Abstract
CVST is a rare cerebrovascular condition commonly associated with young adults and females. The primary aim of this study was to identify key risk factors associated with CVST and assess the outcomes of participants with CVST. This is an ongoing multicenter hospital-based study conducted from July 2022 to October 2023. A total of 152 CVST participants were selected from seven participating sites. The diagnosis of CVST was confirmed via a CT scan or MRI/MRV. Sociodemographic variables, i.e., lifestyle variables, type of objective testing, clinical presentations, risk factors and hospital outcomes, were recorded. Logistic regression was applied to identify risks associated with CVST and was adjusted for confounders such as age, sex, and comorbidity. The median (range) age of the CVST patients was 29 (0–69) years, with a significantly higher proportion of the registered CVST participants being males than females (63.8% vs 36.2%, P < 0.001). The peak frequency of CVST participants was recorded among those aged 21–30 years, accounting for 32.9% of the participants. The most common clinical manifestation was vomiting in 39.5% of the participants, followed by headache in 29.6% of the participants. The study identified young adults to be at increased risk of CVST (OR 0.28; 95% CI 0.18–0.42; P = < 0.001) and alcohol consumption with higher incident of CVST than never used alcohol (OR 1.95; 95% CI 1.17–3.23; P = 0.010) after adjusted for confounders. Study reported around 97% of participants were discharged after treatment, and mortality was reported in 3.2% of participants. CVST was strongly associated with males and young adults in this study, raising serious concerns. Alcohol intake was associated with a greater risk of CVST. The findings of this study could inform the development of region-specific protocols and targeted public health efforts, ultimately enhancing patient outcomes and reducing CVST-related mortality and morbidity in India.
Similar content being viewed by others
Introduction
Cerebral venous sinus thrombosis (CVST) is a rare cerebrovascular condition in which thrombosis developed in the dural venous sinuses or within one or more cerebral veins1 (Fig. 1). It is commonly associated with young adults and predominantly affects females, with a female-to-male ratio of 3:12. Studies across the globe indicate a strong tendency toward CVST among females due to the use of contraceptive pills (CPs), pregnancy, and puerperium1,3. The sex ratio remains balanced among children considering the absence of sex‐specific risk factors4. In Asian countries, only 5% of CVST cases are related to the use of CP, and 36% are associated with pregnancy and puerperium5. In India, Srinivasan and Natarajan (1974) reported pregnancy-associated CVST at 450/100,000 deliveries, which was higher than that reported in developed nations6. However, some recent studies have shown a changing trend in the sex distribution of CVST incidence. A study based on hospital records from Christian Medical College Vellore, India, reported a higher frequency of males (59.4%) among CVST patients7. In addition, the study revealed that 30% of female CVST cases occurred in the postpartum phase. Magnetic resonance imaging (MRI) combined with MRV is known as the preferred imaging technique for diagnosing CVST8. CVSTs constitute 0.5 to 1% of all types of strokes9 and primarily affect young adults10. The incidence of CVST varies between 1.30 and 1.57 per 100,000 persons per year in European and Australian populations1,11,12. In the United States, it was 2.62 per 100,000 hospitalized adults in 201613.
Anatomy of the cerebral venous system and commonly affected sinuses (created via https://app.biorender.com).
CVSTs are generally associated with symptoms such as headache, vomiting, dizziness, seizures, unresponsiveness and unconsciousness14. The risk factors for CVST can be broadly divided into acquired and genetic factors, primarily inherited thrombophilia15. Major acquired risk factors include pregnancy, puerperium, metabolic disorders such as hypertension and gestational diabetes, malignancy, head trauma, hyperhomocysteinemia, infections and surgeries2,9,16,17,18. Genetic risk factors contribute to 20–30% of CVST cases with factor V Leiden mutation and deficiencies in proteins C and S predominant genetic risks9,16,19. In India, the epidemiology of CVST cases is not well studied ; therefore, in this study, an attempt has been made to highlight the clinical presentations, major risk factors, and outcomes of participants with CVST from the ICMR-National Hospital-based Registry on Venous Thromboembolic Disorder (i-RegVeD registry).
