Abstract
The literature suggests that a mindfulness breastfeeding can help mothers cope with postpartum difficulties, appreciate the uniqueness of the moment, strengthen the bond between mother and baby, and provide psychological relief. This study aimed to examine mothers’ mindfulness breastfeeding and breastfeeding self-efficacy and to reveal the relationship between these two factors. A descriptive-correlational design was conducted at the mother-baby adaptation clinic of the neonatal intensive care unit of a baby-friendly maternity hospital in Ankara, Turkiye. The sample consisted of 91 mothers who met the sample criteria. For data collection, the Personal Information Form, the Mindfulness Breastfeeding Scale, and the Breastfeeding Self-Efficacy Scale were used. The median score of the Mindfulness Breastfeeding Scale for the mothers was found to be 43.00, and the median score of the Breastfeeding Self-Efficacy Scale was found to be 59.00. A statistically significant difference was found between the duration of breastfeeding, economic level, the mother’s assessment of her breastfeeding success, and the total scores on the Mindfulness Breastfeeding Scale and the Breastfeeding Self-Efficacy Scale. This study followed the STROBE guidelines. It could be said that the mothers had a good level of mindfulness breastfeeding and breastfeeding self-efficacy. Additionally, as mindfulness breastfeeding increased, breastfeeding self-efficacy also increased. Based on the findings, knowledge and practices that enhance mindfulness breastfeeding and self-efficacy should be incorporated into training programs beginning from the pregnancy process.
Similar content being viewed by others
Introduction
Breast milk is the most comprehensive form of nutrition for babies, providing an ideal balance of proteins, fats, carbohydrates, and essential nutrients necessary for the baby’s growth and is easily digestible1. The American Academy of Pediatrics (AAP) and the World Health Organization (WHO) recommend that infants be exclusively breastfed for the first six months and continue breastfeeding with appropriate complementary foods up to two years of age and beyond2. Breastfeeding is the safest and healthiest method of feeding a baby and has both short-term and long-term benefits for both mothers and babies3,4. Breastfeeding is important for both the mother and the baby, and its contribution to improving global public health is crucial for both low-income and high-income populations alike5.
There are several factors that contribute to initiating and maintaining breastfeeding, which has many benefits for maternal and infant health, such as social support, healthcare provider assistance, breastfeeding intention, maternal mental health, and breastfeeding self-efficacy6. Breastfeeding self-efficacy demonstrates the mother’s ability to cope with challenges she may encounter during the breastfeeding process7,8. Breastfeeding self-efficacy is derived from Bandura’s (1977) concept of self-efficacy and is defined as a mother’s perceived ability to breastfeed her child. It influences her decision to initiate breastfeeding, the effort she believes is necessary, her persistence in breastfeeding attempts until she succeeds, and her perception of how to respond to breastfeeding challenges9. Mothers with high self-efficacy are more likely to choose breastfeeding, persist despite encountering difficulties, use encouraging thoughts, and respond positively to challenges7.
A review of the literature indicates that several factors influence breastfeeding self-efficacy, including previous breastfeeding experiences10,11, social support11,12,13, mother’s age11,14, delay in breastfeeding after birth and the mother and baby being in separate environments15, had a vaginal delivery13,16 and pospartum stress and support from nurses and midwives13.
Interest and understanding of mindfulness have developed in the context of postpartum and breastfeeding in recent years. Mindfulness-based breastfeeding, is defined as focusing on breastfeeding in the present moment and experiencing breastfeeding moment by moment17. Amidst the inevitable stressors of motherhood, such as hormonal changes, psychosocial issues, insomnia, fatigue, and adapting to a new role while ensuring the baby’s healthy development, mindfulness-based breastfeeding may serve as a valuable coping resource18,19. The literature suggests that a mindfulness breastfeeding can help mothers cope with postpartum difficulties20, appreciate the uniqueness of the moment, strengthen the bond between mother and baby21, and provide psychological relief22.
Mindfulness practices aim to help mothers focus on the present moment, recognize the uniqueness of their motherhood journey, and connect with their babies20. Mindful motherhood practices teach mothers to embrace their experiences without judgment, enjoy the motherhood process, and open their eyes and hearts to their babies19,23. The literature suggests that being a mindful mother can help women accept stressful situations, manage them more effectively, understand the transient nature of experiences, and maintain their mental well-being24,25.
