Abstract
Incomplete peripheral nerve injuries with structural pathological changes in the epineurium present treatment challenges, particularly when epineurotomy is required. This study investigates whether the combination of bovine collagen artificial nerve conduit (BCANC) and platelet-rich plasma (PRP) can mitigate the adverse effects of epineurotomy and promote more effective sensory and motor nerve recovery.A total of 222 patients (ages 16–75) with incomplete peripheral nerve injuries were enrolled. The test group underwent epineurotomy combined with BCANC and PRP implantation, while the control group received epineurotomy alone. Sensory and motor recovery were evaluated using electromyography and clinical measures at 1 and 3 months post-surgery, with analyses stratified by nerve type (Median, Ulnar, Radial). For median nerve injuries, the test group showed significant improvements across multiple electrophysiological parameters; clinically, both muscle strength (MRC scale, 3 months, p = 0.008) and sensory function (MRC scale, 1 and 3 months, p < 0.05) were significantly enhanced. For ulnar nerve injuries, significant electrophysiological improvements were observed; however, clinical muscle strength and sensory function did not significantly differ. For radial nerve injuries, part of electrophysiological parameters significantly improved in the test group, and clinical sensory function (3 months, p = 0.030) was also significantly better, while muscle strength showed no significant difference. Overall functional evaluation (Disabilities of the Arm, Shoulder and Hand score) did not significantly differ between groups for any nerve type. No severe complications were noted. BCANC with PRP following epineurotomy is safe and yields significant short-term electrophysiological improvements for median, ulnar, and radial nerve injuries. Clinically, benefits included enhanced muscle strength and sensory function for median nerves, and improved sensory function for radial nerves; ulnar nerve clinical recovery and overall DASH scores were not significantly different. These findings suggest nerve-dependent clinical benefits, and further long-term studies are warranted.
Similar content being viewed by others
Introduction
Peripheral nerve injuries (PNI) are typically observed during emergency surgery and trauma orthopedics, affecting an estimated one to two million individuals annually1. These injuries can lead to diminished sensation, weakened muscles, pain, and discomfort in the innervated area. In more severe instances, they may result in muscular atrophy, loss of movement, and eventual disability2,3,4. Existing literature suggests that 60–70% of severe peripheral nerve injuries do not exhibit complete transection (neurotmesis) but rather retain a continuous appearance5,6.
Neurolysis, encompassing external and internal procedures, is often the primary surgical approach for these incomplete PNI7. While external neurolysis, which involves freeing the nerve from surrounding scar tissue, is a common prerequisite for nerve repair6,8, the role of internal neurolysis techniques, particularly epineurotomy (a longitudinal incision into the epineurium), remains debated. For instance, in the context of carpal tunnel syndrome (CTS), guidelines generally discourage routine epineurotomy alongside standard decompression, citing a lack of proven additional benefit and potential for increased adverse events9,10,11. Similar observations have been reported in multiple prior investigations12,13,14.
However, epineurotomy may be considered necessary in specific incomplete PNIs presenting with significant structural epineurial pathology (e.g., fibrosis, constriction), based on the rationale that external decompression alone might not fully address these challenging scenarios15,16,17. Yet, this intervention carries inherent risks, including potential nerve trauma, disruption of the local inflammatory microenvironment, and critically, induction of secondary perineural scar formation. This scarring can tether the nerve, impede gliding, compromise vascularity, hinder axonal regeneration, and ultimately limit functional recovery9,18,19.
To address the challenge of mitigating these adverse effects when epineurotomy is deemed necessary, innovative adjunctive strategies are needed. Absorbable nerve conduits (ANCs), typically used to bridge gaps in completely transected nerves, function by creating a protective microenvironment that guides regeneration and prevents scar tissue infiltration20,21,22. We hypothesize that applying a similar principle using a bovine collagen artificial nerve conduit (BCANC) – enveloping the nerve after epineurotomy – might provide mechanical protection and reduce detrimental scarring in this specific context of incomplete injury repair. Furthermore, to actively promote nerve healing within this protected space, we explored the concurrent application of Platelet-Rich Plasma (PRP). PRP is an autologous blood concentrate rich in platelets and a multitude of growth factors (e.g., NGF, PDGF, TGF-β, VEGF) and bioactive molecules known to be crucial for tissue repair23,24,25 (Fig. 2). Extensive research supports PRP’s potential to enhance nerve regeneration by stimulating key cellular processes like Schwann cell activity, promoting revascularization, modulating inflammation, and potentially reducing fibrosis26,27,28,29,30.