Materials and methods
Study setting
This study is a part of an ongoing multicentric study involving the development of a prospective hospital-based venous thromboembolism registry, i-RegVeD, comprising 16 sites from all over India, representing different geographical regions and healthcare settings. The analysis presented in this study is based on the dataset collected in the registry from July 2022 to October 2023. The detailed study protocol and criteria have been published elsewhere20.
Study design
A prospective hospital-based observational study design was adopted for this study. The i-RegVeD registry included 16 hospital sites for the selection of VTE patients; however, in the initial phase, 13 hospital sites were operational.
Selection of CVST cases from the i-RegVeD registry
The i-RegVeD registry comprises seven sections with more than 950 variables. In total, 1006 VTE patients were recruited through 13 hospital sites between July 2022 and October 2023. Twenty-two participants were excluded because they were artery-related cases and did not have final diagnosis records for VTE, leaving a total of 984 participants with confirmed final diagnosis records for VTE. These 984 participants with VTE were further categorized into two groups: CVST and other VTEs. Upon screening, 152 cases of CVST (approximately 15%) and 832 cases of other VTEs (approximately 85%) were identified. Among the 152 individuals with CVST, 146 had only CVST, whereas the remaining 6 had different types of VTE along with CVST. These participants were recruited from hospital sites operating during the study period. Approximately 91% of the participants with CVST were from three hospital sites only, viz., PGIMER, Chandigarh, NIMHANS, Bengaluru, and JIPMER, Puducherry. The remaining 9% of the participants were from four other participating hospital sites, viz., BMCRI Chennai, PIMSR Gujrat, KIMS Bhubaneswar and AIIMS Delhi (Fig. 3). These participants were recruited through emergency, outpatient department (OPD), intensive care unit (ICU), and inpatient department (IPD) units after their written informed consent was obtained (Fig. 2). All individuals with CVST included in this study had MRI/MRV or CT scans confirming the diagnosis of CVST. Participants across all age groups were included in this study.
Data variables
At each registry site, data were collected via a standardized form and entered by trained technical or paramedical staff with the guidance of the principal investigator or attending physician. Data include details on baseline parameters such as sociodemographic variables, lifestyle variables, type of objective testing (especially computed tomography (CT) scans and magnetic resonance imaging (MRI)/magnetic resonance venography (MRV)), clinical presentations (viz., vomiting, headache, blurring of vision, etc.), and hospital outcomes. Data completeness from the registry forms was ensured through systematic training of site staffs, regular site visits, and periodic virtual monitoring meetings.
Methods of confirmation: radiological features of CVST participants
Magnetic resonance imaging (MRI) has been considered the imaging modality of choice for CVST diagnosis21. For this study, a CVST diagnosis was established clinically and confirmed through CT scan and MRI/MRV. Among the 152 participants included in the study confirmed through neuroimaging modalities, around 31% underwent both CT and MRI/MRV for diagnostic confirmation, more than 55% were diagnosed using MRI/MRV and more than 74% underwent CT scans. The superior sagittal sinus (SSS) was most common affected venous sinuses followed by transverse sinus and lateral sinus (left and right both), the combination of another sinus with SSS were also observed i.e. SSS & right lateral sinus, SSS & bilateral and lateral sinus, SSS & right transverse sinus, SSS & transverse sinus & sigmoidal sinus & cortical vein, etc. (Fig. 3).
