Abstract
Nosocomial infections have become one of the major causes of mortality among hospitalized patients. To improve the quality of cleaning and disinfection for hospital environmental surfaces, we conducted a multidisciplinary team (MDT) intervention study with a non-randomized control group in a general hospital in China. The MDT comprised members with educational backgrounds in nursing, clinical medicine, public health, or laboratory science. Fluorescent labeling and microbiological sampling were used to evaluate the cleaning levels of environmental surfaces. A questionnaire was employed to assess cleaners’ knowledge awareness, cleaners’ misconduct was examined via on-site inspection, and detection of multi-drug resistant organisms and calculation of hospital-acquired infection (HAI) rate were also conducted. After MDT intervention, cleaning levels were significantly improved (e.g., total cleaning rate was increased from 66.75 to 82.10%, P < 0.001), cleaners’ knowledge awareness was enhanced (total qualified rate was increased from 51.61 to 83.15%, P < 0.01), misconduct rate was reduced (from 38.48 to 10.43%, P < 0.001), and detection rates of multi-drug resistant organisms and the HAI rate (from 1.29 to 0.88%, P < 0.01) were both significantly reduced. Our study demonstrates that the MDT model shows promising potential in the management of cleaning and disinfection in hospital environmental surfaces.
Similar content being viewed by others
Introduction
The cleaning quality of environmental surfaces in healthcare facilities is the foundation of infection prevention and control1. Studies have shown that pathogens such as Clostridium difficile, norovirus, or multi-drug resistant organisms in the hospital environment may spread to patients, and also pose a threat to healthcare workers2. Contaminated environmental surfaces are critical in driving the outbreaks of hospital-acquired infections (HAIs), which are the primary cause of preventable death and disability among hospitalized patients3. In the United States, HAIs is the sixth leading cause of death4. In 2002, there were 1.7 million of HAIs, about 99,000 hospitalized patients died of HAIs, and 1 in 31 hospitalized patients developed HAIs each day5,6. It was estimated that the direct economic burden of HAIs in the United States was between 28 and 34 billion, of which 25 to 32 billion could be saved with effective infection control programs7. Intensive cleaning and disinfection of environmental surfaces can reduce the incidence of infections caused by multi-drug resistant organisms and Clostridium difficile by 10 to 30 percent8. Therefore, cleaning and sterilizing the hospital environmental surfaces has become a indispensable measure for preventing nosocomial infection9.
The cleaning staff play a key role in the cleaning and disinfection of hospital environmental surfaces10. However, the effective management and systematic training by their superiors are essential for achieving a higher level of efficiency in their work. The multidisciplinary team (MDT) model was initially a multidisciplinary diagnosis and treatment model, which originated in the United States in the 1950s. This model integrates the professional knowledge and skills of multiple related disciplines to provide patients with comprehensive diagnosis and treatment plans11. Now it is widely applied in hospital management and has achieved remarkable results, such as improving tumor diagnosis and treatment12enhancing the management of major and rare diseases13 and pain14cutting the cost of non-chargeable consumables15and optimizing blood glucose management16 and multi-drug resistant organism control17.
In this study, we first conducted a baseline survey on the quality of cleaning and disinfection of hospital environmental surfaces prior to any intervention. Subsequently, we implemented the MDT model to enhance the management of this critical process. Our MDT model comprised members from the Infection Control Office (ICO), the Property Management Office (PMO), and different clinical departments. The members with different educational backgrounds (including nursing, clinical medicine, public health, or laboratory science) worked together to manage surface cleaning and disinfection in the hospital. Our initial hypothesis posited that the implementation of the MDT model would significantly improve the effectiveness of environmental surface cleaning and disinfection protocols. As expected, our data strongly supported this hypothesis. Overall, our findings highlight the promising future applications of the MDT model in optimizing hospital environmental surface cleaning and disinfection management, thereby contributing to enhanced patient safety and infection control practices.