Guiding the mother to make eye contact with her baby, smell her baby, feel the baby’s body in her arms, and recognize the baby’s need for care and maternal love are important mindfulness practices24. Despite numerous studies on the effects of mindfulness-based exercises on maternal and infant health during the transition to motherhood26,27,28, to our knowledge, no previous studies have specifically evaluated the relationship between mindful breastfeeding and breastfeeding self-efficacy. Therefore, the aim of this study was to investigate mindfulness breastfeeding and breastfeeding self-efficacy among postnatal women, and to explore the relationship between these factors. This study aims to fill a gap in the literature by providing insights into mindfulness-based breastfeeding among postnatal women. It is expected to enhance the understanding of mindful breastfeeding in this population and inform future practices and research on the topic.
Methods
Design
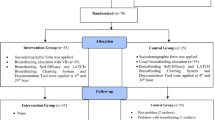
The study used a descriptive-correlational design to explore mothers’ mindfulness breastfeeding, breastfeeding self-efficacy, and the relationship between these factors.
Participants
The research was conducted at the mother-baby adaptation clinic of the neonatal intensive care unit of a baby-friendly maternity hospital in Ankara, Turkiye which encourages breastfeeding in the first six months. Power analysis was used to calculate the sample size. Due to the absence of a similar study in the literature, the sample size calculation considered the highest number recommended by statistical methods to be applied. In this study, the sample size was calculated using the “G. Power-3.1.9.2” software, with a confidence level of 95%29. As a result of the analysis, with α = 0.05 and a standardized effect size of 0.30, considering the absence of a similar study, the minimum sample size was calculated to be 84 with a theoretical power of 0.80. The sample consisted of 91 mothers who met the following sample criteria: they were over 18 years old, able to speak and understand Turkish, had no contraindications to breastfeeding, were staying in the mother-baby adaptation clinic, had no health problems, and voluntarily participated in the study. With a sample size of 91, the power analysis yields a power of 0.83.
Data collection tools
In the study, data were collected through “Personal Information Form”, “Mindfulness Breastfeeding Scale” and the “Breastfeeding Self-Efficacy Scale”.
Personal information form
It was created by the researchers through a review of the literature and consists of four sections with 26 questions: sociodemographic characteristics, obstetric characteristics, introductory information about the baby, and information about breastfeeding30,31,32.
Mindfulness breastfeeding scale (MINDF-BFS)
The Mindfulness Breastfeeding Scale developed by Körükcü et al. (2023) is a nine-item measurement tool that evaluates an awareness-based breastfeeding practice in the postpartum period32.The scale is one-dimensional and was developed as a five-point Likert type. Cronbach’s alpha value was determined as 0.83. The total score to be obtained from the scale is scored between 9 and 45, and as the total score obtained from the scale increases, the awareness rate on breastfeeding also increases. The Cronbach’s alpha value of the MINDF-BFS for this study was calculated as 0.894.
Breastfeeding self-efficacy scale (BSES)
It is a 5-point Likert scale developed by Dennis (1999) to evaluate mothers’ breastfeeding self-efficacy levels, the first form of which consists of 33 items7. In 2003, the scale was shortened and its 14-item version was created33. The Turkish validity and reliability study of the scale was conducted by Tokat et al. (2010)34. Cronbach’s alpha value of the Breastfeeding Self-Efficacy scale was calculated as 0.94. The lowest score from the scale is 14 and the highest score is 70. As the score increases, breastfeeding self-efficacy also increases. The Cronbach’s alpha value of the scale for this research was calculated as 0.894.
Data collection
The data were collected by the principal author through face-to-face interviews with mothers staying in the mother-baby adaptation clinic from September 23.2022, to March 31.2023.
Analysis of data
Data were analyzed using IBM SPSS version 25. Descriptive statistics, including frequency, percentage, mean, standard deviation, median, minimum, and maximum, were provided for the data analysis. The assumption of normality was tested using the Shapiro-Wilk test. Since the scale scores did not follow a normal distribution, they were presented using the median and quartiles. The Mann-Whitney U test was used to compare two independent groups with non-normal distributions, and the Kruskal-Wallis test was used for comparing three or more independent groups. A Post Hoc Bonferroni test was conducted to identify which specific groups differed. Spearman’s correlation was used to assess the relationship between the MINDF-BFS score and the BSES score.
