Abstract
Recently, superior capsule reconstruction (SCR) has achieved some results in the treatment of irreparable massive rotator cuff tears (IMRCT), but the incidence of various postoperative complications is high. The study aims to establish a model of IMRCT in rabbits, and compare the histomorphology and molecular biology differences between superior fulcrum reconstruction (SFR) and SCR, so as to provide a new and effective treatment method for the clinical treatment of IMRCT. Thirty-six mature New Zealand white rabbits were required for the experiment to build the model of IMRCT. The supraspinatus and subscapular muscle of the thirty-six rabbits were cut off and randomly divided into two groups of eighteen rabbits in each group, with SFR and SCR. Six rabbits in each group were sacrificed at 4, 8, and 12 weeks after surgery for histological and molecular assessment. Macroscopically, no retear occurred in SFR group and SCR group after surgery. The results of molecular biological showed that the expression levels of COL1, BMP2, SCX and SOX9 in the SFR group were significantly higher than those in the SCR group at 4 and 8 weeks (P < 0.05), while the expression of COL3 was lower than that in the SCR group. There was no significant difference in the expression of Aggrecan between the two groups at 4 weeks (P > 0.05). At 12 weeks after surgery, the expression levels of COL1, BMP2 and Aggrecan in the SFR group were significantly higher than those in the SCR group (P < 0.05), while COL3, SCX and SOX9 were not significantly difference between the two groups (P > 0.05). Histologically, collagen fiber maturity and fibrocartilage regeneration in the SFR group were superior to those in the SCR group at 8 and 12 weeks (P < 0.05). However, at 4 weeks, there was no significant difference between the two groups (P > 0.05). In an IMRCT rabbit model, healing processes of SFR and SCR are different, but both repair techniques were effective. SFR outperformed SCR in collagen fiber maturity, fibrocartilage regeneration, and tendon regeneration.
Similar content being viewed by others
Rotator cuff tears (RCTs) are among the most common disorders that result in shoulder pain and functional disabilities1,2. According to statistics3, 8% of the population in the United States is suffering from shoulder pain and dysfunction, the reason of which is about 50% caused by RCT. Due to economic constraints and uneven distribution of healthcare resources, many patients fail to receive timely intervention, resulting in progression from RCT to irreparable massive rotator cuff tears (IMRCTs)4. This ultimately leads to permanent functional impairment and irreversible joint degeneration5,6. Therefore, exploring effective treatment strategies for IMRCT is of paramount clinical importance.
The current treatments for IMRCT include partial repair6, tendon transfer7,8, superior capsule reconstruction (SCR)9 and reverse shoulder arthroplasty (RSA)10, etc. While tendon transfer demonstrates short-term functional benefits, their irreversible disruption of native shoulder anatomy and unproven long-term biomechanical efficacy lack robust evidence-based support11. Despite RSA being a more established procedure, is primarily indicated for elderly patients with low functional demands, significantly limiting its applicability in younger populations. Since Professor Mihata12 first proposed SCR and published his paper in 2012, SCR has attracted more and more clinical attention in recent years, but SCR demonstrates heterogeneous short-term outcomes, requires further validation of long-term efficacy, and remains constrained by limited graft thickness availability and potential long-term creep risks13,14, all of which compromise therapeutic stability. Recently, Ding15 et al. innovatively proposed a ‘sandwich’ composite graft technique (autologous fascia lata combined with artificial ligament). This novel material-composite reconstruction strategy enhances structural rigidity and creep resistance while maintaining adequate graft thickness16. However, several challenges remain, including donor-site morbidity associated with autograft harvest17, biological healing uncertainty at the graft-bone interface due to 'surface-contact’ fixation7, and the steep learning curve of this technically demanding procedure.
