Abstract
Our study aims to investigate the production of nanocapsules containing chamomile essential oil and assess their antifungal properties. We have developed a technological process for producing nanocapsules, selected chamomile raw materials, extracted the essential oil, and conducted research on the antimicrobial activity of nanocapsules against four fungal cultures: Candida albicans CGMCC 2.538, Aspergillus fumigatus CGMCC 3.5925, Trichophyton rubrum CGMCC 3.3777 and Epidermophyton floccosum CGMCC 3.3722. Our research revealed significant antimicrobial activity of chamomile-containing nanocapsules against all tested fungi. The zones of fungal inhibition varied depending on the oil concentration and were statistically significant (P < 0.05). The obtained results hold practical significance for the development of antimicrobial agents based on plant oils in the treatment of fungal infections. Further research may focus on the molecular mechanisms of chamomile oil’s action, clinical trials in humans, and the optimization of nanocapsule formulations. These steps may contribute to the development of more effective and targeted antimicrobial agents for combating fungal infections and improving patient health.
Similar content being viewed by others
Introduction
Modern pharmacology is actively evolving, offering new approaches to the treatment and prevention of diseases. One of the notable recent advancements is the use of nanocapsules—microscopic shells designed for the precise delivery of active substances to specific areas of the body1. These structures are spherical carriers capable of encapsulating medicinal components, enhancing their stability and bioavailability while reducing toxicity, making them a promising tool in medicine and therapy2.
In recent years, particular interest has been directed toward the encapsulation of medicinal plant extracts. The diverse array of biologically active compounds found in flowers, leaves, and roots of plants makes them attractive candidates for inclusion in nanocapsule formulations. This approach improves the effectiveness of natural ingredients, prolongs their action, and expands their scope of medical and cosmetic applications3.
Chamomile (Matricaria chamomilla) holds a special place among medicinal plants due to its unique essential oil composition, which includes anti-inflammatory, antiseptic, and antifungal compounds. In recent years, the potential use of chamomile in nanocapsule formulations has been actively studied to enhance its therapeutic effects, especially in treating fungal infections4.
The relevance of this research area is driven by the increasing resistance of fungal pathogens to traditional antifungal drugs, as well as the ongoing search for safe and effective natural alternatives. Nanocapsules enable controlled and prolonged release of active substances, which makes them particularly promising in the treatment of chronic fungal infections5.
One of the key challenges in modern pharmacology is the low bioavailability of certain plant extracts. Many valuable phytocomponents are poorly absorbed in the human body, which limits their therapeutic potential. Encapsulation of chamomile essential oil into nanostructures addresses this issue by ensuring stable and efficient delivery of active substances6. Additionally, synthetic drugs often cause adverse side effects. In this context, chamomile offers a safer alternative, and nanocapsules help reduce risks through targeted and localized action.
Given the increasing prevalence of fungal diseases and the limitations of current treatment options, the application of chamomile-based nanocapsules opens new prospects for developing innovative, natural, and targeted therapeutic agents7.
Thus, this study aims to address pressing issues in modern pharmacology related to the safety and efficacy of fungal disease treatment, while also contributing to the promising field of medicinal plant use in nanopharmaceutics.
Various types of nanocapsules have been developed for the effective delivery of active substances. Among the most studied are liposomes—membrane vesicles with a double lipid bilayer that can encapsulate hydrophilic and lipophilic substances, providing protection and targeted delivery8. Nanoparticles, ranging from 1 to 100 nm, made from polymers, metals, and other materials, are widely used for drug encapsulation9. Microemulsions are stable systems based on oil, water, and emulsifiers that can transport fat-soluble compounds. Nanoaggregates, which are clusters of active substance molecules, improve the solubility and bioavailability of drugs10. Nanogels are gel-based structures capable of controlled release, often made from biodegradable polymers11. Polymeric nanoparticles, synthesized from polylactide, polyglycolide, and other polymers, are known for their high stability. Nanospheres are uniform spherical formations that effectively encapsulate active substances12. The choice of nanocapsule type depends on the research objectives, the physicochemical properties of the compound, and the desired release profile.
