Abstract
The high rate of unexplained female infertility significantly affects public health and women’s mental well-being. Research on dietary nutrients’ impact on infertility often overlooks vitamin B2. Exploring this vitamin’s role could be crucial for understanding and addressing female infertility. A cross-sectional study was conducted on women of reproductive age, utilizing data from the National Health and Nutrition Examination Surveys (NHANES) for the period 2013–2018. To assess the relationship between vitamin B2 intake and female infertility, multivariable logistic regression analysis was employed. Furthermore, subgroup analysis was performed on baseline categorical variables. The results were summarized using an odds ratio (OR) with a 95% confidence interval (CI). Additionally, restricted cubic splines were applied to explore linear correlations. Among a total of 3,208 women, 524 were found to be infertile. The results indicated that, within a fully adjusted model, a higher intake of vitamin B2 was associated with a lower prevalence of female infertility (OR [95% CI]: 0.81 [(0.69, 0.96)]), and the highest quartile of vitamin B2 intake (Q4) offered greater protection against infertility compared to the lowest quartile (Q1) (OR [95% CI]: 0.58 [0.38, 0.89]). Subgroup analysis showed the association between vitamin B2 intake and female infertility was independent across all baseline variable groups, with no observed interaction. A negative linear relationship was also confirmed through RCS (P for non-linearity = 0.503). Increased vitamin B2 intake is associated with a reduced risk of infertility in women. Our findings suggest that maintaining adequate vitamin B2 levels could help lower infertility risks. Dietary modifications and vitamin supplementation may be key in preventing and treating infertility early on.
Similar content being viewed by others
Introduction
Female Infertility, defined as the failure to achieve a clinical pregnancy after 12 months or more of regular unprotected intercourse, affects 8.8% of US women aged 15–49 years, and is an important medical and social problem worldwide1,2. Female infertility is also associated with an increased prevalence of adverse pregnancy outcomes such as preterm birth and low birth weight3,4. Assisted reproductive technologies to address female infertility are not only costly but are also associated with an increased prevalence of adverse pregnancy and birth outcomes5. More importantly, the proportion of unexplained female infertility remains high, with significant impacts on public health and women’s psychological stress6.
Common causes of infertility include gynecological disorders (including premature ovarian insufficiency, endometriosis, uterine fibroids and endometrial polyps), endocrine disorders (including polycystic ovary syndrome, underweight, overweight, diabetes and thyroid disorders) and psychological factors (including anxiety and depression)7,8,9 and environmental factors, such as cigarette smoking, have also been suggested as potential causes10,11. In addition, dietary nutrients are also considered to be important factors in the development of infertility. The intake of folic acid, vitamin A, and vitamin C is thought to reduce the risk of infertility, while the intake of fatty acids increases the risk of infertility in women, highlighting the importance of nutritional factors, such as vitamin intake, for the risk of female Infertility in women12,13,14.
Vitamin B2, also known as riboflavin, is a heterocyclic isoalloxazine derivative. As a member of the B-vitamins, vitamin B2 acts as a coenzyme in 1-carbon metabolism, participates in energy metabolism and redox reactions, and directly influences the maintenance of lipid metabolism, energy metabolism, redox balance and metabolism of drugs and xenobiotics, is a water-soluble essential vitamin15,16. Furthermore, vitamin B2 is usually derived from food, and insufficient intake of milk and meat predisposes to riboflavin deficiency, especially under certain physiological conditions such as pregnancy or lactation16,17.