Therefore, this retrospective case-control study aims to assess the effectiveness of employing BCANC in conjunction with PRP following epineurotomy for the treatment of incomplete peripheral nerve injuries in patients with structural nerve changes, such as scarring, fibrosis, or edema, that required epineurotomy. This case-control study has been reported in line with the STROCSS guidelines31.
Methods
Patients
This retrospective study analyzed clinical data from the Traumatic Osteopathic Department at Nanfang Hospital between January 1, 2021, and April 1, 2024. A total of 222 patients (ages 16–75 years) with incomplete peripheral nerve injuries of the upper extremities requiring epineurotomy were enrolled. Each patient presented with an injury to a single nerve type (Median, Ulnar, or Radial).
Inclusion criteria included:
-
1.
Age: 16–75 years.
-
2.
Diagnosis: Incomplete peripheral nerve injury of the upper extremity (Median, Ulnar, or Radial nerve) located between the elbow and wrist, resulting specifically from a motor vehicle accident, blunt trauma, or a fall.
-
3.
Intraoperative confirmation of significant structural changes (e.g., marked epineural thickening, scarring, or edema interfering with nerve gliding or indicating intraneural pressure) requiring epineurotomy. Preoperative assessment including clinical examination, EMG, and ultrasound guided surgical indication, but final decision for epineurotomy and inclusion relied on intraoperative findings.
-
4.
All included nerves maintained anatomical continuity.
-
5.
Availability of complete preoperative, 1-month postoperative, and 3-month postoperative electromyography (EMG) recordings and other efficacy assessment results.
Exclusion criteria included:
-
1.
Patients whose preoperative EMG showed no recordable action potentials in the injured nerve.
-
2.
Chronic peripheral nerve entrapment syndromes (e.g., carpal tunnel syndrome, cubital tunnel syndrome not of acute traumatic origin as specified above).
-
3.
Severe concomitant injuries such as open fractures, extensive soft tissue damage, or active infections at the injury site.
-
4.
Central nervous system diseases.
-
5.
Serious liver or kidney function abnormalities, immunodeficiency diseases, psychiatric disorders, and diabetes mellitus.
This study was approved by the Ethics Committee of Nanfang Hospital (NFEC-2024-248), and informed consent was waived by the Committee for retrospective data use. All methods were performed in accordance with the relevant guidelines and regulations, including the principles outlined in the Declaration of Helsinki.
Surgical procedure
The same experienced surgical team performed all surgeries. The surgical procedures for the control and test groups shared initial steps but differed in the application of BCANC and PRP, as detailed below and illustrated in Figs. 1 and 2A:
Combination of nerve conduits and PRP gel for PNI. (A) The injured nerve was released, then the nerve was wrapped with a nerve conduit, and the space between the nerve and conduit was filled with PRP gel. (B) In the preoperative nerve ultrasound, the nerve was seen to be compressed, the cross-sectional area was thickened, and the nerve was edematous. In the postoperative nerve ultrasound, the edema was reduced, and the nerve was released from the compression.
-
1.
Exposure of the nerve: following the administration of satisfactory anesthesia, sequential incisions were made through the skin, subcutaneous tissue, and fascia to expose the damaged nerve. The nerve was meticulously dissected from surrounding scar or adhesion tissue, and any significant scar tissue adhering to the nerve surface was removed (External Neurolysis).
-
2.
Epineurotomy: following nerve exposure and external neurolysis, using an operating microscope, a longitudinal incision was made in the pathologically thickened, scarred, or edematous epineurium over the affected nerve segment. The length of the epineurotomy incision was determined based on the intraoperatively observed extent of these structural abnormalities (mean incision lengths for both groups are reported in Table 2). Care was taken to incise only the epineurium without damaging the underlying nerve fascicles.
-
3.
Control group procedure: In the control group (n = 112), the procedure concluded after Step 2 (Epineurotomy). No BCANC or PRP was applied.
