Abstract
This cross-sectional observational study involved 1052 non-pregnant women aged 18–65 who had undergone TCC and sought care at a tertiary-level gynecology clinic. We documented participants’ medical histories, Pap smear results, and TCC histories. Pap smear results were analyzed using the 2014 Bethesda classification, and obstetric outcomes, including pregnancies, deliveries, miscarriages, and preterm births (PTD), were evaluated. Data analysis was performed using SPSS 22.0, with statistical significance set at p < 0.05. This cross-sectional observational study involved 1052 non-pregnant women aged 18–65 who had undergone TCC and sought care at a tertiary-level gynecology clinic. We documented participants’ medical histories, Pap smear results, and TCC histories. Pap smear results were analyzed using the 2014 Bethesda classification, and obstetric outcomes, including pregnancies, deliveries, miscarriages, and preterm births (PTD), were evaluated. Data analysis was performed using SPSS 22.0, with statistical significance set at p < 0.05. The mean age of participants was 34.4 ± 7.4 years. Abnormal Pap smear results were observed in 11.5% of patients, with a higher prevalence (29.9%) among those who underwent TCC within the last year. The frequency of TCC was inversely related to the rate of abnormal smear results (p < 0.005). However, frequent TCC procedures were associated with significantly increased rates of abortion (18.9%) and PTD (10.3%) (both p < 0.005). While the time elapsed since the last TCC procedure influenced abortion and PTD rates, both were statistically significant (p = 0.016 and p = 0.029, respectively). TCC is associated with a higher incidence of cervical abnormalities and adverse pregnancy outcomes, particularly when performed more frequently. These findings suggest a potential link between TCC and disruptions in cervical health, which may increase the risk of pregnancy complications, underscoring the need for cautious use and further research. Educating communities about the potential risks and advocating for safer medical practices are crucial steps towards improving gynecological and obstetric care in regions where TCC is still prevalent.
Similar content being viewed by others
Introduction
Traditional cervical cauterization (TCC) represents a long-standing medical practice, where heated instruments, such as metal rods or wooden sticks, are applied to the cervix to address various gynecological issues. This method, with roots dating back to at least 2500 BCE, has been documented across diverse regions including China, the Middle East, and Africa, and continues to be utilized in places with limited access to modern medical care, such as Somalia1. TCC is typically performed by traditional healers or non-medical individuals in non-clinical settings. The procedure generally involves heating a metal rod or wooden stick over an open flame and applying it directly to the cervix without the use of anesthesia or sterile conditions. The method lacks standardization, and the intensity, duration, and area of application can vary widely depending on the practitioner’s technique. Such practices are often carried out in rural or underserved communities where modern gynecological care is inaccessible2. Despite its historical and cultural significance, a notable deficiency remains in the scientific understanding of the cellular and macroscopic effects of TCC on cervical health. While the use of TCC is prevalent in areas lacking advanced healthcare infrastructure, the biological impact of this traditional practice on cervical tissues is inadequately explored in contemporary medical literature. TCC is frequently employed in regions like Somalia to manage conditions such as vaginal infections, pelvic pain, and infertility, yet it involves the application of uncontrolled thermal trauma to the cervix3. This practice, although widespread, is conducted without the rigor of modern hygiene standards or precise thermal control, leading to potential disturbances in the cervix’s microenvironment. Existing research has indicated that such thermal injury can disrupt the delicate balance of the cervical microbiome, alter secretions, damage cellular structures, and compromise connective tissue integrity, thus impeding the natural healing process4.
However, the specific consequences of TCC on cervical cytology and the broader implications for long-term cervical health have not been thoroughly investigated. Alterations in the microenvironment of the vagina and cervix can stimulate cervical lesions and carcinogenesis5. The Bethesda classification system, widely used for reporting cervical cytology, categorizes Pap smear results into several categories including Normal, Atypical Squamous Cells (ASC), Low-Grade Squamous Intraepithelial Lesion (LSIL), High-Grade Squamous Intraepithelial Lesion (HSIL), and Squamous Cell Carcinoma (SCC)6. Despite the utility of this classification system, the impact of TCC on these categories remains unclear, creating a significant gap in the literature. Furthermore, cervical insufficiency, a condition associated with disruptions in cervical structure, can lead to adverse pregnancy outcomes including preterm labor and miscarriage7. Disruptions in innate immunity can also contribute to preterm labor8.