The map illustrates the distribution of participating hospital sites and enrolled CVST cases. Map was generated using https://www.mapchart.net/india.html. 152 CVST cases reported from 7 sites (represented with red star mark) [i.e. Postgraduate Institute of Medical Education & Research (PGIMER) Chandigarh, All India Institute of Medical Sciences (AIIMS), New Delhi, Parul Institute of Medical Sciences and Research (PIMSR), Gujrat, National Institute of Mental Health and Neurosciences (NIMHANS) Bangaluru, Bangalore, Bangalore Medical College & Research Institute, (BMC & RI), Bangalore, Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER) Puducherry, Kalinga Institute of Medical Sciences (KIMS), Bhubaneshwar]. CVST cases not reported from 6 sites (represented with black star mark) [i.e. Sher- E-Kashmir Institute of Medical Science (SKIMS) Srinagar, National Institute of Immunohaematology and KEM Hospital, (KEM & NIIH) Mumbai, Rajiv Gandhi Government General Hospital (RGGGH), Chennai, All India Institute of Medical Sciences (AIIMS), Telangana, All India Institute of Medical Sciences (AIIMS)Guwahati, and North Eastern Indira Gandhi Regional Institute of Health and Medical Science (NEIGRIHMS), Shillong.]
CT scan of the CVST
Head CT in most cases shows direct signs of CVST, i.e., the cord sign (seen through CT contrast), hyperdense thrombosed cortical vein, fresh thrombus of the sagittal sinus (at the posterior part), and dense triangle (on noncontrast CT), and the most common direct sign is the empty triangle or delta sign (which can be observed through nonfilling of the confluence of sinuses after contrast injection)10,22. The indirect signs on contrast CT are similar to local or generalized swelling of the brain, flexing of the tentorium, and localized hypodense or hyperdense, indicating hemorrhagic transformation. Moreover, CT with helical CT venography can significantly increase the sensitivity of venous anatomy10. The few most common signs can be seen through CT scans (Images A–D).

CT images of the CVST: direct sign of the CVST from patients’ records (arrows): (A) Male, Age 38, CT brain plain image showing a cord sign involving the SSS; (B) Female, Age 33, CT brain plain image showing a cord sign involving the SSS; (C) Male, Age 38, CT brain plain image involving the internal cerebral vein and vein of the gallbladder; (D) Female, Age 33 contrast CT image showing an empty delta sign in the SS and bilateral lateral sinus.
MRI/MRV of the CVST
MRI/MRV is a highly sensitive technique used in most suspicious CVST-related cases, and conventional MRI shows patient dural sinuses as flow voids. The superior sagittal, sigmoid and transverse sinuses are best visualized through coronal images. A plane parallel to the dural sinus provides the best depiction of the extent of thrombosis within these sinuses. MRV is primarily performed to confirm the diagnosis of suspected cases of CVST, especially at acute stages (as direct visualization of thrombi may be difficult through MRI)10. The following are the most typical findings on MRI/MRV of CVST cases from patient records in this study (images A–H).

MRI images: Typical findings of CVST cases from patients’ records (arrows): (A) Male, Age 45 years, MRI brain lateral FLAIR image showing thrombosis of the right lateral sinus; (B) Male, Age 45 years, MRI T2 image showing thrombosis of the SSS; (C) Female, Age 33 years, MRI brain coronal T2 image showing thrombosis of the SSS and right lateral sinus; (D) Female, Age 33 years, T2 MRI sagittal image showing thrombosis of the SSS; (E) Female, Age 33 years, MRI axial image showing thrombosis of the SSS and cortical veins; (F) Male, Age 45 years, MRI brain coronal T2 image showing thrombosis of the right lateral sinus. MRV images: (G) Female, Age 33 years, MRV showing thrombosis of the SSS. (H) Female, Age 20 years, MRV showing thrombosis of the bilateral lateral sinus and SSS.
Statistical analysis
A sexwise descriptive summary of the sociodemographic and lifestyle factors of the individuals with CVST is tabulated. Age is presented as the median with interquartile range, and categorical variables are described as numbers (N) and percentages (%). Age was checked for a normal distribution via histograms and was found to be normally distributed. The chi-square test for independence of attributes was used to assess the bivariate interdependency of the categorical variables with sex. The significance of the difference in the median age of the male and female CVST participants was tested via the Mann‒Whitney U test. Logistic regression was used to identify factors contributing to the risk of CVST among individuals with VTE. Univariate and multivariable logistic regressions were used to obtain unadjusted and adjusted odds ratios, respectively, associated with risk factors such as age, sex, comorbidities, and lifestyle habits. All the statistical analyses were performed via STATA software (STATA version 17.0 MP-Parallel Edition, Stata Corp., Texas, USA), and the clinical presentations and hospital outcome graphs were generated via Microsoft Excel.
