Abstract
The Pain Vigilance and Awareness Questionnaire (PVAQ) is widely used to assess attention to pain, but no validated Polish version has been previously available. This study aimed to translate the PVAQ into Polish and evaluate its psychometric properties. Two studies were conducted: Study 1 included 418 chronic pain patients recruited online who completed the scale alongside measures of depression, anxiety, pain catastrophizing, pain anxiety, pain intensity, functional limitations, and psychological flexibility. A follow-up was completed by 79% after 30 days. Study 2 involved 148 hospital-recruited chronic pain patients who completed the adapted scale and measures of pain intensity and functional limitations. None of the previously proposed models describing the factor structure of the PVAQ scale adequately fit the data. However, factor analyses indicated that a 12-item version with two correlated factors–Passive Awareness and Active Vigilance–provided acceptable model fit. The Polish PVAQ showed good internal consistency, moderate test–retest reliability, and expected correlations with related constructs. Interestingly, Passive Awareness (but not Active Vigilance) was positively associated with components of psychological flexibility. The Polish 12-item PVAQ is reliable and valid instrument for assessing pain-related attention in chronic pain samples, aiding healthcare professionals in identifying highly vigilant individuals to tailor interventions accordingly.
Similar content being viewed by others
Introduction
Pain, as defined by the International Association for the Study of Pain, is “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage”1. This definition emphasizes not only the physical aspects of pain but also the critical role of emotion and closely related processes. In humans this implicates cognitive and attentional responses to the bodily sensations that contribute to the pain experience.
Pain automatically captures attention when it occurs. When attention is focused on the experience of pain, it may serve as a moderator of pain perception, often amplifying pain intensity and emotional impact2,3,4,5. This, in turn, can lead to greater emotional distress, disability, and increased use of healthcare services6,7.
Attention directed toward pain can be conceptualized as pain vigilance or pain awareness. Pain vigilance refers to heightened, often maladaptive focus on pain, characterized by excessive monitoring and hyperattention, which can amplify distress and impair adaptive coping. The second component, pain awareness involves recognizing and observing pain as it arises and subsides8,9. Its implications can be considered twofold. On the one hand, pain awareness has been shown to be positively associated with pain intensity, catastrophizing, and fear of pain9,10,11,12. This suggests that it may reflect heightened attention to pain, which contributes to both pain and distress. On the other hand, observing pain in non-judgmental way, as part of one’s experience, can serve as a foundation for developing pain acceptance: the ability to experience pain without attempting to control, reduce, or avoid it. Pain acceptance is an essential component of psychological flexibility8,9,13,14, which has been shown to protect individuals from pain-related interference15.
The Pain Vigilance and Awareness Questionnaire (PVAQ), developed by Lance McCracken8, is a self-report tool designed to assess the two distinct yet related dimensions of attention to pain highlighted above: heightened awareness of pain and increased pain vigilance. The psychometric properties of PVAQ have been assessed in several language versions, including English8,9,16, Dutch10,17, Chinese12, Spanish18,19, Swedish20, German21, Italian11, and Brazilian-Portuguese22. Validations have been performed in both non-clinical16,17,21,22 and clinical groups, such as those with chronic pain of various origins8,9,11,18,19, including chronic low back pain8,11, and fibromyalgia10,20, highlighting the scale’s utility across a spectrum of pain experiences.
Differences in the factor structure of PVAQ have emerged across language versions. Originally one-factor was hypothesized8, but subsequent studies have suggested that a more complex model is needed. Most language adaptations have supported a two-factor structure of PVAQ, though the specific composition of the factors varied across studies. In five studies, the obtained factors were labelled as “active vigilance” and “passive awareness”11,12,18,19,20. Four other studies identified the factors as “attention to pain” and “attention to changes in pain”10,17,21,22. Broadly, the first factor (active vigilance/attention to pain) corresponded to pain vigilance, while the second (passive awareness/attention to changes in pain) aligned more closely with pain awareness. Additionally, one study proposed a three-factor model comprising “awareness of change”, “intrusion” and “monitoring”16. These variations reflect differences in the assignment of specific items to each subscale across studies.
Adaptations of PVAQ have also resulted in modifications to its original length. While some studies retained the full 16-item version8,16,17,21, others proposed shortened versions, including 14-item10, 13-item9,11,12,22, 9-item18,19 and 8-item20 versions. Taken together, these findings suggest that PVAQ may be sensitive to cultural and linguistic differences.
Previous studies have established in general positive associations between PVAQ – either as an overall score or through specific subscales – and various pain-related variables, including pain intensity, depression, anxiety, fear of pain, disability, pain catastrophizing, pain acceptance, and kinesiophobia10,11,12,16,17,18,19,20,21,23.The relationship between PVAQ and depression has been assessed using the Beck Depression Inventory8 and the Hospital Anxiety and Depression Scale (HADS)11,12,18,19,21. Observed correlations were low and positive, ranging from r = 0.2019 to r = 0.2811. For anxiety, as measured by HADS, one study found no significant relationship21, while others reported low to moderate positive correlations, ranging from r = 0.22 to r = 0.5311,12.
Pain catastrophizing has been evaluated using the Pain Catastrophizing Scale (PCS), with studies reporting strong positive correlations with PVAQ (r = 0.68)10,17.
Similarly, pain-related anxiety, as measured by the Pain Anxiety Symptoms Scale (PASS), has shown strong positive correlations with PVAQ, ranging from r = 0.50 to r = 0.618,10,19,21. The PVAQ attention to pain subscale has demonstrated even higher correlations, ranging from r = 0.66 to r = 0.7010,21.
Disability in pain populations has been shown to correlate positively with PVAQ scores, with correlations ranging from weak to strong (r = 0.13 to r = 0.88)11,12,20. Similarly, pain intensity has demonstrated a positive relationship with PVAQ scores, with correlations ranging from r = 0.17 to r = 0.88, depending on the study12,16,21.
The PVAQ has demonstrated acceptable to good internal consistency across studies, with Cronbach’s alphas for total scores ranging from 0.7512 to 0.9216. For the subscales, Cronbach’s alphas varied from 0.7221 to 0.9218. The test–retest reliability of the Italian version of PVAQ has been evaluated over a 10-day interval, in which its stability was confirmed. Intraclass Correlation Coefficient (ICC) ranged from 0.88 to 0.92 (depending on the score), indicating high reliability11.
Based on these findings, it is anticipated that the Polish version of PVAQ will exhibit good internal consistency and reliability. Significant correlations are hypothesized between PVAQ scores and several pain-related constructs and measures of psychological well-being, including weak positive correlations with depression, weak to moderate positive correlation with anxiety, strong positive correlations with pain catastrophizing, strong positive correlations with pain anxiety, and positive correlation with pain intensity. Additionally, given the consistently positive correlations between PVAQ scores and pain-related disability reported in previous studies11,12,20, it is anticipated that PVAQ scores will vary based on self-reported functional limitation due to pain, such as being on sick leave, ceasing work or academic activities due to pain, and withdrawing from important life activities as a result of pain. Finally, building on theoretical considerations14,24,25,26, we hypothesize that pain awareness but not pain vigilance will show positive correlations with facets of psychological flexibility, such as self-as-context (ability to take a perspective from which one observes thoughts and emotions without being entirely defined by them14) and committed action (engagement in valued activities despite pain14).
