Abstract
To evaluate the correlation between plasma fibrinogen levels and acute myocardial infarction (AMI) in the Chinese Han population. A total of 1522 patients with incident AMI and 6125 controls were recruited between January 1, 2010, and December 31, 2013. The relationship between fibrinogen levels and incident AMI was evaluated using multivariable-adjusted logistic regression, and the possible interaction effects between fibrinogen and other risk factors on incident AMI were investigated. When modeled as a continuous variable, a 1 g/L increase in fibrinogen level was associated with a 91% increase in the risk of AMI [odds ratio (OR):1.91; 95% confidence interval (CI):1.63–2.23 in women, 1.86:1.70–2.03 in men, and 1.85:1.72–2.00 in total]. Compared to 1st quartile of fibrinogen levels, the adjusted ORs for first incident AMI was 3.25 (2.67–3.96) for the fourth quartile, 1.61 (1.30–1.99) for the third one, 1.18 (0.96–1.46) for the second one (P < 0.001). High fibrinogen levels are associated with an increased risk of incident AMI in the Chinese Han population, and fibrinogen could be an important biomarker for AMI risk assessment.
Similar content being viewed by others
Introduction
Biomarkers can provide guidance for the diagnosis and treatment of acute myocardial infarction (AMI), however, the reliable and easy-to-assess biomarkers are lacking. Troponins are the most important cardiac proteins involved in the diagnosis of AMI, but it can be elevated under clinical conditions except for AMI1. Natriuretic peptides, as quantitative biomarkers of hemodynamic myocardial stress and heart failure, can be significantly increased in AMI patients2. However, natriuretic peptides are rapidly degraded both in vivo and in vitro, moreover, show larger and more asymmetrical intra- and inter-individual distributions3. Therefore, it is necessary to pay more attention to identify new biomarkers with possible roles in the diagnosis of AMI. Plasma fibrinogen, an acute phase reactant, is involved in platelet cross-linking, aggregation, and clot formation in acute coronary events4,5. Data supports a positive association between plasma fibrinogen levels and AMI risk6,7,8. However, most of these research data were acquired before the wide application of coronary angiography and interventional treatment strategy when the diagnosis of AMI was largely based on manifestations, cardiac enzymes, and 12-lead ECG9,10, but not on the “gold” standard of coronary angiography. Most of these studies were conducted in Western participants, who have different genetic backgrounds and disease patterns compared to Asian patients11,12. Meanwhile, geographical and ethnic variations also contribute to the discrepancy in fibrinogen levels among different populations13,14, as evidenced by a modestly higher level of fibrinogen in Blacks than in Whites15. Therefore, how fibrinogen affects AMI in the Chinese population with coronary angiography remains undetermined.
Moreover, published studies focusing on the association of plasma fibrinogen with AMI in the Han population were mostly based on small sample study subjects, ranging from 418 male myocardial infarction patients7 to 650 coronary artery disease (CAD) patients16. No studies with large sample sizes are available to investigate how fibrinogen affects AMI in Chinese patients. Therefore, we conducted the present large sample-sized study among Chinese participants to investigate plasma fibrinogen levels and how it affects AMI in the Chinese Han population, as well as to explore the interactions between fibrinogen and other risk factors.
Materials and methods
Database
Case Collection and Scientific ReSearch System for Clinical Cardiology (CCSSSCC), which contains more than 80 000 consecutive patients from the Division of Cardiology in 1st Affiliated Hospital of Soochow University from 2002-01-0117, was authorized for use in this study18. Data on demographic factors, lifestyle, vital signs, history of cardiovascular disease and other comorbidities, laboratory measurements, medications at discharge, and coronary angiography results were systematically collected19. The study adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of our hospital (361).