Results
Participant characteristics
Sociodemographic and lifestyle factors are presented in Table 1. The median (range) age of the CVST participants was found to be 29 (0–69) years, with no significant difference observed between male and female participants. A significantly higher proportion of the registered CVST participants were males than females, and the difference was statistically significant (63.8% vs 36.2%, P < 0.001). The peak frequency of CVST occurrence was recorded among the age categories 21–30 years in 50 (32.9%) participants, and the lowest was noted in the age category 60 years and above in 7 (4.6%) participants. There was a statistically significant difference observed between male and female participants with CVST for lifestyle variables such as smoking and alcohol consumption (26.3% vs. 2.6 and 36.2% vs. 1.3, P < 0.001, respectively). The occupation categories also significantly differed between the male and female participants (P < 0.001). The majority of the participants were found to be associated with a rural background (63.8%), preferring a nonvegetarian diet (68.4%), and not engaging in physical activity (68.4%). Approximately 43% of the participants with CVST had a history of preexisting comorbidities. However, no significant difference was observed for these variables between males and females.
Clinical manifestations
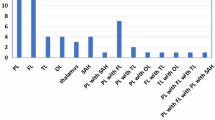
Participants with CVSTs presented with variations in clinical manifestations on physical examination. Vomiting was the most common clinical presentation in 60 (39.5%) participants, followed by headaches in 45 (29.6%) participants, fever in 24 (15.8%) participants, blurring of vision in 22 (14.5%) participants, nausea in 15 (9.9%) participants and leg pain in 15 (9.9%) participants. Other symptoms, such as breathlessness, leg swelling, anxiety, diplopia, bleeding from any site, chest pain, and palpitations, were also reported in approximately 29% of the participants with CVST (Fig. 4).
The majority of CVST participants presented with headaches of acute or sub-acute onset, while chronic and thunderclap-type headache was reported by only a small subset. In terms of localization, headache was predominantly Holocranical or left-lateralized. The most commonly reported headache characteristics were aching and throbbing in nature, although some participants described pressure- like or sharp sensations.
Hospital outcomes of CVST and other VTEs
Hospital outcomes of participants with CVST, including discharge, death, and leave against medical advice (LAMA), and referral status were recorded, and the date and cause of death were also recorded. When the outcomes of the CVST participants were analyzed, the majority (88.2%) were successfully discharged following clinical treatment. A smaller proportion (9.2%) were on LAMA, and no patients required referral to another hospital. Majority of CVST participants received anticoagulant treatment followed by antibiotics and thrombolytic treatment. The mortality rate among participants with CVST was 2.6%. The causes of mortality included septic shock and sepsis, hypertensive-related cardiorespiratory arrest, and prolonged or recurrent seizures. When comparing hospital outcomes between CVST and other VTEs, the discharge rate after clinical treatment was slightly higher in other VTE patients (90.8%), with a lower percentage of participants with LAMAs (5.5%). There were five referred cases (0.6%) among the other participants with VTE, while no referral cases were observed in the CVST group. The mortality rate was marginally higher in other participants with VTE than in participants with CVST, indicating the effectiveness of treatment in participants with CVST conditions (Fig. 5).
Risk factors
Bivariate associations with CVST status
The risk of CVST was found to be higher among individuals in the younger age group (0–45 years), with 21.9% of those affected compared with 7.3% of those in the older age group (46–91 years) (P = 0.001). Males had a higher occurrence of CVST cases (18.1%) than females did (12.3%) (P = 0.012), indicating a significant gender difference in CVST risk. Alcohol consumption was associated with a higher occurrence of CVST (21.8%) than never alcohol consumption was (13.1%) (P = 0.001). There was no significant association between smoking status or comorbidity status and CVST risk (Table 2).