The mechanisms of drug delivery using nanocapsules depend on their design, but several general principles can be identified. One of these is penetration through mucous membranes (oral cavity, gastrointestinal tract, respiratory tract), enabling rapid absorption of the drug13. Systemic delivery via the bloodstream is also important: nanocapsules circulate throughout the body and reach target tissues, which is particularly significant for multi-organ therapies14. Another crucial factor is protection from metabolism: the capsule shell can prevent the degradation of the active compound by liver enzymes, prolonging its action. Furthermore, functionalizing the surface of nanocapsules with molecular markers allows for targeted delivery of the drug to specific cells or organs15. Controlled release ensures gradual delivery of the substance into the body, maintaining stable concentrations and reducing the risk of side effects.
Chamomile oil contains several bioactive compounds, such as bisabolol—an anti-inflammatory and antimicrobial agent that promotes skin regeneration16, and azulene, which has antiseptic activity and is effective for treating skin inflammation and itching17. Other antiseptic components are also present and beneficial for surface skin damage17,18. Chamomile is known for its antispasmodic and sedative properties, useful in managing pain and anxiety; some compounds also exhibit antifungal activity18.
Despite its widespread use in traditional medicine, chamomile’s antifungal properties remain insufficiently studied. Laboratory studies have confirmed the activity of bisabolol and azulene against dermatophytes and Candida species17,18,19,20,21,22. However, clinical studies are needed to confirm their effectiveness in practice.
Thus, further investigation into the antifungal activity of chamomile oil, particularly in nanocapsule form, represents a relevant scientific task with significant clinical application potential.
Fungal diseases such as dermatomycoses and candidiasis represent a significant medical concern. The resistance of pathogens to conventional antifungal drugs complicates treatment and increases the risk of complications20,21,22.
Given the growing interest in natural and safe treatment methods, plant extracts like chamomile are gaining particular importance. Its well-known antiseptic and anti-inflammatory properties, as well as the proven laboratory activity of specific components against fungi, make this plant a promising candidate for the development of new antifungal agents.
Modern nanotechnologies significantly enhance the efficacy of plant-based extracts through precise delivery and controlled release of active substances. The use of nanocapsules containing chamomile essential oil can provide prolonged action, minimize side effects, and improve the treatment of fungal infections.
This study aims to develop chamomile oil nanocapsules and evaluate their antifungal activity addresses relevant pharmaceutical and medical challenges and holds high practical significance.
Research objective
To develop a production technology for nanocapsules containing chamomile essential oil and to evaluate their antifungal properties.
Research tasks
-
(a)
To develop a technological process for obtaining nanocapsules containing chamomile oil;
-
(b)
To assess the antifungal activity of the resulting nanocapsules using in vitro models.
Methods and materials
Materials
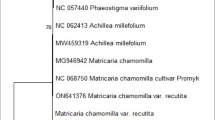
The study was conducted in 2022 at a pharmaceutical laboratory in Beijing, China. Fresh Chamomile flowers (Matricaria chamomilla) were harvested in late May, during the full flowering phase, in the agricultural zone of Hebei Province, known for its moderate continental climate with average May temperatures of 18–23 °C, low rainfall, and high sunlight exposure. These climatic conditions favor the accumulation of bioactive compounds in chamomile.
Flowers were harvested on sunny mornings, when the essential oil content peaks. Post-harvest, the flowers were dried in a YZG-600 vacuum drying cabinet (Shanghai Tofflon Science) at 38 °C for 48 h, monitored via a digital thermostat and internal sensor system.
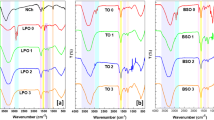
To extract the essential oil, steam distillation was performed using a Clevenger-type apparatus (Borosil, India). In this setup, the dried plant material was boiled in water; the resulting vapor was cooled in a condenser (25 °C) and condensed into a liquid. The oil was then separated based on its lower density using the same apparatus. To obtain 1 L of essential oil, 3–4 kg of dried chamomile flowers were required. The oil was then purified by filtration and drying over anhydrous sodium sulfate.
Plant material identification and herbarium deposition
The chamomile plant material (Matricaria chamomilla L.) used in this study was formally identified by Dr. Mojiao Zhao, a specialist in traditional Chinese medicinal plants from the Department of Chinese Medicine and Health Care, Changchun Humanities and Sciences College, Changchun, Jilin Province, China. A voucher specimen of the plant has been deposited in the Herbarium of Medicinal Plants at the College of Pharmacy, Yanbian University (Yanji, Jilin Province, China), under the accession number YBU-MP-2024-078. This specimen is publicly accessible and available for reference to support verification and reproducibility of the study.