Given that previous validation studies of the PVAQ have yielded various factor structures, we did not hypothesize a single specific factor structure a priori. Instead, we planned to test several previously reported structures using Confirmatory Factor Analysis to evaluate their fit in the Polish sample. If none of the previously reported models demonstrated acceptable fit, we intended to conduct an exploratory factor analysis to further examine the underlying structure.
Study 1
The aim of Study 1, conducted with a relatively large sample of individuals experiencing chronic pain, was to develop a Polish version of PVAQ and to evaluate the structure and psychometric properties of the translation.
Results
Preliminary analyses
All PVAQ items exhibited skewness and kurtosis values from – 1 to 1, indicating approximately normal univariate distributions. However, Mardia’s test revealed a significant deviation from multivariate normality (χ2 = 2415.49, df = 816, p < 0.001, multivariate kurtosis: z = 33.36, p < 0.001). Consequently, an appropriate estimator was selected to account for these deviations. Descriptive statistics for each item are presented in the supplementary materials (Supplementary Table 1).
Structural validity
The tested models that were obtained in previous studies (see: Supplementary Table 2 for details) did not demonstrate an acceptable fit. Modification Indices (MIs) indicated shared covariance among several pairs of item errors across the models. Specifically, Model 1, which exhibited the poorest fit, identified 25 error pairs with MI values ≥ 15. In contrast, Model 8, which showed the best relative fit, had 5 error pairs with MI values ≥ 15. Importantly, many of these correlations involved items from different scales. Even in the best-fitting model (Model 8), incorporating at least five additional covariances was necessary to achieve a reasonable fit.
These findings suggest that the factor structure of the Polish version of PVAQ may differ from previously established models. Consequently, we randomly divided the sample in half and conducted an exploratory factor analysis (EFA) on the first half (N = 209). The Kaiser–Meyer–Olkin statistic was 0.85, indicating good suitability of the data for factor analysis. Principal axis factoring with Promax rotation, performed on polychronic correlations, preceded by parallel analysis and visual inspection of the scree plot (Fig. 1), revealed a three-factor solution explaining 61% of variance. Items 1 and 10 exhibited a low factor loading (< 0.50) and cross-loaded equally on two factors, leading to their removal (resulting in 14 items total). The EFA that followed showed a three-factor solution explaining 63% variance (Supplementary Table 3).
Next, we examined item-rest correlations (IRC) and item reliability statistics to eliminate redundant items and items that were not well-aligned with the broader construct that the overall scale was intended to measure. Except for two items (item 8: IRC = 0.11, item 16: IRC = -0.04), all IRCs fell in the range 0.30–0.69 (see: Supplementary Table 4). Therefore, we excluded items 8 and 16 resulting in 12 items. After running EFA once more, a two-factor solution was revealed that explained 63% variance.
We subsequently performed Confirmatory Factor Analysis (CFA) on the second half of the sample (N = 209) to test the obtained structure of the 12-item version of PVAQ (PVAQ-12). Although Comparative Fit Index (CFI), Normed Fit Index (NFI), chi square/df ratio (χ2/df ) fell in a reasonable range, the Root Mean Square Error of Approximation (RMSEA) did not indicate acceptable fit (CFI = 0.98, NFI = 0.97, RMSEA = 0.097, 90% CI 0.08–0.11, χ2/df = 3.05). MIs revealed correlated residuals between items 2 and 3, as well as between 13 and 14. These error pairs consistently emerged as the top suggested modifications in six (item 2 and 3) and four (13 and 14) of the eight tested models from the previous studies. These items are positioned next to each other within the questionnaire and assess similar concepts (e.g., item 2, “I am aware of quick changes in pain”, and item 3, “I am quick to notice when pain goes up or down”), thus justifying adding these covariates to the model. The final model exhibited acceptable to good descriptive fit, depending on the index (CFI = 0.99, NFI = 0.98, RMSEA = 0.075, 90% CI 0.06–0.09, χ2/df = 2.22) (see Fig. 2 and Supplementary Table 5). The full list of the 12 items comprising the Polish PVAQ is included in the Supplementary Materials.
Reliability and items properties
In the first measurement, 0% participants recorded the lowest or highest possible scores on the total PVAQ. For the Passive Awareness subscale, 0% obtained the minimum score, while 5.7% reached the maximum. The Active Vigilance subscale had 0.2% at the minimum and 3.6% at the maximum. In the second measurement, 0.2% scored at the minimum and 0% at the maximum on the total scale. For Passive Awareness, 0.5% scored at the minimum and 3.6% at the maximum, while for Active Vigilance, 1% and 2.4% reached the minimum and maximum scores, respectively. These results indicate no floor or ceiling effects.
McDonald’s omega values (calculated for the total sample: N = 418) indicated good to excellent reliability of the Polish PVAQ-12 subscales: Passive Awareness ω = 0.88, 95% CI 0.86–0.90, Active Vigilance ω = 0.88, 95% CI 0.86–0.90 and for the total scale ω = 0.90, 95% CI 0.88–0.91. The item-rest correlations were all > 0.50 (details in Supplementary Table 6).
The Intraclass Correlation (ICC) analysis indicated that the test–retest reliability of the total PVAQ-12 score was 0.63, 95% CI 0.56–0.70 (p < 0.001). The subscales demonstrated the following ICC values: 0.63, 95% CI 0.54–0.70 for the Passive Awareness subscale and 0.63, 95% CI 0.56–0.69 for the Active Vigilance subscale. These results suggest that the Polish PVAQ-12 demonstrates moderate stability over time (30-day interval) across all subscales.
The Minimal Detectable Change (MDC95%) for the PVAQ-12 total score was 16.30, signifying that a change of at least 17 points in the questionnaire is necessary to denote an actual change rather than simply a measurement error. The MDC95% values for the subscales were: 9.62 for Passive Awareness and 9.07 for Active Vigilance.
Construct validity
Correlation analysis indicated a strong positive relationship between the PVAQ-12 total score and general pain anxiety (r = 0.55, p < 0.001). Additionally, there was a moderate positive correlation with pain catastrophizing (r = 0.39, p < 0.001). Positive but weak correlations were observed between PVAQ-12 total and depression, anxiety, pain intensity and self-as-context.
The Passive Awareness subscale demonstrated weak positive correlations with pain intensity (both at the time of the study, r = 0.15, p = 0.002, and during the previous week, r = 0.29, p < 0.001), pain catastrophizing (r = 0.18, p < 0.001) and committed action (r = 0.20, p < 0.001). Additionally, a moderate positive correlation was observed with pain anxiety (r = 0.35, p < 0.001) as well as self-as-context (r = 0.33, p < 0.001).
The Active Vigilance subscale of PVAQ-12 showed weak positive correlations with pain intensity (at the time of the study, r = 0.23, p < 0.001; in the previous week, r = 0.20, p < 0.001), and depression (r = 0.20, p < 0.001), and a very weak negative correlation with committed action (r = – 0.13, p = 0.007). Furthermore, it exhibited a moderate positive correlation with anxiety (r = 0.30, p < 0.001). Strong positive correlations with pain catastrophizing (r = 0.51, p < 0.001) and general pain anxiety (r = 0.60, p < 0.001) were observed (see Supplementary Table 7).