CVST related risk factors for males and females
A larger proportion of both males 72 (47.4%) and females 48 (31.6%) were younger (0–45 years). Older individuals (46–91 years) were less represented, particularly among females 7 (4.6%). The alcohol consumption showed a significant difference between males and female as 55 (36.2%) males reported alcohol use compared to only 2 (1.3%) females (P < 0.001). Similarly, smoking (ever users) is significantly more prevalent among males 40 (26.3%) than females 4 (2.6%) (P < 0.001). Co-morbid conditions were reported in 43 (28.3%) males and 22 (14.5%) females (Supplementary Fig. 1).
Odds ratios associated with the risk factors
The identification of major risk factors like age, sex, lifestyle variables, co-morbidity have been analysed using multivariable logistic regression (Table 3). ROC curve was plotted after fitting the logistic regression (postestimation) to assess the model’s ability to classify between CVST and non-CVST cases (Fig. 6). The AUC 0.72 suggests acceptable discriminatory ability, especially given that the objective of the model is to identify risk factors associated with CVST, rather than predicting CVST cases23. Analysis revealed that young adults were associated with an increased risk of CVST after adjusted for confounders (OR 0.28; 95% CI 0.18–0.42; P = < 0.001). Lifestyle factor,alcohol consumption was significantly associated with higher incident of CVST compare to never used alcohol (OR 1.95; 95% CI 1.17–3.23; P = 0.010) (Table 3). However, no associations with CVST were found for gender, smoking intake and existing co-morbidity in this study, males were associated with a higher risk of CVST in the unadjusted model only.
Discussion
Cerebral venous sinus thrombosis (CVST) is an uncommon condition accounting for 1% of all strokes24. Recent studies from Europe on CVST revealed a shift in sex trends, with a higher incidence among males than females. The findings of the present study also revealed a similar trend, namely, that CVST occurrence was significantly higher among males than among females (63.8% vs 36.2%, P < 0.001). The male predominance in India may be tied to higher alcohol consumption, cultural access bias, or underdiagnosis in women. Earlier Indian study from south region also showed similar findings (50.4% vs 40.6%, respectively)7. One more Indian study documented similar observations: 78.1% of males experienced CVST; however, these studies excluded pregnant or puerperium-related participants with CVST25. The CVST was found more frequently in men (53.7%), as documented from Nizam′s Institute Venous Stroke Registry, Hyderabad, India, by Narayan et al.22. Our study showed a contradictory finding when compared with studies from Mogadishu, Somalia, the majority of patients were female (86.8%)26, and another study showed females accounted for (63.2%)27, which is much higher than our study (36.2%). These discrepancies may due to regional demographic or healthcare access differences influencing the gender distribution of CVST cases.
In our study, the median age of the CVST participants tended to be young, i.e., 29 years (range 0–69 years). This finding was consistent with a study from Pakistan, where the mean age of participants with CVST was 28.39 ± 7.19 years28. Other study from India showed mean age was 31.3 years (range 8–65 years), which is consistent with our results22. Another study from Tibet observed median age 31 years, also consistent with our study27. A multicenter cross-sectional study from Sudan reported a slightly higher median age (35 years; range 23–75 years)29, the selection of the age range could be the reason behind this difference, as it was different from our study. Similarly, a recent hospital based retrospective study from Thailand demonstrated a higher mean age among CVST patients (42.7 ± 20.4 years)30, another study from Saudi Arabia also showed higher mean age of 35.5 ± 14.1 years31, indicating potential regional or demographic differences in age distribution. In our previous study among VTE patients, younger age was associated with longer hospital length of stay32. Mortality was reported in four participants (2.6%) in our study, which is slightly higher (1.9%) than that reported in a study conducted in Oman33. Narayana et al. (2012) from Hyderabad, India, reported a higher mortality rate (in-house mortality) than our study did (7.7% vs 2.6%, respectively)22.