Study design
The study followed an experimental design to evaluate the antifungal activity of nanocapsules containing chamomile essential oil. The stages included:
Nanocapsule production
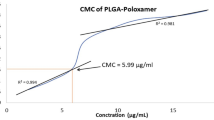
The emulsion–diffusion method was used.
The biopolymer chitosan (MW ~ 100 kDa) was used as the encapsulating agent.
Chamomile essential oil was mixed into a 1% acetic acid chitosan solution.
Emulsification was performed via ultrasonic treatment using a VCX-750 ultrasonic processor (Sonics & Materials, USA) at 40% amplitude, 20 kHz, for 10 min.
The organic solvent (dimethyl sulfoxide, DMSO) was removed using rotary evaporation (RE-52AA, Yarong Biochemical) at 40 °C under reduced pressure.
Characterization
Nanocapsule size was analyzed using dynamic light scattering (DLS) (Zetasizer Nano ZS, Malvern Instruments).
The size distribution was in the range of 100–500 nm, with a positive zeta potential due to chitosan.
Test microorganisms
Strains were obtained from the China General Microbiological Culture Collection Center (CGMCC):
-
Candida albicans CGMCC 2.538.
-
Aspergillus fumigatus CGMCC 3.5925.
-
Trichophyton rubrum CGMCC 3.3777.
-
Epidermophyton floccosum CGMCC 3.3722.
Fungi were cultivated on Sabouraud Dextrose Agar (SDA) (Oxoid, UK) under standard conditions.
Antifungal testing
The agar well diffusion method was employed.
Inoculum: 100 µL of fungal suspension adjusted to 106 CFU/mL.
Wells (6 mm) were filled with 100 µL of nanocapsule suspension (concentrations of 0.1%, 0.25%, 0.5% essential oil).
Plates were incubated at 30 °C, 75% RH for 48 h.
A standard antifungal agent, Fluconazole (25 µg/mL) (Pfizer, China), served as the positive control.
Sterile water was used as a negative control.
Measurement and evaluation
Zones of inhibition were measured manually using Vernier calipers with ± 0.1 mm precision, in triplicate.
The minimum inhibitory concentration (MIC) was defined as the lowest concentration with visible inhibition.
Statistical analysis
Data were processed using IBM SPSS Statistics 25.0. Results are expressed as mean ± standard deviation (SD). Comparisons were made using the Student’s two-tailed t-test, with P < 0.05 considered statistically significant. Trends (0.05 ≥ P < 0.1) were also noted. Correlation analysis was performed using Pearson’s correlation coefficient, assuming normal distribution of data. The assumption of normality was tested using the Shapiro–Wilk test prior to performing parametric analyses. For data not following a normal distribution (e.g., Epidermophyton floccosum CGMCC 3.3722), non-parametric testing using the Wilcoxon signed-rank test was performed to ensure valid comparison. A linear regression model was used to determine the relationship between oil concentration and inhibition zone diameter; the model was selected based on the best R2 value and residual analysis.
Results
The study evaluated the antifungal activity of capsules containing chamomile (Matricaria chamomilla) essential oil against four fungal species. The tables present the mean inhibition zone diameters (in mm), minimum inhibitory concentrations (MICs), growth kinetics, morphological changes, and survival rates of the microorganisms at various oil concentrations.
The results demonstrate a clear dose-dependent antifungal effect of chamomile essential oil encapsulated in nanocapsules against both Candida albicans CGMCC 2.538 and Aspergillus fumigatus CGMCC 3.5925. In Table 1 and Fig. 1, increasing the concentration of chamomile oil from 0.1 to 1.0 g/100 g nanocapsules led to a statistically significant enlargement of the inhibition zone, reaching 15.7 ± 0.6 mm at the highest concentration (P < 0.001). Although the activity remained lower than the positive control (20.0 ± 0.5 mm), the results indicate a strong inhibitory effect, especially at concentrations ≥ 0.5 g/100 g.
In Table 2, a similar dose-dependent trend was observed against Aspergillus fumigatus CGMCC 3.5925, although the inhibition zones were generally smaller than those seen with Candida albicans CGMCC 2.538. The highest concentration of 1.0 g/100 g resulted in an inhibition zone of 9.4 ± 0.3 mm, significantly greater than at lower doses and compared to the control (P < 0.001, Fig. 2). These findings suggest that while Aspergillus fumigatus CGMCC 3.5925 is less sensitive to chamomile oil than Candida albicans CGMCC 2.538, the nanocapsule formulation still confers measurable antifungal activity.