Addressing these limitations, Dr Ning team’s 2023 introduction of superior fulcrum reconstruction (SFR) technology18 achieved breakthrough innovations through biomechanical and tissue engineering advancements. This technique utilizes the peroneus longus tendon (PLT) to construct a suture-bridge-like structure at the proximal humerus, optimizing tendon-bone interface stress distribution via bone tunnel redesign. Compared to conventional techniques like SCR, this approach significantly simplifies surgical procedures and technical demands while demonstrating excellent functional recovery in clinical follow-up19. Subsequent biomechanical studies by Wang20 et al. have further validated the superior mechanical properties of this technique. From a biological healing perspective, the bone tunnel fixation method significantly enhances tendon-bone interface contact area, effectively addressing the issues of localized stress concentration and insufficient contact surface associated with traditional anchor fixation. These advantages have been conclusively demonstrated through both animal studies and biomechanical investigations21,22. Furthermore, as an autograft, PLT offers both biomechanical compatibility (high tensile strength and elastic modulus) and clinical practicality (low donor-site morbidity and excellent biocompatibility), with established successful applications in knee and ankle ligament reconstruction procedures23,24,25. The underlying pathophysiological mechanism of this technique may involve PLT promoting the regeneration of collagen fibers and cartilage at the tendon-bone interface through the establishment of bone tunnels, demonstrating better histological morphology and molecular expression compared to conventional reconstruction methods. To validate this hypothesis, we conducted animal model experiments and in-depth investigations into related pathophysiological markers, aiming to elucidate the application of SFR technology in IMRCT from the perspective of tissue microenvironment remodeling. The findings are reported as follows.
Materials and methods
Animal model setup
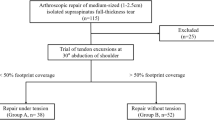
This study utilized New Zealand White rabbits as the experimental model. Based on established protocols from previous investigations in this field26,27, a total of 36 skeletally mature New Zealand White rabbits, with a mean body weight of 3.2 kg, were selected for the experiments. 36 rabbits were randomly allocated into two groups (n = 18 per group): the SFR group and the SCR group. Following the establishment of an IMRCT model, the SFR and SCR procedures were performed in the respective groups. Moreover, this study was approved by animal experiment ethics committee of our institution (LLSC-YY2019-54). In each group, six rabbits were euthanized at postoperative weeks 4, 8, and 12 (n = 6 per time point), with tendon-bone interface tissues harvested for molecular biological assays and histological analysis. (Fig. 1).
Based on previous study28, we established a rabbit model of IMRCT by creating injuries to both the supraspinatus and subscapularis tendons. All rabbits underwent right shoulder surgery following ≥ 6 h of preoperative fasting. Animals were secured on a sterile operating table and anesthetized via marginal ear vein injection of 20% urethane solution (5 mL/kg). Anesthesia depth was monitored by assessing pedal withdrawal reflex, corneal reflex, and muscle tone, with supplemental doses administered intraoperatively as needed. After achieving satisfactory anesthesia, rabbits were positioned in left lateral decubitus and received intravenous cefazolin sodium (50 mg/kg) for antimicrobial prophylaxis. Following standard skin preparation, disinfection, and draping centered on the supraspinatus-greater tuberosity junction, a 3-cm anterolateral longitudinal incision was made. After incising the skin and fascia, the deltoid muscle was bluntly dissected to expose the tendon insertions of both supraspinatus and subscapularis at the greater tuberosity. Using a No. 15 scalpel, we completely transected both tendon insertions and excised all surrounding tissue to create the IMRCT model.
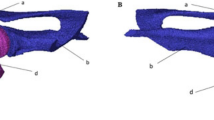
A 2-cm longitudinal incision was made approximately 3 cm medial to the lateral malleolus of the right hindlimb. After incising the skin, subcutaneous tissue and fascial layers were dissected layer by layer to fully expose the peroneus longus tendon (PLT). The PLT was carefully isolated, partially resected, and a 5-cm segment (approximately 2 mm in diameter) was completely excised. After achieving complete hemostasis in the surgical field, the fascia and skin were closed in layers. The wound was dressed with sterile compressive bandages. On the operating table, the harvested PLT was woven using 4–0 absorbable sutures, leaving 3-cm suture tails at both ends (Fig. 2A). The prepared tendon graft was preserved in saline-moistened gauze to maintain hydration until use. Following IMRCT establishment, two parallel 2.0-mm bone tunnels were established in the humeral head using K-wires, directed from intra-articular to extra-articular in an inferolateral trajectory. The intra-articular tunnel entries were spaced approximately 5.0 mm apart, while the extra-articular exits converged at a single point on the lateral aspect of the greater tuberosity (Fig. 2B). Subsequently, a 2.0-mm bone tunnel was created in the glenoid using K-wires, with the tunnel entrance and exit positioned at the 10:30 and 1:30 clock-face orientations respectively (Fig. 2C). Special care was taken to preserve the superior and lateral cortical bone during tunneling. Under traction assistance, the woven PLT graft was pulled through the glenoid bone tunnel into the joint cavity. Using traction sutures, both ends of the graft were then passed separately through the humeral head tunnels, creating a continuous path through: (1) the first humeral tunnel, (2) the glenoid tunnel, and (3) the second humeral tunnel. After tensioning the graft, all suture tails were secured with surgical knots at the convergent exit point on the lateral proximal humerus (Fig. 2D).