The presenting symptoms related to CVST vary widely, and the current study showed variation in presenting symptoms compared with previous studies. Vomiting was the most common presenting symptom in our study (39.5%) of participants, and headache in (29.6%) of participants. In a hospital-based retrospective and prospective observational study at IHBAS, Delhi, India, headache was the major symptom (85%), followed by vomiting (42%)34. Another study from a tertiary care multispecialty hospital in central Kashmir reported findings, such as headache (79.2%) and vomiting (54.8%), which were the most common clinical presentations35. A study from Pakistan reported similar observations, i.e., headache (92.4%) and vomiting (75.5%), among 3261 CVST participants28. Hospital of Soochow university from China also reported headache as a most common symptoms (75%) in CVT patients, which is higher than our findings36. Our study identified alcohol consumption (ever user) was associated with an increased risk of CVST (OR 1.95, 95% CI 1.17–3.23, P < 0.010).Similar findings from a meta-analysis identified the risk of CVST increased with alcohol consumption (OR 2.67, 95% CI 1.84–3.88, P < 0.001)37. Narayan et al. (2012) from India also reported a link between heavy alcohol consumption and the occurrence of CVST, especially in men, which corresponds with our results22. Alcohol consumption is currently a common lifestyle that increases the risk of conditions such as hypercoagulability, which might contribute to the development of CVST.
Limitations and future directions
Despite a thorough analysis of medical records, this study has some limitations common to retrospective assessment, such as the inability to obtain complete records of every participant. There was no randomization or blinding during selection of participants, making it difficult to control biases. The follow-up data of the participants were not available after discharge from hospitals. The study lacks follow-up data post-discharge and relies only on hospital-based data. Over 90% of the study participants were recruited from only three hospital sites; therefore, these data do not accurately represent the true Indian demography. As this registry continue to expand, future analyses will benefit from a more geographically representative, enabling deeper insights into regional variations, risk factors, and outcomes. Moreover, population-based epidemiological studies and genetic profiling studies needed to better understand the broader determinants of CVST in the Indian population.
Conclusion
In conclusion, this study highlighted CVST epidemiology, common clinical presenting symptoms, and key risk factors across various patient populations in India, enabled by the i-RegVeD registry. Notably, its relatively high occurrence among males and young adults is a serious concern. The high prevalence of vomiting and headache as presenting symptoms among participants suggests that these symptoms could serve as early diagnostic indicators, potentially improving timely intervention. The high rate of clinical recovery and relatively low mortality compared with other forms of VTE suggest effective management strategies for CVST. Alcohol consumption is a key risk factor associated with CVST and impacts its occurrence and outcomes; thus, there is a need to develop targeted prevention strategies and public health interventions aimed at these high-risk groups. The findings of this study could inform the development of region-specific protocols and targeted public health efforts, ultimately enhancing patient outcomes and reducing CVST-related mortality and morbidity in India.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation. Authors can contact corresponding author in case of need of data from this study.
Abbreviations
- CVST:
-
Cerebral venous sinus thrombosis
- VTE:
-
Venous thromboembolism
- i-RegVeD:
-
ICMR-National Hospital-based Registry on Venous Thromboembolic Disorder
- CT-scan:
-
Computed tomography scan
- MRI:
-
Magnetic resonance imaging
- MRV:
-
Magnetic resonance venography
- OPD:
-
Outpatient department
- ICU:
-
Intensive care unit
- IPD:
-
Inpatient department
- DVT:
-
Deep vein thrombosis
- PTE:
-
Pulmonary thromboembolism
- GI:
-
Gastrointestinal tract
- LAMA:
-
Leave against medical advice
- IJV:
-
Internal jugular vein thrombosis
References
Coutinho, J. M., Zuurbier, S. M., Aramideh, M. & Stam, J. The incidence of cerebral venous thrombosis: a cross-sectional study. Stroke 43(12), 3375–3377 (2012).
Bousser, M. G. & Ferro, J. M. Cerebral venous thrombosis: an update. Lancet Neurol. 6(2), 162–170 (2007).
Zuurbier, S. M., Middeldorp, S., Stam, J. & Coutinho, J. M. Sex differences in cerebral venous thrombosis: a systematic analysis of a shift over time. Int. J. Stroke 11(2), 164–170 (2016).
