Abstract
Metastatic differentiated thyroid cancer (mDTC) can exhibit aggressive growth and disseminate to distant organs, thereby reducing survival rates. The benefits of primary tumor resection (PTR) for patients with mDTC are still debated. In this study, we utilized the Surveillance, Epidemiology, and End Results (SEER) database to evaluate mDTC patients, focusing on the impact of organ-specific metastases and the number of metastatic sites on prognosis, as well as the potential efficacy of PTR as a therapeutic intervention. 904 patients with mDTC at initial diagnosis from 2010 to 2015 were studied. Lung and bone were the most common sites of metastasis. Patients with brain, lung and liver metastasis had significantly worse overall survival (OS) (all p < 0.05) and cancer-specific survival (CSS) (all p < 0.05). Among all the patients, 550 (60.84%) underwent PTR, which was associated with reduced risk of overall mortality (OM) and cancer-specific mortality (CSM) (all p < 0.05). When analyzing different metastatic patterns, PTR significantly lowered the risk of OM and CSM for patients with bone, brain, lung, liver, or distant lymph node (DLN) involvement (all p < 0.05). Surgical resection also improved OS and CSS (both p < 0.05) in patients with multiple organ involvement or one/two metastases. Our findings suggest that PTR may confer benefits to select individuals with metastatic DTC. To validate these results and facilitate their integration into clinical practice, multicenter prospective studies are warranted.
Similar content being viewed by others
Introduction
Differentiated thyroid carcinoma (DTC), originating from aberrant follicular cells, generally demonstrates indolent growth and carries a favorable prognosis, accounting for more than 90% of all thyroid cancers globally1,2. The utilization of advanced ultrasonographic techniques and fine needle aspiration biopsy (FNAB) has resulted in the increased detection of thyroid cancer at early stages, particularly papillary thyroid microcarcinoma. Nevertheless, a subset of DTC patients (approximately 1–10%) present with distant metastases at the time of initial diagnosis, which is considered to be the leading cause of DTC-related mortality3,4,5. Those individuals with distant metastases experience a significantly poorer prognosis, with 10-year survival rates ranging from 30 to 80%6,7,8.
The association between primary tumor resection (PTR) and improved survival outcomes has been demonstrated in various metastatic solid tumors such as breast cancer, lung cancer, and colorectal cancer9,10,11. However, further evidence is required to elucidate the specific benefits of PTR for patients with distant metasta.
ses from DTC and to identify subgroups with distinct metastatic patterns.
Therefore, this study employed population-based data from the Surveillance, Epidemiology, and End Results (SEER) database to evaluate the prognostic significance of site-specific metastases and varying numbers of metastases. It also analyzed the roles played by PTR in treatment, and sought to identify optimal candidates for PTR among patients with mDTC.
Materials and methods
Data sources
Data from 904 patients initially diagnosed with mDTC were derived from the SEER program of the National Cancer Institute. The SEER program is a population-based cancer registry system collecting data from 18 cancer registries across the United States of America, covering approximately 28% of incident cases of the whole country. This online program collects patient information and provides comprehensive details on diagnosis, demographics, tumor characteristics, initial treatment, and follow-up for vital status. The protocol for this study was approved by the Ethics Committee of Chengdu Fifth People’s Hospital (The Second Clincal Medical College, Affiliated Fifth People’s Hospital of Chengdu University of Traditional Chinese Medicine). As the SEER database was publicly accessible, the present study did not require informed patient consent.
Patient selection
We extracted the clinicopathological characteristics of patients with papillary thyroid carcinoma (PTC, ICD-O-3 codes 8050/3, 8260/3, 8341/3, 8342/3, 8343/3, and 8344/3), follicular thyroid carcinoma (FTC, ICD-O-3 codes 8330/38331/3, and 8335/3), and follicular variant of papillary carcinoma (PTCF, ICD-O-3 codes 8340/3) in SEER database. The inclusion criteria were: (i) primary DTC patients with distant metastasis at initial diagnosis (ii) DTC as the first primary cancer; (iii) diagnosis between 2010 and 2020, as detailed information on metastatic sites was not available before 2010, and the cut-off follow-up year of the latest released SEER data was 2020. The exclusion criteria are as follows: (i) patients with imcomplete follow-up information; (ii) patients with other primary cancers; (iii) according to “ICD-O-3 Hist/behav, malignant”, patients with undifferentiated pathological type; (iv) patients with unknown cause of death; (v) patients with staging T0, Tx, Nx and survival time of 0 months.