In Somalia, traditional cervical cauterization (TCC) is commonly utilized for gynecological concerns such as vaginal infections, pelvic pain, and infertility. TCC is typically performed by non-healthcare individuals, without proper hygiene conditions. Despite the widespread use of TCC, there is a notable lack of studies elucidating this procedure’s cellular and macroscopic effects on the cervix. The application of uncontrolled thermal trauma to the cervix during TCC can disrupt the balance of the cervical microbiome, alter secretions, damage cellular elements, and impact the integrity of connective tissue, potentially delaying the healing process. Furthermore, the involvement of bacterial taxa such as Proteobacteria and Actinobacteria in proinflammatory processes within the vagina and cervix suggests a potential link between these microorganisms and the inflammatory response following traditional cauterization9. These disruptions may contribute to the high incidence of cervicovaginal smear abnormalities observed in regions where TCC is practiced.
This study aims to address these gaps by investigating the cellular changes and pregnancy outcomes associated with TCC. By evaluating the prevalence of cervical abnormalities and the incidence of adverse pregnancy outcomes among women who have undergone TCC, this research seeks to provide a comprehensive understanding of the potential risks and long-term effects of this traditional practice. Such insights are essential for informing health interventions and public health strategies in regions where TCC remains prevalent, ultimately contributing to improved gynecological and obstetric care.
Materials and methods
Search strategy and selection criteria
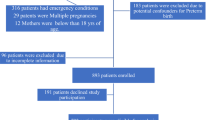
This cross-sectional observational study was conducted at a tertiary-level gynecology and obstetrics clinic to assess the effects of traditional cervical cauterization (TCC) on cervical cellular changes and pregnancy outcomes. Non-pregnant women aged 18–65 who sought care at the clinic between 01.11.2021 and 31.12.2022 were eligible for participation. Participants were recruited through a combination of clinic-based recruitment and community outreach. Informed consent was obtained from all participants prior to inclusion in the study. The inclusion criteria for the study required participants to be women aged 18–65 years who had a documented history of Traditional Cervical Cauterization (TCC) and were actively seeking gynecological care at the clinic. Conversely, the exclusion criteria encompassed pregnant women, individuals with a history of cervical surgery or other medical interventions that might affect the cervix, and those with incomplete medical records or who were unable to provide informed consent.
Data extraction and analysis
Data were analyzed using SPSS version 22.0. The normal distribution of numerical data was assessed using the Kolmogorov-Smirnov test. Descriptive statistics, including mean and standard deviation, were calculated for continuous variables. Chi-square tests were used for categorical variables to assess associations between TCC frequency, Pap smear abnormalities, and obstetric outcomes. A significance level of p < 0.05 was considered statistically significant.
Results
A total of 1052 patients who underwent TCC were included in the study, with a mean age of 34·4 ± 7·4 years. The most common reasons for TCC included vaginal discharge, pelvic pain, infertility, vaginal itching, and other causes, respectively. The number of TCC procedures was analyzed, categorizing patients into three groups: once, twice, and more than twice. The time since the last TCC was divided into three categories: within the last year, 2–5 years ago, and more than 5 years ago.
Pap smear results revealed abnormalities in 121 patients (11·5%). Abnormal smear results were more frequent in those who had TCC within the last year (29·9%). A decrease in the frequency of abnormal smears was observed as the time since the last TCC increased (p < 0·005). Additionally, an increase in the number of TCC procedures correlated with a decrease in the frequency of abnormal smear results (p < 0·005).
The relationship between the number of TCC procedures and pregnancy outcomes was examined. Abortion was detected with a prevalence of 18·9% (n = 199) and preterm delivery with a prevalence of 10·3% (n = 108) among all patients. As the number of TCC procedures increased, there was a statistically significant increase in the frequency of abortion and PTD (both p < 0·005). While an increase in the duration since the last TCC was associated with an increase in abortion and PTD counts, both were statistically significant (p = 0·016 and p = 0·029, respectively). Results are summarized in Table 1; Fig. 1.
Discussion
Our study reveals that traditional cervical cauterization (TCC) is associated with a notable increase in abnormal Pap smear results and adverse pregnancy outcomes. Specifically, 29.9% of women who had TCC within the past year showed abnormal Pap smear results, significantly higher than the general prevalence of 4% reported in the literature10,11. This suggests that recent TCC is associated with cervical trauma, which may contribute to a higher rate of cellular abnormalities. The overall frequency of abnormal smears was 11.5%, but decreased as the time since the last TCC increased, indicating that while immediate post-TCC trauma results in higher abnormality rates, some degree of healing occurs over time.