Wasay, M., Dai, A. I., Ansari, M., Shaikh, Z. & Roach, E. S. Cerebral venous sinus thrombosis in children: a multicenter cohort from the United States. J. Child Neurol. 23(1), 26–31 (2008).
Wasay, M. et al. Asian study of cerebral venous thrombosis. J. Stroke Cerebrovasc. Dis. 28(10), 104247 (2019).
Srinivasan, K. & Natarajan, M. Cerebral venous and arterial thrombosis in pregnancy and puerperium. Neurol. India 22(3), 131–140 (1974).
Aaron, S. et al. Cerebral venous thrombosis, seasonal trends, and Climatic influence: A region-Specificstudy. Ann. Indian Acad. Neurol. 23(4), 522–527 (2020).
Fink, J. N. & McAuley, D. L. Cerebral venous sinus thrombosis: a diagnostic challenge. Intern. Med. J. 31(7), 384–390 (2001).
Saposnik, G. et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42(4), 1158–1192 (2011).
Dash, D., Prasad, K. & Joseph, L. Cerebral venous thrombosis: An Indian perspective. Neurol. India 63(3), 318–328 (2015).
Devasagayam, S., Wyatt, B., Leyden, J. & Kleinig, T. Cerebral venous sinus thrombosis incidence is higher than previously thought: a retrospective population-based study. Stroke 47(9), 2180–2182 (2016).
Kristoffersen, E. S. et al. Incidence and mortality of cerebral venous thrombosis in a Norwegian population. Stroke 51(10), 3023–3029. https://doi.org/10.1161/STROKEAHA.120.030800 (2020).
Otite, F. O., et al. Trends in incidence and epidemiologic characteristics of cerebral venous thrombosis in the United States. Neurology. 95(16) (2020).
Fan, Y., et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of cerebral venous sinus thrombosis. Stroke Vasc. Neurol. 5(2), 152–158 (2020).
de Freitas, G. R. & Bogousslavsky, J. Risk factors of cerebral vein and sinus thrombosis. Handb. Cereb. Venous Thromb. 23, 23–54 (2008).
Park, D. S. et al. Clinical characteristics of cerebral venous thrombosis in a single center in Korea. J. Korean Neurosurg. Soc. 56(4), 289–294 (2014).
Silvis, S. M. et al. Cancer and risk of cerebral venous thrombosis: a case–control study. J. Thromb. Haemost. 16(1), 90–95 (2018).
Ferro, J. M. et al. European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis–endorsed by the European Academy of Neurology. Eur. Stroke J. 2(3), 195–221 (2017).
Agnelli, G. & Verso, M. Epidemiology of cerebral vein and sinus thrombosis. Handb. Cereb. Venous Thromb. 23, 16–22 (2008).
Tabassum, H. et al. Development of prospective hospital-based venous thromboembolism registry across India: a study protocol. BMJ Open 13(8), e066644 (2023).
Digge, P., Prakashini, K. & Bharath, K. V. Plain CT vs MR venography in acute cerebral venous sinus thrombosis: Triumphant dark horse. Indian J. Radiol. Imaging. 28(03), 280–284 (2018).
Narayan, D. et al. Risk factors, clinical profile, and long-term outcome of 428 patients of cerebral sinus venous thrombosis: Insights from Nizam′ s Institute Venous Stroke Registry, Hyderabad (India). Neurol. India 60(2), 154–159 (2012).
Hosmer Jr, D. W., Lemeshow, S., Sturdivant, R. X. Applied Logistic Regression (Wiley, 2013).
Hieber, M., Von Kageneck, C., Weiller, C. & Lambeck, J. Thyroid diseases are an underestimated risk factor for cerebral venous sinus thrombosis. Front. Neurol. 22(11), 561656 (2020).
Murugaiyan, S., Sivaji, A. R. & Julin, A. Alcohol emergence: A study on various risk factors and clinical characteristics in patients with cerebral venous sinus thrombosis from a tertiary care hospital in South India. Cureus. 16(7), e65528 (2024).