Overall, the data support the potential of chamomile essential oil nanocapsules as a natural antifungal agent, with efficacy varying by fungal species and dosage.
The antifungal effect of chamomile essential oil in nanocapsules was also evident against dermatophytes, specifically Trichophyton rubrum CGMCC 3.3777 and Epidermophyton floccosum CGMCC 3.3722. As shown in Table 3, the inhibition zone diameters progressively increased with higher oil concentrations, indicating a robust dose–response relationship. Even at the lowest tested dose (0.1 g/100 g), some inhibitory activity was noted, while the maximum concentration (1.0 g/100 g) approached the efficacy of the positive control (Figs. 3 and 4). This suggests that Trichophyton rubrum CGMCC 3.3777 are moderately susceptible to the tested formulation.
In contrast, Table 4 reveals that Epidermophyton floccosum CGMCC 3.3722 exhibited the lowest sensitivity among the four tested fungal species. Although antifungal activity was statistically significant at all concentrations (P < 0.001, Fig. 5), the inhibition zones remained smaller compared to other fungi, including Trichophyton rubrum CGMCC 3.3777. The response to increasing concentrations, while significant, remained relatively modest, suggesting a more resistant phenotype.
These findings emphasize the varying degrees of fungal susceptibility to chamomile oil and support the potential for its selective use in treating dermatophytic infections, particularly those caused by Trichophyton rubrum CGMCC 3.3777.
Analysis of variance (ANOVA) revealed statistically significant differences between the groups with different oil concentrations (P < 0.001 in all cases). The Student’s t-test also showed significant differences between each treatment group and the positive control (P < 0.001).
Regression analysis showed a strong positive correlation between chamomile oil concentration and the diameter of fungal inhibition zones (r = 0.92, P < 0.001). On average, a 0.1 g/100 g increase in oil concentration led to a 3.5 mm increase in inhibition zone diameter (P < 0.001) across all tested fungal strains. This relationship was not strictly linear in all species: Candida albicans CGMCC 2.538 and Trichophyton rubrum CGMCC 3.3777 showed more pronounced responses, while Epidermophyton floccosum CGMCC 3.3722 exhibited weaker sensitivity and a potential threshold effect.
Quantitative assessment of fungal growth (Table 5) revealed dose-dependent suppression. For instance, the growth of Candida albicans CGMCC 2.538 was nearly halted (1.0 ± 0.2 mm/day) compared to the control (8.2 ± 0.4 mm/day, P < 0.001). Morphological analysis confirmed these findings: the alteration score reached 4.8 ± 0.2 for Candida albicans CGMCC 2.538, indicating severe structural disruption, whereas the control group showed minimal changes (0.5 ± 0.2). Similar patterns, though less pronounced, were observed in other fungi.
These results demonstrate not only fungistatic but also fungicidal potential of the oil, confirmed by drastic reductions in colony size and visible destruction of cellular structures.
Figure 6 further illustrates differential fungal susceptibility. At the highest concentration (1.0 g/100 g), the survival rate of Candida albicans CGMCC 2.538 dropped to 0%, while other fungi exhibited varying degrees of resistance. The greater sensitivity of Candida albicans CGMCC 2.538 may be attributed to the higher affinity or uptake of chamomile oil constituents—such as α-bisabolol and chamazulene—by yeast-like cells compared to dermatophytes.
While the positive control consistently produced the largest inhibition zones (Tables 1, 2, 3 and 4), at the highest tested dose (1.0 g/100 g), chamomile oil nanocapsules demonstrated comparable antifungal activity, particularly against Candida albicans CGMCC 2.538 (15.7 ± 0.6 mm vs. 20.0 ± 0.5 mm) and Trichophyton rubrum CGMCC 3.3777 (14.1 ± 0.5 mm vs. 18.0 ± 0.5 mm), supporting the clinical relevance of chamomile-based formulations.
Discussion
The present study offers important insights into the antifungal potential of chamomile oil-loaded nanocapsules and allows for a deeper understanding of their pharmacological prospects. Our findings indicate a clear dose-dependent inhibition of fungal growth, with the highest activity observed against Candida albicans CGMCC 2.538, and lesser effects against Aspergillus fumigatus CGMCC 3.5925 and Epidermophyton floccosum CGMCC 3.3722. This differential response likely reflects structural and metabolic differences between fungal species, which should be considered when designing targeted antifungal therapies.
