Abstract
Unilateral maxillary sinusitis and maxillary fungal ball (FB) have diverse etiologies. Maxillary sinus diseases are predominantly associated with odontogenic origins. This study aimed to investigate and compare the clinical characteristics of odontogenic maxillary sinus diseases between implant-related and implant-non-related etiologies. This retrospective study enrolled 195 patients with odontogenic maxillary sinus diseases undergoing endoscopic sinus surgery. The patients were categorized into four groups: implant-related and -non-related odontogenic sinusitis and implant-related and -non-related odontogenic FB. The study analyzed sinonasal symptoms, SNOT-22 scores, comorbidities, social history, allergic status, and olfactory function. Computed tomography scans were performed to assess dental disease, implant numbers, implant protrusion depth, and sinus inflammation degree. Smoking and alcohol consumption were significant risk factors for odontogenic maxillary sinusitis development, whereas hypertension and older age were associated with an increased odontogenic FB risk. However, the four groups demonstrated no statistically significant differences in terms of Lund-Mackay scores, SNOT-22 scores, olfactory function tests, allergic status, or comorbidities. Periodontitis and the length of the intramaxillary implant protrusion were important contributing factors in odontogenic maxillary sinus diseases. Odontogenic maxillary sinusitis and odontogenic FB exhibit distinct pathophysiological and clinical characteristics; therefore, these conditions need to be thoroughly understood for effective patient management.
Similar content being viewed by others
Introduction
Unilateral sinus diseases in adults encompass various disease categories with infection or inflammatory disease, as well as benign or malignant tumors. Chronic rhinosinusitis is the most prevalent form of unilateral sinus disease, followed by fungal diseases, benign tumors, and malignancies1. Approximately 25% of patients who underwent endoscopic sinus surgery present with unilateral sinus disease2. Among these patients, the maxillary sinus is the most predominantly affected site. Odontogenic maxillary sinusitis developed due to the close anatomical association between the floor of the maxillary sinus and the premolar and molar teeth. It originates from the spread of inflammation from the maxillary teeth or as a consequence of iatrogenic damage to the Schneiderian membrane of the maxillary sinus during dental procedures3,4. Odontogenic maxillary sinusitis accounts for 25–40% of all maxillary sinusitis cases. The incidence of odontogenic sinusitis (OS) is rising with an aging population and increased opportunities for dental care and dental implants5. With age, the thickness of the maxillary alveolar bone decreases, and only the thin periosteum separates the maxillary sinus from the oral cavity. Furthermore, odontogenic maxillary diseases present as a maxillary fungal ball (FB).
FB is the most prevalent form of noninvasive fungal sinusitis, with the maxillary sinus being the most frequently involved site. The exact pathogenesis of FB remains unclear; however, its incidence has been reported to rise with the increased use of antibiotics, global warming, and dental procedures6,7. An impaired innate mucosal defense system may fail to eliminate inhaled fungal spores from the sinonasal mucosa, resulting in the accumulation of fungal conidia and the subsequent development of FB. Odontogenic factors, such as oroantral fistula, tooth extraction, periodontitis, and endodontic treatment, may contribute to odontogenic FB development8. Maxillary augmentation, the sinus bone graft to increase alveolar bone height for dental implants, frequently uses bone graft materials such as deproteinized bovine bone substitute, which has been associated with FB formation in the maxillary sinus9. The metallic components of endodontic sealers and root canal filling materials promoted fungal biofilm formation and facilitated FB development10,11. Further, exposure of the dental implant surface within the maxillary sinus may serve as a nidus for fungal biofilm formation. This causes mucosal inflammation by impairing the mucociliary transport system, irritating the sinus mucosa, and causing mucosal swelling12.
OS has long been underestimated as a cause of maxillary sinusitis, accounting for approximately 45%–75% of unilateral maxillary sinusitis3,13. The prevalence of OS has elevated with the aging population, the increase in dental procedures, and the development of high-quality diagnostic tools. The incidence of classical odontogenic sinus diseases caused by periodontitis or periodontal abscess has decreased with the improvement in national healthcare systems and dental hygiene. In contrast, the incidence of iatrogenic odontogenic sinus diseases caused by dental procedures and dental implantation continues to increase14. The length of dental implants protruding into the maxillary sinus is associated with the development of maxillary sinusitis. Titanium and zirconia are the main metallic components of dental implants to form osseointegration15. These metallic components exposed to the maxillary sinus could induce fungal growth in the sinus11,12. In this study, we aimed to investigate and compare the clinical characteristics of odontogenic maxillary sinus diseases, specifically maxillary sinusitis and maxillary FB, between implant-related and implant-non-related etiologies.