Study population
This study was retrospectively designed. The patient data were collected from the Department of Cardiovascular Medicine in the First Affiliated Hospital of Soochow University for the period 1 January 2010 to 31 December 2013. The Institutional Review Boards waived the need for informed consent before analysis due to its retrospective nature. The collection of blood samples and measurement of fibrinogen levels were part of routine procedure for both the research and control groups. Patients with the following conditions were excluded18:1) hepatic/renal/thyroid function abnormalities; 3) uremia or dialysis; 5) malignant tumors; 6) anemia; 7) ischemic heart disease or prior coronary artery disease (defined below); 8) chronic inflammatory diseases; and 9) coexistence of anyone mentioned above.
Admission data was obtained from patients with multiple hospitalizations. A total of 42 (0.55%), 47 (0.61%), and 54 (0.71%) systolic blood pressure, diastolic blood pressure, and heart rate, respectively, were missing.
CAD was diagnosed according to coronary angiography (CAG) showing stenosis ≥ 50% and involving at least one epicardial coronary artery. The first incident of AMI was identified as the 1st AMI diagnosis in our study20. A total 1522 of incident AMI patients and 6125 non-CAD patients from the same period were included. Initial ischemic heart disease was defined as signs of heart disease caused by restricted coronary blood supply and was first diagnosed by our hospital without coronary procedures. Prior CAD was defined based on MI history or coronary procedures.
Laboratory test
Blood samples were collected after eight hours of fasting on 2nd morning of admission for laboratory testing. Fibrinogen levels were measured using an automatic coagulometer (CS-5100 analyzer; Sysmex Corporation, Japan). The assay range was 2.0–4.0 g/L. The other biochemical markers were determined according to the manufacturer’s instructions.
Statistical analysis
The participants were categorized into four groups based on fibrinogen quartiles. All continuous variables were non-normally distributed and expressed as median (inter quartile range, IQR). The categorical variables were expressed as frequencies and percentages. Unconditional logistic regression with fibrinogen quartiles as dummy variable and the 1st quartile as a reference, was performed for model fitting of first incident AMI on the fibrinogen. Crude model reported crude odds ratios (ORs) without adjustment for any risk factors and Adjusted model 1 generated adjusted ORs with the adjustment for age, sex, smoking, triglycerides, hypertension, diabetes, drinking, and lipoprotein (a) (Lp(a)); adjusted model 2 generated adjusted ORs with the adjustment for age, sex, smoking, triglycerides, hypertension, diabetes, drinking, Lp(a), aspirin use and anticoagulant use. Variance inflation factor (VIF) was used to identify the potential presence of multi-collinearity among covariates in the models, and a VIF > 5 was considered for the presence of collinearity. Therefore, total cholesterol (TC), low density lipoprotein cholesterol (LDL-C), weight, body mass index (BMI) and apo A were removed from the model fitting. The stratification/interaction test of risk factors was performed dichotomously, trichotomously or medially when appropriate. Propensity score matching (PSM) was performed to balance potential confounders between the low-fibrinogen and high-fibrinogen groups. The propensity score was estimated using a logistic regression model that included the following covariates: age, sex, smoking status, total cholesterol, marital status, hypertension, diabetes, triglycerides, body mass index (BMI), heart rate, fasting glucose, anticoagulant use, lipoprotein(a), apolipoprotein A, apolipoprotein B, apolipoprotein A1B, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). Matching was performed using a 1:1 nearest neighbor algorithm with a caliper of 0.2. The balance of covariates between groups was assessed using standardized mean differences (SMD), with an SMD < 0.1 indicating good balance. All analysis and graphics were completed with STATA 15.0. Two-tailed P < 0.05 was considered to be statistically significant.
Results
The data of 13,004 patients were firstly collected, and because of complications, repeat hospitalizations, and ischemic heart disease or CAD, the data of 1345, 2067, and 1945 patients were removed, respectively. Finally, the data of 7647 individuals (1522 AMI patients and 6125 non-CAD ones, Fig. 1) were analyzed.