The statistically confirmed correlation and regression analyses reinforce the robustness of the dose–response relationship, suggesting that precise titration of the oil concentration could enhance efficacy while minimizing toxicity risks. However, the translation of these in vitro findings to clinical settings requires caution. Nanocapsule-based delivery systems, while effective in increasing bioavailability, may also alter the oil’s interaction with host tissues, which warrants further investigation.
Compared to similar studies involving other plant-derived essential oils, the antifungal activity of chamomile oil is comparable. For instance, nanocapsules with tea tree and garlic oils demonstrated inhibition zones and MIC values within the same range as chamomile23,24,25,26,27,28. This suggests that chamomile may be a viable alternative or complement to other phytotherapeutic agents, especially considering its known anti-inflammatory and wound-healing properties.
Nevertheless, previously reported differences in MIC values and inhibition zones for various essential oils—such as melissa, lavender, rosemary, thyme, ginger, and rose29,30,31,32,33,34 highlight the complexity of plant-based antifungal therapy. These differences may stem not only from intrinsic chemical compositions but also from variations in nanocapsulation techniques, oil purity, and fungal strain susceptibility. Hence, a standardized approach to evaluating antifungal activity is crucial for meaningful comparisons.
Despite promising results, our study has limitations. The exclusive reliance on laboratory models restricts the ecological validity of our findings. Only four fungal species were tested, limiting broader generalization. Moreover, potential interactions between the nanocapsules and the fungal microenvironment, including resistance mechanisms or biofilm formation, were not explored.
Our proposed technological scheme for the production of chamomile oil nanocapsules adds practical value to the research, paving the way for scalable manufacturing. However, future studies should not only optimize dosing and assess long-term stability but also include cytotoxicity assessments and in vivo validation.
Importantly, the observed antifungal effect of chamomile oil was comparable to that of other well-studied plant oils, including chilli, laurel, orange, and thyme31,35,36. This reinforces the relevance of chamomile as a competitive natural agent in antifungal treatment development.
In conclusion, this study contributes to the growing body of evidence supporting the therapeutic potential of plant-derived nanocapsules. Our findings emphasize the importance of species-specific responses, dose optimization, and delivery method refinement. Further research, particularly involving clinical trials and mechanistic studies, is essential to establish chamomile oil as a safe and effective antifungal agent in modern medicine.
Conclusions
This study confirms the significant antifungal potential of nanocapsules containing chamomile essential oil, with a clear dose-dependent response observed across all tested fungal strains. Candida albicans CGMCC 2.538 and Trichophyton rubrum CGMCC 3.3777 were particularly sensitive, while Epidermophyton floccosum CGMCC 3.3722 showed greater resistance.
The nanocapsule formulation enhanced the bioavailability and efficacy of chamomile oil, supporting its potential as a natural alternative to conventional antifungal agents. Notably, our technological approach—from raw material selection to final encapsulation—offers a reproducible and scalable method for producing bioactive plant-based formulations.
These findings provide a foundation for future research into molecular mechanisms, clinical testing, and optimization of nanocapsule design for targeted antifungal therapies.
Data availability
Data will be available on request from corresponding author.
References
Karam, T. K., Ortega, S., Nakamura, T. U., Auzély-Velty, R. & Nakamura, C. V. Development of chitosan nanocapsules containing essential oil of Matricaria chamomilla L. for the treatment of cutaneous leishmaniasis. Int. J. Biol. Macromol. 162, 199–208. https://doi.org/10.1016/j.ijbiomac.2020.06.149 (2020).
Das, S. et al. Antimicrobial activity of chamomile essential oil: Effect of different formulations. Molecules 24(23), 4321. https://doi.org/10.3390/molecules24234321 (2019).
Yilmaz, M. T. et al. Electrospraying method for fabrication of essential oil loaded-chitosan nanoparticle delivery systems characterized by molecular, thermal, morphological and antifungal properties. Innov. Food Sci. Emerg. Technol. 52, 166–178. https://doi.org/10.1016/j.ifset.2018.12.005 (2019).
Raveau, R., Fontaine, J. & Lounès-Hadj Sahraoui, A. Essential oils as potential alternative biocontrol products against plant pathogens and weeds: A review. Foods 9(3), 365. https://doi.org/10.3390/foods9030365 (2020).