There were significant differences between participants who had to give up work or school due to pain and those who did not, with the former group reporting higher PVAQ-12 scores (Total: t(416) = 3.63, p < 0.001, d = 0.36, Passive Awareness: t(416) = 2.96, p = 0.004, d = 0.29, Active Vigilance: t(416) = 3.40, p < 0.001, d = 0.34). Individuals who reported giving up activities important to them due to chronic pain had higher PVAQ-12 total scores (t(416) = 3.54, p = 0.002, d = 0.42) and scored higher on the Passive Awareness subscale (t(416) = 3.50, p = 0.001, d = 0.42). No significant differences were found on the Active Vigilance subscale (t(416) = 2.66, p = 0.009, d = 0.32). Participants who reported being on sick leave did not differ in PVAQ-12 scores from those who were not (Total: t(260) = 0.94, p = 0.357, d = 0.15, Passive Awareness: t(260) = 0.29, p = 0.763, d = 0.05, Active Vigilance: t(260) = 2.01, p = 0.040, d = 0.32).
Study 2
The aim of Study 2 was to verify the structure of the Polish Pain Awareness and Vigilance Questionnaire identified in Study 1, this time using a clinical sample of patients with chronic pain recruited from a hospital.
Results
Preliminary analyses
Mardia’s test indicated a significant deviation from multivariate normality, with a skewness chi-square statistic of 916.87 (df = 364, p < 0.001) and a multivariate kurtosis z-score of 11.06 (p < 0.001). There was no evidence of ceiling or floor effects: 0% of participants obtained the minimum, and 1.50% obtained the maximum total score on PVAQ-12. For Passive Awareness, 0.80% of participants obtained the minimum score and 4.50% obtained the maximum score; for Active Vigilance, 0.70% obtained the minimum score and 5.90% obtained the maximum score. Descriptive statistics for the items and subscales are in the Supplementary Table 8.
Structural validity
CFA was performed to evaluate the two-factor structure of PVAQ-12 obtained in Study 1. Fit indices showed the good fit of this model, indicating that it describes the structure of the Polish version of the scale very well: CFI = 0.99, NFI = 0.98, RMSEA = 0.063, 90% CI 0.03–0.09, χ2/df = 1.53. The items showed high and significant factor loadings, ranging from 0.55 to 0.89 (Fig. 3).
Reliability and item properties
The Polish version of PVAQ-12 demonstrated good internal consistency: ω = 0.84, 95% CI 0.76–0.90 for the Passive Awareness subscale, ω = 0.84, 95% CI 0.79–0.88 for the Active Vigilance subscale, and ω = 0.88, 95% CI 0.83–0.92 for the total score. All item-rest correlations were > 0.45 (Supplementary Table 9).
Construct validity
The total PVAQ-12 score showed a significant positive correlation with pain intensity, both at the time of the study (r = 0.29, p < 0.001) and during the previous week (r = 0.33, p < 0.001). Similarly, the Active Vigilance subscale demonstrated significant moderate positive correlations with pain intensity (at the time of the study: r = 0.31, p < 0.001; during the previous week: r = 0.35, p < 0.001). The Passive Awareness subscale correlated positively but weakly with average pain intensity during the previous week (r = 0.25, p = 0.005) but not with pain intensity at the time of the study (r = 0.21, p = 0.028).
Participants who had given up work and/or school due to pain did not differ in PVAQ-12 scores from those who had not (Total: t(124) = 2.02, p = 0.054, d = 0.36, Passive Awareness: t(124) = 1.27, p = 0.213, d = 0.23, Active Vigilance: t(124) = 2.29, p = 0.024, d = 0.43). Similarly, no significant difference was observed between patients who reported being on sick leave and those who did not (Total: t(118) = 0.84, p = 0.84, d = 0.06, Passive Awareness: t(118) = 0.74, p = 0.462, d = 0.22, Active Vigilance: t(118) = 0.43, p = 0.672, d = 0.13), and between those who had had to resign from activities important to them and those who had not (Total: t(128) = 2.49, p = 0.019, d = 0.63, Passive Awareness: t(128) = 2.49, p = 0.032, d = 0.63, Active Vigilance: t(128) = 1.92, p = 0.042, d = 0.49).
Discussion
The current project aimed to adapt PVAQ into Polish and evaluate its structure, item properties, reliability, and validity. The findings from the two studies provided support for the acceptable psychometric properties of the Polish translation. Analyses supported a two-factor structure of PVAQ, retaining 12 items. Additionally, the scale exhibited good internal consistency, robust factor loadings, and moderate temporal stability over a one-month interval. Construct validity was supported by significant positive correlations with the PASS total score, CSQ Catastrophizing score, DASS-21 Depression and Anxiety scores, and pain measures. Additionally, the two identified factors – Passive Awareness and Active Vigilance – exhibited some distinct correlation patterns with the scales measuring components of psychological flexibility (CAQ, SEQ-8), supporting construct differentiation. Associations with self-reported functional limitations due to pain were evident in the online sample but not in the hospital-recruited sample.
Reliability
In Study 1, the Polish PVAQ revealed excellent internal consistency, with McDonald’s omega values of 0.90 for the full scale and 0.88 for the subscales. Similarly, in Study 2 internal consistency was excellent (0.88) for the total score and good (0.84) for the two subscales. These findings align with previous research11,12,18,19,20. Additionally, high item-rest correlations (> 0.50 in Study 1 and > 0.45 in Study 2) indicated strong item homogeneity.
The stability of the Polish PVAQ over time was examined using the test–retest method, revealing moderate stability across all subscales (total = 0.63). This value was lower than in a previous study11, which had been expected considering the three times longer time interval applied in the current project. The MDC95% values indicate that a minimum change of 17 points in the PVAQ-12 total score is required to reflect true changes in individuals’ pain-related attention and awareness after 1 month.
Construct validity
The hypothesized associations between PVAQ and related constructs were largely confirmed. Additionally, distinct correlation patterns were observed for the subscores, thus supporting the division of the Polish PVAQ-12 into two distinct scales: Passive Awareness and Active Vigilance.
Average pain intensity scores showed weak to moderate positive correlations with the PVAQ-12 total score and its subscales, mirroring findings from several validation studies9,11,20,21. In contrast, the Chinese version of PVAQ reported a strong correlation between the Passive Awareness subscale and pain intensity (r = 0.8812). However, it is worth noting that Wong et al.12 applied a broader definition of pain intensity, calculating it as the mean of current, average, and worst pain ratings. This composite approach may provide a more accurate estimate of overall pain experience, potentially reducing measurement error and resulting in stronger associations with cognitive factors such as attention to pain. Future research should therefore clarify how different approaches to pain measurement influence the relationship between attention to pain and pain intensity across various cultural contexts.
As is consistent with our hypothesis, individuals with higher and lower levels of functional limitations due to pain, differed significantly in the PVAQ scores. In the online sample, participants who had quit work or studies due to pain scored higher on PVAQ in comparison to those who had not. Moreover, participants who indicated forgoing important activities because of pain scored higher on both the total PVAQ and the Passive Awareness subscale. However, these differences were not observed in the hospital-recruited sample, likely due to the more homogeneous nature of the clinical group, which was characterized by high levels of disability.