Fibrinogen quartiles
Plasma fibrinogen levels were higher in AMI patients compared to non-CAD ones (3.0 vs. 2.8 g/L, P < 0.01). As expected, patients in higher fibrinogen quartiles had a higher prevalence of risk factors, including older age, hypertension, and diabetes. Laboratory results also showed higher LDL-C, increased Lp(a), higher triglyceride levels, and lower albumin concentrations in the higher fibrinogen quartiles (Table 1).
Distribution of plasma fibrinogen and its quartile partitioning in non-CAD patients
The plasma fibrinogen levels were approximately normally distributed, as shown in Fig. 2. The mean and median in men, women, and the whole population were 2.75 and 2.80; 2.84 and 2.90; and 2.80 and 2.80 g/L, respectively. Table 2 presents fibrinogen quartiles and their statistical parameters.
High fibrinogen level and first incident AMI
In multivariable analysis, a 1.0 g/L fibrinogen increase was associated with an increased OR (95%CI) for 1st incident AMI in females, males, and the whole population (1.91 (1.63–2.23); 1.86 (1.70–2.03); and 1.85 (1.72–2.00); Table 3).
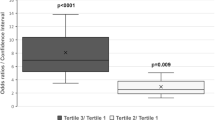
Association of fibrinogen levels with first incident AMI on a categorical scale
Compared to 1st quartile, adjusted OR (95%CI) for first incident AMI was 3.25 (2.67–3.96), 1.61 (1.30–1.99), and 1.18 (0.96–1.46) for the 4th, 3rd, and 2nd quantile, respectively (P < 0.001, Fig. 3) in adjusted model 1, and the trend held truth when further adjusted with aspirin use and anticoagulant use.
Fibrinogen and other risk factors
In our study, fibrinogen levels were significantly correlated with sex, smoking, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), lipoprotein (a) (Lp(a)), triglycerides (TG), body mass index (BMI), primary hypertension, ischemic stroke, and age, with correlation coefficients of 0.0020, 0.0508, 0.0981, -0.0869, 0.1451, 0.0014, 0.0323, 0.1301, -0.0702, and 0.1781, respectively. The significant correlations between fibrinogen levels and other risk factors, such as LDL-C, triglycerides, and hypertension, suggest that fibrinogen may be influenced by metabolic and inflammatory pathways. These associations highlight the complex interplay between fibrinogen and cardiovascular risk factors, underscoring the need for a comprehensive approach to risk assessment and management.
Subgroup analysis
The results demonstrated a consistent association between fibrinogen and incident AMI, although interactions were observed between fibrinogen, triglyceride, HDL-C, and drinking on the risk of the first incident AMI (P < 0.05) (Table 4).
Sensitive analysis
To further validate the robustness of our findings while preserving the original sample size, we conducted a post-hoc propensity score matching (PSM) analysis. Patients were stratified into two groups based on the median fibrinogen level, with the low-fibrinogen group (≤ median) and the high-fibrinogen group (> median). PSM was performed using a logistic regression model that incorporated the following covariates: age, sex, smoking status, total cholesterol, marital status, hypertension, diabetes, triglycerides, body mass index (BMI), heart rate, fasting glucose, anticoagulant use, lipoprotein(a), apolipoprotein A, apolipoprotein B, apolipoprotein A1B, high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). The Love plot demonstrates the standardized mean differences (SMD) for all covariates before and after propensity score matching. After matching, all covariates were well-balanced (SMD < 0.1), indicating that the matching process effectively reduced potential confounding. (Fig. 4). Subsequent logistic regression analysis revealed that elevated fibrinogen levels remained significantly associated with acute myocardial infarction (AMI) (OR = 1.33, 95% CI: 1.25–1.42, p < 0.001), which was consistent with our primary findings. This methodological approach not only addressed potential confounding through rigorous matching but also maintained statistical power by retaining the full cohort in the analysis.