Yien, R. M. K. et al. Nanotechnology promoting the development of products from the biodiversity of the Asteraceae family. Nutrients 15(7), 1610. https://doi.org/10.3390/nu15071610 (2023).
Parashar, P. & Pathak, K. Augmented stability and efficacy of essential oils through encapsulation approach. In Essential Oils: Extraction Methods and Applications (eds Altalhi, T. & Cruz, J. N.) 269–289 (Scrivener Publishing LLC, 2023).
Mehta, S. & MacGillivray, M. Aromatherapy in textiles: A systematic review of studies examining textiles as a potential carrier for the therapeutic effects of essential oils. Textiles 2(1), 29–49. https://doi.org/10.3390/textiles2010003 (2022).
Nair, A. et al. Nanoparticles—Attractive carriers of antimicrobial essential oils. Antibiotics 11(1), 108. https://doi.org/10.3390/antibiotics11010108 (2022).
Mamusa, M., Resta, C., Sofroniou, C. & Baglioni, P. Encapsulation of volatile compounds in liquid media: Fragrances, flavors, and essential oils in commercial formulations. Adv. Colloid Interface Sci. 298, 102544. https://doi.org/10.1016/j.cis.2021.102544 (2021).
AbouAitah, K. & Lojkowski, W. Nanomedicine as an emerging technology to foster application of essential oils to fight cancer. Pharmaceuticals 15(7), 793. https://doi.org/10.3390/ph15070793 (2022).
Pinto, G. B., dos ReisCorrêa, A., da Silva, G. N. C., da Costa, J. S. & Figueiredo, P. L. B. Drug development from essential oils: New discoveries and perspectives. In Drug Discovery and Design Using Natural Products (ed. Cruz, J. N.) 79–101 (Springer, 2023). https://doi.org/10.1007/978-3-031-35205-8_4.
El Mihyaoui, A. et al. Chamomile (Matricaria chamomilla L.): A review of ethnomedicinal use, phytochemistry and pharmacological uses. Life 12(4), 479. https://doi.org/10.3390/life12040479 (2022).
Kumar, A., Singh, P., Gupta, V. & Prakash, B. Application of nanotechnology to boost the functional and preservative properties of essential oils. In Functional and Preservative Properties of Phytochemicals (ed. Prakash, B.) 241–267 (Academic Press, 2020).
Sharma, N. et al. Nanoencapsulation-a novel strategy for enhancing the bioactivity of essential oils: A review. Indian J. Agric. Res. 56(3), 241–248. https://doi.org/10.18805/IJARe.A-5806 (2022).
Jugreet, B. S., Suroowan, S., Rengasamy, R. K. & Mahomoodally, M. F. Chemistry, bioactivities, mode of action and industrial applications of essential oils. Trends Food Sci. Technol. 101, 89–105. https://doi.org/10.1016/j.tifs.2020.04.025 (2020).
Nuță, D. C. et al. Contribution of essential oils to the fight against microbial biofilms—A review. Processes 9(3), 537. https://doi.org/10.3390/pr9030537 (2021).
Ashraf, M., El-Sawy, H. S., El Zaafarany, G. M. & Abdel-Mottaleb, M. M. Can essential oils/botanical agents smart-nanoformulations be the winning cards against psoriasis?. Pharmaceutics 15(3), 750. https://doi.org/10.3390/pharmaceutics15030750 (2023).
Ni, Z. J. et al. Recent updates on the chemistry, bioactivities, mode of action, and industrial applications of plant essential oils. Trends Food Sci. Technol. 110, 78–89. https://doi.org/10.1016/j.tifs.2021.01.070 (2021).
Elmowafy, E., El-Marakby, E. M., Gad, H. A. & Gad, H. A. Delivery systems of plant-derived antimicrobials. In Promising Antimicrobials from Natural Products (eds Rai, M. & Kosalec, I.) 397–442 (Springer, 2022).
Mun, H. & Townley, H. E. Nanoencapsulation of plant volatile organic compounds to improve their biological activities. Planta Med. 87(03), 236–251. https://doi.org/10.1055/a-1289-4505 (2021).
Wang, W. et al. Advancing aggregation-induced emission-derived biomaterials in viral, tuberculosis, and fungal infectious diseases. Aggregate 6, e715. https://doi.org/10.1002/agt2.715 (2025).
Lodi, R. S. et al. Current research on the medical importance of Trametes species. Fungal Biol. Rev. 51, 100413. https://doi.org/10.1016/j.fbr.2025.100413 (2025).