The total PVAQ score demonstrated only a moderate (not strong as hypothesized) positive correlation with pain catastrophizing. However, correlation patterns varied across subscales: the Active Vigilance subscale showed a strong correlation, while the Passive Awareness subscale showed only a weak one. This finding is theoretically consistent, given that pain catastrophizing – characterized by an exaggerated perception of threat, feelings of helplessness, and difficulty suppressing pain-related thoughts27 – is closely linked to vigilant attention to pain. Moreover, these constructs appear to influence each other: ongoing worry about chronic pain may sustain heightened vigilance, perpetuating the perception of threat28.
The hypothesized strong correlations between the PVAQ scores and the measure of pain anxiety were largely confirmed. The PVAQ-12 total score exhibited a strong positive correlation with pain anxiety, with even higher correlations observed for the Active Vigilance subscale. In contrast, the Passive Awareness subscale demonstrated only a moderate association. These results are consistent with previous studies9,10,18,19,21, highlighting the capacity of the Active Vigilance subscale to effectively measure heightened sensitivity to anxiety-driven pain responses. This suggests that the Active Vigilance dimension is closely related to pain anxiety, reflecting a strong conceptual and empirical link between these constructs. These findings support the utility of PVAQ in identifying hypervigilant, anxiety-driven pain patterns.
Anxiety was weakly and positively correlated with the total PVAQ-12 score and moderately with the Active Vigilance subscore. Additionally, weak positive correlations were observed between depression and both the PVAQ-12 total score and the Active Vigilance subscale. These findings are consistent with earlier research11,12,19 and show that while anxiety, depression, and pain attention are interrelated, they likely represent distinct constructs.
In the current study, the Passive Awareness and Active Vigilance subscales appeared to demonstrate distinct associations with pain-related variables. Active Vigilance showed strong links to maladaptive constructs such as pain anxiety and catastrophizing, and it correlated significantly with psychopathological symptoms like anxiety and depression. In contrast, Passive Awareness demonstrated weaker associations with pain anxiety and catastrophizing and did not significantly correlate with depression or anxiety symptoms, thus supporting the findings of some previous studies (e.g.,9).
Further differences emerged in relation to psychological flexibility. Passive Awareness was positively associated with two components of psychological flexibility – committed action and self-as-context – whereas Active Vigilance either showed no relationship or negative correlations with these constructs. These patterns align with theoretical models distinguishing between constructive awareness and maladaptive vigilance, suggesting that different forms of attentional focus on pain may play distinct roles in adaptation to chronic pain9,13,14,24.
The current findings can be better understood within the broader framework of psychological flexibility, a concept central to Acceptance and Commitment Therapy (ACT). Psychological flexibility refers to the ability to stay aware of thoughts, emotions, and bodily sensations–such as pain–while choosing behaviors aligned with one’s values and recognizing as well as adapting to situational demands24. ACT-based interventions aim to cultivate these skills and have demonstrated considerable effectiveness in improving well-being in individuals with chronic pain29,30,31,32,33,34.
Psychological flexibility is built on six core skills: present-focused awareness, acceptance, cognitive defusion, self-as-context, value-based action, and committed action14. Among these, committed action involves goal-directed behavior that is both persistent (allowing individuals to continue despite setbacks or discomfort) and flexible (enabling adjustments when necessary). Within ACT, committed action fosters engagement in valued activities despite pain, contributing to better mental health and overall functioning24. Similarly, self-as-context is a crucial aspect of psychological flexibility that refers to the ability to take a perspective from which one observes thoughts and emotions without being entirely defined by them. Improvements in self-as-context, particularly through ACT, are associated with enhanced psychological functioning, as individuals become less entangled in distressing self-evaluations and more capable of adaptive, values-driven action25,26.
From this perspective, the Active Vigilance – as measured by PVAQ appears to reflect a rigid and threat-driven monitoring of pain, potentially motivated by fear or perceived danger. Such hypervigilance may interfere with flexible functioning and engagement in values-based actions. In contrast, Passive Awareness may represent a more observational mode of attention to changes in pain. While this heightened focus can be associated with increased pain intensity and distress—especially when accompanied by efforts to control or avoid pain—it may also reflect a capacity to notice pain without immediately reacting to it. In this sense, awareness encompasses dual possibilities: one can be aware-and-resist or aware-and-allow9. Individuals who relate to their pain in a more receptive and non-reactive way may be better equipped to sustain goal-directed behavior and maintain a broader, more stable sense of self that is not wholly defined by the pain experience.
Taken together, these results suggest that Passive Awareness as measured by the PVAQ may represent a more nuanced–and potentially less maladaptive–form of pain attention than Active Vigilance in chronic pain contexts, thus highlighting the importance of using these distinct subscales for clinical assessment. Furthermore, Passive Awareness may itself encompass distinct subtypes, some of which may be more adaptive than others depending on the context- such as whether it is accompanied by acceptance–and on how pain influences emotion and behavior. This complexity may explain why Passive Awareness is positively associated with both pain-related distress and facets of psychological flexibility. The current version of the PVAQ does not address this potential distinction, which may be a valuable avenue for future research.
Structural validity
There is no consensus regarding the structure of PVAQ, as different language adaptations have resulted in varying subscales and different numbers of items9,10,16. This suggests that the scale may be influenced by cultural and language-related factors.
In the current study, CFAs were conducted to assess the fit of several previously identified PVAQ structures. As none of these models achieved acceptable fit, an EFA was performed to explore the structure of the Polish PVAQ. This analysis identified a two-factor structure with 12 items, which demonstrated acceptable to good fit and high factor loadings in subsequent CFAs performed on both online and hospital-recruited samples. The resulting structure aligns with previous adaptation studies9,11,12,18,19,20 (a comparison of the factor structures identified in this study and those proposed in previous research is presented in Supplementary Table 10).
To achieve an acceptable fit for the two-factor model in the CFA, correlations were introduced between items 2–3 and 13–14. Items 2 and 3 both refer to awareness of changes in pain intensity, while items 13 and 14 reflect a constant, background monitoring of pain sensations. In addition to their conceptual similarity, each item pair also shares highly similar wording and appears consecutively in the questionnaire, which may contribute to shared variance due to factors such as context effects–where respondents draw on information activated by one item when answering the next35. Omitting correlated residuals in such cases may lead to model misspecification35. It is also worth noting that the inclusion of residual covariances between item pairs (in some cases up to four) has been reported in previous language adaptations of the PVAQ11,22.
Four items (1, 8, 11, and 16) were excluded from the Polish version of PVAQ due to low factor loadings and weak item-rest correlations. Notably, items 8 and 16 are reverse scaled, which may lead to participant confusion and difficulties in answering these questions22. Furthermore, these two items have frequently been excluded in prior studies evaluating the psychometric properties of PVAQ9,10,11,12,18,19,20,22. Items 1 and 11 have also been removed in some language adaptations; for instance, both were excluded in the Swedish validation study20, while item 1 was additionally removed in the Spanish and Brazilian Portuguese adaptations18,22. It is worth mentioning that the translations of the full 16-item PVAQ are generally not regarded as psychometrically sound20, and shorter versions are considered more practical in clinical settings. Taken together, these findings support the decision to shorten the Polish version of the scale.