Surgical procedure. (A) The harvested tissue of autologous peroneus longus tendon was braided. (B) The bone tunnels were in the humeral head. (C)The bone tunnel was in the superior glenoid. (D) The braided autologous peroneus longus tendon passed the bone tunnels and was tied on the proximal lateral humerus. (E) The harvested tissue of autologous fascia lata. (F) The bone tunnel was in the humeral head. (G) The bone tunnel was in the superior glenoid. (H) The fixed fascia lata.
For SCR, we made a 3-cm longitudinal incision on the proximal lateral aspect of the right thigh and dissected through the subcutaneous tissue layer by layer to expose the fascia lata (FL). Using surgical scissors and a scalpel, we harvested a 10 × 10 mm FL graft (Fig. 2E). The harvested FL was then folded to double its thickness and preserved in saline-moistened sterile gauze to maintain its biomechanical integrity and hydration. Following IMRCT model establishment, a 10 × 1 mm bone tunnel perpendicular to the supraspinatus fiber orientation was created along the medial border of the humeral greater tuberosity and the superior glenoid rim (Fig. 2F). Additionally, two 1-mm diameter bone tunnels were prepared in the glenoid and greater tuberosity, respectively (Fig. 2G). The FL graft was secured to the superior glenoid using two No. 3 absorbable sutures, while its lateral end was fixed to the greater tuberosity via transosseous suture technique (Fig. 2H). After achieving complete hemostasis and copious irrigation with normal saline, the wound was closed in layers (fascia and skin) and dressed with sterile bandages. Postoperatively, rabbits were housed individually with unrestricted activity. For infection prophylaxis, intravenous cefazolin sodium (50 mg/kg) was administered daily for the first 3 days. All animals were closely monitored for mental status, food intake, and excretory function throughout the recovery period.
Histologic analysis
At 4, 8, and 12 weeks postoperatively, six rabbits from each SFR and SCR group were euthanized via CO₂ overdose, and the tendon-bone interface tissues were harvested. The collected specimens were fixed in 4% paraformaldehyde for 3 days, followed by decalcification in 10% ethylenediaminetetraacetic at room temperature for 30–35 days. After complete decalcification, the specimens were sequentially dehydrated through a graded ethanol series and subsequently embedded in paraffin. Coronal sections of 5 µm thickness were cut along the longitudinal axis of the humerus, then stained with hematoxylin and eosin (H&E) as well as Safranin O/Fast Green. Following staining, all specimens were examined under a light microscope (NI-U; Nikon) by two independent investigators who were blinded to the reconstruction methods.
Routine histological staining with hematoxylin and eosin (H&E) was performed to examine the tissue morphology at the tendon-bone healing interface. To quantitatively assess the healing process, we employed a modified tendon maturing scoring system29,30 incorporating six histologic parameters: cellularity, proportion of parallel cells, tenocytes, vascularity, fiber diameter and histological findings of tendon-to-bone insertion (Table 1). Safranin O/Fast Green staining was employed to evaluate fibrocartilage regeneration at the tendon-bone interface, where newly formed tissue appeared red against a green background31. Metachromasia served as the indicator for fibrocartilage formation in semi-quantitative analysis. Representative sections of the healing interface were selected, and metachromatic regions were carefully outlined under microscopy. Digital images were then imported into ImageJ software (National Institutes of Health, USA) for direct quantification.
Immunohistochemical analysis
Immunohistochemical staining was performed for collagen I (COL1) and collagen III (COL3) to evaluate the maturity of the tendon-to-bone healing process. The harvested specimens were fixed in 4% paraformaldehyde, dehydrated through a graded ethanol series, embedded in paraffin, and sectioned at 5 µm thickness. After deparaffinization, rehydration, and antigen retrieval in sodium citrate buffer (pH 6.0, 95 °C), sections were blocked with 10% goat serum. They were then incubated overnight at 4 °C with primary antibodies against COL1 (ab5315, Abcam) and COL3 (ab6647, Abcam), followed by 1-h incubation with biotinylated secondary antibodies at room temperature. The immunoreactivity was visualized using 3,3ʹ-diaminobenzidine (DAB) as the chromogen, with hematoxylin counterstaining applied to identify nuclei. Following dehydration through graded alcohols, clearing in xylene, and coverslipping, microscopic images were acquired for quantitative analysis of COL1 and COL3 expression levels.