The rationale for this study stems from the critical yet understudied role of vitamin B2 in female reproductive health. Previous studies have suggested that regular multivitamin supplements may reduce the risk of ovulatory infertility, a result that can be explained by folic acid, but fewer studies have examined the individual effects of various vitamins18. Meanwhile, although Ji et al. explored the association between multiple dietary nutrients and infertility including folic acid, vitamin B2 was not mentioned, leaving a gap in understanding its potential protective or risk-modifying effects13. High-dose folic acid (vitamin B9) supplementation before conception reduces the risk of miscarriage and stillbirth19. The intake of niacin (vitamin B3) and vitamin B6 had a significant effect on free androgen index (FAI)20. Polzikov et al. proposed through Randomized Controlled trials that elevated serum folate levels are associated with worse outcomes of assisted reproductive technology in women with normal fertility21. Ovayolu et al. found that lower levels of niacin may be associated with premature ovarian insufficiency22. Considering the potential role of dietary nutrients in infertility, we believe that it is proposed and aimed to investigate the association between vitamin B2 and female infertility. The novelty of this work lies in its focused examination of vitamin B2 using the National Health and Nutrition Examination Survey (NHANES) database, a large-scale, cross-sectional dataset that captures diverse demographic and dietary variables across the U.S. population. This approach not only enhances statistical power but also allows for stratification by key confounders to isolate vitamin B2’s specific association with infertility. Additionally, this is the first to investigate vitamin B2 in relation to female infertility, addressing a critical gap in both nutritional epidemiology and reproductive medicine.
Therefore, the aim of this study was to examine the association between vitamin B2 and female infertility by analyzing nationally representative cross-sectional data obtained from the NHANES.
Materials and methods
Data sources
We obtained data from publicly accessible files spanning the 1999 to 2018 cycle of NHANES, a continuous cross-sectional observational investigation capturing health data from a representative cross-section of the noninstitutionalized U.S. populace. The NHANES study protocol garnered approval from the Institutional Review Board of the National Center for Health Statistics (NCHS), with all participants consenting to their involvement. Our focus was on women aged 20 years and above who provided self-reported data within NHANES. Further elucidation of the survey’s framework can be sought on another website23.
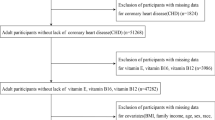
Our study utilized data from three consecutive NHANES cycles spanning from 2013 to 2018. We implemented specific exclusion criteria targeting women of reproductive age (n = 5,866). Criteria included absence of infertility data (n = 851), lack of vitamin B2 data (n = 791), missing demographic information (n = 343) encompassing age, race/ethnicity, marital status, poverty income ratio (PIR), and education level, as well as unavailable miscellaneous data (n = 77) such as physical activity, alcohol consumption, smoking habits, body mass index (BMI), healthy eating index-2015 (HEI-2015), age at menarche, history of pelvic infection/pelvic inflammatory disease (PID), use of birth control pills, and use of female hormones. The final analysis comprised 3,804 eligible participants, as depicted in Fig. 1.
Assessment of vitamin B2 intake
In order to measure the intake of energy, nutrients, and various food components, every participant in the NHANES provided comprehensive dietary interview data over two separate 24-hour periods, using a standardized and validated approach conducted by trained interviewers using the United States Department of Agriculture (USDA) Automated Multiple-Pass Method (AMPM)24,25,26. This is a structured, computerized five-step interview designed to enhance recall accuracy and minimize underreporting. The 5 steps are followed: (1) Forgotten Foods: Participant is asked about consumption of foods commonly forgotten during the Quick List step. (2) Time and Occasion: Time and eating occasion are collected for each food. (3) Detail Cycle: For each food, a detailed description, amount eaten, and additions to the food are collected. (4) Eating occasions and times between eating occasions are reviewed to elicit forgotten foods. (5) Final Probe: Additional foods not remembered earlier are collected. During the first recall (Day 1), participants underwent an in-person dietary interview at the Mobile Examination Center. The second dietary recall occurred via phone call 3 to 10 days following the initial recall, which took place at the Mobile Examination Center27,28. The USDA’s Food and Nutrient Database for Dietary Studies (FNDDS) was then used to match reported foods with their nutrient profiles and estimate daily intakes of riboflavin (vitamin B2) in milligrams. This approach is consistent with prior published studies using NHANES data and has been widely used in the literature for nutrient intake assessment29,30.
Assessment of infertility
Infertility was evaluated through self-reports using two questions: “Have you ever attempted to become pregnant over at least a year without becoming pregnant?” and “Have you ever been to a doctor or other medical provider because you have been unable to become pregnant?”. A definitive “yes” to either question indicated infertility, which was then analyzed as an outcome variable9,31,32.