Adam, B. A. et al. Study of radioclinical and risk factors of cerebral venous thrombosis: a retrospective analysis of patients presenting to a tertiary hospital in Mogadishu, Somalia. Int. J. Gen. Med. 31, 371–378 (2025).
Sha, Y. et al. Clinical and prognostic characteristics of cerebral venous thrombosis at high altitude: a single-center retrospective study of Tibet. J. Neurol. 270(5), 2688–2692 (2023).
Bano, S. et al. Structural imaging characteristic, clinical features and risk factors of cerebral venous sinus thrombosis: A prospective cross-sectional analysis from a tertiary care hospital in Pakistan. Diagnostics. 11(6), 958 (2021).
Ibrahim, E. A. et al. Clinical profile and risk factors of cerebral venous sinus thrombosis (CVST) in Sudan: A multicenter cross-sectional study. Ann. Med. Surg. 1(84), 104891 (2022).
Sitthilok, P. et al. Clinical course and neurological outcomes of cerebral venous sinus thrombosis: A single center retrospective observational study. PLoS ONE 20(1), e0316849 (2025).
Alqahtani, M. S. et al. Clinical and epidemiological profile of cerebral venous thrombosis. Neurosci. J. 25(5), 380–385 (2020).
Aggarwal, S., Rulu, P., i-RegVed, T., Tabassum, H. Factors Associated with Hospital Length of Stay among VTE Cases: Insights from the i-RegVed Registry. J. Primary Care Com Health. 2024 Aug;15:21501319241266815.
Al Hashmi, K., Al Wahaibi, K., Al-Khabori, M. & Al, L. S. Characteristics and outcomes of patients with cerebral venous sinus thrombosis. Oman Med. J. 34(5), 434 (2019).
Khosya, S. A study of clinical profile, risk factors and outcome of the cerebral venous sinus thrombosis (CVST): An experience at a tertiary care center, India. Austin J. Neurol. Disord. Epilepsy. 5(2), 1041 (2018).
Raina, A. F. et al. Clinicoetiological profile of cerebral venous sinus thrombosis patients at a tertiary care center. Curr. Med. Issues. 21(1), 14–18 (2023).
Wang, Y., Shen, X., Wang, P. & Fang, Q. Clinical characteristics of cerebral venous sinus thrombosis patients with new-onset of headache. BMC Neurol. 23(1), 56 (2023).
Green, M. et al. Non-genetic and genetic risk factors for adult cerebral venous thrombosis. Thromb. Res. 1(169), 15–22 (2018).
Acknowledgements
We would like to acknowledge all the study participants and all the participating sites who were enrolled in this study. We would also like to acknowledge all the site project staff for their timely response regarding data correction and completion.
Funding
Indian Council of Medical Research, New Delhi (Grant No. i-RegVeD/Site10/BMS-2022).
Author information
Authors and Affiliations
Consortia
Contributions
S.A. and A.K. performed conceptualization, data curation, methodology, formal analysis, software, visualization, validation, original draft writing, and writing—review and editing; V.D. performed formal analysis, software, and writing—review and editing; and i-RegVeD Team performed data curation, methodology, investigation, resources, and writing-review and editing. H.T. performed conceptualization, data curation, funding acquisition, methodology, project administration, supervision, validation, and writing, review, and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Approval for this study was given by the Institutional Ethics Committee with IEC no. NCDIR/BEU/ICMR-CECHR/75/2020 [Reference Number: CECHR 003/2022 dated 24th March 2022] and all participants were included in accordance with Declaration of Helsinki.
Informed consent
All study participants were recruited after written informed consent, in accordance with the ethics guidelines of the respective ethics committees at each participating site.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Aggarwal, S., Kumar, A., Deo, V. et al. Epidemiology and risk factors for cerebral venous sinus thrombosis: insights from leading centres in the i-RegVeD registry, India. Sci Rep 15, 22712 (2025). https://doi.org/10.1038/s41598-025-07599-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-07599-x