Discussion
This study demonstrated that (i) fibrinogen level was approximately normally distributed with a mean of 2.80 g/L; (ii) plasma fibrinogen level was positively correlated with AMI risk when assessed both as continuous and categorical variables, and this association remained consistent in various subgroup analyses with multivariable adjustment; and (iii) the fibrinogen-AMI association was dose-dependent. An approximately normal distribution of fibrinogen in this Chinese population has been similarly observed in a European population21. The baseline fibrinogen levels were reported to be 263.5 ± 81.98 mg/dL in the NSTEMI group and 291.72 ± 76.63 mg/dL in the STEMI group in an Indian study22, which were lower than our results (326 ± 96 mg/dL). The difference may be explained by the older mean age in our study (63.53 ± 12.54 years vs. 57.5 ± 10.36 years) because previous studies have demonstrated that fibrinogen levels increased with age23,24. And it’s essential to consider whether elevated fibrinogen levels in AMI patients are a primary factor or a secondary response to underlying triggers such as inflammation, metabolic disturbances, lifestyle factors, or genetic predisposition. While fibrinogen is undoubtedly linked to increased cardiovascular risk, understanding its role as a marker or mediator can significantly influence management strategies. Identifying and addressing the primary causes behind fibrinogen elevation through targeting inflammatory pathways, improving metabolic health, or modifying lifestyle factors—could provide more effective approaches to reducing AMI risk. Further research is necessary to unravel the complex interplay of these factors and to develop tailored interventions that address the specific underlying mechanisms leading to increased fibrinogen levels and cardiovascular risk. Our study demonstrated that per 1.0 g/L increase of fibrinogen was correlated to an adjusted OR of 1.85 (1.72–2.00) for first incident AMI, similar to the results (1.78 (95%CI 1.19–2.66]) of a meta-analysis of 154 211 people from 31 prospective studies25. The positive association remained consistent when the fibrinogen level was assessed as a categorical variable. In De Luca, G., et al. ’s study, patients with stable angina were divided into quintiles of fibrinogen levels. Compared to the 1st quartile, the adjusted OR of the 5th one was 1.34, (1.03–1.76) (P = 0.034)21. The correlation between fibrinogen and angina or AMI is due to fixed stenosis, plaque rupture, and thrombosis26. These findings suggest that lifestyle modification could decrease the occurrence of the first incident of AMI27,28,29,30.
The potential mechanisms that explain the positive association between elevated fibrinogen levels and increased AMI risk are as follows: Previous studies have reported the role of fibrinogen in coronary plaques, including endothelial dysfunction, extracellular matrix degradation, and platelet activation25,26,31,32,33,34. Fibrinogen interacts with activated platelets and causes platelet aggregation, which is enhanced during inflammation35 and modulates subsequent clotting and fibrinolysis21. More importantly, higher fibrinogen levels are associated with hypercoagulative states, which affect thrombus formation during coronary injuries.
In this study, it is identified that fibrinogen level is influenced by other risk factors. These associations highlight a complex interplay between fibrinogen and various cardiovascular risk factors. Elevated fibrinogen levels, particularly in combination with these risk factors, may indicate an increased risk of acute myocardial infarction. This suggests that fibrinogen could serve as a valuable biomarker for cardiovascular risk stratification. Emerging literature supports the clinical utility of fibrinogen as a prognostic tool. For instance, a study found that fibrinogen levels predict future cardiovascular events independently of traditional risk factors14. Moreover, the interaction of fibrinogen with factors like triglycerides and HDL-C could provide insights into the pathophysiology of cardiovascular diseases, potentially guiding more tailored therapeutic strategies. Thus, while fibrinogen’s role in cardiovascular pathology is influenced by its interaction with other risk factors, its assessment in clinical settings can provide additional, meaningful information for the management of cardiovascular health, underscoring its potential inclusion in comprehensive risk assessment models.
Strengths
To the best of our knowledge, this is the first large-scale cross-sectional study of fibrinogen and AMI in Han Chinese, which demonstrated the distribution, concentration, and relationship between fibrinogen and AMI. This study is based on a large-scale cohort of 7,647 patients (1,522 AMI cases and 6,125 non-CAD controls), which, by employing minimal exclusion criteria, encompasses a broader spectrum of clinical heterogeneity (e.g., varying glycemic control levels and comorbid conditions). This approach enhances the generalizability and clinical applicability of the findings.