Covariates
This study accounted for various potential influencing factors based on published research and clinical judgment13,33. These factors include age, race, marital status, education level, PIR, BMI, physical activity, smoking habits, alcohol consumption, HEI-2015, age at menarche, history of pelvic infection/PID, use of birth control pills, and use of female hormones, except for covariates used for subgroup analysis.
Age, PIR, BMI, physical activity, HEI-2015, and age at menarche were treated as continuous variables. Age was classified as < 30 and ≥ 30. BMI was calculated as weight in kilograms divided by the square of height in meters, and when used as an exposure variable or in subgroup analyses, BMI was classified as < 25 (normal) and ≥ 25 (overweight)34.
Self-reported race was categorized into Mexican American, non-Hispanic White, non-Hispanic Black, other Hispanic, and others (including multi-racial participants). Education level was grouped into less than high school, high school or equivalent, and above high school. Marital status was classified into married, never married, living with a partner, and other (e.g., widowed, divorced, or separated).
Smoking status was categorized as never (fewer than 100 cigarettes), former (more than 100 cigarettes but quit), and current (more than 100 cigarettes and currently smoking) 23. Drinking status was grouped into never (< 12 lifetime drinks), former (< 12 lifetime drinks, no drinks in the past year), mild (≤ 1 drink per day in the past year), moderate (≤ 2 drinks per day in the past year), and heavy (≥ 3 drinks per day in the past year). Pelvic infection/PID history, use of birth control pills, and use of female hormones were reported as “Yes” or “No”.
Based on published research and clinical judgment13,33this study adjusted for several potential confounding variables, including age, race, marital status, education level, PIR and marital status, BMI, physical activity, smoking status, drinking status, HEI-2015, age at menarche, pelvic infection/PID history, use of birth control pills, and use of female hormones, except for covariates used for subgrouping. Age, PIR, BMI, physical activity, HEI-2015 and age at menarche were considered continuous variables.
Statistical analysis
The analysis adhered to NHANES Analytic Guidelines, accounting for the complex sampling design and sampling weights35. Participant characteristics were presented as means (standard error, SE) for continuous variables and n (frequency, as percentages) for categorical variables. As the continuous data, the t-test was used for normally distributed data and the Wilcoxon rank-sum test was used for complex survey samples, while categorical data were classified using the chi-squared test with Rao & Scott’s second-order correction. Logistic regression models were employed to calculate odds ratios (OR) and 95% confidence intervals (95%CI) to evaluate the relationship between vitamin B2 and infertility. Model 1 represented an unadjusted model, while Model 2 adjusted for age, race, marital status, education level, PIR, and marital status. Model 3 was further adjusted for BMI, physical activity, smoking status, drinking status, and HEI-2015. Additionally, Model 4 included adjustments for age at menarche, pelvic infection/PID history, use of birth control pills, and use of female hormones based on Model 3. A trend test was conducted by converting vitamin B2 from a continuous to a categorical variable. The association between vitamin B2 and infertility was further examined using restricted cubic spline (RCS) analysis with three knots (10th, 50th, and 90th percentiles).
We categorized the population based on race, BMI group, smoking status, drinking status, history of pelvic infection/PID treatment, use of birth control pills, and use of female hormones. Subsequently, we examined the relationship between vitamin B2 and infertility across these various groups. Additionally, we conducted an interaction test to assess whether the effect of intervention on the outcome of interest was influenced by baseline or demographic factors.
All statistical analyses were performed using R (version 4.2.3) and Free Software Foundation statistics software (version 1.9.2). Specifically, the “survey” package (version 4.2-1) was utilized for survey sample analysis. Statistical significance was determined by two-sided P values less than 0.05.