Methods
Study design
To investigate the effect of MDT model application in cleaning and disinfection of hospital environmental surface, we conducted a MDT intervention study with a non-randomized control group in a universal hospital in China from November 2020 to December 2022. For the control group, the study was conducted in the period ranging from November 2020 to March 2021 and no intervention was used; for the intervention group, the MDT model was employed to intervene the management of cleaning and disinfection of environmental surface from April 2021 to December 2022. Informed consent was obtained from all subjects. All experimental protocols were approved by the Ethics Committee of Weifang People’s Hospital, Shandong Second Medical University. All experiments were performed in accordance with relevant guidelines and regulations.
Intervention
From April 2021 to December 2022, the MDT model was employed to intervene in the quality management of cleaning and disinfection of the hospital environmental surface in this study. The MDT included three nurses, one laboratory physician, and one public health physician from the ICO, one property manager and one nurse from the PMO, and about 40 infection control doctors and nurses from different clinical departments. MDT members worked together to establish an efficient management system.
Two ICO nurses conducted quarterly theoretical training for cleaners using the case-based learning (CBL) method18weekly inspections on key clinical departments like ICU and Burn Unit, and monthly on-site inspection in general areas like consulting rooms. The ICO public health physician and another nurse reviewed surveillance footage weekly to assess the cleaning quality and provided feedback via infection control system. They also refined and standardized the work processes. For example, they designed a flowchart for bed unit cleaning and disinfection and posted them on cleaning carts for easy reference. This flowchart is provided in the Supplementary Information. The ICO laboratory physician was responsible for the fluorescent labeling and microbiological sampling and shared the results with clinical departments and the PMO within 48 h. Subsequently, rewards or sanctions for cleaners were implemented based on the assessment outcomes.
The PMO property manager was in charge of the establishment of assessment standards for the property company and cleaners, and conducted quarterly evaluations and issued notifications. The PMO nurse conducted weekly and scenario-based training of cleaners, and also provided one-on-one and hands-on training for new hires. Work of new hires (less than 3 months) was examined 2–3 times per week while those with more than six months’ experience were only subjected to monthly inspection.
One doctor and one nurse from each clinical department involved were responsible for providing personalized training to cleaners on cleaning and disinfection, to cope with challenges and risks specific to clinical departments. Monthly inspections were conducted to monitor cleaners’ performance, with timely feedback and guidance provided for any issues identified during the process.
Fluorescent labeling and microbiological sampling
We adopted the methods of fluorescent labeling19 and microbiological sampling to evaluate the cleaning and disinfection of hospital environmental surface. 40 wards and consulting rooms were selected for the control group and 47 wards and consulting rooms were chosen for the MDT intervention group. Briefly, ICO members used fluorescent markers to label the surfaces of bedside tables, door handles, buttons, desks, computer equipment, and others with an “O” symbol, and recorded the detailed positions and quantities. The cleaners were not informed of the existence of fluorescent labeling and next inspection. After 24 h, ICO members used a special flashlight to check the existence of fluorescent symbols. Complete disappearance of the labels was considered as clean. We calculated the cleaning rate of environmental surface as following: The cleaning rate = (number of clean spots/number of fluorescent labeling spots) ×100%.
In addition, we also used microbiological sampling method to evaluate the cleaning level of environmental surface in some of the selected spots, following the protocol from Chinese hygienic standard for disinfection in hospitals (GB15982—2012). Briefly, take a standard sterilized frame of 5 cm×5 cm and place it on the surface of the object to be tested. Use a sterile cotton swab soaked in a sterile solution containing the corresponding neutralizing agent. Wipe back and forth horizontally and vertically 5 times within the frame, and rotate the cotton swab accordingly. Cut off the part that has been in contact with the hand, put the cotton swab into a test tube containing 10 ml of the sampling solution, and send it for determination immediately. If the colony forming unit (CFU) per square centimeters is less than 10, it is regarded that the cleaning level of the detection spot is qualified. The qualification rate = (number of qualified spots/number of detection spots) ×100%.