Evaluation of variables clinicopathological variable assessment
Variables, encompassing demographics (age at diagnosis, sex, race), tumor features (tumor grade, tumor size, regional lymph node status, and metastatic status in lung, bone, liver, brain and distant lymph node (DLN), along with the number of involved organs) as well as treatment details (procedures like PTR, neck dissection, and interventions like radiation, chemotherapy) were gathered from the SEER database. The rationale for including metastatic status for the specific five sites (lung, bone, liver, brain, and DLN) in the analyses was that the SEER program exclusively provides information on distant metastasis for these organs. We obtained survival information from the following options: “Vital status recodes”, “SEER cause-specific death classification”, and “Survival months”. Overall survival (OS) and cancer-specific survival (CSS) was selected as the primary end point. PTR was defined as cancer-direct surgery on the primary site, excluding procedures such as photodynamic therapy, cryosurgery, electrocautery and excisional biopsy.
Statistical analysis
The research group was divided into two groups based on therapy, PTR versus non-PTR. Differences in categorical variables were compared by using the Chi-square test and Fisher’s exact test, while that in continuous variables were compared using Student’s t-test. OS and CSS were estimated.
by the Kaplan-Meier method and compared with the log-rank test. Univariable and multivariable Cox proportional hazard regression was used to determine independent prognostic factors, with hazard ratios (HR) and 95% confidence intervals (95%CI).
For the statistical analyses, we employed IBM SPSS Statistics 24.0 (IBM Corporation, Armonk, NY, USA) and R Studio version 4.3.0 software (The R Foundation for Statistical Computing, Austria, Vienna). A p value less than 0.05 was considered to have statistical significance.
Results
Baseline demographic and clinicopathological characteristics
Our study comprised a total of 904 patients initially diagnosed with mDTC. The mean age at diagnosis was 63.23 ± 17.50 years old. Female patients (n = 501, 55.42%) slightly outnumbered male patients (n = 403, 44.58%). Tumor characteristics, including T stage, N stage and status of metastases, were detailed in Table 1 as well.
Among these patients, PTR was conducted in over half of the total cases (n = 550, 60.84%). Table 1 presented the baseline characteristics for both PTR and non-PTR groups, as well as statistically significant correlations between some characteristics and the status of PTR.
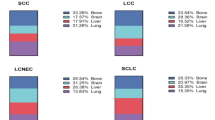
Different metastatic patterns in the overall cohort
Table 1 provided a summary of information on distant metastatic organs in different patients. To visually illustrate the distribution of metastatic organs, a Venn diagram was employed (Fig. 1). The most frequent metastatic sites were lung (n = 657, 72.68%) and bone (n = 358, 39.60%). Brain metastasis was diagnosed in 61 (6.75%) patients, while 61 (6.75%) patients had liver metastasis, and 36 (5.4%) patients had DLN metastasis. Overall, 683 (75.55%), 184 (20.35%), 33 (3.65%), and 4 (0.44%) patients had one, two, three, and four metastatic organs, respectively. The Venn diagram’s overlapping areas depicted the detailed metastatic sites for patients with more than one organ metastasis. Particularly, no patients in our cohort were found to have metastases in all five organs.
Impact of metastatic patterns on survival outcomes
We conducted separate comparisons of OS and CSS outcomes among patients with various metastatic organs. Kaplan-Meier analyses revealed that patients with brain, liver, and lung metastasis exhibited significantly worse survival outcomes compared to those without corresponding involvement (all p < 0.05 for both OS and CSS). Conversely, for bone and DLN involvement, no substantial survival differences were observed between patients with or without these organ metastases (all p > 0.05 for both OS and CSS) (Supplemental Figure S1).