Materials and methods
Patient selection
A total of 3,623 patients underwent endoscopic sinus surgery between 2013 and 2023, among whom 1,118 received unilateral sinus surgery. Of these, the study enrolled 195 patients based on odontogenic maxillary sinusitis or FB diagnoses, with persistent symptoms despite maximal medical therapy (Fig. 1). The study participants were categorized into four groups: implant-non-related OS (INR-OS), implant-related OS (IR-OS), implant-non-related FB (INR-FB), and implant-related FB (IR-FB). The exclusion criteria were as follows: (1) patients younger than 18 years, (2) diagnosed with antrochoanal polyp, (3) postoperative maxillary cyst or mucocele, (4) invasive fungal sinusitis, (5) inverted papilloma or benign tumors, and (6) malignant tumors. This retrospective study was conducted and all experimental protocols were approved by the Institutional Review Board of Daegu Catholic University Medical Center (CR-24–004). The study was conducted under the guideline of the Institutional Review Board of Daegu Catholic University Medical Center and performed following the Declaration of Helsinki. Due to the retrospective nature of this study, the Institutional Review Board of Daegu Catholic University Medical Center waived the need of obtaining informed consent.
Clinical data collection
Chief complaints, 22-item sinonasal outcome test (SNOT-22) scores, comorbidities, olfactory function test, peripheral blood eosinophil counts, and allergic status were assessed from the medical records. The extent of the disease was identified using preoperative computed tomography (CT) scans and scored according to the Lund–Mackay (LM) scoring system. Endoscopic findings, including the presence of nasal polyps, purulent discharge in the middle meatus, bulging of the uncinate process, and septal deviations, were recorded. Allergic status was determined with either a skin prick test or multiple allergen simultaneous test–chemiluminescent assay against a standard panel of aeroallergen. Olfactory function was assessed using the Korean version of the Sniffin’s Stick test, which assesses the total threshold–discrimination–identification score16.
Diagnostic CT findings
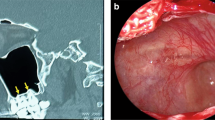
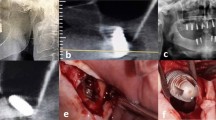
OS and FB were diagnosed based on CT findings and dental examination. Periapical or periodontal pathologies were identified on CT as nonexpansile radiolucency within the alveolar bone. An oroantral fistula was defined as a direct communication between the oral cavity and the maxillary sinus observed during the clinical examination. The number of inserted dental implantations and the presence of periimplantitis, defined as radiolucency in the alveolar bone surrounding the implants, were identified using CT. The intramaxillary exposed length of the dental implant was the distance from the point of implant extrusion into the maxillary sinus to thee bony cortical lining of the maxillary sinus floor (Fig. 2)15. Other dental pathologies, such as dental extraction, endodontic treatment, and maxillary augmentation, were assessed based on the dental treatment history.
Odontogenic maxillary sinusitis identified by coronal view of paranasal sinus computed tomography. (A) Periapical lucency in left maxillary sinus floor. (B) endodontic-maxillary erosion in left maxillary sinus. (C) Implant protrusion into the left maxillary sinus. The distance between the post of greatest protrusion (a) and the inner bony cortical lining of the maxillary sinus (b) was measured to determine the length of the implant extrusion into the maxillary sinus.
Statistical analysis
Statistical Package for the Social Sciences version 25.0 Software (IBM Inc., Armonk, NY, USA) was used for statistical analysis. Clinicopathologic differences between OS and FB were evaluated using the two-sample t-test and chi-square test. Comparisons among the four groups were conducted using one-way analysis of variance and the chi-square test for univariate analysis. Multivariate analysis was conducted using multinomial logistic regression analysis to calculate the odds ratio (OR), adjusting for potential clinical confounding factors such as age, sex, hypertension, smoking, and alcohol consumption. Two-tailed statistical analysis with a p-value of 0.05 indicated statistical significance.