On-site inspection and questionnaire survey
The ICO members adopted on-site inspection method to evaluate the quality of cleaning and disinfection of environmental surface, which included the visibility of stains or blood and the accuracy of cleaning and disinfection records. 134 wards and consulting rooms were selected for the control group and 185 wards and consulting rooms were selected for the MDT intervention group. Misconduct problems were regarded as positive when there were visible stains or blood on the surface of the objects or inaccurate records of cleaning and disinfection. The misconduct rate = (number of inspection items with misconduct/number of total inspection items) × 100%.
For the questionnaire survey, the cleaners who worked in wards and consulting rooms were involved. The control group includes 80 cleaners and the intervention group includes 108 ones. The content of questionnaire20 includes five categories: preparation and use of disinfectants, usage methods of cleaning rags, terminal disinfection methods for bed units, cleaning and disinfection methods for surfaces contaminated by multi-drug resistant bacteria, and required frequency of cleaning and disinfection. The awareness rate of specific knowledge of each category among cleaners = (number of cleaners giving right answers/number of cleaners taking the survey) × 100%. The questionnaire was provided in the Supplementary Information.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 10. Enumeration data were expressed as cases and percentages (%). The chi-square test was used for comparisons between groups. A value of P < 0.05 was considered to indicate a statistically significant difference.
Results
The cleaning levels of hospital environmental surfaces
To determine the cleaning levels of hospital environmental surfaces, we adopted fluorescent labeling and microbiological sampling methods to analyze the cleaning rate and qualification rate, respectively. The results analyzed by both methods showed consistency. Compared with the control group, the clearing levels of environmental surfaces (e.g. bed units, workbenches/computers, and switches) were significantly increased in the MDT intervention group. The clearing levels of door handles and handrails both showed a slight increase, but the difference did not reach statistical significance. (Tables 1 and 2).
Awareness of cleaning and disinfection knowledge among cleaners
A questionnaire survey was employed to evaluate the awareness of cleaning and disinfection knowledge among the cleaners and the qualified rate was calculated to reflect the level of awareness. After the MDT intervention, the qualified rates showed significant improvements in the following aspects: knowledge of the preparation and application of disinfectant solutions, usage methods of cleaning cloths, terminal disinfection methods for bed units, cleaning and disinfection methods for surfaces of objects contaminated with multi-drug resistant organisms, and the frequency of cleaning and disinfection (Table 3).
The misconduct problem in cleaning and disinfection
In this study, if visible stains or blood were detected on the surface of an object, it could be considered that the cleaner had committed misconduct in cleaning and disinfection. Misconduct rates were calculated to reflect the existing problems. After MDT intervention, the misconduct rate of environmental cleaning and disinfection was significantly decreased (Table 4).
The detection rate of multi-drug resistant organisms in in-hospital patients
Four types of multi-drug resistant organisms were used as indicators to refect the quality of cleaning and disinfection of hospital environmental surfaces in this study. After MDT intervention, the detection rates of carbapenem-resistant Enterobacteriaceae (CRE), methicillin-resistant Staphylococcus aureus (MRSA), carbapenem-resistant Acinetobacter baumannii (CRAB), or carbapenem-resistant Pseudomonas aeruginosa (CRPA) in in-hospital patients decreased from 9.84%, 32.19%, 73.27%, or 22.76–7.97%, 22.5%, 65.67%, or 16.74%, respectively. The differences were all statistically significant (Table 5).
The occurrence of HAIs
The HAI rate is one of the core indicators for measuring the level of infection prevention and control in medical institutions. Before the MDT intervention, the HAI rate in the whole hospital was 1.29%, and it was reduced to 0.88% after the intervention. The differences was statistically significant (Table 6).