Real-time quantitative reverse transcription PCR (qRT-PCR) analysis
Following euthanasia of six rabbits per group, the tendon-bone interface specimens were immediately harvested and pulverized under cryogenic conditions using a liquid nitrogen-cooled grinding mill to preserve RNA integrity32. We estimated the relative expression of collagen I (COL1), collagen III (COL3), bone morphogenetic protein 2(BMP2), SOX9, Scleraxis (SCX) and Aggrecan gene, which reflected collagen expression, bone formation, tendon regeneration and cartilage formation respectively33. The powdered tissue is quickly transferred into a centrifuge tube containing Trizol reagent and thoroughly homogenized to lyse the cells and release RNA34. Following the protocol of Trizol (Trizol, theero15596026) reagent, chloroform is added for phase separation, and the aqueous phase containing total RNA is collected after centrifugation. The aqueous phase is then transferred to a new tube, and RNA is precipitated using isopropanol. After washing to remove impurities, the RNA is dissolved in RNase-free water to obtain pure RNA samples. The purity and concentration of RNA are measured using a spectrophotometer to ensure suitability for downstream experiments. Subsequently, the extracted RNA is reverse transcribed into cDNA using a reverse transcription kit. In the qRT-PCR reaction system, the cDNA template, specific primers, and fluorescent dye are combined, and the optimized program is run on a real-time PCR machine to perform amplification reactions. β-actin served as the internal reference control. Primers for all genes are shown in Table 2. All experiments were performed in triplicate to determine mean gene expression levels.
Western blot analysis
The tissue specimens were ground into fine powder at 4℃, washed 3 times with PBS, treated with lysate, and centrifuged for 12,000 r/min for 20 min. The concentration of total protein in the supernatant was determined according to the instructions of bicinchoninic acid kit (Shanghai Beyotime Biotechnology Co, Ltd, Shanghai, China). Whole cell extracts of isolated muscle were prepared by radioimmunoprecipitation (RIPA) buffer (Elpis-Biotech). The protein was isolated by 15% SDS-PAGE and transferred to the nitrocellulose membrane. Similarly, we estimated the protein expression of COL1, COL3, BMP2, SCX, SOX9 and Aggrecan. The membrane was detected with anti-FABP4 or anti-A tubulin antibodies. Immunoreactive proteins were observed with the Amersham ECL kit according to the manufacturer’s instructions. The immunoreactive protein was detected by LAS-3000 image analyzer (Fuji Film). The protein content was determined by densitometry using Image J software (National Institutes of Health).
Statistical analysis
All statistical analyses were performed using GraphPad Prism software (version 8.0; GraphPad Software, San Diego, CA, USA). Data are presented as the mean ± standard deviation (SD). To determine statistical significance, a two-way analysis of variance (ANOVA) was employed, following by Bonferroni’s post hoc test for multiple comparisons between specific groups at individual time points. A probability value (p) of less than 0.05 was considered statistically significant for all analyses.
Results
Macroscopic observations
Postoperative observations revealed no signs of re-tears or infections in any of the experimental rabbits. During specimen collection, all grafts were maintained continuity with the humeral bone at the shoulders. Gross examination during necropsy showed no qualitative differences between the two shoulder groups or across different time points, as illustrated in Fig. 3.
Macroscopic view of the harvested specimens. (A) Gross specimen from the SFR group at 4 weeks. (B) Gross specimen from the SFR group at 8 weeks. (C) Gross specimen from the SFR group at 12 weeks. (D) Gross specimen from the SCR group at 4 weeks. (E) Gross specimen from the SCR group at 8 weeks. (F) Gross specimen from the SCR group at 12 weeks. SFR, superior fulcrum reconstruction; SCR, superior capsule reconstruction.