Results
Demographic characteristics and risk factors for the development of maxillary sinus diseases
This study enrolled 66 patients with INR-OS (38 men, 28 women, mean age of 52.1 ± 14.2), 31 patients with IR-OS (21 men, 10 women, mean age of 52.6 ± 8.8), 57 patients with INR-FB (14 men, 43 women, mean age of 66.9 ± 8.9), and 41 patients with IR-FB (21 men, 20 women, mean age of 65.6 ± 8.6). Patients with FB were generally older and more prevalent in females compared with patients with sinusitis. Notably, the proportion of females was significantly higher in the INR-FB group than in the other groups (INR-OS: 42.4%, IR-OS: 32.3%, INR-FB: 75.4%, and IR-FB 48.8%). Patients with INR-OS were younger (52.1 ± 14.2) than those with IR-OS (62.63 ± 8.8). No significant differences in terms of L-M CT scores, peripheral blood eosinophil counts, olfactory test scores, or SNOT-22 scores were found among four groups. Similarly, the incidence of comorbidities such as allergy, hypertension, and diabetes did not differ significantly among the groups. However, smoking rate and alcohol consumption were significantly different among the four groups. Further, the smoking and alcohol consumption rates were more prevalent in the sinusitis groups than to the FB groups (Table 1). To identify the risk factors associated with OS development, multivariate analysis was performed, including variables such as age, sex, hypertension, diabetes, smoking, and alcohol consumption. Compared to the INR-OS group, the other groups demonstrated a higher risk of disease development in older age groups and the INR-FB group exhibited a higher risk in female patients. Hypertension was strongly associated with the implant-related groups (IR-OS: OR = 2.66, IR-FB: OR = 3.27). In contrast, smoking and alcohol consumption were inversely associated with the FB group (INR-FB: smoking OR = 0.21, alcohol OR = 0.34; IR-FB: smoking OR = 0.36, alcohol OR = 0.31) (Table 2).
Clinical characteristics
The main symptoms reported by patients with INR-OS were foul odor (22.7%), posterior nasal drip (21.2%), nasal obstruction (19.7%), and facial pain (18.2%). The most prevalent symptoms in patients with IR-OS were foul odor (19.4%), followed by rhinorrhea (19.4%) and nasal obstruction (16.1%). Approximately one-third of the patients in FB cases visited without nasal discomfort (25.5%) or any other symptoms (16.3%). In patients with sinusitis, more than 30% of cases involved more than one sinus (32.0%), whereas patients with FB, over 85% of cases were confined to the maxillary sinus (87.8%). Nasal polyp and septal deviation are predominantly observed in patients with sinusitis (18.6% and 25.8% respectively), whereas 53.1% of patients with FB demonstrated no abnormal findings on endoscopic examination (Table 3).
CT findings
Periodontitis was the most prevalent pathological finding on CT scans in implant-non-related sinus disease groups (INR-OS: 53.0%, INR-FB: 91.2%). In the implant-related sinus disease groups, dental implant protrusion into the maxillary sinus was the most frequent finding (IR-OS: 71.0% and IR-FB 58.5%), followed by periimplantitis and osteomyelitis. The average number of dental implants was not significantly different between the two groups, the length of the intramaxillary protrusion was significantly longer in the sinusitis group (4.9 ± 2.7 mm) than in the FB group (3.3 ± 1.9 mm) (Table 4).
Trends in odontogenic sinus diseases
The number of odontogenic sinus diseases increased from 11 to 49 cases from 2013 to 2023, and implant-related sinus diseases tended to increase from 18.2% in 2013 to 69.4% in 2023 (Fig. 3).