Limitations
Some limitations of the study should be acknowledged. In Study 1, self-reported chronic pain diagnoses were not confirmed through clinicians’ assessments. In contrast, Study 2 involved hospital patients undergoing chronic pain treatment, ensuring clinically verified diagnoses. Additionally, the study assessed only convergent validity, without examining divergent validity. However, this was also the case for most of the previous PVAQ adaptations11,12,18,20,21. Future research should address these limitations and further explore how PVAQ-12 scores correlate with treatment progress or improvements in patients’ functionality in order to establish their predictive value and utility in clinical settings.
Conclusions
The Polish 12-item version of PVAQ demonstrated good psychometric properties in chronic pain samples. Its two-factor structure aligns with previous research, including the English version9. A strength of this adaptation study is the rigorous translation process and the evaluation of psychometric properties in two independent samples comprising both the community sample and patients. The study provides additional evidence regarding the scale’s stability over a one-month interval, thus addressing a gap in the literature as previous assessments were usually limited to shorter intervals. Furthermore, the findings reinforce the measure’s validity by revealing positive associations between Passive Awareness (but not Active Vigilance) and components of psychological flexibility, highlighting the differentiation of the two facets of attention to pain. Overall, the results enhance our understanding of PVAQ’s applicability in both research and clinical settings.
Internationally, PVAQ is widely used8,10,11,12,16,17,18,19,20,21,22 as a valid measurement of pain vigilance and awareness. However, it has not been available for Polish-speaking populations. This translated and evaluated 12-item version of PVAQ is a valuable tool for Polish healthcare professionals and researchers that provides a resource for monitoring adaptation to chronic pain and treatment progress, especially in the context of the growing popularity of ACT. Additionally, this tool may encourage further cross-cultural research into the role of pain-related attention in chronic conditions.
Methods
Study 1
Participants
The minimum sample size required to test the hypothesized structure of PVAQ was determined a priori based on the criterion proposed by Bentler and Chou36: a minimum ratio of 5:1 cases per estimated parameter in the structural equation model. For the most complex structure identified in previous studies, which involved three latent variables and 16 items (resulting in 35 parameters to be estimated), a minimum of 175 participants reporting chronic pain was deemed necessary to perform CFA, assuming high factor loadings and multiple indicators per latent variable. Given that the project aimed to validate multiple scales (see: Measures), the final sample included 418 participants. The study recruited participants from “ARIADNA”—a large Polish research panel. Before the study, an initial survey was conducted to identify individuals with chronic pain, revealing that 22% of panelists met this criterion, with 53% having a physician’s diagnosis. To participate, individuals had to be over 18 years of age, fluent in Polish, have pain lasting over 3 months, and have a physician’s diagnosis of chronic pain. Of the 15,760 invited panelists, 2569 completed the survey, with 418 meeting all inclusion criteria. The final sample included 168 men (40.19%), 249 women (59.57%), and one non-binary individual (0.24%); age range was 19–86 years (M = 49.37, SD = 15.20). Participants completed the survey twice to evaluate test–retest reliability. A total of 330 participants completed both measurements, conducted one month apart, including 144 men (85.71%) and 186 women (74.70%) aged 19–84 (M = 51.21, SD = 14.79). The sociodemographic and pain characteristics of the participants are described in detail in Kłosowska et al.37.
Measures
Participants completed an online survey which included the following: (1) demographic information (sex, age, employment status, income, marital status, education, and residence); (2) chronic pain details (diagnosis, duration, location, intensity); (3) medical care history (current and past treatments for chronic pain, including duration, and type of treatment); and (4) functional limitations due to pain (being on sick leave, leaving work or university, or limiting important activities due to pain).
The survey included binary, multiple-choice, and open-ended questions. Average pain intensity (at the time of the study and in the previous week) was assessed using an 11-point numerical rating scale, where 0 indicated no pain and 10 represented the worst pain imaginable.
After the survey, participants also filled out the following questionnaires:
-
The Pain Vigilance and Awareness Questionnaire (PVAQ)8 is a measure of attention to pain that is applicable to a variety of pain populations. PVAQ contains 16 items rated on a 6-point Likert scale from 0 (Never) to 5 (Always). The Pain Vigilance and Awareness Questionnaire has a Cronbach’s alpha of 0.86 for the English version8.
-
The Depression Anxiety Stress Scales 21 (DASS-21)38; Polish adaptation39 of the DASS consists of 21 items designed to measure three closely related negative emotional states: (1) depression, (2) anxiety, and (3) stress. Respondents rate each item on a 4-point Likert scale, ranging from 0 ('Did not apply to me at all/never’) to 3 ('Applied to me very much, or most of the time/almost always’). Since previous validation studies have not examined the relationship between stress symptoms and PVAQ scores–limiting our ability to formulate clear hypotheses regarding this association–for the current study, only the depression and anxiety subscales were used to assess the validity of the PVAQ. The Polish adaptation of the DASS-21 demonstrates excellent internal consistency with a Cronbach’s alpha of 0.93 for the total score 39. In the current sample McDonald’s omega for the total score: 0.96, for the depression subscale: 0.92, for the anxiety subscale: 0.90.
-
The Catastrophizing Scale from the Coping Strategies Questionnaire (CSQ)40; Polish adaptation41 consists of six items designed to assess catastrophizing as a cognitive strategy for managing pain. Each item is scored from 0 (Never) to 6 (Always). The Catastrophizing Scale has Cronbach’s alpha of 0.80 for the total score in the Polish adaptation41. In the current sample McDonald’s omega for this subscale was 0.88.
-
The Pain Anxiety Symptoms Scale 20 (PASS-20)42; is a 20-item questionnaire measuring pain-related anxiety. Polish adaptation37 of the PASS-20 consists of four subscales: physiological responses, cognitive anxiety, fearful appraisal of pain, escape and avoidance behaviors. Total score reflecting general pain anxiety can also be calculated. Each item is scored on a scale from 0 (Never) to 5 (Always). Cronbach’s alpha for the total score in the Polish adaptation, based on the current sample, was 0.96 (McDonald’s omega also = 0.96).
-
CAQ-8 The Committed Action Questionnaire (CAQ-8)43; Polish adaptation44 is a validated shorter version of the 18-item Committed Action Questionnaire (CAQ). This 8-item self-report instrument is intended to measure committed action – a facet of psychological flexibility. Each item assesses goal-directed behavior and flexibility in the face of difficulties. Respondents are asked to rate the extent to which each item applies to them on a Likert scale from 0 (Never True) to 6 (Always True). CAQ-8 has a Cronbach’s alpha of 0.84 for the total score in the Polish adaptation44. In the current study McDonald’s omega was 0.74.
-
Self-Experiences Questionnaire (SEQ)25; Polish adaptation44 is a 15-item questionnaire for measuring “self-as-context” in two aspects: self as a distinction (the ability to differentiate oneself from thoughts and feelings) and self as an observer (a sense of self as observer of one’s experiences). Each item is scored on a scale from 0 (Never true) to 6 (Always true). Cronbach’s alpha for the Polish adaptation is 0.91 for the self as a distinction subscale, and 0.89 for the self as an observer subscale44. In the current study McDonald’s omega was 0.89 for the self as a distinction subscale and 0.92 for the self as an observer subscale.