Histological analysis-H&E staining
H&E-stained sections revealed distinct differences in tendon-bone healing between groups (Fig. 4). At 4 weeks post-operation, the tendon-bone interface was identifiable, primarily composed of inflammatory cells and granulation tissue, without complete inflammatory cell infiltration. Both groups exhibited limited numbers of osteoblasts and chondrocytes. No significant difference was observed in tendon maturing score between the two groups (P > 0.05) (Table 3). By 8 weeks post-operation, inflammatory cell infiltration had diminished at the tendon-bone interface in both groups, with evident osteoblast and chondrocyte formation. In the SFR group, the healing interface exhibited structural similarity to native tendon-bone junctions, though cellular alignment remained irregular. In contrast, SCR specimens displayed persistent fibrovascular granulation tissue at the interface. The tendon maturing score was higher in the SFR group compared to the SCR group (P < 0.05). At 12 weeks, inflammatory cells were rarely observed in either group. The SFR group demonstrated a more mature tendon-bone interface with organized alignment of osteoblasts and chondrocytes. In contrast, the SCR group exhibited irregularly distributed chondrocytes at the healing interface. The tendon maturing score was significantly higher in the SFR group (P < 0.01, Table 3).
Comparison of healing interface maturity between SFR group and SCR group using hematoxylin and eosin–staining. (A) Tissue section of SFR group at 4 weeks. (B) Tissue section of SFR group at 8 weeks. (C) Tissue section of SFR group at 12 weeks. (D) Tissue section of SCR group at 4 weeks. (E) Tissue section of SCR group at 8 weeks. (F) Tissue section of SCR group at 12 weeks. (G) The graph shows the difference of the tendon maturing scores between groups. b, bone; i, interface; t, tendon; SFR, superior fulcrum reconstruction; SCR, superior capsule reconstruction. (100 × magnification, N = 6, *P < 0.05; **P < 0.01; ***P < 0.001).
Histological analysis-safranin O/fast green staining
Fibrocartilage formation at the tendon-bone interface was evaluated histologically using Safranin O/Fast Green staining, which selectively highlights proteoglycan-rich cartilage matrix (Safranin O, red) and collagenous tissue (Fast Green). This analysis revealed significant intergroup disparities in cartilage regeneration dynamics postoperatively (Fig. 5). While both cohorts exhibited a progressive increase in the Safranin O-positive area—indicative of nascent fibrocartilage—over the observation period, the SFR group consistently demonstrated a more extensive and intensely stained region compared to the SCR group. This qualitative observation suggested superior proteoglycan deposition and, by extension, enhanced fibrocartilage maturation capacity in the SFR group. Quantitative morphometric analysis corroborated these findings, confirming that the area of newly formed, structurally organized fibrocartilage was significantly greater in the SFR group relative to the SCR group at both 8 weeks (P < 0.001) and 12 weeks (P < 0.001). In contrast, no statistically significant difference in fibrocartilage area was detectable between groups at the 4-week time point (P > 0.05, Table 4), indicating comparable initial fibrocartilage formation potential during the early inflammatory and proliferative phases of healing.
Evaluation of fibrocartilage repair via Safranin O/Fast Green at the tendon-bone junction. (A) Tissue section of SFR group at 4 weeks. (B) Tissue section of SFR group at 8 weeks. (C) Tissue section of SFR group at 12 weeks. (D) Tissue section of SCR group at 4 weeks. (E) Tissue section of SCR group at 8 weeks. (F) Tissue section of SCR group at 12 weeks. (G) The graph shows the difference of the cartilage staining area between groups. b bone, i interface, t tendon, SFR superior fulcrum reconstruction, SCR superior capsule reconstruction. (100 × magnification, N = 6, *P < 0.05; **P < 0.01; ***P < 0.001).
Immunohistochemical analysis
Immunohistochemical analysis delineated a temporally progressive increase in COL1 deposition (Fig. 6A–F) concomitant with a gradual reduction in COL3 immunopositivity, predominantly localized within the newly formed fibrocartilage (Fig. 6G–L). This evolving collagen profile signifies the expected shift towards a more mature, load-bearing extracellular matrix during enthesis healing. Quantitative assessment revealed that the COL1 protein density at the healing interface was significantly higher in the SFR group relative to the SCR group at both the 8-week (P < 0.001) and 12-week (P < 0.001) time points (Table 5). However, no statistically significant intergroup difference in COL1 expression was detected at the 4-week assessment (P > 0.05), suggesting comparable early-stage collagen I synthesis. Conversely, for COL3, the immunohistochemical data consistently demonstrated lower collagen density in the SFR group across all postoperative intervals compared to the SCR group. While this trend was observable throughout, a statistically significant difference (P < 0.001) was only confirmed at the 8-week mark (Table 5). Collectively, these findings illustrate the characteristic transition from a COL3-rich provisional matrix towards a COL1-dominated mature scar during tendon-to-bone healing. The accelerated attenuation of COL3 coupled with the enhanced accumulation of COL1 observed in the SFR group implies a more favorable progression towards a mechanically competent tendon-bone interface.