Ebadi, P. & Azizkhani, M. Evaluation of antimicrobial and antioxidant activity of Carum copticum L. essential oil encapsulated in electrospun cellulose acetate nanofibers. J. Essent. Oil Res. 35(6), 579–588. https://doi.org/10.1080/10412905.2023.2270547 (2023).
Ibili, H. et al. Investigation of poly (lactic acid) nanocapsules containing the plant extract via coaxial electrospraying method for functional nonwoven applications. J. Ind. Text. 51, 5304S-5327S. https://doi.org/10.1177/1528083721988950 (2022).
Abisheva, A. et al. AK-2011 strain for the development of a vaccine against equine rhinopneumonitis. Transbound. Emerg. Dis. 69(5), e1972–e1981. https://doi.org/10.1111/tbed.14531 (2022).
Ivkin, DYu., Karavaeva, A. V., Chernykh, T. F. & Krasnova, M. V. Antifungal activity of thiadiazole derivative in experimental candidiasis in mice. Drug Dev. Regist. 13(4), 251–258. https://doi.org/10.33380/2305-2066-2024-13-4-1923 (2024).
Chernykh, T. F. et al. Updating information of mycoses and antifungal medicines to find effective platforms for the production of new thiazole compounds. Drug Dev. Regist. 13(4), 27–44. https://doi.org/10.33380/2305-2066-2024-13-4-1871 (2024).
Grishin, A., Spaska, A. & Kayumova, L. Correction of overactive bladder with botulinum toxin type A (BTX-A). Toxicon 200, 96–101. https://doi.org/10.1016/j.toxicon.2021.07.005 (2021).
Froiio, F. et al. Edible polymers for essential oils encapsulation: Application in food preservation. Ind. Eng. Chem. Res. 58(46), 20932–20945. https://doi.org/10.1021/acs.iecr.9b02418 (2019).
Perinelli, D. R., Palmieri, G. F., Cespi, M. & Bonacucina, G. Encapsulation of flavours and fragrances into polymeric capsules and cyclodextrins inclusion complexes: An update. Molecules 25(24), 5878. https://doi.org/10.3390/molecules25245878 (2020).
Guzmán, E. & Lucia, A. Essential oils and their individual components in cosmetic products. Cosmetics 8(4), 114. https://doi.org/10.3390/cosmetics8040114 (2021).
Selvakumar, V. et al. Seed-based oil in nanomaterials synthesis and their role in drug delivery and other applications. In Secondary Metabolites Based Green Synthesis of Nanomaterials and Their Applications (ed. Husen, A.) 241–290 (Springer, 2023).
Paul, S., El Bethel Lalthavel Hmar, J. H. & Zothantluanga, H. K. S. Essential oils: A review on their salient biological activities and major delivery strategies. Sci. Vis. 20(2), 54–71. https://doi.org/10.33493/scivis.20.02.01 (2020).
dos Santos, M. K. et al. A chitosan hydrogel-thickened nanoemulsion containing Pelargonium graveolens essential oil for treatment of vaginal candidiasis. J. Drug Deliv. Sci. Technol. 56, 101527. https://doi.org/10.1016/j.jddst.2020.101527 (2020).
Paramanya, A., Sharma, S., Bagdat, R. B. & Ali, A. Recent practices of medicinal and aromatic plants in nanotechnology. In Nanomaterials for Agriculture and Forestry Applications (eds Husen, A. & Jawaid, M.) 435–467 (Elsevier, 2020).
Amalraj, A., Haponiuk, J. T., Thomas, S. & Gopi, S. Preparation, characterization and antimicrobial activity of polyvinyl alcohol/gum arabic/chitosan composite films incorporated with black pepper essential oil and ginger essential oil. Int. J. Biol. Macromol. 151, 366–375. https://doi.org/10.1016/j.ijbiomac.2020.02.176 (2020).
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
T.L., X.Q., M.Z., D.Z., and J.G. contributed equally to the experimentation. T.L. and X.Q. wrote and edited the article. M.Z. and D.Z. equally designed and conducted the experiment. J.G. studied scientific literature about the topic. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, T., Qu, X., Zhao, M. et al. Investigation of the production and antifungal properties of nanocapsules containing chamomile essential oil. Sci Rep 15, 23981 (2025). https://doi.org/10.1038/s41598-025-08802-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08802-9