As part of the larger project, several additional tools were employed, though they are not detailed in this section. These include the Chronic Pain Acceptance Questionnaire–Revised (CPAQ-R)13, the Chronic Pain Values Inventory (CPVI)45, the Pain Sensitivity Questionnaire (PSQ)46; Polish version:47, and the State-Trait Anxiety Inventory (STAI)48; Polish adaptation:49.
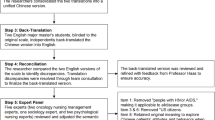
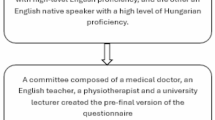
Procedure
The Polish translation of the questionnaire followed the ISPOR Task Force for Translation and Cultural Adaptation guidelines50. Approval was obtained from Professor McCracken, who also offered guidance on the translation and study design. A forward–backward translation approach was used: two professional translators created independent Polish versions, which were then merged into a single consensus translation. An independent translator subsequently produced a back-translation into English, reviewed by the project principal investigator and a native English speaker. A harmonization meeting compared all versions against each other and the original source. Ten Polish-speaking individuals participated in cognitive testing, and the translation was finalized based on their feedback. To ensure broader applicability, both pain-free individuals and participants suffering from chronic pain (50% each) were included in the debriefing phase. This approach is consistent with previous research demonstrating that the PVAQ is valid for use in both pain-free and clinical populations21, and it acknowledges the potential for the Polish version to be applied in a wider range of populations in future studies.
Data collection occurred via an online survey platform. Participants first viewed information about the study’s aims and were informed that participation was voluntary and anonymous. Informed consent was obtained by having them select the appropriate option. They then completed a 45-min set of questionnaires (PVAQ, CPAQ-R, PASS-20, CPVI, CSQ, PSQ, STAI-T, DASS-21, CAQ-8, and SEQ), plus a sociodemographic and illness history form. After one month, participants were invited to a shorter 20-min follow-up survey consisting of PVAQ, CPAQ-R, CPVI, and PASS-20. To ensure data quality, two instructional manipulation checks were embedded in the questionnaire51,52. Each question asked participants to select specific numbers on a 4-point scale. Completion times were also monitored, and participants with times outside 2 standard deviations from the mean were excluded (commonly used approach for identifying response time outliers in online surveys53). Compensation for participation was provided through “ARIADNA” panel in the form of reward points. The study protocol for the project was preregistered (https://osf.io/aewrc) and received approval from the Local Ethics Committee (KE/20_2023). The research was conducted in compliance with the ethical standards outlined in the 1964 Declaration of Helsinki and its subsequent amendments. All participants have given written informed consent in electronic format. Detailed information on the study procedure is available in a separate publication37.
Statistical analyses
In the initial phase, we examined descriptive statistics of items and checked the suitability of data for factor analysis. Next, we performed CFA using JASP Version 0.19 to validate the different factor structures identified in previous studies. To account for the ordinal nature and non-normal distribution of the data, we employed the diagonally weighted least squares (DWLS) estimator with robust standard errors54,55,56. The overall fit of the model was assessed using (a) Comparative Fit Index (CFI), (b) Normative Fit Index (NFI), (c) Root Mean Square Error of Approximation (RMSEA) with 90% confidence interval, and (d) chi-square to degrees of freedom ratio (χ2/df). A model was considered a good fit if the χ2/df ratio was ≤ 2, NFI and CFI were ≥ 0.95, and RMSEA was close to 0.06. A model was considered an acceptable fit if the χ2/df ratio was ≤ 5, NFI ≥ 0.90, CFI ≥ 0.90, RMSEA < 0.0854,57,58. Additionally, modification indices (MI) were reviewed to identify potentially overlapping items that could be compromising model fit59.
Then, we calculated McDonald’s omega (ω) values (< 0.60: poor; 0.60–0.69: marginal; 0.70–0.79: acceptable; > 0.80: good) and item-rest correlations to assess the internal consistency of the scales. Moreover, we evaluated the potential presence of floor and ceiling effects at both the subscales and total score levels. These effects were deemed to exist if more than 15% of participants achieved the minimum or maximum possible score60. To evaluate test–retest reliability, the intraclass correlation (ICC) was employed using a two-way random effects model to measure absolute agreement (single rater) in a group of 330 participants. It was interpreted as follows: 0.50–0.75, moderate reliability; 0.75–0.90, good reliability; > 0.90, excellent reliability. The minimal detectable change (MDC) was determined using the formula61: 1.96 × SEM × √2, with SEM representing the standard error of measurement. SEM was computed as baseline SD × √1-ICC (SD—standard deviation from the initial measurement).
Correlation analyses were conducted to assess the construct validity of the scale by examining its associations with the DASS-21 depression and anxiety subscales, PASS-20, CSQ Catastrophizing, CAQ-8, SEQ, and pain intensity (both current and over the previous week). The strength of correlation coefficients was interpreted using Cohen’s62 guidelines. Bonferroni correction was applied to account for multiple comparisons. For the associations between PVAQ and DASS-21 subscales, PASS-20 total, CSQ, CAQ-8 and SEQ scores, the α-level was adjusted by dividing it by 3 (reflecting the PVAQ total score and two PVAQ subscales), resulting in a significance threshold of α < 0.017. For the associations between PVAQ and pain intensity, the significance threshold was adjusted by dividing the α-level by 6 (considering two measures of pain intensity and three PVAQ scores), resulting in a significance threshold of α < 0.00863,64.
To assess group-known validity, a series of independent sample t-tests with bootstrapping (5,000 resamples) was conducted. Given that the hypothesis regarding differences in PVAQ scores between disabled and non-disabled individuals involved nine comparisons (three indicators of functional limitations due to pain: sick leave, resignation from work/studies, and resignation from important activities due to pain, and three PVAQ scores), a Bonferroni correction was applied, setting the significance threshold at α < 0.006 for these comparisons.
Study 2
Participants
Since Study 2 began before the final structure of the Polish PVAQ was established, the initial sample size calculation was conducted using the A-Priori Sample Size Calculator for Structural Equation Modelling65, assuming the most complex structure of the scale established in the previous studies, including three latent variables and 16 items. This analysis indicated that a minimum sample size of N = 119 was required for adequate model estimation, assuming a medium effect size (0.30). The final collected sample comprised 148 participants, including 33 men (22.30%), 114 women (77.03%), and one individual with unspecified gender (0.68%), with ages ranging from 18 to 85 years (M = 56.56, SD = 16.33).
Participants were recruited from the Pain Research and Treatment Unit of the University Hospital in Krakow. The eligibility criteria were identical to Study 1. All participants provided written informed consent to take part in the study and did not receive any financial compensation for their involvement. The research was conducted in compliance with the ethical standards outlined in the 1964 Declaration of Helsinki. The study protocol was approved by the Local Ethics Committee (KE/20_2023) Detailed participant characteristics are described elsewhere37.
Measures and procedure
Similarly to Study 1, participants were asked to complete a preliminary survey and a set of questionnaires: PVAQ (full 16-item version), CPAQ, PASS-20 and CPVI.
The data were collected from September to December 2023. Patients were recruited by researchers during their visits to the pain treatment facility, either completing the paper-based survey on-site or accessing the online version via the provided Quick Response (QR) Code. In total, 131 paper surveys and 17 online responses were obtained (see:37 for details).