-
4.
Test group procedure (BCANC + PRP Application): In the test group (n = 110), following Step 2, the procedure continued with:
-
BCANC application: A BCANC (Tianxin Fu, China) was selected and appropriately sized to cover the entire length of the epineurotomy site, ensuring it extended approximately 0.25 cm beyond the incision margins at each end. The conduit was carefully placed around the nerve segment encompassing the epineurotomy and secured to the intact epineurium using 7 − 0 non-absorbable sutures at both ends. Care was taken to ensure the nerve bundles were fully covered but not constricted by the conduit or sutures.
-
PRP and thrombin preparation and injection: Autologous PRP was prepared as detailed below. Lyophilized thrombin powder (2000 U, Hunan Yige Pharmaceutical Co., Ltd.) was reconstituted with 2 mL of sterile saline. Using a sterile three-way stopcock connecting two syringes (one containing the prepared PRP, the other containing the thrombin solution) and a single non-sharp injection needle, the two components were injected simultaneously into the space between the nerve surface and the inner wall of the BCANC. The typical injection ratio was approximately 1 mL of PRP to 200 U of thrombin. A volume of 1.5-2.0 mL of the mixture was slowly injected until the conduit space was adequately filled. This technique allowed the PRP and thrombin to mix immediately before delivery, forming a stable gel in situ that surrounded the nerve bundles and minimized leakage.
-
5.
Wound closure (Both Groups): At the conclusion of the procedures for both groups, absorbable sutures were employed to close the deep fascial layers and the skin incisions.
This retrospective study’s group allocation reflects an evolution in our surgical practice. The control group underwent our department’s established standard epineurotomy technique, common during the earlier study period. The test group’s approach, incorporating BCANC and PRP, was adopted more recently for patients with identical indications. Critically, the primary surgical team, operating conditions, and perioperative protocols remained consistent across both periods.
PRP Preparation and characteristics
Autologous PRP was prepared intraoperatively for each patient in the test group using the TriCell PRP KIT (REV-MED Inc., South Korea), a commercially available and validated closed-system device, strictly following the manufacturer’s instructions. Briefly, 3 mL of anticoagulant (typically citrate-based) was drawn into the collection syringe, followed by 30 mL of the patient’s venous blood (maintaining a 1:10 anticoagulant-to-blood ratio). The collected blood within the kit underwent a standardized two-step centrifugation process: an initial centrifugation at 3000 rpm for 4 min to separate red blood cells, followed by a second centrifugation of the resulting plasma at 3300 rpm for 3 min to concentrate the platelets and isolate the platelet-rich plasma layer from the platelet-poor plasma.
Based on manufacturer validation data, this specific kit and protocol typically yield Leukocyte-Poor Platelet-Rich Plasma (LP-PRP). The reported average characteristics of the final PRP product are: a platelet recovery rate of approximately 80.3%, a platelet concentration rate of approximately 7.6-fold over baseline whole blood levels, a final mean platelet concentration of approximately 1482 × 109/L, and a low white blood cell concentration of approximately 0.3 × 106/L.
Outcome assessment
Each of the 222 patients participated in a complete assessment protocol encompassing preoperative, one-month postoperative, and three-month postoperative evaluations. We used preoperative, surgical, and follow-up records to document the patient’s age, gender, BMI, nerve repaired, complications, and subjective and objective recovery of nerve function.
Electromyographic reports included recordings of distal motor latency (DML), compound muscle action potential amplitude (CMAP), motor conduction velocity (MCV), distal sensory latency (DSL), sensory nerve action potential amplitude (SNAP), and sensory conduction velocity (SCV). Delta changes for EMG parameters were calculated as the difference between the postoperative and preoperative values at 1 and 3 months (Delta = Follow-up Value − Baseline Value). These delta values were used to compare improvements between the test and control groups. The Disability of Arm, Shoulder, and Hand (DASH) questionnaire was used to assess overall upper extremity function, with higher scores indicating greater disability32.
Muscle strength assessment was based on the Medical Research Council (MRC) grading method33while the evaluation of sensory function was performed using the MRC scale of sensory recovery34. The detailed evaluation criteria are provided in Table 1.