The analysis extended to evaluate the impact of the number of distant metastatic organs on patients’ prognosis. Results indicated that patients with varying numbers of metastatic organs exhibited OS and CSS differences. In detail, patients with single-organ metastasis demonstrated a significantly better survival advantage than those with more than two metastases (p < 0.001), impacting both OS and CSS. Morever, the hazard ratio (HR) for overall mortality (OM) and cancer-specific mortality (CSM) increases progressively in conjunction with the number of distant metastatic organs (Supplemental Figure S2, Supplemental Table S1 and S2).
In the univariable Cox analysis, brain, liver, lung metastasis, but not involvements of other metastatic organs, emerged as an independent prognostic factor for unfavorable overall and cancer-specific survival. Whereas, it was not correlated with OS or CSS when further adjusted in the multivariable Cox analysis. Simiarly, multi-organ metastases were independent predictor for poor survival compared with single-organ metastasis in the univariable Cox analysis. However, it was not correlated with OS or CSS when further adjusted in the multivariable Cox analysis (Supplemental Table S1 and S2).
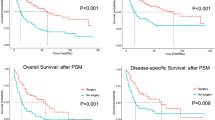
Prognostic value of PTR in the overall cohort
The impact of PTR on OS and CSS was evaluated in the entire cohort of 904 patients. The log-rank test conducted for the overall patients revealed a significant association between PTR and improved OS and CSS (both log-rank p < 0.001) (Fig. 2). As outlined in Supplemental Table S1 and S2, PTR served as a favorable predictor for both OS and CSS after further adjusting for other covariables in the multivariable regression (PTR vs. non-PTR, HR: 0.36, 95% CI: 0.27–0.47, p < 0.001 for OS; HR: 0.34, 95%CI: 0.25–0.46, p < 0.001 for CSS).
Optimal candidates for undergoing PTR in patients with mDTC
Survival analyses were conducted among patients with site-specific metastases. Kaplan-Meier estimates and log-rank tests revealed that prognostic effect of PTR varied depending on the involved sites. PTR conferred a significant survival benefit for patients with bone (log-rank p < 0.001 for both OS and CSS), brain (log-rank p < 0.001 for both OS and CSS), DLN (log-rank p = 0.007 for OS; log-rank p = 0.021 for CSS), liver (log-rank p < 0.001 for both OS and CSS) and lung metastases (log-rank p < 0.001 for both OS and CSS) (Fig. 3).
For patients with one metastasis, those who received surgical resection of the primary tumor were significantly associated with better OS and CSS (both p < 0.001), irrespective of the specific metastatic organs (Fig. 4A and B). This survival advantage persisted in patients with two organ metastases (log-rank p < 0.001 for both OS and CSS) (Fig. 4C and D). In patients with more than two metastatic organs, however, the surgery did not appear to bring any improvement of survival (both OS and CSS: p > 0.05) (Fig. 4E, F, G and H).
Subgroup multivariable Cox analyses also yielded similar conclusions. The HR and 95% CI for PTR versus non-PTR of each metastatic site were summarized in forest plots (Fig. 5). Surgical resection to the primary tumor independently predicted lower OM and CSM in patients with bone (PTR vs. non-PTR, HR: 0.28, 95%CI: 0.21–0.36 for OM; HR: 0.27, 95%CI: 0.20–0.37 for CSM), brain (PTR vs. non-PTR, HR: 0.24, 95%CI: 0.13–0.46 for OM; HR: 0.24, 95%CI: 0.12–0.46 for CSM), liver (PTR vs. non-PTR, HR: 0.30, 95%CI: 0.16–0.58 for OM; HR: 0.33, 95%CI: 0.17–0.65 for CSM), lung (PTR vs. non-PTR, HR: 0.22, 95%CI: 0.18–0.27 for OM; HR: 0.23, 95%CI: 0.18–0.28 for CSM) and DLN metastases (HR: 0.31, 95%CI: 0.12–0.77 for OM; HR: 0.35, 95%CI: 0.14–0.90 for CSM). A decreased risk of death was also observed in patients with one or two metastases who received PTR (for one metastasis: HR: 0.20, 95%CI: 0.16–0.25 for OM; HR: 0.19, 95%CI: 0.15–0.24 for CSM; for two metastases: HR: 0.35, 95%CI: 0.25–0.50 for OM; HR: 0.39, 95%CI: 0.27–0.57 for CSM). However, PTR didn’t show any survival advantage in patients with more than two metastases.