Limitations
This study had several limitations. First, because of the inherent limitations of a cross-sectional study, the causality between fibrinogen levels and the onset of AMI was inadequately established, and the potential confounding factors might not have been fully addressed despite adjustments. For example, it would be better to stratify CAG data according to the fibrinogen level. Second, 1345 patients were excluded because of liver and renal abnormalities, uremia, on dialysis, thyroid function abnormalities, malignant tumors, and anemia, which may impede the extrapolation of our results and reduce potential bias in our analysis. Third, this was a single-center study with Han Chinese patients, and the exclusion criteria might introduce selection bias, limiting the generalizability to a healthier subset of the population. Whether these findings can be generalized to other populations remains unclear. Further multicenter studies are required to confirm our findings. And some major limitations in study design exist.
It is important to acknowledge that our study design, being observational in nature, cannot establish a causal relationship between fibrinogen levels and acute myocardial infarction (AMI). The possibility that fibrinogen levels might have risen secondary to AMI itself must be acknowledged. The timing of blood sampling (the morning after admission) may not fully capture the dynamic changes in fibrinogen levels during the acute phase of AMI. However, this design was chosen based on the feasibility of clinical practice, as post-admission morning sampling is a routine procedure in many hospitals. While our study primarily aimed to explore the association between fibrinogen levels and AMI risk, we recognize that future studies should adopt more rigorous designs, such as prospective cohort studies or randomized controlled trials, to investigate the causal relationship. Additionally, measuring fibrinogen levels at the time of admission, alongside troponin levels, could provide more clinically relevant insights. These limitations highlight the need for further research to validate the potential role of fibrinogen as a biomarker in AMI risk assessment.
While our findings suggest that fibrinogen may serve as a valuable biomarker for AMI risk assessment, the clinical utility of fibrinogen is limited by the timing of blood sampling in this study. Since fibrinogen levels were measured the morning after admission, they may have been influenced by the acute phase response to AMI. It is important to note that our current sampling time aligns with routine clinical practice, and our results demonstrate the relationship between fibrinogen levels measured on the morning after admission and AMI risk. However, to further explore the potential of fibrinogen as an early diagnostic biomarker, future studies should aim to collect blood samples at the time of hospital presentation and evaluate its diagnostic performance in conjunction with established markers such as troponin.
Conclusions
High plasma fibrinogen levels were associated with AMI risk in the Chinese Han individuals in a dose-dependent manner. It is suggested that fibrinogen could be an important biomarker for AMI risk assessment and significantly influence management strategies. Further studies are necessary to clarify the nature of this association and explore potential causal mechanisms.
Data availability
All relevant data are within the manuscript and its supplementary Table 1. The data are uploaded into Figshare repository that the link to access the raw data is: https://figshare.com/search? q=10.6084%2Fm9.figshare.23898021.This published article https://pubmed.ncbi.nlm.nih.gov/26471834/ has been referred to in the current manuscript for the description of CCSSSCC database and the exclusion criteria of patients. Both studies were conducted by our team on the basis of the same dataset CCSSSCC.
References
Aydin, S., Ugur, K., Aydin, S., Sahin, İ. & Yardim, M. Biomarkers in acute myocardial infarction: current perspectives. Vasc Health Risk Manag. 15, 1–10. https://doi.org/10.2147/VHRM.S166157 (2019).
Shi, J., Wang, W., Sun, Y., Zhou, M. & Liu, J. Diagnostic value of cTnl, NT-pro BNP, and combined tests in acute myocardial infarction patients. Altern. Ther. Health Med. 29 (7), 412–417 (2023).
Clerico, A., Padoan, A., Zaninotto, M., Passino, C. & Plebani, M. Clinical relevance of biological variation of cardiac troponins. Clin Chem Lab Med. 59 (4) 641–652. (2020). https://doi.org/10.1515/cclm-2020-1433.