Complications were monitored and categorized as minor or severe during the postoperative follow-up period. Minor complications included transient postoperative pain, localized edema, and mild wound irritation, all of which resolved with conservative treatment. Severe complications were defined as wound infections requiring medical or surgical intervention, nerve re-entrapment, or significant functional deficits that persisted beyond three months. Additionally, the length of the epineurotomy incision performed during surgery was retrieved from the operative records for each patient.
Statistical methods
SPSS 27.0.1 software was used for statistical analysis. The values were presented as the mean ± SD for normally distributed data and as the median and interquartile range (IQR) for data that were not normally distributed. The differences between groups for continuous variables were derived from the Mann-Whitney U test or independent samples t-test, as appropriate, following assessment of data distribution. Fisher’s exact test or Chi-square test was used to assess the distribution of categorical observations between two groups. Mann-Whitney U test was used for comparison of MRC grade distributions (Supplementary Tables S1-S3). All statistical analyses for EMG parameters, MRC grades, and DASH scores were performed separately for Median, Ulnar, and Radial nerve injury subgroups. A p-value less than 0.05 was statistically significant.
Results
Participant characteristics
A total of 222 patients meeting the inclusion criteria were enrolled in this study and allocated to treatment groups as described in the Methods section. For median nerve injuries, 40 patients were in the test group and 36 in the control group. For ulnar nerve injuries, 32 patients were in the test group and 36 in the control group. For radial nerve injuries, 38 patients were in the test group and 40 in the control group. The baseline demographic and clinical characteristics of the participants, stratified by nerve injury type and group, are presented in Table 2. There were no statistically significant differences between the test and control groups within each nerve-specific cohort regarding age, Body Mass Index (BMI), gender distribution, side of injury, or cause of injury (all p > 0.05, Table 2).
Electrophysiological outcomes
The changes in electrophysiological parameters for median nerve injuries are detailed in Table 3. Compared to the control group, the test group showed significantly greater improvement in DSL at 1 month (p = 0.001) and 3 months (p < 0.001), and SCV at 1 month (p < 0.001) and 3 months (p < 0.001). Significant improvements were also seen in the test group for SNAP at 3 months (p = 0.002), DML at 3 months (p = 0.038), and MCV at 3 months (p = 0.014). No significant inter-group differences were observed in the change from baseline for CMAP (p = 0.229 at 3 months).
For ulnar nerve injuries (Table 4), the test group exhibited significantly greater improvements compared to the control group in DML at 1 month (p = 0.003) and 3 months (p = 0.004), DSL at 1 month (p = 0.028) and 3 months (p < 0.001), MCV at 3 months (p = 0.001), SNAP at 3 months (p = 0.011), and SCV at 1 month (p = 0.004) and 3 months (p < 0.001). Changes in CMAP were not significantly different between the groups (p = 0.177 at 3 months).
Electrophysiological data for radial nerve injuries are presented in Table 5. Significant improvements in the test group compared to the control group were noted for DML at 3 months (p = 0.015), MCV at 3 months (p = 0.028), DSL at 1 month (p = 0.005) and 3 months (p = 0.002), and SCV at 1 month (p = 0.003) and 3 months (p < 0.001). No significant inter-group differences were found for changes in CMAP (p = 0.982 at 3 months) or SNAP (p = 0.426 at 3 months).
Clinical functional recovery
Clinical outcomes for median nerve injuries are detailed in Supplementary Table S1. Muscle strength recovery, assessed by MRC grades, was significantly better in the test group compared to the control group at 3 months postoperatively (p = 0.008). Sensory function recovery (MRC grades) was also significantly superior in the test group at both 1 month (p = 0.019) and 3 months (p = 0.020).
For ulnar nerve injuries (Supplementary Table S2), there were no statistically significant differences in the distribution of muscle strength grades (p = 0.181 at 3 months) or sensory function grades (p = 0.098 at 3 months) between the test and control groups at 3 months postoperatively.
Clinical recovery for radial nerve injuries is shown in Supplementary Table S3. Sensory function recovery (MRC grades) was significantly better in the test group compared to the control group at 3 months postoperatively (p = 0.030). No significant differences were found in muscle strength grade distributions between the two groups at 3 months (p = 0.803).