Results
Characteristics of the participants
Table 1 summarizes the characteristics of the study’s participants (n = 3804), representing over 75 million U.S. women, with an average age of 39.91 years (SE = 0.35). The cohort was split into a control group (n = 3208) and an infertility group (n = 524), highlighting distinct demographic and health-related differences. Women in the infertility group were older on average (41.65 years vs. 39.61 years), had a higher percentage of married individuals (65.93% vs. 49.96%), and exhibited a higher household PIR (3.01 vs. 2.87), suggesting slight economic advantages. Their BMI was also higher (32.08 vs. 29.53), and more likely to have received treatment for pelvic infections/PID (11.82% vs. 4.61%) and to have used female hormones (14.76% vs. 10.06%). No significant differences were observed in race, education, physical activity, smoking, alcohol consumption, HEI-2015 nutritional scores, age at menarche, and contraceptive use history, indicating these factors did not vary significantly between the groups.
Association between vitamin B2 intake and infertility
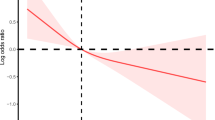
The association between vitamin B2 intake and infertility is depicted in Table 2. In the crude model, a significant association was observed between vitamin B2 as a continuous variable and infertility (OR [95% CI]: 0.86 [0.74, 1.002]). However, in the quartile-based model, a significant inverse correlation was observed in the highest quartile (Q4, > 2.15 mg) compared to the lowest quartile (Q1, < 1.22 mg) (OR [95% CI]: 0.64 [0.43, 0.97]), indicating a lower prevalence of infertility with higher vitamin B2 intake. No similar associations were detected in the second (Q2, 1.22–1.65 mg) and third quartiles (Q3, 1.66–2.15 mg). Upon fully adjusting all confounding factors and analyzing the results of multivariable logistic regression, an increase in vitamin B2 intake was associated with a 19% reduction in the prevalence of infertility (OR [95% CI]: 0.81[(0.69, 0.96]). Within the quartile model, compared to Q1, Q4 (OR [95% CI]: 0.58 [0.38, 0.89]) demonstrated a significant negative correlation with female infertility, with a significant trend observed (p for trend = 0.03). Figure 2 presents the association between vitamin B2 and infertility as estimated by RCS. In the RCS analysis, a significant linear negative correlation was observed between vitamin B2 intake and self-reported infertility (P for non-linearity = 0.503), further substantiating the robustness of the findings.
Association between vitamin B2 and infertility estimated by Restricted cubic splines (RCS). (A). Distribution of Vitamin B2 Intake Among Fertile and Infertile Groups. (B). Association Between Vitamin B2 Intake and Infertility estimated by Restricted cubic splines. Model was adjusted for age, race, marital status, education level, PIR and marital status, BMI, physical activity, smoking status, drinking status, HEI-2015, age at menarche, pelvic infection/PID history, use of birth control pills, and use of female hormones.
Subgroup analyses
Table 3 presents the association between vitamin B2 intake and infertility across various baseline subgroups. The multivariable linear analyses, stratified by race, BMI categories, smoking status, alcohol consumption, history of pelvic infection/PID, and history of contraceptive and female hormone use, revealed no significant interaction effects between these baseline variables and the association between vitamin B2 intake and self-reported infertility (p > 0.05). This indicates that the relationship between vitamin B2 intake and infertility is consistent across different demographic and health-related strata, underscoring the independence of the study’s findings.
Discussion
In this nationally representative cross-sectional study, we observed a significant inverse relationship between vitamin B2 intake and female infertility. Furthermore, subgroup analyses revealed no significant interactions between baseline variables and the association, suggesting the consistency of this relationship across different demographic and health-related factors.