Vilar, R. et al. Fibrin(ogen) in human disease: both friend and foe. Haematologica 105 (2), 284–296 (2020).
Ang, L. & Mahmud, E. Monitoring oral antiplatelet therapy: is it justified? Ther. Adv. Cardiovasc. Dis. 2 (6), 485–496 (2008).
Makkar, K., Sharma, Y. P., Batta, A., Hatwal, J. & Panda, P. K. Role of fibrinogen, albumin and fibrinogen to albumin ratio in determining angiographic severity and outcomes in acute coronary syndrome. World J. Cardiol. 15 (1), 13–22. https://doi.org/10.4330/wjc.v15.i1.13 (2023).
Wang, X. et al. Predictive impact of fibrinogen-to-albumin ratio (FAR) for left ventricular dysfunction in acute coronary syndrome: a cross-sectional study. Eur. J. Med. Res. 28 (1), 68. https://doi.org/10.1186/s40001-023-01029-2 (2023).
Matsudo, M. et al. Association of hemostasis and inflammation biomarkers with outcomes in acute coronary syndromes. Blood Coagul Fibrinolysis. 34 (3), 179–183 (2023).
White, A. D. et al. Community surveillance of coronary heart disease in the atherosclerosis risk in communities (ARIC) study: methods and initial two years’ experience. J. Clin. Epidemiol. 49 (2), 223–233 (1996).
The Atherosclerosis Risk in Communities (ARIC). Study: design and objectives. The ARIC investigators. Am. J. Epidemiol. 129 (4), 687–702 (1989).
Forouhi, N. G. & Sattar, N. CVD risk factors and ethnicity–a homogeneous relationship? Atheroscler suppl, 7(1) 11–19. (2006).
Gazzola, K., Reeskamp, L. & van den Born, B. J. Ethnicity, lipids and cardiovascular disease. Curr. Opin. Lipidol. 28 (3), 225–230 (2017).
Cook, D. G. et al. Ethnic differences in fibrinogen levels: the role of environmental factors and the β-Fibrinogen gene. Am. J. Epidemiol. 153 (8), 799–806 (2001).
Kain, K. et al. Increased fibrinogen levels among South Asians versus Whites in the united Kingdom are not explained by common polymorphisms. Am. J. Epidemiol. 156 (2), 174–179 (2002).
Kaptoge, S. et al. Associations of plasma fibrinogen levels with established cardiovascular disease risk factors, inflammatory markers, and other characteristics: individual participant meta-analysis of 154,211 adults in 31 prospective studies: the fibrinogen studies collaboration. Am. J. Epidemiol. 166 (8), 867–879 (2007).
Zheng, Y. et al. Comparative study of clinical characteristics between Chinese Han and German Caucasian patients with coronary heart disease. Clin. Res. Cardiol. 99 (1), 45–50 (2010).
He, Y. M. et al. Serum albumin concentrations, effect modifiers and first incident acute myocardial infarction: A cross-sectional study of 1552 cases and 6680 controls. Clin. Chim. Acta. 454, 49–56 (2016).
Cai, D. P. et al. Lipoprotein (a) is a risk factor for coronary artery disease in Chinese Han ethnic population modified by some traditional risk factors: A cross-sectional study of 3462 cases and 6125 controls. Clin. Chim. Acta. 451(Pt B), 278–286 (2015).
He, Y. et al. Association between serum uric acid and hypertension in a large cross-section study in a Chinese population. J. Cardiovasc. Dev. Dis., 9(10). (2022).
Thygesen, K. & Fourth universal definition of myocardial infarction. J. Am. College Cardiol. 72 (18) 2231–2264. (2018).
De Luca, G. et al. High fibrinogen level is an independent predictor of presence and extent of coronary artery disease among Italian population. J. Thromb. Thrombolysis. 31 (4), 458–463 (2011).