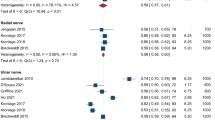
As shown in Fig. 3, there were no statistically significant differences in DASH scores between the test and control groups at any of these time points for median nerve injuries, ulnar nerve injuries, or radial nerve injuries (all p > 0.05).
Comparison of DASH scores for functional recovery in Test and Control groups after (A) median nerve, (B) ulnar nerve, and (C) radial nerve injury. ns indicates no significant difference (p > 0.05, using independent samples t-test for inter-group comparisons) between Test and Control groups at the respective time points.
Complications
The safety profiles of both treatment approaches were evaluated. Overall, the procedures were well-tolerated. No severe complications were observed in either the test group or the control group during the 3-month follow-up period.
Minor, transient complications were observed in a small number of patients across both groups. In the test group (n = 110), 3 (2.7%) patients reported mild, localized pain at the surgical site beyond the immediate postoperative period, which resolved within 1 week with oral analgesics. In the control group (n = 112), 4 (3.6%) patients reported similar mild, localized pain at the surgical site, also resolving with conservative management.
Discussion
The management of incomplete peripheral nerve injuries requiring epineurotomy remains a clinical challenge due to the risks associated with the procedure itself, including potential iatrogenic trauma and subsequent perineural scarring11,12,14,15,16,35,36. This study aimed to assess whether the adjunctive use of a BCANC combined with PRP following epineurotomy could offer a safer and more effective approach for these specific injuries. Our findings indicate that this combined treatment is safe and yields significant short-term electrophysiological improvements across median, ulnar, and radial nerve injuries, with nerve-dependent benefits in clinical sensory and motor function.
A key observation was the discernible electrophysiological recovery across the three assessed nerve types in the test group. These improvements in nerve conduction parameters suggest an underlying enhancement in axonal function and/or myelination. Such benefits may stem from the BCANC providing a protected microenvironment for nerve regeneration and minimizing external scar adhesion36,37,38,39, while PRP, rich in various growth factors, likely contributed by promoting local cellular processes essential for nerve repair, such as Schwann cell activity and neovascularization26,27,28,29,30. The containment of PRP within the conduit might also offer a more sustained release of these bioactive molecules, potentially amplifying their regenerative effects, a contrast to simple PRP injection where rapid dispersal can occur. The general lack of significant change in CMAP within the study timeframe might indicate that while nerve conduction efficiency improved, a substantial increase in the quantity of reinnervated motor units may require a longer observation period.
The clinical implications of these electrophysiological changes appeared nerve-specific. For median nerve injuries, the observed electrophysiological recovery was paralleled by significant improvements in both muscle strength and graded sensory function in the test group. Radial nerve injuries in the test group also showed significant clinical sensory recovery, although muscle strength improvements did not reach statistical significance within the 3-month follow-up. In contrast, for ulnar nerve injuries, the notable electrophysiological enhancements did not translate into statistically significant improvements in clinical muscle strength or sensory function grading during the observation period, though a trend towards sensory improvement was noted. Several factors may contribute to this, including the long regeneration distance to the intrinsic muscles of the hand, the ulnar nerve’s anatomical vulnerability, and the specific characteristics of hand intrinsic muscles which are challenging to reinnervate successfully40.
Despite these specific electrophysiological and clinical improvements, the overall upper extremity function, as measured by the DASH score, did not significantly differ between the test and control groups for any nerve type. This finding suggests that the DASH score, which assesses a broad range of activities, may not be sensitive enough to detect changes resulting from specific sensory or isolated motor improvements within a short timeframe, especially when more complex coordinated movements or overall strength might still be recovering or influenced by other factors. Nevertheless, the observed clinical sensory improvements, particularly for median and radial nerves, are highly valuable, as they can reduce the risk of secondary injuries, enhance fine motor coordination reliant on sensory feedback, and improve quality of life by potentially reducing neuropathic pain and discomfort. Early and robust sensory recovery might also create a more favorable environment for subsequent motor recovery by improving patient engagement in rehabilitation and providing essential feedback for motor learning, though this requires confirmation in longer-term studies.