Previous research has explored the association between nutrients like folic acid and vitamin D with infertility13,19. However, there remains a dearth of investigation into the association between vitamin B2 and female infertility. Ji et al. conducted a study investigating the association between nutrient intake, including vitamin A, vitamin C, iron, and folic acid, and infertility. Their findings demonstrated that a higher intake of vitamins such as vitamin A, and vitamin C can reduce the risk of infertility13. While Ji et al. focused on antioxidant vitamins, our study extends this line of inquiry by specifically examining vitamin B2, a nutrient not previously emphasized in fertility research. A cohort study by Jorge et al. followed 116,671 premenopausal female nurses for 8 years and revealed a negative correlation between the consumption of multivitamin supplements and ovulatory infertility18. Interestingly, the findings of Jorge et al. are consistent with our results, suggesting that vitamin use may be protective for infertility. However, their study did not examine the effects of vitamin B2 alone, highlighting the novelty of our study. Roshanzadeh et al. proposed through a case-control study of 156 women that there is a negative correlation between vitamin B12, B2, B6, and C and endometriosis36. Badri-Fariman et al. explored the association between dietary patterns and polycystic ovary syndrome (PCOS) through a case-control study, and they found that women with PCOS had lower B2, B6, B12 intake, and infertility was one of the characteristic manifestations of PCOS37. This study is the first to find a significant association between vitamin B2 intake and female infertility in a nationally representative population, providing a potential strategy for infertility treatment prevention.
The potential mechanism underlying the influence of vitamin B2 on female infertility may involve the following pathway. Riboflavin exhibits antioxidant properties and undergoes intracellular phosphorylation to form flavin mononucleotide (FMN), subsequently metabolizing into flavin adenine dinucleotide (FAD). FMN and FAD serve as crucial coenzymes for various oxidoreductases, such as glutathione reductase, facilitating pivotal roles in cellular redox reactions38. Oxidative stress has been linked to diverse reproductive disorders, including endometriosis and polycystic ovary syndrome, which can ultimately culminate in female infertility39. Therefore, vitamin B2 may mitigate oxidative stress through its antioxidative function, thereby protecting female reproductive function. Additionally, animal studies have demonstrated that vitamin B2 enhances survival rates in bacteria-infected mice and exhibits anti-inflammatory properties by reducing plasma concentrations of IL-6, TNF-α, and other inflammatory markers40,41. Inflammatory responses contribute significantly to female infertility, exemplified by conditions such as bacterial vaginosis, PID, and other reproductive tract infections42,43. Consequently, the anti-inflammatory properties of vitamin B2 could potentially mitigate the risk of infertility by dampening inflammatory responses. However, the precise mechanism underlying the association between vitamin B2 and infertility remains unclear, necessitating further investigation.
This study possesses several strengths. Firstly, it represents the inaugural cross-sectional investigation examining the relationship between vitamin B2 intake and female infertility. Secondly, the study meticulously adhered to NHANES standards in terms of study design, data collection, and processing, thereby minimizing the potential for non-sampling and measurement errors. Thirdly, the incorporation of complex sampling weights and careful consideration of sample design ensured the derivation of nationally representative sample estimates.
Nevertheless, this study is not without its limitations. Firstly, the reliance on self-reported infertility diagnoses may introduce discrepancies compared to objective reality, and employing more robust data collection methods could have enhanced the credibility of the study. Secondly, akin to other observational studies, our investigation lacked the capability to conclusively eliminate residual or unidentified confounders, as well as the potential confounding effects arising from measurement error and variables assessed for measurement. To bolster the validity of our findings, a prospective randomized controlled trial in the future may help address these concerns. Lastly, given the inherent nature of observational studies, establishing a definitive causal relationship is currently beyond reach.
Conclusions
Increased vitamin B2 intake is correlated with a decreased risk of infertility in women. Our results imply that sustaining sufficient vitamin B2 intake may contribute to lowering the risk of infertility in women. Subsequent interventions focused on dietary adjustments and vitamin supplementation could potentially play a crucial role in the early prevention and treatment of infertility.
Data availability
The NHANES data are publicly available at https://wwwn.cdc.gov/nchs/nhanes which is publicly available. The data underlying this article will be shared on reasonable request to the corresponding author.
References
Pavli, P. et al. Infertility improvement after medical weight loss in women and men: A review of the literature. Int. J. Mol. Sci. 25, 1909 (2024).
Carson, S. A. et al. Diagnosis and management of infertility: A review. JAMA 326, 65–76 (2021).