Discussion
Initially, MDT primarily focused on the diagnosis and treatment of diseases, leveraging the advantages of interdisciplinary collaboration to enhance diagnostic accuracy21. As the demand for refined medical management increased, its scope gradually expanded to include hospital infection control22environmental cleaning, and disinfection23becoming an important model for optimizing hospital operational quality. In the management of hospital surface cleaning and disinfection, MDT integrates professional knowledge and practical experience to form a scientific and standardized management model. For example, infection control experts, determine the priority of cleaning and disinfection in high-risk areas such as operating rooms; environmental hygiene experts use their expertise to provide technical guidance on aspects like disinfectant composition, duration of action, and concentration ratios; clinical nursing teams, provide personalized cleaning needs for different departments; the property department coordinates the scheduling of cleaning personnel, equipment maintenance, and material supply, forming a comprehensive cleaning and disinfection execution network across the entire hospital24,25. This multi-dimensional collaborative management effectively improves the environmental cleanliness quality of hospitals and reduces the risk of infection caused by environmental factors26. In the current study, we applied the MTD model in the management of cleaning and disinfection of the hospital environmental surface and found the cleaning rate of hospital environmental surfaces was significantly increased and the detection rate of multi-drug resistant organisms and HAIs were remarkably decreased. Our findings are consistent with those from Yang Li who adopted27 bundled intervention measures to improve the cleaning and disinfection effect of environmental surfaces. Similarly, Katrina Browne and others28 improved the quality of environmental cleaning and disinfection through measures such as personnel training, system improvement, supervision and feedback, and adjustment of cleaning and disinfection methods. Studies confirmed that the MDT model could improve the quality of cleaning and disinfection of environmental surfaces and reduce the detection rate of multi-drug resistant organisms and incidence of HAIs, enhancing patients’ safety.
The current study includes several limitations: First, this is a pre-post intervention study with a non-randomized control group. For the control group, the study was conducted in the period ranging from November 2020 to March 2021, however, for the intervention group, the MDT model was employed to intervene the quality management of environmental surface cleaning and disinfection in the hospital from April 2021 to December 2022. Difference in study periods between control and intervention groups may introduce a potential seasonality bias that could invalidate the results. Second, we adopted the cleaning assessment methods using fluorescent labeling and visual inspection which may introduce subjective judgement of environmental surface cleaning and reduce the reliability of the data. In order to reduce this concern, we also conducted microbiological surface sampling in some experimental scenarios, which showed the consistency of results with methods of fluorescent labeling and visual inspection. Third, the number of cleaners surveyed differed between the control (n = 80) and intervention (n = 108) groups, which may represent a minor limitation. Fourth, while our study observed concurrent improvements in both surface cleanliness and reductions in infection rates, it was not designed to statistically establish a direct causal link between these two outcomes. Our study is limited by its single-hospital setting and relatively small sample size. Therefore, additional studies with larger samples conducted in diverse medical facilities are needed to confirm the effectiveness of the MDT model in the quality management of environmental surface cleaning and disinfection.
Conclusions
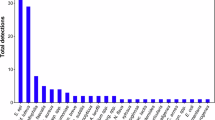
A great many studies demonstrated that hospital cleaning staff manifested an acceptable level of cognition regarding environmental cleaning and disinfection while their compliance with disinfection protocols remained relatively low. This study applied the MDT model to manage the cleaning and disinfection of hospital environmental surface, which improved the hospital’s infection management level and effectively reduced the occurrence of HAIs. The MDT model, which includes multi-department collaboration, change of training strategies, strengthened supervision, and optimized operation procedures, shows promising potential in the management of cleaning and disinfection of environmental surface (Fig. 1).