The use of epineurotomy is often debated, with guidelines typically advising against its routine use. However, our study focused on a distinct population: patients with incomplete traumatic PNIs exhibiting significant structural epineurial pathology where external neurolysis alone was deemed insufficient. In such selected cases, epineurotomy may be necessary, and our approach of combining it with BCANC and PRP aims to mitigate its inherent risks. The principle of enriching the conduit microenvironment is supported by other studies, such as those using BDNF in nerve conduits, although in different injury models41. While the clinical application of PRP in nerve regeneration has shown variable results and remains a subject of discussion, our findings, particularly the nerve-specific clinical benefits, contribute positively to this debate, suggesting that the method of application (e.g., contained within a conduit) and patient selection are critical42. The safety profile of the combined intervention in our study was favorable, with no severe complications reported, aligning with previous studies on the biocompatibility of collagen conduits and autologous PRP27,37. This underscores the feasibility of the approach from a safety perspective.
This study has several limitations. Its retrospective design is susceptible to inherent biases. The 3-month follow-up period is relatively short for peripheral nerve regeneration, which can take many months or even years to reach its maximum potential; thus, long-term functional outcomes may not have been fully captured. We did not include groups treated with BCANC alone or PRP alone, making it difficult to dissect the individual contributions of each component. While we stratified by nerve type, heterogeneity within these groups (e.g., exact lesion length and specific muscles affected) might still exist. Furthermore, the extent of nerve ischemia at the time of injury or during the surgical procedure was not systematically evaluated or controlled for in this study, which can significantly impact nerve health and regenerative capacity. Potential confounding factors like variations in rehabilitation protocols or patient-specific NSAID use were not exhaustively controlled.
Clinically, these findings suggest that the combination of BCANC and PRP with epineurotomy may be a beneficial adjunctive treatment for carefully selected incomplete traumatic peripheral nerve injuries, with outcomes appearing to be nerve-dependent. Future research should focus on prospective randomized controlled trials with larger sample sizes for each nerve type, incorporating longer follow-up periods to assess sustained functional recovery and patient-reported outcomes.
Conclusion
In conclusion, this study demonstrates that combining BCANC and PRP with epineurotomy is a safe approach for incomplete traumatic peripheral nerve injuries with structural epineurial changes. This combination significantly enhances short-term electrophysiological recovery across median, ulnar, and radial nerves. Importantly, it also translates to tangible clinical benefits in muscle strength and sensory function for median nerve injuries and sensory function for radial nerve injuries. However, it must be emphasized that these are early findings, while promising for early nerve recovery, the true long-term efficacy and impact of this combined treatment await confirmation from more extensive and prolonged investigations.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PNI:
-
Peripheral nerve injuries
- CTS:
-
Carpal tunnel syndrome
- BCANC:
-
Bovine collagen artificial nerve conduit
- PRP:
-
Platelet-rich plasma
- EMG:
-
Electromyography
- DML:
-
Distal motor latency
- CMAP:
-
Compound muscle action potential amplitude
- MCV:
-
Motor conduction velocity
- DSL:
-
Distal sensory latency
- SNAP:
-
Sensory nerve action potential amplitude
- SCV:
-
Sensory conduction velocity
- DASH:
-
The disability of arm, shoulder, and hand questionnaire
- MRC:
-
The medical research council
- IQR:
-
Interquartile range
- BMI:
-
Body mass index
- ANC:
-
Absorbable nerve conduit
References
Jiang, M., Chen, M. & Liu, N. Interactions between Schwann cell and extracellular matrix in peripheral nerve regeneration. Front. Neurol. 15, 1372168 (2024).
Lanier, S. T., Hill, J. R., Dy, C. J. & Brogan, D. M. Evolving techniques in peripheral nerve regeneration. J. Hand Surg. Am. 46, 695–701 (2021).
Cook, H. et al. Does prophylactic decompression of distal nerves following nerve repair improve functional recovery? A systematic review. J. Plast. Reconstr. Aesthet. Surg. 91, 200–206 (2024).
Temiz, N. C. et al. Radial nerve injuries and outcomes: our surgical experience. Ulus Travma Acil Cerrahi Derg. 27, 690–696 (2021).
Lee, S. K. & Wolfe, S. W. Peripheral nerve injury and repair. J. Am. Acad. Orthop. Surg. 8, 243–252 (2000).