Ethical considerations
The study was conducted with the approval of the Hacettepe University Ethics Committee (Approval number E-35853172-000-00002336323, dated July 5, 2022). All necessary institutional approvals were obtained. Verbal explanations were provided to the participating mothers, and written informed consent was obtained from each participant. The research methods were performed in accordance with the Helsinki Declaration. Participants’ information was kept confidential throughout the study, and all collected data was coded to ensure anonymity.
Findings
Mothers’ sociodemographic and obstetric characteristics are presented in Table 1. It was found that 36.3% of mothers were university graduates, 54.9% were aged between 24 and 31 years, 13.2% were employed, and 93.4% had employed spouses. In terms of economic status, 51.6% of mothers reported their family’s economic situation as “matching income with expenses,” while 47.3% indicated living in an urban area. Furthermore, 34.1% of mothers had one living child, 53.8% gave birth between 31 and 35 weeks of gestation, 81.3% had a cesarean delivery, 78% intended to breastfeed their babies for 24 months or more, and 55.2% breastfed their previous babies for 13 months or longer.
Table 2 presents the sociodemographic and obstetric characteristics of the mothers, as well as the distributions of the MINDF-BFS and BSES total scores. A statistically significant difference was found between the mothers’ economic status and both the MINDF-BFS and BSES total scores (p = .027 and p = .019, respectively). It was determined that this difference was due to the higher MINDF-BFS and BSES scores observed in mothers whose income was less than their expenses, compared to those whose income exceeded their expenses. Mothers’ education level, employment status, partner’s employment status, family type, place of residence, number of living children, gestational weeks, childbirth type, planned pregnancy status, intention to breastfeed duration, duration of breastfeeding for previous child/children, and total scores of MINDF-BFS and BSES did not show statistically significant differences (p > .05).
Table 3 displays the scores for the MINDF-BFS and BSES, as well as the relationships between them. There was found to be a statistically significant, positively moderate correlation (r = .348, p < .05) between MINDF-BFS and BSES scores.
Discussion
In this study, which was conducted to examine mothers’ mindfulness breastfeeding and breastfeeding self-efficacy and to determine the relationship between them, the findings of mindfulness breastfeeding and breastfeeding self-efficacy were discussed separately.
To the best of our knowledge, this is the first study to evaluate mindfulness breastfeeding in mothers. As the inaugural study on this topic, it discusses mindfulness breastfeeding and its influencing factors, referencing related studies from the limited literature.
When the mothers’ mindfulness breastfeeding scale total score is evaluated, it can be said that the mothers’ mindfulness breastfeeding levels are high because it is close to the maximum score. However, since there is no similar study in the literature to make a comparison, it is believed that having at least two children and planning to breastfeed their babies for 24 months or longer may influence the mothers’ mindfulness breastfeeding levels.
Based on the family’s economic status, it was determined that mothers whose income is less than their expenses are more likely to mindful breastfeeding compared to those whose income exceeds their expenses (p = .027). In literature, it is suggested that mothers with poor financial status, facing financial difficulties in accessing complementary foods, are more likely to have a stronger intention and higher persistence in breastfeeding their babies35,36. In line with these findings, it can be said that the difficulty mothers with poor financial status face in accessing infant formula may lead to an increased awareness of breastfeeding, as it is a cost-free and easily accessible option for feeding their babies.
According to the duration of breastfeeding for previous children, it was found that mothers who breastfed their previous child or children for 13 months or more have higher awareness compared to those who breastfed for a shorter duration (p = .002). Since there are no other studies in the literature on mindful breastfeeding for comparison, no direct comparisons can be made. However, it can be inferred that mothers who breastfed their previous child or children for longer durations tend to exhibit higher mindfulness in breastfeeding.
Regarding mothers’ education level, employment status, spouse’s employment status, place of residence, childbirth type, gestational age, and intention to breastfeed duration, no significant differences were found with the MINDF-BFS scores. Given that these results are specific to this sample, future research using the Mindfulness Breastfeeding Scale should explore these variables further and provide comparisons and implications based on broader studies.
As for the breastfeeding self-efficacy of mothers and the effective factors, it can be said that the breastfeeding self-efficacy of mothers is regarded as high, given that their scores are close to the maximum. Similarly, in the literature, studies have also found that mothers have high self-efficacy37,38. There was no significant difference between the mothers’ educational status and the BSES total score. Additionally, studies in the literature indicate that there is no relationship between mothers’ educational status and the BSES scores39,40. The lack of difference is thought to be due to the sample in this study may not have had enough diversity in educational backgrounds, as more than half of the mothers in the sample had completed high school or higher education. This homogeneity could potentially reduce the variability needed to detect a meaningful relationship between education level and breastfeeding self-efficacy. Literature suggests that working mothers tend to have higher average breastfeeding self-efficacy scores11,37. Since nearly all of the mothers in this study’s sample are not working, this may explain the absence of a significant difference.