These findings are consistent with previous research showing that uncontrolled thermal trauma from procedures like TCC disrupts cervical cellular integrity and impairs the healing process9. The thermal trauma inflicted during TCC adversely affects various components of the cervical microenvironment, including the balance of the cervical microbiome, alterations in secretion, and connective tissue integrity. Our observation that abnormal smear results decrease with time supports the notion that some healing occurs, though the trauma from recent TCC appears to have a more pronounced impact.
The involvement of bacterial taxa such as Proteobacteria and Actinobacteria in inflammatory processes within the cervix, as noted in our study, suggests a potential link between these bacterial groups and the inflammatory response following TCC9. This aligns with existing literature, which highlights how thermal damage can exacerbate inflammatory responses and disrupt cervical cellular function.
Our study also demonstrated a higher frequency of miscarriages (18.9%) and preterm deliveries (10.3%) among women who underwent TCC more frequently. This is consistent with previous research linking cervical insufficiency to adverse pregnancy outcomes12,13,14. The disruption of cervical architecture, particularly the collagen tissue and extracellular matrix, may be involved in mechanisms underlying cervical insufficiency, leading to an increased risk of miscarriage and preterm birth.
The correlation between frequent TCC and elevated rates of miscarriage and preterm delivery emphasizes the need to consider cervical health when evaluating traditional cauterization methods. The findings suggest that repeated TCC may be associated with compromised cervical structural integrity, which could be linked to adverse pregnancy outcomes.
While traditional cervical cauterization (TCC) is not a practice employed by modern healthcare providers, its continued use in certain regions underscores the need for greater awareness of its potential risks. The significant associations found between TCC and increased rates of abnormal cervical smears, miscarriages, and preterm deliveries highlight the adverse effects this procedure can have on cervical health and pregnancy outcomes. This emphasizes the importance of educating communities where TCC is practiced about the potential dangers and the benefits of safer, evidence-based medical interventions. Public health initiatives and educational programs should aim to inform individuals about the risks associated with TCC and advocate for alternative approaches that mitigate these risks while addressing gynecological concerns.
Strengths and limitations
This study’s strengths lie in its large sample size of 1,052 patients, which enhances the reliability and generalizability of the findings. The comprehensive data collection on cervical cellular changes and reproductive health provides a detailed analysis of the effects of traditional cervical cauterization (TCC). By focusing on a practice still used in some regions, the study offers valuable insights into the risks associated with TCC, and its temporal analysis of recent versus past procedures provides statistically significant evidence regarding the duration and progression of its impacts on miscarriage and preterm delivery. Additionally, the study’s examination of the correlation between TCC frequency and adverse pregnancy outcomes, such as miscarriages and preterm deliveries, contributes significant evidence to the understanding of how TCC affects reproductive health.
The study’s sole reliance on Pap smear results for the assessment of cervical lesions represents a limitation. While a Pap smear is a valuable screening tool, it may not provide a comprehensive evaluation, especially considering the evolving landscape of cervical lesion assessment that includes additional diagnostic methods. The absence of information regarding HPV testing in the study introduces a limitation. The absence of HPV test results may limit the depth of understanding regarding the relationship between TCC and HPV-related cervical changes. The study’s focus on patients who exclusively underwent TCC introduces a potential selection bias. This limitation may impact the generalizability of the findings to a broader population and could overlook potential cervical health variations in individuals who did not undergo TCC.
Another limitation of this study is the lack of a control group comprising women without a history of TCC. This omission limits the strength of the conclusions and precludes causal inference. Nevertheless, the observed associations — several of which reached statistical significance — contribute important preliminary evidence and underscore the need for further controlled studies.
Additionally, the lack of data on key confounding factors such as HPV infection, parity, and history of sexually transmitted infections limits the ability to isolate the independent effects of TCC. HPV testing, in particular, is not routinely available as part of the national screening program in Somalia, which reflects broader limitations in local healthcare infrastructure. This unavailability may have influenced the observed cytological outcomes and should be addressed in future research designs.
Conclusion
In individuals subjected to Traditional Cervical Cauterization (TCC), a notable increase in the incidence of abnormal smear results is observed within the first year post-procedure. Additionally, the frequency of both miscarriages and preterm deliveries demonstrates an upward trend with an increasing number of TCC sessions.