Kline, D. G. & Hudson, A. R. Nerve Injuries: Operative Results for Major Nerve Injuries, Entrapments, and Tumors (W.B. Saunders, 1995).
Patel, B. H., Ravella, K. C. & Gonzalez, M. H. Nerve compression syndromes of the upper extremity. Instr Course Lect. 72, 595–609 (2023).
Kim, J. et al. Outcome analysis of external neurolysis in Posture-Induced compressive peroneal neuropathy and the utility of magnetic resonance imaging in the treatment process. J. Korean Neurosurg. Soc. 66, 324–331 (2023).
Borisch, N. & Haussmann, P. Neurophysiological recovery after open carpal tunnel decompression: comparison of simple decompression and decompression with epineurotomy. J. Hand Surg. Br. 28, 450–454 (2003).
Scholten, R. J. P. M., van der Mink, A., Uitdehaag, B. M. J., Bouter, L. M. & de Vet, H. C. W. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev CD003905 (2007).
Keith, M. W. et al. Treatment of carpal tunnel syndrome. J. Am. Acad. Orthop. Surg. 17, 397–405 (2009).
Foulkes, G. D., Atkinson, R. E., Beuchel, C., Doyle, J. R. & Singer D. I. Outcome following epineurotomy in carpal tunnel syndrome: a prospective, randomized clinical trial. J. Hand Surg. Am. 19, 539–547 (1994).
Blair, W. F., Goetz, D. D., Ross, M. A., Steyers, C. M. & Chang, P. Carpal tunnel release with and without epineurotomy: a comparative prospective trial. J. Hand Surg. Am. 21, 655–661 (1996).
Leinberry, C. F., Hammond, N. L. & Siegfried, J. W. The role of epineurotomy in the operative treatment of carpal tunnel syndrome. J. Bone Joint Surg. Am. 79, 555–557 (1997).
Crnković, T. et al. The effect of epineurotomy on the median nerve volume after the carpal tunnel release: a prospective randomised double-blind controlled trial. Int. Orthop. 36, 1885–1892 (2012).
Azad, A., Lin, H., Green, S. M. & Posner, M. A. Adjunctive procedures for median nerve decompression in carpal tunnel syndrome an intraoperative somatosensory evoked potential study. Bull. Hosp. Jt. Dis. 80, 213–217 (2022).
Jacobson, L., Dengler, J. & Moore, A. M. Nerve entrapments. Clin. Plast. Surg. 47, 267–278 (2020).
Robinson, L. R. Traumatic injury to peripheral nerves. Muscle Nerve. 66, 661–670 (2022).
Jack, M. M., Smith, B. W. & Spinner, R. J. Neurosurgery for the neurologist: peripheral nerve injury and compression (What can be Fixed?). Neurol. Clin. 40, 283–295 (2022).
Houshyar, S., Bhattacharyya, A. & Shanks, R. Peripheral nerve conduit: materials and structures. ACS Chem. Neurosci. 10, 3349–3365 (2019).
Lopes, B. et al. Peripheral nerve injury treatments and advances: one health perspective. Int. J. Mol. Sci. 23, 918 (2022).
Vijayavenkataraman, S. Nerve guide conduits for peripheral nerve injury repair: A review on design, materials and fabrication methods. Acta Biomater. 106, 54–69 (2020).
Gupta, S., Paliczak, A. & Delgado, D. Evidence-based indications of platelet-rich plasma therapy. Expert Rev. Hematol. 14, 97–108 (2021).
Paichitrojjana, A. & Paichitrojjana, A. Platelet rich plasma and its use in hair regrowth: A review. Drug Des. Devel Ther. 16, 635–645 (2022).
Egierska, D., Perszke, M., Mazur, M. & Duś-Ilnicka, I. Platelet-rich plasma and platelet-rich fibrin in oral surgery: A narrative review. Dent. Med. Probl. 60, 177–186 (2023).
Zhang, Y. et al. Platelet-rich plasma-derived exosomes enhance mesenchymal stem cell paracrine function and nerve regeneration potential. Biochem. Biophys. Res. Commun. 699, 149496 (2024).
Wang, S., Liu, X. & Wang, Y. Evaluation of platelet-rich plasma therapy for peripheral nerve regeneration: A critical review of literature. Front. Bioeng. Biotechnol. 10, 808248 (2022).