Discussion
The maxillary sinus is the most commonly affected anatomical site in unilateral sinusitis, which is caused by various conditions, including nasal polyps, FB, inverted papilloma, and benign or malignant tumors. Acute or chronic maxillary sinusitis and FB are the most prevalent cases of unilateral maxillary sinus diseases that require surgical treatment. The floor of the maxillary sinus is located close to the first and second molar teeth and is separated only by a thin layer of alveolar bone and the Schneiderian membrane, which facilitates the spread of dental infection into the sinus. During the study period, 1118 patients underwent endoscopic sinus surgery for unilateral sinusitis. Among them, 436 had unilateral maxillary diseases, 201 with unilateral maxillary sinusitis, and 235 with unilateral FB. Of the patients with unilateral maxillary sinus diseases, 97 had odontogenic maxillary sinusitis and 98 had unilateral FB. This study focused on 195 patients with odontogenic sinus diseases, including 123 with simple odontogenic cases and 72 with implant-related cases. The proportion of patients with unilateral maxillary sinus diseases among those undergoing unilateral endoscopic sinus surgery has increased along with a marked rise in the number of patients since 2021. However, the proportion of odontogenic maxillary sinus diseases among all unilateral maxillary sinus diseases has not significantly changed (33.3%– 55.0%) (Table S1).
The increasing elderly population and the rising frequency of dental procedures contribute to the higher incidence of odontogenic maxillary sinusitis and FB3,9,17. As reported in previous studies, odontogenic FB (INR-FB and IR-FB) occurred more frequently in older (66.3 ± 8.7 years) female (64.3%) patients compare with sinusitis (INR-OS and IR-OS) (55.5 ± 13.6 years and 39.2%, respectively). However, this female predominance was not observed in IR-FB cases, indicating that dental implants may be an important risk factor for the development of maxillary sinus FB. Dental implants are predominantly performed in the elderly population; thus, the average age of patients in the IR-OS group (62.6 ± 8.8 years) was older than that in the INR-OS group (52.1 ± 14.2 years). The number of dental implants did not significantly differ between the IR-OS and IR-FB groups; however, the intramaxillary penetration length of the dental implant was significantly longer in the IR-OS (4.9 ± 2.7 mm) than in the IR-FB group (3.3 ± 1.9 mm) (p = 0.044). These results indicate that longer implant protrusion into the maxillary sinus may cause Schneiderian membrane perforation and promote bacterial growth and mucosal inflammation. Park et al. revealed that dental implants protruding more than 4 mm into the maxillary sinus are significantly associated with implant-related OS15. Among 72 patients, whom associated with dental implants, the incidence of FB was higher (56.9%) than patients with INR-FB cases (46.3%). The exact reason is difficult to explain, it is hypothesized that metal ions from the implant may act as a nidus for fungal growth. Intramaxillary fungal spores inhaled during respiration may come into contact with the metallic components of dental implant, which can serve as a medium for fungal growth and biofilm12. The overfilling or displacement of root canal sealers during endodontic treatment may contribute to the development and progression of maxillary sinus fungal ball18.
Foul odor, nasal obstruction, posterior nasal drip, and facial pain were common symptoms in patients with OS (INR-OS and IR-OS). Over than 30% of these cases involved multiple sinuses and approximately 20% presented with middle meatal nasal polyps. Rhinorrhea, posterior nasal drip, and facial pain were the predominantly reported symptoms in cases of odontogenic FB (INR-FB and IR-FB). However, more than one-third patients with FB demonstrated no sinonasal symptoms (45.6% in INR-FB and 36.6% in IR-FB). The higher incidence of FB being diagnosed without specific discomfort or sinus symptoms may be attributed to an increased aging population, advancement in imaging diagnostic techniques such as CT and magnetic resonance imaging, and the increased frequency of routine health checkups. Over 80% of patients with FB involved only the maxillary sinus and less than 5% demonstrated nasal polyps. OS frequently responds poorly to antibiotics or medical therapy without controlling the underlying dental pathology. Compared with odontogenic FB, OS may induce a more sustained and active inflammatory response in the sinonasal mucosa. This can lead to nasal obstruction and the involvement of not only the maxillary sinus but also other paranasal sinuses, frequently accompanied by nasal polyps. Anaerobic bacteria, which are predominantly implicated in OS, may contribute to the characteristic symptom of a foul odor.