Discussion
The presentation of metastatic differentiated thyroid cancer (mDTC) often manifests as mass-forming lesions, frequently involving cervical lymph nodes or distant organs, with concurrent multi-organ involvement being a frequent occurrence7,12. Our research findings indicate that the lung and bone are the most prevalent sites of metastasis in mDTC, aligning with existing literature13,14. The metastatic patterns observed in mDTC, as illustrated in Figs. 2 and 3, were also identified as prognostic indicators. Given the significant metastatic diversity in mDTC, the optimal management strategies for patients with mDTC still remain controversial. The potential beneficial impact of PTR on survival outcomes in mDTC patients, as observed in other cancer types15,16,17, warrants further investigation.
This study represents a pioneering examination of the therapeutic implications of PTR in mDTC patients, utilizing the largest cohort from the SEER database. Notably, we assessed the prognostic implications of PTR in various patient subgroups, offering valuable insights for identifying individuals who may benefit from primary tumor surgery.
Our study, which utilized the SEER database to investigate survival outcomes in patients with DTC initially diagnosed with metastases, demonstrated significant improvements in both OS and CSS among individuals who underwent PTR. The results indicate that patients with mDTC may benefit from PTR, particularly for those with solitary metastases to the lung, bone, liver, brain, or DLN. Additionally, patients with involvement of one or two organs may experience favorable survival outcomes following surgery. Conversely, PTR did not result in better OS or CSS in those with mDTC presenting multiple (three or four) metastatic organs. This observation aligns with the widely recognized clinical finding that individuals with mDTC affecting multiple organs often exhibit rapid systemic disease progression and derive limited benefit from surgical intervention8,18.
The prognostic significance of various metastatic locations in mDTC remains a topic of debate. Accurately assessing the risk stratification of these patients is of great clinical importance. Our research revealed that patients with metastases in multiple sites exhibit the poorest prognosis. This prognostic data is valuable for patient counseling and can aid clinicians in determining appropriate local or systemic treatment options. Patients at high risk may be eligible for participation in upcoming clinical trials investigating novel targeted therapies.
While multikinase inhibitors (MKIs) have greatly improved the prognosis of patients with advanced DTC in recent years, regulatory approval for targeted drugs in mDTC remains limited19,20. However, it is imperative to acknowledge that the use of certain drugs is limited to patients with radioactive iodine-refractory (RAI-R) DTC, and their effectiveness is influenced by the specific tumor subtype. Additionally, the development of resistance to both specific and multikinase inhibitors presents a significant challenge in the management of DTC21. Consequently, surgical resection remains a preferred treatment option for patients with mDTC.
The 2015 guidelines from the American Thyroid Association (ATA) advocate for the administration of radioactive iodine (RAI) therapy following PTR in patients with mDTC to improve prognosis2. Consequently, PTR is a crucial precursor to RAI therapy, exerting a substantial influence on the survival outcomes of individuals with mDTC. These primary lesions frequently invade adjacent anatomical structures, leading to complications such as airway obstruction and respiratory insufficiency, which are the most common fatal conditions22,23. Hence, local decompression via PTR may have a significant impact on extending the survival of patients with mDTC who are undergoing surgery. Additionally, several hypotheses have been proposed to elucidate the prognostic significance of PTR. Insights from studies on breast cancer suggest that the primary tumor may be associated with elevated levels of circulating tumor cells (CTCs) that contribute to distant metastases, and therefore reducing CTCs through PTR may improve survival outcomes24,25. Previous research has also linked PTR to enhanced immune function in metastatic colorectal cancer, potentially contributing to better clinical outcomes26,27.
Patients with mDTC generally have a worse prognosis and shorter survival, with no standardized treatment protocols, especially regarding the debated benefit of PTR. Our study identifies the lungs, bones, brain, liver, and distant lymph nodes as primary metastatic sites and suggests that resecting the primary tumor is beneficial when metastases are limited to two sites.