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- MDT:
-
Multidisciplinary Team
- HAIs:
-
Hospital-Acquired Infections
- CRE:
-
Carbapenem-Resistant Enterobacteriaceae
- MRSA:
-
Methicillin-Resistant Staphylococcus Aureus
- CRAB:
-
Carbapenem-Resistant Acinetobacter Baumannii
- CRPA:
-
Carbapenem-Resistant Pseudomonas Aeruginosa
- CBL:
-
Case-Based Learning
References
Protano, C., Cammalleri, V., Spica, R., Valeriani, V., Vitali, M. & F. & Hospital environment as a reservoir for cross transmission: cleaning and disinfection procedures. Annali Di Igiene: Med. Preventiva E Di Comunita. 31, 436–448. https://doi.org/10.7416/ai.2019.2305 (2019).
Yano, R. et al. Diversity changes of microbial communities into hospital surface environments. J. Infect. Chemother. 23, 439–445. https://doi.org/10.1016/j.jiac.2017.03.016 (2017).
Boev, C. & Kiss, E. Hospital-Acquired infections: current trends and prevention. Crit. Care Nurs. Clin. N. Am. 29, 51–65. https://doi.org/10.1016/j.cnc.2016.09.012 (2017).
Liu, J. Y., Dickter, J. K. & Nosocomial Infections A history of Hospital-Acquired infections. Gastrointest. Endosc. Clin. N. Am. 30, 637–652. https://doi.org/10.1016/j.giec.2020.06.001 (2020).
Klevens, R. M. et al. Estimating health care-associated infections and deaths in U.S. Hospitals, 2002. Public. Health Rep. (Washington D C : 1974). 122, 160–166. https://doi.org/10.1177/003335490712200205 (2007).
Silvestri, L. & van Saene, H. K. Hospital-acquired infections due to gram-negative bacteria. N. Engl. J. Med. 363, 1482. https://doi.org/10.1056/NEJMc1006641 (2010). author reply 1483-1484.
RD, S. The direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. (2009).
Anderson, D. J. et al. Enhanced terminal room disinfection and acquisition and infection caused by multidrug-resistant organisms and Clostridium difficile (the benefits of enhanced terminal room disinfection study): a cluster-randomised, multicentre, crossover study. Lancet 389, 805–814. https://doi.org/10.1016/s0140-6736(16)31588-4 (2017).
Lei, J. et al. Extensively drug-resistant Acinetobacter baumannii outbreak cross-transmitted in an intensive care unit and respiratory intensive care unit. Am. J. Infect. Control. 44, 1280–1284. https://doi.org/10.1016/j.ajic.2016.03.041 (2016).
Ng, Q. X. et al. Impact of COVID-19 on environmental services workers in healthcare settings: a scoping review. J. Hosp. Infect. 130, 95–103. https://doi.org/10.1016/j.jhin.2022.09.001 (2022).
Pan, Y. et al. The application of MDT model for calciphylaxis management in patients with end-stage renal disease. Int. Wound J. 20, 3717–3723. https://doi.org/10.1111/iwj.14265 (2023).
Keller, D. S., Berho, M., Perez, R. O., Wexner, S. D. & Chand, M. The multidisciplinary management of rectal cancer. Nat. Rev. Gastroenterol. Hepatol. 17, 414–429. https://doi.org/10.1038/s41575-020-0275-y (2020).
Brennan, F., Gardiner, M. D. & Narasimhan, M. The neuropalliative multidisciplinary team-Members and their roles. Handb. Clin. Neurol. 190, 33–59. https://doi.org/10.1016/b978-0-323-85029-2.00010-5 (2022).
Staudt, M. D. The multidisciplinary team in pain management. Neurosurg. Clin. N Am. 33, 241–249. https://doi.org/10.1016/j.nec.2022.02.002 (2022).
Song, Y. et al. Geriatrician-led multidisciplinary team management improving polypharmacy among older inpatients in China. Front. Pharmacol. 14, 1167306. https://doi.org/10.3389/fphar.2023.1167306 (2023).
Lu, C. Analysis of the effectiveness of multi-disciplinary team integrated management combined with full-media health education intervention in patients with coronary heart disease and diabetes mellitus. Biotechnol. Genet. Eng. Rev. 40, 2745–2759. https://doi.org/10.1080/02648725.2023.2202518 (2024).