Smoking and alcohol consumption are lifestyle habits that contribute to various diseases and negatively affect public health. Smoking alters ion conduction, mucociliary clearance, and local inflammatory pathways in the sinonasal mucosa19,20. Alcohol consumption is not significantly associated with sinusitis, but it may aggravate nasal symptoms with largely unknown underlying mechanisms20,21. High blood pressure is a potential risk factor affecting bone metabolism and microcirculation. Hypertension negatively affects on bone remodeling and angiogenesis22. We conducted a multivariate analysis of smoking, alcohol consumption, and hypertension to identify risk factors for the development of OS and FB. Smoking and alcohol consumption were associated with significantly lower OR of being diagnosed with INR-FB (OR = 0.21 and 0.34, respectively) or IR-FB (OR = 0.36 and 0.31, respectively), compared with INR-OS. This indicates that smoking exhibited approximately 4.76 and 2.78 times higher odds of being diagnosed with INR-OS than with INR-FB and IR-FB, respectively. Similarly, alcohol consumers had approximately 2.94 and 3.23 times higher odds of being diagnosed with INR-OR than with INR-FB and IR-FB, respectively. In contrast, hypertension was significantly associated with an approximately 2.66 times and 3.27 times higher odds of having a FB than INR-OR. These results indicate smoking and alcohol consumption as significant risk factors for INR-OS development, whereas hypertension is an independent risk factor for developing FB.
This study has several limitations. First, this is a single-center study, which may have limited the number of patients included. Further, accurately identifying the preceding or concurrent dental diseases at the time of sinus surgery was difficult. Furthermore, the varying follow-up periods after sinus surgery made it difficult to assess the prognosis of the enrolled patients. Finally, there was no unified definition of odontogenic sinus diseases and diagnosing odontogenic diseases based on CT findings and medical records poses a limitation in this study.
Odontogenic maxillary sinusitis and odontogenic FB exhibit distinct pathophysiological and clinical characteristics; therefore, a thorough understanding of these conditions is crucial for effective patient management. Our study demonstrated that smoking and alcohol consumption as significant risk factor OS development, whereas hypertension and older age are associated with an increased risk of odontogenic FB. Further, intramaxillary dental implant plays a significant role as a causative factor in odontogenic maxillary diseases. In general, dental implants and other dental diseases are associated with the development of OS and odontogenic FB. Close collaboration between dentistry and rhinology is crucial for advancing our understanding of the pathophysiology, treatment, and prognosis of odontogenic sinus diseases.
Data availability
Data are available from the corresponding author upon reasonable request.
References
Paz Silva, M. et al. Diagnostic algorithm for unilateral sinus disease: A 15-year retrospective review. Int. Forum. Allergy. Rhinol. 5, 590–596. https://doi.org/10.1002/alr.21526 (2015).
Beswick, D. M. et al. Comparison of surgical outcomes between patients with unilateral and bilateral chronic rhinosinusitis. Int. Forum. Allergy. Rhinol. 7, 1162–1169. https://doi.org/10.1002/alr.22020 (2017).
Craig, J. R. et al. Diagnosing odontogenic sinusitis: An international multidisciplinary consensus statement. Int. Forum. Allergy. Rhinol. 11, 1235–1248. https://doi.org/10.1002/alr.22777 (2021).
Lin, J. et al. Expert consensus on odontogenic maxillary sinusitis multi-disciplinary treatment. Int. J. Oral. Sci. 16, 11. https://doi.org/10.1038/s41368-024-00278-z (2024).
Galie, M. et al. Unilateral sinus disease: not just odontogenic! - A retrospective study. Ann. Maxillofac. Surg. 10, 397–401. https://doi.org/10.4103/ams.ams_268_19 (2020).
Lee, J. S., Shin, S. Y., Lee, K. H., Kim, S. W. & Cho, J. S. Change of prevalence and clinical aspects of fungal ball according to temporal difference. Eur. Arch. Otorhinolaryngol. 270, 1673–1677. https://doi.org/10.1007/s00405-012-2234-x (2013).
Kim, D. W. et al. Clinicopathologic characteristics of paranasal sinus fungus ball: Retrospective, multicenter study in Korea. Eur. Arch. Otorhinolaryngol. 277, 761–765. https://doi.org/10.1007/s00405-019-05738-5 (2020).
Pagella, F. et al. Paranasal sinus fungus ball: Diagnosis and management. Mycoses 50, 451–456. https://doi.org/10.1111/j.1439-0507.2007.01416.x (2007).
Scolozzi, P., Perez, A., Verdeja, R., Courvoisier, D. S. & Lombardi, T. Association between maxillary sinus fungus ball and sinus bone grafting with deproteinized bovine bone substitutes: A case-control study. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 121, e143-147. https://doi.org/10.1016/j.oooo.2016.01.022 (2016).