Our study is the first to show that survival outcomes for patients with mDTC vary based on organ-specific metastases and the number of metastatic sites. PTR may benefit certain individuals, offering a more accurate survival assessment for mDTC patients in clinical research. The study’s strengths include a large cohort, comprehensive treatment data, and detailed survival analysis by metastasis location. Notably, even patients with brain metastases who underwent PTR showed improved survival, challenging the idea that such cases should be managed palliatively rather than with aggressive tumor removal28,29.
Acknowledging limitations in our study is crucial. Firstly, the SEER database is lacking important information, such as incomplete data on radioactive iodine treatment and chemotherapy regimen details. Secondly, the SEER database only covers five main specific organs of metastases, excluding patients with other types of metastases like adrenal glands, pancreas, kidney, or peritoneum. Lastly, the retrospective nature of the SEER database is a significant limitation, highlighting the necessity for future prospective research.
Conclusions
Ultimately, the results of this population-based study indicate that surgical excision of the primary tumor may enhance survival outcomes for patients with mDTC who meet specific criteria. The study delineated ideal candidates for PTR as those with singular involvement of bone, lung, liver, brain, or DLN, or involvement in one or two organs.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cabanillas, M. E., McFadden, D. G. & Durante, C. Thyroid Cancer. Lancet 10061, 2783–2795 (2016).
Haugen, B. R. et al. 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid Cancer. Thyroid 1, 1–133 (2016).
Hirsch, D. et al. Long-Term outcomes and prognostic factors in patients with differentiated thyroid Cancer and distant metastases. Endocr. Pract. 10, 1193–1200 (2017).
Leite, A. et al. Deaths related to differentiated thyroid cancer: A rare but real event. Arch. Endocrin Metab. 3, 222–227 (2017).
Sohn, S. Y. et al. Prognostic indicators of outcomes in patients with lung metastases from differentiated thyroid carcinoma during Long-Term Follow-Up. Clin. Endocrinol. 2, 318–326 (2018).
Lee, J. & Soh, E. Y. Differentiated thyroid carcinoma presenting with distant metastasis at initial diagnosis clinical outcomes and prognostic factors. Ann. Surg. 1, 114–119 (2010).
Haq, M. & Harmer, C. Differentiated thyroid carcinoma with distant metastases at presentation: prognostic factors and outcome. Clin. Endocrinol. 1, 87–93 (2005).
Vuong, H. G., Le, M. K., Hassell, L., Kondo, T. & Kakudo, K. The differences in distant metastatic patterns and their corresponding survival between thyroid Cancer subtypes. Head Neck-J Sci. Spec. 4, 926–932 (2022).
Leone, N. et al. Colorectal Cancer with synchronous unresectable liver metastases: resecting the primary tumor improves survival. Int. J. Colorectal Dis. 1, 169 (2023).
Vohra, N. A., Brinkley, J., Kachare, S. & Muzaffar, M. Primary tumor resection in metastatic breast cancer: A Propensity-Matched analysis, 1988–2011 SEER data base. Breast J. 4, 549–554 (2018).
Rodriguez-Quintero, J. H. et al. Resection of the primary tumor and survival in patients with Single-Site synchronous oligometastatic Non-Small cell lung cancer: Propensity-Matched analysis of the National Cancer database. J. Am. Coll. Surg. 6, 1122–1136 (2024).
Shoup, M. et al. Prognostic indicators of outcomes in patients with distant metastases from differentiated thyroid carcinoma. J. Am. Coll. Surg. 2, 191–197 (2003).
Sugino, K. et al. Prognosis and prognostic factors for distant metastases and tumor mortality in follicular thyroid carcinoma. Thyroid 7, 751–757 (2011).
Sugitani, I., Fujimoto, Y. & Yamamoto, N. Papillary thyroid carcinoma with distant metastases: survival predictors and the importance of local control. Surgery 1, 35–42 (2008).
Shi, X. et al. Prognostic significance and optimal candidates of primary tumor resection in major salivary gland carcinoma patients with distant metastases at initial presentation: A Population-Based study. Oral Oncol. 78, 87–93 (2018).