Comparison of collagen expression between SFR group and SCR group using immunohistochemical staining, including COL1 (A–F) and COL3 (G–L). (A–C) Tissue sections of COL1 from the SFR group at 4, 8, and 12 weeks postoperatively. (D–F) Tissue sections of COL1 from the SCR group at 4, 8, and 12 weeks postoperatively. (G–I) Tissue sections of COL3 from the SFR group at 4, 8, and 12 weeks postoperatively. (J–L) Tissue sections of COL3 from the SCR group at 4, 8, and 12 weeks postoperatively. (M) The graph shows the difference of the collagen staining area of COL1 between groups. (N) The graph shows the difference of the collagen staining area of COL3 between groups. b bone, i interface, t tendon, SFR superior fulcrum reconstruction, SCR superior capsule reconstruction. (100 × magnification, N = 6, *P < 0.05; **P < 0.01; ***P < 0.001).
Gene and protein expression
qRT-PCR results demonstrated upregulation of all genes of interest at the repaired enthesis (Fig. 7). At 4 and 8 weeks, the SFR group exhibited higher mRNA expression levels of COL1, BMP2, SCX, and SOX9 compared to the SCR group (P < 0.05), while COL3 expression was lower in the SFR group. These findings indicate that the SFR group exhibited superior collagen synthesis, osteogenesis, and chondrogenesis during the early and intermediate healing phases. For the Aggrecan gene, no significant intergroup difference was observed at 4 weeks (P > 0.05), which may be attributed to the limited regenerative capacity of tendons during the early healing phase. By 12 weeks post-operation, the SFR group showed significantly elevated expression of COL1, BMP2, and Aggrecan (P < 0.05), whereas COL3, SCX, and SOX9 displayed no statistically significant differences between groups (P > 0.05). Western blot analysis (Fig. 8 and Fig. S1) corroborated the qRT-PCR findings, revealing higher protein expression of COL1, BMP2, and SCX in the SFR group at 4 and 8 weeks (P < 0.05). At the 12-week timepoint, BMP2 and Aggrecan protein levels peaked in the SFR group, suggesting more robust tendon regeneration and cartilage formation compared to the SCR group.
Protein expression analysis of COL1, COL3, BMP2, SCX, SOX9, and Aggrecan at the tendon-bone junction in the SFR and SCR groups. (A) The expression of various proteins 4 weeks after operation. (B) The expression of various proteins 8 weeks after operation. (C) The expression of various proteins 12 weeks after operation. All gels and blots are cropped, and the original gels and blots are presented in Supplementary Figure S1. SFR superior fulcrum reconstruction, SCR superior capsule reconstruction. (*P < 0.05; **P < 0.01; ***P < 0.001).
Discussion
In this study, to explore the clinical value of SFR, we established IMRCT in a rabbit model and conducted in-depth investigations into critical pathophysiological changes during tendon-bone healing. The results demonstrated that SFR outperformed SCR in collagen fiber maturity, fibrocartilage regeneration, and tendon regeneration, suggesting that optimized graft fixation and microenvironment remodeling through SFR technology can more effectively promote tendon-bone interface healing compared to SCR. These findings provide a robust molecular foundation and theoretical support for the clinical research conducted by Dr. Ning’s team18,19.