Khandelwal, V. et al. Exploring the association of fibrinogen and CRP with the clinical spectrum of CAD and periprocedural outcomes in patients undergoing percutaneous coronary interventions. Ann. Card Anaesth. 25 (1), 34–40 (2022).
Fu, A. & Nair, K. S. Age effect on fibrinogen and albumin synthesis in humans. Am. J. Physiol. 275 (6), E1023–E1030 (1998).
Kumar, A. et al. Cardiovascular risk factors in elderly normolipidemic acute myocardial infarct patients–a case controlled study from India. Southeast. Asian J. Trop. Med. Public. Health. 40 (3), 581–592 (2009).
Danesh, J. et al. Plasma fibrinogen level and the risk of major cardiovascular diseases and nonvascular mortality: an individual participant meta-analysis. Jama 294 (14), 1799–1809 (2005).
Ragino Iu, I. et al. Oxidized fibrinogen and its relationship with hemostasis disturbances and endothelial dysfunction during coronary heart disease and myocardial infarction. Kardiologiia 49 (9), 4–8 (2009).
Doll, R. et al. Mortality in relation to smoking: 50 years’ observations on male British doctors. Bmj 328 (7455), 1519 (2004).
Lu, Y. et al. Mediators of the effect of body mass index on coronary heart disease: decomposing direct and indirect effects. Epidemiology 26 (2), 153–162 (2015).
Lee, A. J. et al. Fibrinogen in relation to personal history of prevalent hypertension, diabetes, stroke, intermittent claudication, coronary heart disease, and family history: the Scottish heart health study. Br. Heart J. 69 (4), 338–342 (1993).
Montasser, M. E. et al. Genetic and functional evidence links a missense variant in B4GALT1 to lower LDL and fibrinogen. Science 374 (6572), 1221–1227 (2021).
Yano, K. et al. Plasma fibrinogen as a predictor of total and cause-specific mortality in elderly Japanese-American men. Arteriosclerosis, thrombosis, and vascular biology. J. Am. Heart Association. 21, 1065–1070 (2001).
Lowe, G. D. & Rumley, A. Fibrinogen and its degradation products as thrombotic risk factors. Ann. N Y Acad. Sci. 936, 560–565 (2001).
Reinhart, W. H. Fibrinogen–marker or mediator of vascular disease? Vasc Med. 8 (3), 211–216 (2003).
Tousoulis, D. et al. Pathophysiology of atherosclerosis: the role of inflammation. Curr. Pharm. Des. 17 (37), 4089–4110 (2011).
Stec, J. J. et al. Association of fibrinogen with cardiovascular risk factors and cardiovascular disease in the Framingham offspring population. Circulation 102 (14), 1634–1638 (2000).
Funding
This work was supported in part by the Jiangsu Commission of Health (M2021019 to He YM) and the Sci-Tech Development Program of Suzhou City (SKY2021005 to He YM). This funding had no impact on the conclusions of the study.
Author information
Authors and Affiliations
Contributions
Jian-Ping Xu and Yang He contributed to the conception of the work and wrote the draft. Yong-Ming He designed the study. Ting-Bo Jiang, Dong-Ping Cai, and Heng Wang analyzed the data and created tables. Li-Hong Zhang, Xu Li, and Xiao-Dong Qian participated in clinical data collection. All authors were involved in drafting, revising, and approving the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of The First Affiliated Hospital of Soochow University (No. 361). All methods were carried out in accordance with Declaration of Helsinki.
Consent for publication
According to the review by the ethics committee of The First Affiliated Hospital of Soochow University, the proposed study project is a retrospective/non-interventional clinical study, with a scientifically sound research design that is in line with ethical principles. The requirement for written informed consent has been waived by The First Affiliated Hospital of Soochow University Ethics Committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, JP., He, Y., Li, X. et al. Correlation of fibrinogen levels with acute myocardial infarction risk in the Chinese Han population. Sci Rep 15, 20779 (2025). https://doi.org/10.1038/s41598-025-08215-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08215-8