Xiao, W. et al. Primary tumor resection in stage IV breast cancer: A systematic review and Meta-Analysis. Ejso-Eur J. Surg. Onc. 10, 1504–1512 (2018).
Zheng, M., Li, Y., Li, T., Zhang, L. & Zhou, L. Resection of the primary tumor improves survival in patients with Gastro-Entero-Pancreatic neuroendocrine neoplasms with liver metastases: A SEER-Based analysis. Cancer Med-Us. 11, 5128–5136 (2019).
Wang, L. Y. et al. Multi-Organ distant metastases confer worse Disease-Specific survival in differentiated thyroid Cancer. Thyroid 11, 1594–1599 (2014).
Brose, M. S. et al. Multikinase inhibitors for the treatment of asymptomatic radioactive Iodine-Refractory differentiated thyroid cancer: global noninterventional study (RIFTOS MKI). Thyroid 9, 1059–1068 (2022).
Jing, R. et al. Efficacy and safety of multikinase inhibitors for patients with refractory thyroid cancer: systematic review and network Meta-Analysis. J Clin. Endocr. Metab. 109(10), 2658–2672 (2024).
Shen, H. et al. Radioiodine-Refractory differentiated thyroid cancer: molecular mechanisms and therapeutic strategies for radioiodine resistance. Drug Resist. Update 72, 101013 (2024).
Kitamura, Y. et al. Immediate causes of death in thyroid carcinoma: clinicopathological analysis of 161 fatal cases. J. Clin. Endocr. Metab. 11, 4043–4049 (1999).
Beasley, N. J., Walfish, P. G., Witterick, I. & Freeman, J. L. Cause of death in patients with Well-Differentiated thyroid carcinoma. Laryngoscope 6, 989–991 (2001).
Mu, Z. et al. Prospective assessment of the prognostic value of Circulating tumor cells and their clusters in patients with Advanced-Stage breast Cancer. Breast Cancer Res. Tr. 3, 563–571 (2015).
Budd, G. T. et al. Circulating tumor cells versus Imaging–Predicting overall survival in metastatic breast Cancer. Clin. Cancer Res. 21, 6403–6409 (2006).
Anwar, S., Peter, M. B., Dent, J. & Scott, N. A. Palliative excisional surgery for primary colorectal Cancer in patients with incurable metastatic disease. Is there a survival benefit?? A systematic review. Colorectal Dis. 8, 920–930 (2012).
Kim, M. S. et al. Prognostic factors predicting survival in incurable stage IV colorectal Cancer patients who underwent palliative primary tumor resection. Retrospective cohort study. Int. J. Surg. 49, 10–15 (2018).
Yoo, J., Kim, H. J., Kim, S. M. & Park, H. H. Prognostic factors to predict the efficacy of surgical interventions against brain metastasis secondary to thyroid Cancer. Eur. Thyroid J. 11(5) (2022).
Saito, F. et al. Prognosis after brain metastasis from differentiated thyroid carcinoma. World J. Surg. 3, 574–581 (2016).
Funding
This work received financial support from the Chengdu High-level Key Clincal Specialty Construction Projiect.
Author information
Authors and Affiliations
Contributions
(I) Conception and design: JQ Dan, JH Huang; (II) Data curation: JY Tan, X Lu: JD; (III) Formal analysis: JQ Dan, RX Tang; (IV) Funding acquisition: Y Guo, ZY Yuan; (V) Methodology: JY Li, Y Leng; (VI) Manuscript writing: JD, JT; (VII) Final approval of manuscript: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement and consent to participate
The protocol for this study was approved by the Ethics Committee of Chengdu Fifth People’s Hospital (The Second Clincal Medical College, Affiliated Fifth People’s Hospital of Chengdu University of Traditional Chinese Medicine). As the SEER database was publicly accessible, the present study did not require informed patient consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.


Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dan, J., Tan, J., Guo, Y. et al. Survival benefits of primary tumor resection in metastatic differentiated thyroid cancer: an analysis of SEER data. Sci Rep 15, 21932 (2025). https://doi.org/10.1038/s41598-025-08845-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-08845-y