Messerlian, C. et al. Infertility and the risk of adverse pregnancy outcomes: a systematic review and meta-analysis. Hum. Reprod. 28, 125–137 (2013).
Basso, O. et al. Infertility and preterm delivery, birthweight, and caesarean section: a study within the Danish National birth cohort. Hum. Reprod. 18, 2478–2484 (2003).
Guideline Group on Unexplained Infertility. Evidence-based guideline: unexplained infertility. Hum. Reprod. 38, 1881–1890 (2023).
Practice committee of the American society for reproductive medicine. Electronic address: asrm@asrm.org & practice committee of the American society for reproductive medicine. Evidence-based treatments for couples with unexplained infertility: a guideline. Fertil. Steril. 113, 305–322 (2020).
Vander Borght, M. et al. Fertility and infertility: definition and epidemiology. Clin. Biochem. 62, 2–10 (2018).
Bellver, J. et al. Introduction: infertility etiology and offspring health. Fertil. Steril. 111, 1033–1035 (2019).
Rooney, K. L. et al. The relationship between stress and infertility. Dialogues Clin. Neurosci. 20, 41–47 (2018).
Skakkebæk, N. E. et al. Environmental factors in declining human fertility. Nat. Rev. Endocrinol. 18, 139–157 (2022).
Practice committee of the American society for reproductive medicine. Electronic address: asrm@asrm.org & practice committee of the American society for reproductive medicine. Smoking and infertility: a committee opinion. Fertil. Steril. 110, 611–618 (2018).
Gaskins, A. J. et al. Diet and fertility: a review. Am. J. Obstet. Gynecol. 218, 379–389 (2018).
Ji, X. et al. Association between nutrient intake and female infertility: a study based on NHANES database. J. Obstet. Gynaecol. 43, 2285025 (2023).
Xu, W. et al. Insights into modifiable risk factors of infertility: A Mendelian randomization study. Nutrients 14, 4042 (2022).
Pinto, J. T. et al. Adv. Nutr. 7, 973–975 (2016).
Thakur, K. et al. Riboflavin and health: A review of recent human research. Crit. Rev. Food Sci. Nutr. 57, 3650–3660 (2017).
Boisvert, W. A. et al. Prevalence of riboflavin deficiency among Guatemalan elderly people and its relationship to milk intake. Am. J. Clin. Nutr. 58, 85–90 (1993).
Chavarro, J. E. et al. Use of multivitamins, intake of B vitamins, and risk of ovulatory infertility. Fertil. Steril. 89, 668–676 (2008).
Ichikawa, T. et al. Associations of nutrients and dietary preferences with recurrent pregnancy loss and infertility. J. Nippon Med. Sch. 91, 254–260 (2024).
Hestiantoro, A. et al. Vitamin B3 (niacin), B6, C, and iron intake are associated with the free androgen index, especially in normoandrogenic polycystic ovary syndrome. J. Turk. Ger. Gynecol. Assoc. 23, 130–136 (2022).
Polzikov, M. et al. Association of the serum folate and total calcium and magnesium levels before ovarian stimulation with outcomes of fresh in vitro fertilization cycles in normogonadotropic women. Front. Endocrinol. (Lausanne). 13, 732731 (2022).
Ovayolu, A. et al. A prospective and comparative investigation of blood sFlt-1, P1GF, and niacin concentrations in women with premature ovarian insufficiency. J. Obstet. Gynaecol. Res. 49, 1198–1205 (2023).
Questionnaires, N. H. A. N. E. S. & Documentation, R. Datasets, and https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/
Dietary data - continuous NHANES. https://wwwn.cdc.gov/nchs/nhanes/search/datapage.aspx?Component=Dietary
CDC. Data and analysis tools. National Center for Health Statistics (2024). https://www.cdc.gov/nchs/data-analysis-tools/index.html
Moshfegh, A. J. et al. The US department of agriculture automated multiple-pass method reduces bias in the collection of energy intakes. Am. J. Clin. Nutr. 88, 324–332 (2008).