Statistical analyses
In the initial step, multivariate normality as well as floor and ceilings effects were assessed. Then, a CFA (using the DWLS estimator) was performed to evaluate the two-factor structure of the Polish PVAQ-12 obtained in Study 1. CFI, NFI, RMSEA, χ2/df were utilized to examine model fit. McDonald’s Omega was calculated as a measure of internal consistency.
Correlation analysis was conducted to examine the relationship between PVAQ-12 and pain intensity. Consistent with Study 1, the significance threshold was adjusted by dividing the α-level by 6. Independent t-tests (with Bootstrap, N = 5000) were performed to explore differences in the total PVAQ-12 score between individuals who were on sick leave due to pain and those who were not, between those who reported having left their job or university due to pain and those who had not, and between those who reported having to give up or limit activities important to them and those who had not (known-group validity). Since the hypothesis regarding differences in PVAQ-12 scores between disabled and non-disabled individuals was tested across nine comparisons (three indicators of functional limitations due to pain and three PVAQ-12 scores), Bonferroni correction was applied, setting a significance threshold of α < 0.006. Cases with missing data were deleted listwise.
Data availability
The datasets analyzed in the current study are available in the RODBUK repository (https://doi.org/https://doi.org/10.57903/UJ/VOPA3J).
References
Raja, S. N. et al. The revised International Association for the study of pain definition of pain: concepts, challenges, and compromises. Pain 161, 1976 (2020).
Billens, A. et al. The influence of expectations and attention on conditioned pain modulation: a systematic review and meta-analysis. Clin. Psychol. Rev. 114, 102517 (2024).
Melzack, R. & Wall, D. P. The Challenge of Pain. (1982).
Todd, J. et al. Towards a new model of attentional biases in the development, maintenance, and management of pain. Pain 156, 1589 (2015).
Van Ryckeghem, D. M. L., Noel, M., Sharpe, L., Pincus, T. & Van Damme, S. Cognitive biases in pain: an integrated functional–contextual framework. Pain 160, 1489 (2019).
Fordyce, W. E. Behavioral Methods for Chronic Pain and Illness (Mosby, 1976).
Fordyce, W. E. Pain and suffering: a reappraisal. Am. Psychol. 43, 276–283 (1988).
McCracken, L. M. ‘Attention’ to pain in persons with chronic pain: a behavioral approach. Behav. Ther. 28, 271–284 (1997).
McCracken, L. M. A contextual analysis of attention to chronic pain: what the patient does with their pain might be more important than their awareness or vigilance alone. J. Pain 8, 230–236 (2007).
Roelofs, J., Peters, M. L., McCracken, L. & Vlaeyen, J. W. S. The Pain Vigilance and Awareness Questionnaire (PVAQ): further psychometric evaluation in fibromyalgia and other chronic pain syndromes. Pain 101, 299–306 (2003).
Monticone, M. et al. Development of the Italian Version of the Pain Vigilance and Awareness Questionnaire in subjects with chronic low back pain: cross-cultural adaptation, confirmatory factor analysis, reliability and validity. Int. J. Behav. Med. 23, 214–223 (2016).
Wong, W. S., McCracken, L. M. & Fielding, R. Factorial validity and reliability of the Chinese Version of the Pain Vigilance and Awareness Questionnaire (ChPVAQ) in a sample of Chinese patients with chronic pain. Pain Med. 12, 1018–1025 (2011).
McCracken, L. M., Vowles, K. E. & Eccleston, C. Acceptance of chronic pain: component analysis and a revised assessment method. Pain 107, 159–166 (2004).
McCracken, L. M. Psychological flexibility, chronic pain, and health. Annu. Rev. Psychol. 75, 601–624 (2024).
Gentili, C. et al. Psychological flexibility as a resilience factor in individuals with chronic pain. Front. Psychol. 10, 2016 (2019).
McWilliams, L. A. & Asmundson, G. J. G. Assessing individual differences in attention to pain: psychometric properties of the Pain Vigilance and Awareness Questionnaire modified for a non-clinical pain sample. Personal. Individ. Differ. 31, 239–246 (2001).
Roelofs, J., Peters, M. L., Muris, P. & Vlaeyen, J. W. S. Dutch version of the Pain Vigilance and Awareness Questionnaire: validity and reliability in a pain-free population. Behav. Res. Ther. 40, 1081–1090 (2002).
Esteve, R., Ramírez-Maestre, C. & López-Martínez, A. E. Empirical evidence of the validity of the Spanish version of the Pain Vigilance Awareness Questionnaire. Int. J. Behav. Med. 20, 59–68 (2013).
Martínez, M. P. et al. Spanish version of the Pain Vigilance and Awareness Questionnaire: psychometric properties in a sample of women with fibromyalgia. Spanish J. Psychol. 17, E105 (2014).
Hoffmann, A. A., Frostell, E., Hedman-Lagerlöf, M., McCracken, L. M. & Axelsson, E. Psychometric evaluation of the Pain Vigilance and Awareness Questionnaire (PVAQ) in fibromyalgia: confirmatory factor analysis and the development of a Swedish 8-item version. Eur. J. Pain 28, 396–407 (2024).
Kunz, M. et al. Psychometric properties of the German version of the Pain Vigilance and Awareness Questionnaire (PVAQ) in pain-free samples and samples with acute and chronic pain. Int. J. Behav. Med. 24, 260–271 (2017).
Sampaio Bonafé, F. S., Marôco, J. & Duarte Bonini Campos, J. A. Cross-cultural validation of the Brazilian Portuguese version of the pain Vigilance and Awareness Questionnaire. J Oral Facial Pain Headache 32, e1–e12 (2018).
Gupta, S. & Bhardwaj, R. Pain awareness and pain vigilance as predictors of pain tolerance and pain acceptance in patients with chronic pain. J. Indian Acad. Appl. Psychol. 47, 7–14 (2021).
McCracken, L. M. & Morley, S. The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J. Pain 15, 221–234 (2014).
Yu, L., McCracken, L. M. & Norton, S. The Self Experiences Questionnaire (SEQ): preliminary analyses for a measure of self in people with chronic pain. J. Context. Behav. Sci. 5, 127–133 (2016).
Yu, L., Scott, W., Goodman, R., Driscoll, L. & McCracken, L. M. Measuring ‘self’: preliminary validation of a short form of the self experiences questionnaire in people with chronic pain. Br. J. Pain 15, 474–485 (2021).
Quartana, P. J., Campbell, C. M. & Edwards, R. R. Pain catastrophizing: a critical review. Expert Rev. Neurother. 9, 745–758 (2009).
Petrini, L. & Arendt-Nielsen, L. Understanding pain catastrophizing: putting pieces together. Front. Psychol. 11, 603420 (2020).
Hughes, L. S., Clark, J., Colclough, J. A., Dale, E. & McMillan, D. Acceptance and commitment therapy (ACT) for chronic pain: a systematic review and meta-analyses. Clin. J. Pain 33, 552 (2017).
Lai, L., Liu, Y., McCracken, L. M., Li, Y. & Ren, Z. The efficacy of acceptance and commitment therapy for chronic pain: a three-level meta-analysis and a trial sequential analysis of randomized controlled trials. Behav. Res. Ther. 165, 104308 (2023).