According to the family economic status, mothers with lower income had higher scale scores compared to those with higher income (p = .019). Similarly, Mercan and Tari Selçuk (2021) found that mothers with lower income levels had higher breastfeeding self-efficacy37. However, a review of the literature also reveals studies that show no relationship between family economic status and breastfeeding self-efficacy10,11,12. A Based on this study’s results, it is believed that mothers with lower economic status may exhibit better breastfeeding self-efficacy due to the cost-effectiveness of breastfeeding35,36.
No significant differences were found between the BSES total score and variables such as mothers’ employment status, spouse’s employment status, place of residence, gestational age, childbirth type, intention to breastfeed duration, and the duration of breastfeeding for previous children. Similarly, in the spouse’s employment status16,41, place of residence42, week of birth40, gestational weeks10,43, the intention to breastfeed duration13 and the duration of breastfeeding for previous child15 do not affect breastfeeding self-efficacy levels. In this regard, it can be said that for this sample, the socio-demographic and obstetric characteristics of mothers are not effective factors in breastfeeding self-efficacy.
A statistically significant, positive, moderate-level relationship was found between MINDF-BFS and BSES scores. This indicates that as mindfulness in breastfeeding increases, breastfeeding self-efficacy also tends to increase. It could be said that mindfulness practices may help mothers become more attuned to their emotions, bodily sensations, and the needs of their babies during breastfeeding. This increased awareness and presence can foster a sense of confidence and competence, which are essential components of self-efficacy. When mothers practice mindfulness, they may be better able to manage stress, remain calm, and focus on the breastfeeding process, which in turn strengthens their belief in their ability to breastfeed successfully.
Strengths and limitations
This study possesses both limitations and strengths. A strength of this study is that, to our knowledge, This study is the pioneering research to evaluate mindfulness breastfeeding This study is the pioneering research to evaluate mindfulness breastfeeding in mothers. Additionally, it demonstrates the relationship between mindfulness breastfeeding and breastfeeding self-efficacy.
As for limitations, the descriptive-correlational nature of the study did not allow for causal inferences. Additionally, mothers were recruited from a single maternity hospital, and the small sample size further limits the generalization of the study’s results.
Conclusion and implication for practice
According to the findings, it could be said that the mothers had a good level of mindfulness breastfeeding and breastfeeding self-efficacy. It was found that as mothers’ economic level increases, both their mindfulness breastfeeding and breastfeeding self-efficacy decrease. Additionally, it was determined that a longer duration of breastfeeding previous child/children is associated with increased mindfulness breastfeeding among mothers.
The results of the present study have important implications for practice and future research. Healthcare providers should evaluate the mindfulness breastfeeding of postnatal women using the Mindfulness Breastfeeding Scale. Additionally, health professionals should consider the sociodemographic and obstetric characteristics of pregnant women in training programs to effectively increase breastfeeding self-efficacy and mindfulness breastfeeding. It is also recommended that future studies be conducted with larger and more diverse samples using the Mindfulness Breastfeeding Scale. Furthermore, experimental studies evaluating the effectiveness of mindful breastfeeding can be planned.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Buonocore, G. Mother’s milk: what more can we do? Global Pediatr. 7, 100123 (2024).
Eidelman, A. I. et al. Breastfeeding and the use of human milk. Pediatrics 129 (3), e827–e841 (2012).
Binns, C., Lee, M. & Low, W. Y. The long-term public health benefits of breastfeeding. Asia Pac. J. Public. Health. 28 (1), 7–14 (2016).
Victora, C. G. et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet 387 (10017), 475–490 (2016).
Grummer-Strawn, L. M. & Rollins, N. Summarising the Health Effects of Breastfeeding 1–2 (Wiley, 2015).
Bomer-Norton, C. Breastfeeding: A holistic concept analysis. Public Health Nurs. 31 (1), 88–96 (2014).
Dennis, C. L. Theoretical underpinnings of breastfeeding confidence: a self-efficacy framework. J. Hum. Lactation. 15 (3), 195–201 (1999).