The incidence of IMRCT has been increasing annually and significantly compromises patients’ quality of life1. Consequently, the exploration of superior therapeutic approaches for IMRCT is of paramount importance. The ideal rotator cuff repair aims to restore the anatomical insertion point of the tendon-bone interface while reestablishing its inherent healing capacity and biomechanical functionality35. To achieve this goal, the reconstructed construct must possess sufficient initial mechanical strength to withstand tension at both the suture-tendon and tendon-bone interfaces during early healing phases, while preserving the biological potential essential for tendon-to-bone healing. Histological analysis in this study demonstrated that SFR achieved significantly higher tendon maturing scores and fibrocartilage regeneration rates compared to SCR at both 8 and 12 weeks postoperatively (Tables 3 and 4). These results align with the biological advantages of SFR’s bone tunnel design, which redistributes shear stress into compressive forces, as previously demonstrated by Bockmann et al.36. The suture-bridge-like configuration mimics the native enthesis structure, promoting organized collagen alignment and fibrocartilage formation37. In contrast, SCR group exhibited persistent fibrovascular granulation tissue at 8 weeks (Figs. 4 and 5), likely reflecting its reliance on surface-contact fixation. This fixation method fails to adequately address stress concentration—a limitation frequently reported in clinical studies of SCR 21,38. In the SFR group, the accelerated transition from COL3 to COL1 further supports its capacity to drive mature collagen remodeling (Fig. 6 and Table 5)—a critical determinant of biomechanical strength during tendon healing39. It is noteworthy that COL1 expression at 4 weeks demonstrated borderline statistical significance. While this did not reach the conventional threshold for statistical significance, the absolute expression values revealed a consistent trend toward higher COL1 levels in the SFR group compared to SCR group, suggesting a potentially enhanced tendon-to-bone healing capacity.
A favorable healing microenvironment plays a crucial role in the long-term recovery of IMRCT40. Molecular analyses in this study revealed significantly elevated expression of BMP2 and Aggrecan in the SFR group compared to SCR at both 8 and 12 weeks (P < 0.05) (Figs. 7 and 8), indicating enhanced osteochondral differentiation likely mediated by mechanotransduction pathways activated through PLT fixation within bone tunnels41. This molecular signature mirrors strategies in tissue engineering employing growth factor-embedded scaffolds42, while our SFR further incorporates the unique advantage of autologous PLT integration. We further evaluated the expression of key genes involved in embryonic development of the tendon-bone interface. Scleraxis (SCX), a tendon- and ligament-specific marker, is highly expressed in tendon progenitor cells43. The transcription factor SOX9 plays a pivotal role in organogenesis and cell lineage determination across multiple tissues, including ligaments44. Studies45 demonstrate that tendon cells originate from SOX9-expressing chondrogenic mesenchymal cells within cartilage primordia, which transition to tenocytes during or immediately after mesenchymal condensation. Once tendons form and attach to cartilage, SOX9-expressing cells in cartilage primordia no longer participate in subsequent developmental processes46. In this study, significantly elevated expression of both SOX9 and SCX was observed in the SFR group compared to SCR at 4 and 8 weeks (P < 0.05) (Figs. 7 and 8). This synergistic gene expression pattern molecularly corroborates SFR’s biological superiority in maintaining organized extracellular matrix deposition.
Distinct from the tendinous layers predominantly attaching to the greater tuberosity, the superior capsule constitutes an anatomically and histologically unique structure47. Ebrahimi et al.48 demonstrated that complete RCT are strongly associated with superior capsular compromise, emphasizing its critical role in maintaining glenohumeral stability and biomechanical function. Although SCR has emerged as a pivotal option for managing IMRCT in younger patients, its clinical utility remains constrained by graft availability and unpredictable long-term biomechanical stability. Denard et al.13 highlighted that SCR’s reliance on fascia lata grafts predisposes it to thinning and creep under cyclic loading. Recent clinical refinements, including the incorporation of tendon patches49 and acellular dermal matrices50, have partially mitigated these graft-related limitations. However, such modifications introduce novel challenges, notably immune rejection risks and escalating procedural costs. In this study, we reconstructed the superior capsule using the PLT to create a suture-bridge-like configuration (Fig. 2). As an autograft, PLT has demonstrated proven efficacy in ligament reconstruction and has been extensively validated in clinical practice51. Biomechanical studies52 indicate that maintaining graft tension at 24 N effectively restores the initial force vectors between the humeral head and scapula. The PLT’s ultimate tensile strength exceeding 4000 N53 provides a robust mechanical rationale for clinical reconstruction. Compared to procedures like SCR, which carry risks of donor-site complications (e.g., muscle herniation, phlebitis), anterolateral PLT harvesting significantly reduces postoperative morbidity while preserving lower limb functionality. Furthermore, the use of the peroneus longus tendon (PLT) as an autograft eliminates the risk of immune rejection associated with allografts or xenografts54. Mechanistically, the PLT functions similarly to a subacromial spacer by maintaining the critical humeral head depression effect; however, its non-absorbable nature circumvents the long-term uncertainties inherent to synthetic biodegradable spacers, which may lose mechanical integrity over time due to material degradation55. This dual advantage—biological compatibility and structural permanence—positions the PLT as an optimal graft choice for SFR, particularly in younger patients requiring durable solutions. The histological evidence of robust fibrocartilage regeneration at the tendon-bone interface in our SFR group (Fig. 5 and Table 4) further supports the PLT’s capacity to facilitate functional healing while maintaining its biomechanical role as a dynamic stabilizer.