Saint-Maurice, P. F. et al. Estimated number of deaths prevented through increased physical activity among US adults. JAMA Intern. Med. 182, 349–352 (2022).
Jayanama, K. et al. Relationship between diet quality scores and the risk of frailty and mortality in adults across a wide age spectrum. BMC Med. 19, 64 (2021).
Zhou, L. Association of vitamin B2 intake with cognitive performance in older adults: a cross-sectional study. J. Transl Med. 21, 870 (2023).
Ued, F. V. et al. Vitamin B2 and folate concentrations are associated with ARA, EPA and DHA fatty acids in red blood cells of Brazilian children and adolescents. Nutrients 11, 2918 (2019).
Fan, W. et al. Association between cardiometabolic index and infertility risk: a cross-sectional analysis of NHANES data (2013–2018). BMC Public. Health. 25, 1626 (2025).
Yang, S. et al. Correlation between serum uric acid to serum creatinine ratio and infertility in reproductive-age female of american: data from National health and nutrition examination survey (NHANES), 2013–2016. J. Gynecol. Obstet. Hum. Reprod. 102965 https://doi.org/10.1016/j.jogoh.2025.102965 (2025).
Zhan, W. et al. Association between co-exposure to phenols and phthalates mixture and infertility risk in women. Environ. Res. 215, 114244 (2022).
Rubino, F. et al. Definition and diagnostic criteria of clinical obesity. Lancet Diabetes Endocrinol. 13, 221–262 (2025).
Johnson, C. L. et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat. 2, 1–24 (2013).
Roshanzadeh, G. et al. The relationship between dietary micronutrients and endometriosis: A case-control study. Int. J. Reprod. Biomed. 21, 333–342 (2023).
Badri-Fariman, M. et al. Association between the food security status and dietary patterns with polycystic ovary syndrome (PCOS) in overweight and obese Iranian women: a case-control study. J. Ovarian Res. 14, 134 (2021).
Suwannasom, N. et al. Riboflavin: the health benefits of a forgotten natural vitamin. Int. J. Mol. Sci. 21, 950 (2020).
Agarwal, A. et al. The effects of oxidative stress on female reproduction: a review. Reprod. Biol. Endocrinol. 10, 49 (2012).
Toyosawa, T. et al. Highly purified vitamin B2 presents a promising therapeutic strategy for sepsis and septic shock. Infect. Immun. 72, 1820–1823 (2004).
Toyosawa, T. et al. Effects of intravenous infusion of highly purified vitamin B2 on lipopolysaccharide-induced shock and bacterial infection in mice. Eur. J. Pharmacol. 492, 273–280 (2004).
Ravel, J. et al. Bacterial vaginosis and its association with infertility, endometritis, and pelvic inflammatory disease. Am. J. Obstet. Gynecol. 224, 251–257 (2021).
Chen, Y. et al. Inflammatory markers are associated with infertility prevalence: a cross-sectional analysis of the NHANES 2013–2020. BMC Public. Health. 24, 221 (2024).
Funding
None.
Author information
Authors and Affiliations
Contributions
Zitong Zhao and Zenghui Mao had full access to all the data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. Conceptualization: Zitong Zhao, Zenghui Mao, Zan Liu. Formal analysis: Zitong Zhao. Methodology: Zitong Zhao, Zenghui Mao. Project administration: Zenghui Mao, Zan Liu. Supervision: Zan Liu. Visualization: Zitong Zhao, Zenghui Mao, Min Liu. Writing-original draft: All authors. Writing-review & editing: Min Liu, Ying Liang, Xiaowen Liu, Pan Yang.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The National Health and Nutrition Examination Survey (NHANES) is conducted by the Centers for Disease Control and Prevention (CDC) and the National Center for Health Statistics (NCHS). The NCHS Research Ethics Review Committee reviewed and approved the NHANES study protocol. All participants signed written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, Z., Mao, Z., Liu, M. et al. Association between vitamin B2 intake and female infertility: a cross-sectional study. Sci Rep 15, 23731 (2025). https://doi.org/10.1038/s41598-025-09161-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09161-1