Şahin, M. M. et al. Effects of Chitosan and platelet-rich plasma on facial nerve regeneration in an animal model. Eur. Arch. Otorhinolaryngol. 279, 987–994 (2022).
Yuan, B. et al. Platelet-rich plasma Gel-Loaded collagen/chitosan composite film accelerated rat sciatic nerve injury repair. ACS Omega. 8, 2931–2941 (2023).
Wang, S. L., Liu, X. L., Kang, Z. C. & Wang, Y. S. Platelet-rich plasma promotes peripheral nerve regeneration after sciatic nerve injury. Neural Regen Res. 18, 375–381 (2023).
Rashid, R. et al. The STROCSS 2024 guideline: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int. J. Surg. https://doi.org/10.1097/JS9.0000000000001268 (2024).
Smith, M. V., Calfee, R. P., Baumgarten, K. M., Brophy, R. H. & Wright, R. W. Upper extremity-specific measures of disability and outcomes in orthopaedic surgery. J. Bone Joint Surg. Am. 94, 277–285 (2012).
Wang, Y., Sunitha, M. & Chung, K. C. How to measure outcomes of peripheral nerve surgery. Hand Clin. 29, 349–361 (2013).
Vordemvenne, T., Langer, M., Ochman, S., Raschke, M. & Schult, M. Long-term results after primary microsurgical repair of ulnar and median nerve injuries. A comparison of common score systems. Clin. Neurol. Neurosurg. 109, 263–271 (2007).
Schmid, A. B., Fundaun, J. & Tampin, B. Entrapment neuropathies: a contemporary approach to pathophysiology, clinical assessment, and management. Pain Rep. 5, e829 (2020).
Bushnell, B. D., McWilliams, A. D., Whitener, G. B. & Messer, T. M. Early clinical experience with collagen nerve tubes in digital nerve repair. J. Hand. Surg. 33, 1081–1087 (2008).
Boeckstyns, M. E. H. et al. Collagen conduit versus microsurgical neurorrhaphy: 2-Year Follow-Up of a prospective, blinded clinical and electrophysiological multicenter randomized, controlled trial. J. Hand. Surg. 38, 2405–2411 (2013).
Alluin, O. et al. Functional recovery after peripheral nerve injury and implantation of a collagen guide. Biomaterials 30, 363–373 (2009).
Wangensteen, K. J. & Kalliainen, L. K. Collagen tube conduits in peripheral nerve repair: A retrospective analysis. Hand (N Y). 5, 273–277 (2010).
Ghoraba, S. M., Mahmoud, W. H., Elsergany, M. A. & Ayad, H. M. Ulnar nerve injuries (Sunderland grade V): A simplified classification system and treatment algorithm. Plast. Reconstr. Surg. Glob Open. 7, e2474 (2019).
Taifebagerlu, J. & Mohammadi, R. Effect of local administration of brain derived neurotrophic factor with silicone conduit on peripheral nerve regeneration: a rat sciatic nerve transection model. Iran. J. Veterinary Surg. 10, 43–52 (2015).
Jiang, J., Xing, F., Luo, R. & Liu, M. Effectiveness of Platelet-Rich plasma for patients with carpal tunnel syndrome: A systematic review and meta-Analysis of current evidence in randomized controlled trials. Front. Pharmacol. 13, 834213 (2022).
Funding
The study was supported by Special Fund for Clinical Research, Nanfang Hospital, Southern Medical University, No. 2022CR006; and President Foundation of Nanfang Hospital, Southern Medical University, No. 2020B028.
Author information
Authors and Affiliations
Contributions
SX wrote the original draft. SX, YZ, and PS performed the research. YZ and XT analyzed the data. JY designed the experiment and revised the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Nanfang Hospital (NFEC-2024-248). The requirement for informed patient consent was waived.
Consent for publication
This study has not been published before, and this publication has been approved by all authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xie, S., Zhang, Y., Shi, P. et al. Effectiveness of collagen nerve conduit combined with PRP for incomplete peripheral nerve injury: a retrospective case-control study. Sci Rep 15, 31931 (2025). https://doi.org/10.1038/s41598-025-09305-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09305-3