Ma, T.-W., Yuen, A.S.-K. & Yang, Z. The efficacy of acceptance and commitment therapy for chronic pain: a systematic review and meta-analysis. Clin. J. Pain 39, 147 (2023).
Martinez-Calderon, J., García-Muñoz, C., Rufo-Barbero, C., Matias-Soto, J. & Cano-García, F. J. Acceptance and commitment therapy for chronic pain: an overview of systematic reviews with meta-analysis of randomized clinical trials. J. Pain 25, 595–617 (2024).
Trindade, I. A. et al. Efficacy of online-based acceptance and commitment therapy for chronic pain: a systematic review and meta-analysis. J. Pain 22, 1328–1342 (2021).
Veehof, M. M., Trompetter, H. R., Bohlmeijer, E. T. & Schreurs, K. M. G. Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn. Behav. Ther. 45, 5–31 (2016).
Bandalos, D. L. Item meaning and order as causes of correlated residuals in confirmatory factor analysis. Struct. Equ. Modeling 28(6), 903–913 (2021).
Bentler, P. M. & Chou, C.-P. Practical Issues in structural modeling. Soc. Methods Res. 16, 78–117 (1987).
Kłosowska, J. et al. Development, psychometric properties and cut-off scores of the Polish version of the 20-item Pain Anxiety Symptoms Scale (PASS-20) in a chronic pain sample. Psychol. Assess. 37(5), e28–e44 (2025).
Lovibond, P. F. & Lovibond, S. H. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 33, 335–343 (1995).
Zawislak, D. et al. Evaluation of a Polish version of the depression anxiety stress scales (DASS-21). J. Neurosci. Cogn. Stud. 4, 1015 (2020).
Rosenstiel, A. K. & Keefe, F. J. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain 17, 33–44 (1983).
Juczyński, Z. Narzȩdzia pomiaru w promocji i psychologii zdrowia. Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego. Warszawa (2001).
McCracken, L. M. & Dhingra, L. A short version of the Pain Anxiety Symptoms Scale (PASS-20): preliminary development and validity. Pain Res. Manag. 7, 45–50 (2002).
McCracken, L. M., Chilcot, J. & Norton, S. Further development in the assessment of psychological flexibility: a shortened Committed Action Questionnaire (CAQ-8). Eur. J. Pain 19, 677–685 (2015).
Baran, L. N., Hyla, M. A. & Kleszcz, B. Elastyczność psychologiczna: polska adaptacja narzędzi pomiarowych dla praktyków i badaczy. (Wydawnictwo Uniwersytetu Śląskiego, 2019).
McCracken, L. M. & Yang, S.-Y. The role of values in a contextual cognitive-behavioral approach to chronic pain. Pain 123, 137–145 (2006).
Ruscheweyh, R., Marziniak, M., Stumpenhorst, F., Reinholz, J. & Knecht, S. Pain sensitivity can be assessed by self-rating: development and validation of the Pain Sensitivity Questionnaire. Pain 146, 65–74 (2009).
Latka, D. et al. Translation, validation, and cross-cultural adaptation of the Polish version of the Pain Sensitivity Questionnaire. J. Pain Res. 12, 969–973 (2019).
Spielberger, C. D., Gorsuch, R. L. & Lushene, R. E. Manual for the State-Trait Anxiety Inventory (Consulting Psychologists Press, 1970).
Wrześniewski, K. Inwentarz stanu i cechy lęku STAI: polska adaptacja STAI : podręcznik / Kazimierz Wrześniewski [et al.]. (Pracownia Testów Psychologicznych Polskiego Towarzystwa Psychologicznego, Warszawa, 2011).
Wild, D. et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health 8, 94–104 (2005).
Oppenheimer, D. M., Meyvis, T. & Davidenko, N. Instructional manipulation checks: detecting satisficing to increase statistical power. J. Exp. Soc. Psychol. 45(4), 867–872 (2009).
Morren, M. & Paas, L. J. Short and long instructional manipulation checks: what do they measure?. Int. J. Public Opin. Res. 32(4), 790–800 (2020).
Matjašič, M., Vehovar, V. & Manfreda, K. L. Web survey paradata on response time outliers: a systematic literature review. Metodološki zvezki/Adv. Methodol. Stat. 15(1), 23–41 (2018).
Brown, T. A. Confirmatory Factor Analysis for Applied Research 2nd edn. (Guilford Publications, 2015).
DiStefano, C., McDaniel, H. L., Zhang, L., Shi, D. & Jiang, Z. Fitting large factor analysis models with ordinal data. Educ Psychol Meas 79, 417–436 (2019).
Li, C.-H. The performance of ML, DWLS, and ULS estimation with robust corrections in structural equation models with ordinal variables. Psychol. Methods 21, 369–387 (2016).
Hooper, D., Coughlan, J. & Mullen, M. R. Structural equation modelling: guidelines for determining model fit. Electron. J. Bus. Res. Methods 6, 53–60 (2008).
Hu, L. & Bentler, P. M. Cutoff criteria for fit indexes in covariance structure analysis Conventional criteria versus new alternatives. Struct. Equ. Modeling A Multidisciplinary Journal 6, 1–55 (1999).
Whittaker, T. A. Using the modification index and standardized expected parameter change for model modification. J. Exp. Educ. 80, 26–44 (2012).
Terwee, C. B. et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 60, 34–42 (2007).
Haley, S. M. & Fragala-Pinkham, M. A. Interpreting change scores of tests and measures used in physical therapy. Phys Ther 86, 735–743 (2006).
Cohen, J. Set correlation and contingency tables. Appl. Psychol. Meas. 12, 425–434 (1988).
García-Pérez, M. A. Use and misuse of corrections for multiple testing. Methods Psychol. 8, 100120 (2023).
Rubin, M. When to adjust alpha during multiple testing: a consideration of disjunction, conjunction, and individual testing. Synthese 199, 10969–11000 (2021).
Soper, D. S. Free a-priori sample size calculator for structural equation models [Software]. https://www.danielsoper.com/statcalc/calculator.aspx?id=89 (2023).
Funding
The project and Article Processing Charges were funded by grants from the Strategic Program “Excellence Initiative – Research University” at Jagiellonian University (Faculty of Philosophy). The authors are supported by the National Science Centre in Poland under grants no. 2019/35/B/HS6/04320 (PB, JK, EAB), 2020/38/A/HS6/00470 (PB, MŻ, MN, HB, JBr, EAB), and 2020/39/B/HS6/03551 (EAB, RD, IAŁ, PB).
Author information
Authors and Affiliations
Contributions
J.K., P.B., E.B., L.MC., M.N., M.Ż., D.R., H.B., J.Br., K.WK., J.B. designed the study; D.R., I.Ł., H.B., J.Br., M.N., M.Ż., J.B collected the data; J.K. performed statistical analyses; J.K. and A.B. interpreted the results of the analyses; J.K., A.B., D.R., I.Ł., H.B., J.B., K.WK prepared the first draft of the manuscript, P.B., E.B., M.Ż., A.PM and L.MC revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kłosowska, J., Budzisz, A., Rubanets, D. et al. Development and psychometric evaluation of the 12-item Polish version of the Pain Vigilance and Awareness Questionnaire. Sci Rep 15, 26541 (2025). https://doi.org/10.1038/s41598-025-08449-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-08449-6