Park, G. Y., Kim, H. Y., Min, J. Y., Dhong, H. J. & Chung, S. K. Endodontic treatment: A significant risk factor for the development of maxillary fungal ball. Clin. Exp. Otorhinolaryngol. 3, 136–140. https://doi.org/10.3342/ceo.2010.3.3.136 (2010).
Shin, S. H., Ye, M. K., Lee, D. W. & Choi, M. H. Impact of zinc oxide on the development of aspergillus-induced maxillary sinusitis rabbit model. Curr. Issues. Mol. Biol. 46, 5712–5723. https://doi.org/10.3390/cimb46060342 (2024).
Han, S. A. et al. Dental implant as a potential risk factor for maxillary sinus fungus ball. Sci. Rep. 14, 2483. https://doi.org/10.1038/s41598-024-52661-9 (2024).
Turfe, Z., Ahmad, A., Peterson, E. I. & Craig, J. R. Odontogenic sinusitis is a common cause of unilateral sinus disease with maxillary sinus opacification. Int. Forum. Allergy. Rhinol. 9, 1515–1520. https://doi.org/10.1002/alr.22434 (2019).
Kim, S. J. et al. Clinical features and treatment outcomes of dental implant-related paranasal sinusitis: A 2-year prospective observational study. Clin. Oral. Implants. Res. 27, e100–e104. https://doi.org/10.1111/clr.12570 (2016).
Park, M. J. et al. Features of odontogenic sinusitis associated with dental implants. Laryngoscope 133, 237–243. https://doi.org/10.1002/lary.30069 (2023).
Cho, J. H. et al. The Korean version of the Sniffin’ stick (KVSS) test and its validity in comparison with the cross-cultural smell identification test (CC-SIT). Auris Nasus Larynx 36, 280–286. https://doi.org/10.1016/j.anl.2008.07.005 (2009).
Psillas, G., Papaioannou, D., Petsali, S., Dimas, G. G. & Constantinidis, J. Odontogenic maxillary sinusitis: A comprehensive review. J. Dent. Sci. 16, 474–481. https://doi.org/10.1016/j.jds.2020.08.001 (2021).
Federici, F. R. et al. Correlation between fungus ball of maxillary sinus and previous root canal therapy. Care report and narrative literature review. Ann. Stomatol. 15, 250–255. https://doi.org/10.59987/ads/2024.4 (2024).
Christensen, D. N., Franks, Z. G., McCrary, H. C., Saleh, A. A. & Chang, E. H. A systematic review of the association between cigarette smoke exposure and chronic rhinosinusitis. Otolaryngol. Head. Neck. Surg. 158, 801–816. https://doi.org/10.1177/0194599818757697 (2018).
Wang, X., Bi, Y., Liu, G., Wang, W. & Cui, H. Smoking and alcohol consumption with the risk of 11 common otolaryngological diseases: A bidirectional Mendelian randomization. Eur. Arch. Otorhinolaryngol. 280, 5615–5623. https://doi.org/10.1007/s00405-023-08246-9 (2023).
De Schryver, E. et al. Alcohol hyper-responsiveness in chronic rhinosinusitis with nasal polyps. Clin. Exp. Allergy. 47, 245–253. https://doi.org/10.1111/cea.12836 (2017).
Hamade, L., El-Disoki, S. & Chrcanovic, B. R. Hypertension and dental implants: A systematic review and meta-analysis. J. Clin. Med. 13, 499. https://doi.org/10.3390/jcm13020499 (2024).
Author information
Authors and Affiliations
Contributions
Mi-Kyung Ye and Seung-Heon Shin contributed to the conception of the study; Tae-Gyun Kim and Chang-Ho contributed significantly to analysis and manuscript preparation; Tae-Gyun Kim and Seung-Heon Shin performed the data analyses and wrote the manuscript; All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, TG., WhangBo, CH., Ye, MK. et al. Comparative analysis of clinical characteristics of odontogenic maxillary sinus diseases associated with or without dental implants. Sci Rep 15, 20781 (2025). https://doi.org/10.1038/s41598-025-07832-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-07832-7