Meedya, S., Fahy, K. & Kable, A. Factors that positively influence breastfeeding duration to 6 months: a literature review. Women Birth. 23 (4), 135–145 (2010).
Bandura, A. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 84 (2), 191 (1977).
Ergezen, Y. et al. The relationship between mothers’ breastfeeding self-efficacy perceptions and breastfeeding success in postpartum period. Dokuz Eylül Üniversitesi Hemsirelik Fakültesi Elektronik Dergisi. 14 (3), 1 (2021).
Ngo, L. T. H. et al. Breastfeeding self-efficacy and related factors in postpartum Vietnamese women. Midwifery 70, 84–91 (2019).
Çınar, N. et al. Annelerde postpartum depresyon, Sosyal Destek ve emzirme Öz yeterliliği Arasındaki Ilişkinin incelenmesi. Sürekli Tıp Eğitimi Dergisi. 32 (2), 113–122 (2023).
Yang, X. et al. Predictors of breast feeding self-efficacy in the immediate postpartum period: A cross-sectional study. Midwifery 41, 1–8 (2016).
Tsaras, K. et al. Breastfeeding self-efficacy and related socio-demographic, perinatal and psychological factors: a cross-sectional study among postpartum Greek women. Materia socio-medica. 33 (3), 206 (2021).
Küçükoğlu, S., Aytekin, A. & Ateşeyan, S. Yenidoğan Yoğun Bakim ünitesinde Bebeği Yatan Annelerin bebeklerine Anne Sütü Verme eğilimleri Ile emzirme Öz yeterliliklerinin Karşilaştirilmasi. Balıkesir Sağlık Bilimleri Dergisi. 4 (2), 71–78 (2015).
Şenol, D. K. & Pekyiğit, A. Normal Doğum ve Sezaryende Doğum Sonu Stresin emzirme öz-yeterliliğine Etkisi. Jinekoloji-Obstetrik Ve Neonatoloji Tıp Dergisi. 18 (4), 1062–1069 (2021).
Perez-Blasco, J., Viguer, P. & Rodrigo, M. F. Effects of a mindfulness-based intervention on psychological distress, well-being, and maternal self-efficacy in breast-feeding mothers: results of a pilot study. Arch. Women Ment. Health. 16, 227–236 (2013).
Byrne, J. et al. Effectiveness of a mindfulness-based childbirth education pilot study on maternal self‐efficacy and fear of childbirth. J. Midwifery Women’s Health. 59 (2), 192–197 (2014).
Zhang, H. & Emory, E. K. A mindfulness-based intervention for pregnant African-American women. Mindfulness 6, 663–674 (2015).
Vieten, C. et al. The mindful moms training: development of a mindfulness-based intervention to reduce stress and overeating during pregnancy. BMC Pregnancy Childbirth. 18, 1–14 (2018).
Warriner, S., Hunter, L. & Dymond, M. Mindfulness in maternity: evaluation of a course for midwives. Br. J. Midwifery. 24 (3), 188–195 (2016).
Pan, W. L. et al. Assessing the effectiveness of mindfulness-based programs on mental health during pregnancy and early motherhood-a randomized control trial. BMC Pregnancy Childbirth. 19, 1–8 (2019).
Hulsbosch, L. P. et al. Breastfeeding intention and trait mindfulness during pregnancy. Midwifery 101, 103064 (2021).
Korukcu, O. & Kukulu, K. The effect of the mindfulness-based transition to motherhood program in pregnant women with preterm premature rupture of membranes. Health Care Women Int. 38 (7), 765–785 (2017).
Brassel, A. et al. Maternal perinatal mental health: associations with bonding, mindfulness, and self-criticism at 18 months’ postpartum. Infant Mental Health J. 41 (1), 69–81 (2020).
Duncan, L. G. & Bardacke, N. Mindfulness-based childbirth and parenting education: promoting family mindfulness during the perinatal period. J. Child Fam. Stud. 19, 190–202 (2010).
Kantrowitz-Gordon, I., Abbott, S. & Hoehn, R. Experiences of postpartum women after mindfulness childbirth classes: a qualitative study. J. Midwifery Women’s Health. 63 (4), 462–469 (2018).
Sun, Y. et al. Effectiveness of smartphone-based mindfulness training on maternal perinatal depression: randomized controlled trial. J. Med. Internet. Res. 23 (1), e23410 (2021).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences (Routledge, 2013).
