–118 (2021).
Yi, J. et al. Intraoperative hypothermia and its clinical outcomes in patients undergoing general anesthesia: National study in China. PLoS ONE 12(6), e0177221 (2017).
Garceau, C., Cosgrove, M. S. & Gonzalez, K. Inadvertent perioperative hypothermia. AANA J. 91(4), 303–309 (2023).
Paal, P. et al. Accidental hypothermia: 2021 Update. Int. J. Environ. Res. Public Health 19(1), 501 (2022).
Sessler, D. I. Complications and treatment of mild hypothermia. Anesthesiology 95(2), 531–543 (2001).
Wartzek, T., Mühlsteff, J. & Imhoff, M. Temperature measurement. Biomedizinische Technik. Biomed. Eng. 56(5), 241–257 (2011).
Kirkendall, E. S. et al. Feasibility, acceptability, and performance of a continuous temperature monitor in older adults and staff in congregate-living facilities. J. Am. Med. Dir. Assoc. 23(10), 1729-1735.e1721 (2022).
Fox, R. H. & Solman, A. J. A new technique for monitoring the deep body temperature in man from the intact skin surface. J. Physiol. 212(2), 8p–10p (1971).
Munday, J. et al. Implementation of continuous temperature monitoring during perioperative care: A feasibility study. Patient Saf. Surg. 16(1), 32 (2022).
Pedersen, C., Munch, P., Kjaergaard, J., Grønlykke, L. & Bräuer, A. Accuracy of a zero-heat-flux thermometer in cardiac surgery, a prospective, multicentre, method comparison study. Sci. Rep. 14(1), 3169 (2024).
Park, C., Kim, T., Oh, S. & Bang, Y. S. Prospective comparative analysis of zero-heat-flux thermometer (SpotOn®) compared with tympanic thermometer and bladder thermometer in extremely aged patients undergoing lower extremity orthopedic surgery. Medicine 102(42), e35593 (2023).
Dahyot-Fizelier, C. et al. Accuracy of zero-heat-flux cutaneous temperature in intensive care adults. Crit. Care Med. 45(7), e715–e717 (2017).
Eshraghi, Y. et al. An evaluation of a zero-heat-flux cutaneous thermometer in cardiac surgical patients. Anesth. Analg. 119(3), 543–549 (2014).
Mekjavić, I. B. & Rempel, M. E. Determination of esophageal probe insertion length based on standing and sitting height. J. Appl. Physiol. (Bethesda, Md.: 1985) 69(1), 376–379 (1990).
Pei, L., Huang, Y., Mao, G. & Sessler, D. I. Axillary temperature, as recorded by the iThermonitor WT701, well represents core temperature in adults having noncardiac surgery. Anesth. Analg. 126(3), 833–838 (2018).
Morettini, E. et al. Intraoperative core temperature monitoring: Accuracy and precision of zero-heat flux heated controlled servo sensor compared with esophageal temperature during major surgery; the ESOSPOT study. J. Clin. Monit. Comput. 34(5), 1111–1119 (2020).
Mittnacht, A. J. C., Lin, H. M., Liu, X. & Wax, D. New-onset intra-operative hyperthermia in a large surgical patient population: A retrospective observational study. Eur. J. Anaesthesiol. 38(5), 487–493 (2021).
Torossian, A. et al. Preventing inadvertent perioperative hypothermia. Deutsches Arzteblatt Int. 112(10), 166–172 (2015).
Krizanac, D. et al. Femoro-iliacal artery versus pulmonary artery core temperature measurement during therapeutic hypothermia: An observational study. Resuscitation 84(6), 805–809 (2013).
Pasquier, M. et al. Esophageal temperature measurement. N. Engl. J. Med. 383(16), e93 (2020).
Hymczak, H. et al. Core temperature measurement-principles of correct measurement, problems, and complications. Int. J. Environ. Res. Public Health 18(20), 10606 (2021).
Lu, H. et al. Development of a core body thermometer applicable for high-temperature environment based on the zero-heat-flux method. Sensors (Basel, Switzerland) 23(4), 1970 (2023).
Fiorini, K. et al. Non-invasive monitoring of core body temperature for targeted temperature management in post-cardiac arrest care. Front. Med. 9, 810825 (2022).
Wagner, M. et al. Comparison of a continuous noninvasive temperature to monitor core temperature measures during targeted temperature management. Neurocrit. Care 34(2), 449–455 (2021).
Conway, A. et al. Accuracy and precision of zero-heat-flux temperature measurements with the 3M™ bair hugger™ temperature monitoring system: A systematic review and meta-analysis. J. Clin. Monit. Comput. 35(1), 39–49 (2021).
Carvalho, H., Najafi, N. & Poelaert, J. Intra-operative temperature monitoring with cutaneous zero-heat- flux-thermometry in comparison with oesophageal temperature: A prospective study in the paediatric population. Paediatr. Anaesth. 29(8), 865–871 (2019).
Munday, J. et al. Zero-heat-flux and esophageal temperature monitoring in orthopedic surgery: An observational study. J. Multidiscip. Healthc. 14, 1819–1827 (2021).
Nemeth, M., Lovric, M., Asendorf, T., Bräuer, A. & Miller, C. Intraoperative zero-heat-flux thermometry overestimates esophageal temperature by 0.26 °C: An observational study in 100 infants and young children. J. Clin. Monitor. Comput. 35(6), 1445–1451 (2021).
Verheyden, C., Neyrinck, A., Laenen, A., Rex, S. & Van Gerven, E. Clinical evaluation of a cutaneous zero-heat-flux thermometer during cardiac surgery. J. Clin. Monit. Comput. 36(5), 1279–1287 (2022).
Acknowledgements
The authors thank Professor Jie Yi for his long-term guidance.
Funding
This work was supported by grants Plan for Science and Technology Research of Baoding (2041ZF084 to Doc. Liang and 2441ZF203 to Doc. Liang).
Author information
Authors and Affiliations
Contributions
YL conceived the study and wrote the manuscript. JYW contributed to wrote the manuscript and data analysis. ZGW,MNG and XFS contributed to data collection. HL contributed to concept and supervision. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the ethics committee of Baoding No.1 Central Hospital. Written informed consent was obtained from the participated patients.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, Y., Wang, Jy., Shao, Xf. et al. Accuracy of improved zero heat flux core temperature monitoring in non-cardiac surgery for patients undergoing general anesthesia. Sci Rep 15, 20595 (2025). https://doi.org/10.1038/s41598-025-07314-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-07314-w