Moreover, the duration since the last TCC procedure was found to be statistically significantly associated with abortion and PTD rates, indicating the impact of time-dependent recovery or cumulative damage.
Although there is a possibility of regression in early cellular changes during the initial stages, the cumulative impact of repeated interventions may be associated with macroscopic alterations in the cervical structure. To comprehensively understand the relationship between TCC and the prevalence of abnormal smears, miscarriages, and preterm deliveries, it is imperative to conduct a comparative analysis with individuals who have not undergone TCC.
Data availability
The data that support the findings of this study are not openly available due to technical reasons. Tha data is SPSS file. The data is available from the corresponding author upon reasonable request.
References
Jaladat, A. M. et al. Similarities and differences between Kaiy in Persian medicine and moxibustion in Chinese medicine. J. Integr. Med. 21(4), 354–360 (2023).
Hussein, A. I. et al. Traditional female cervical cauterization and risk of preterm birth in somalia: a single-center prospective observational study. Sci. Rep. 14(1), 20560 (2024).
Tesfai, B. et al. Knowledge, attitude, practice and prevalence of traditional cauterization among patients in Massawa hospital, eritrea: a cross-sectional study. Pan Afr. Med. J. 36, 230 (2020).
Abdullah, A. H. & Dehiol, R. K. Traditional cauterization among children in Bint Al-Huda hospital in Al-Nasiriya city, Iraq. J. Popul. Ther. Clin. Pharmacol. 29 (2), e40–e51 (2022).
Liu, Y. et al. Characteristics of vaginal microbiota in various cervical intraepithelial neoplasia: a cross-sectional study. J. Transl Med. 21 (1), 816 (2023).
Pangarkar, M. A. The Bethesda system for reporting cervical cytology. Cytojournal 19, 28 (2022).
Practice Bulletin No. 142: Cerclage for the Management of Cervical Insufficiency. Obstetrics & Gynecology. ; 123(2 PART 1): 372-9. (2014).
Areia, A. L., Moura, P. & Mota-Pinto, A. The role of innate immunity in spontaneous preterm labor: A systematic review. J. Reprod. Immunol. 136, 102616 (2019).
Gorczyca, K., Obuchowska, A., Kimber-Trojnar, Ż., Wierzchowska-Opoka, M. & Leszczyńska-Gorzelak, B. Changes in the gut Microbiome and pathologies in pregnancy. Int J. Environ. Res. Public. Health ; 19(16). (2022).
Mayer, C. & Mahdy, H. Abnormal Papanicolaou Smear (StatPearls Publishing, 2023).
Kurtay, S., Ali, K. Y. & Hussein, A. I. Frequency of cervical premalignant lesions in the gynecologic patients of a tertiary hospital in mogadishu, Somalia. BMC Womens Health. 22 (1), 501 (2022).
Myers, K. M., Socrate, S., Paskaleva, A. & House, M. A study of the anisotropy and tension/compression behavior of human cervical tissue. Journal Biomech. Engineering ; 132(2). (2010).
Vink, J. & Mourad, M. The pathophysiology of human premature cervical remodeling resulting in spontaneous preterm birth: where are we now? Semin Perinatol. 41 (7), 427–437 (2017).
Han, Y., Li, M., Ma, H. & Yang, H. Cervical insufficiency: a noteworthy disease with controversies. J. Perinat. Med. 48 (7), 648–655 (2020).
Funding
No financial grants were received for this study.
Author information
Authors and Affiliations
Contributions
SK was responsible for conceptualization, methodology, supervision, and writing – review & editing. AIH contributed to data curation, formal analysis, investigation, software, and visualization. KYA handled project administration, resources, validation, writing – original draft, and writing – review & editing. All authors provided critical input into the draft manuscript and had final responsibility for the decision to submit it for publication.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Ethical approval
The study was approved by the Ethical Research Committee of Mogadishu Somali Turkish Training and Research Hospital (Ref. MSTH/7581 − 432). All participants permitted the use of their demographic and medical data. This study was carried out per the content of the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kurtay, S., Hussein, A.I. & Ali, K.Y. The consequences of traditional cervical cauterization on cervical integrity and pregnancy: a cross-sectional study. Sci Rep 15, 32952 (2025). https://doi.org/10.1038/s41598-025-09011-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09011-0