Aslan, Y. Annelerin Emzirme öz-yeterliliği Ve Depresyon Riski Ile Ilişkisi (Sağlık Bilimleri Enstitüsü, 2016).
Çalış, A. Annelerin Emzirme öz-yeterliliği Ve Emzirme Süresine Etki Eden Faktörlerin Incelenmesi (Ege Üniversitesi, Sağlık Bilimleri Enstitüsü, 2019).
Korukcu, O. et al. Development and psychometric testing of the ‘mindful breastfeeding scale’ (MINDF-BFS) among postpartum women in Turkey. Curr. Psychol. 42 (7), 5226–5239 (2023).
Dennis, C. L. The breastfeeding self-efficacy scale: psychometric assessment of the short form. J. Obstetric Gynecologic Neonatal Nurs. 32 (6), 734–744 (2003).
Tokat, M. A., Okumuş, H. & Dennis, C. L. Translation and psychometric assessment of the Breast-feeding Self-Efficacy Scale—Short form among pregnant and postnatal women in Turkey. Midwifery 26 (1), 101–108 (2010).
Camacho, E. M. & Hussain, H. Cost-effectiveness evidence for strategies to promote or support breastfeeding: A systematic search and narrative literature review. BMC Pregnancy Childbirth. 20, 1–8 (2020).
Walters, D. D., Phan, L. T. & Mathisen, R. The cost of not breastfeeding: global results from a new tool. Health Policy Plann. 34 (6), 407–417 (2019).
Mercan, Y., Tari, K. & Selcuk Association between postpartum depression level, social support level and breastfeeding attitude and breastfeeding self-efficacy in early postpartum women. PLoS ONE. 16 (4), e0249538 (2021).
Edis, E. K. et al. Acil ve Planlı Sezaryen Olan Kadınların travmatik Doğum Algısı ve emzirme Öz-Yeterlilik Düzeylerinin belirlenmesi. Celal Bayar Üniversitesi Sağlık Bilimleri Enstitüsü Dergisi. 10 (4), 372–380 (2023).
Oliver-Roig, A. et al. The Spanish version of the breastfeeding self-efficacy scale-short form: reliability and validity assessment. Int. J. Nurs. Stud. 49 (2), 169–173 (2012).
Wheeler, B. J. & Dennis, C. L. Psychometric testing of the modified breastfeeding self-efficacy scale (short form) among mothers of ill or preterm infants. J. Obstetric Gynecologic Neonatal Nurs. 42 (1), 70–80 (2013).
Ağar, T. & Yıldırım, F. Preterm Bebek annelerinin maternal bağlanma, emzirme Özyeterliliği ve Bakıma Katılım düzeyleri. Cumhuriyet Üniversitesi Sağlık Bilimleri Enstitüsü Dergisi. 8 (3), 466–475 (2023).
Gökçe, N. E. 0–12 Aylık Bebeği Olan Annelerin Emzirme öz-yeterliliği Ve Anne Sütünü Arttırmaya Yönelik Tamamlayıcı Ve Alternatif Tedavi Kullanma Eğilimleri (Sağlık Bilimleri Enstitüsü, 2019).
Aksoy, Y. E. et al. Postpartum depresyonun emzirme Üzerine Etkisi. Gümüşhane Üniversitesi Sağlık Bilimleri Dergisi. 5 (3), 90–96 (2016).
Acknowledgements
We extend our deepest gratitude to all the mothers for participating in this study and voluntarily contributing their time and insights.
Author information
Authors and Affiliations
Contributions
Study design: EHÖ and NEŞ. Data collection: EHÖ. Data analysis: EHÖ and NEŞ. Study supervision: NEŞ. Manuscript writing: EHÖ and NEŞ. Critical revisions for important intellectual content: NEŞ.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was conducted with the approval of the Hacettepe University Ethics Committee (Approval number: E-35853172-000-00002336323, date: July 5, 2022). Research implementation permission was obtained from the hospital, and permission to use the scale, developed and validated by the researchers, was also obtained. The research methods were performed in accordance with the Helsinki Declaration. Participants’ information was kept confidential throughout the study, and all collected data was coded to ensure anonymity.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Özdemir, E.H., Ercan-Şahin, N. Determination of mothers’ breastfeeding self-efficacy and mindful breastfeeding levels and their relationship. Sci Rep 15, 35959 (2025). https://doi.org/10.1038/s41598-025-07651-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-07651-w