Teare, L. et al. Acinetobacter - the Trojan horse of infection control? J. Hosp. Infect. 102, 45–53. https://doi.org/10.1016/j.jhin.2018.12.013 (2019).
Donkin, R., Yule, H. & Fyfe, T. Online case-based learning in medical education: a scoping review. BMC Med. Educ. 23 https://doi.org/10.1186/s12909-023-04520-w (2023).
Fattorini, M. et al. Use of a fluorescent marker for assessing hospital bathroom cleanliness. Am. J. Infect. Control. 44, 1066–1068. https://doi.org/10.1016/j.ajic.2016.03.030 (2016).
Xiaoyang Zhang, J. H., Wang, C. & Zhang, L. Survey on the status of knowledge, attitudes and behaviors of environmental surface cleaning and disinfection of hospital cleaners. Chin. J. Disinfection. 39, 928–931 (2022). (in Chinese).
Brown, G. T. F., Bekker, H. L. & Young, A. L. Quality and efficacy of multidisciplinary team (MDT) quality assessment tools and discussion checklists: a systematic review. BMC cancer. 22, 286. https://doi.org/10.1186/s12885-022-09369-8 (2022).
O’Donnell, M. et al. Expanding the team: optimizing the multidisciplinary management of drug Use-Associated infective endocarditis. J. Gen. Intern. Med. 37, 935–939. https://doi.org/10.1007/s11606-021-07313-3 (2022).
Miller, R., Simmons, S., Dale, C., Stachowiak, J. & Stibich, M. Utilization and impact of a pulsed-xenon ultraviolet room disinfection system and multidisciplinary care team on Clostridium difficile in a long-term acute care facility. Am. J. Infect. Control. 43, 1350–1353. https://doi.org/10.1016/j.ajic.2015.07.029 (2015).
Garcia, R. A. et al. Multidisciplinary team review of best practices for collection and handling of blood cultures to determine effective interventions for increasing the yield of true-positive bacteremias, reducing contamination, and eliminating false-positive central line-associated bloodstream infections. Am. J. Infect. Control. 43, 1222–1237. https://doi.org/10.1016/j.ajic.2015.06.030 (2015).
Silva, E. et al. Health care for people with tuberculosis/hiv co-infection from the multidisciplinary team’s perspective. Revista Brasileira De Enfermagem. 76, e20220733. https://doi.org/10.1590/0034-7167-2022-0733 (2023).
Opperman, C. J., Khan, F., Piercy, J. L. & Samodien, N. Barriers to disinfection of mobile touch screen devices amongst a multidisciplinary team in intensive care units at a tertiary hospital. Germs 11, 329–336. https://doi.org/10.18683/germs.2021.1270 (2021).
Li, Y. et al. Impact of environmental cleaning on the colonization and infection rates of multidrug-resistant Acinetobacter baumannii in patients within the intensive care unit in a tertiary hospital. Antimicrob. Resist. Infect. Control. 10 https://doi.org/10.1186/s13756-020-00870-y (2021).
Browne, K. et al. A randomised controlled trial investigating the effect of improving the cleaning and disinfection of shared medical equipment on healthcare-associated infections: the cleaning and enhanced disinfection (CLEEN) study. Trials 24, 133. https://doi.org/10.1186/s13063-023-07144-z (2023).
Author information
Authors and Affiliations
Contributions
SX, AS, and HW conducted the intervention in the cleaning and disinfection of environmental surfaces in the hospital. HZ conceived the study design. LL analyzed the data.YZ and GW were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, S., Sun, A., Wang, H. et al. Enhancing the quality management of hospital environmental surfaces through the application of a multidisciplinary team model. Sci Rep 15, 23035 (2025). https://doi.org/10.1038/s41598-025-08823-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08823-4