With the increasing incidence of IMRCT, various surgical techniques including partial rotator cuff repair6, reverse shoulder arthroplasty (RSA)10, and tendon transfer7,8 have been developed. Among these, although partial rotator cuff repair is able to restore some shoulder function in some patients, the rate of postoperative retear is as high as 48.9%56, and the mechanism of failure may be the difficulty of the repaired tendon to withstand the complex biomechanical stresses of the shoulder, especially during high loads and dynamic activities.
RSA57 represents a definitive surgical option for IMRCT, yet its application must adhere to strict indication criteria. This procedure is primarily recommended for elderly patients with significant glenohumeral joint degeneration and has been widely adopted in clinical practice. However, RSA is technically demanding, requiring meticulous intraoperative reconstruction of osseous structures, and is associated with substantial postoperative risks, including infection, prosthetic mechanical failure, and restricted range of motion—factors that collectively limit its broader utilization. In a 24-month follow-up study of 93 RSA cases by Wall et al.58, the overall complication rate reached 15%, with 5% of patients requiring prosthetic revision. Furthermore, revision surgeries in this population are particularly challenging due to inadequate scapular bone stock and the systematic scarcity of revision-specific implants. These constraints underscore the necessity for thorough risk–benefit analysis and stringent patient selection when considering RSA, particularly in younger patients or those with preserved joint kinematics.
For high-demand athletes or younger patients without severe glenohumeral arthritis, non-arthroplasty options including tendon transfer, SCR, or SFR should be prioritized over RSA. Among these, latissimus dorsi tendon transfer has been the conventional treatment for irreparable posterosuperior massive rotator cuff tears. Garcia et al.59 conducted a systematic review and meta-analysis evaluating mid- to long-term outcomes of this procedure across 11 studies published between 2006 and 2021. Their results demonstrated a mean improvement of 28 points in Constant-Murley scores postoperatively. However, a 13% complication rate underscores significant surgical risks, including surgical site infection, neuropraxia, hematoma, wound dehiscence, and transferred tendon rupture. Furthermore, the procedure’s impact on glenohumeral arthritis progression remains controversial, with conflicting evidence regarding its potential to accelerate joint degeneration. Elhassan et al.60 first reported the clinical application of lower trapezius tendon transfer for irreparable posterosuperior massive rotator cuff tears in 2016, demonstrating satisfactory short-term outcomes. However, this technique currently lacks validation through long-term follow-up studies and large-scale clinical trials. For younger patients with isolated irreparable anterosuperior rotator cuff tears, pectoralis major tendon transfer remains a commonly employed surgical option. The Resch team61 reported promising outcomes in their case series of 12 patients with pectoralis major tendon transfer, showing significant pain relief and improved Constant-Murley scores at 28-month follow-up. Nevertheless, subsequent studies by Luo et al.62,63 revealed diminishing improvements in both range of motion and internal rotation function over time.
Current clinical treatments for IMRCT exhibit limitations in postoperative efficacy and functional recovery. To address this, we designed and conducted a preliminary exploration of SFR for IMRCT using a rabbit model. Although inherent differences exist between rabbits and humans in tendon healing processes, the anatomical and morphological similarities support the translational relevance of this study. Consequently, our findings provide valuable preclinical evidence for the potential clinical application of SFR prior to human trials. SFR integrates the advantages of anatomical preservation from SCR, the biological regenerative potential of autologous tendon grafts, and the mechanical stability traditionally emphasized in RSA. Therefore, we posit that SFR holds broad clinical indications. With the increasing aging population, a growing number of elderly patients with IMRCT prefer non-replacement procedures, for whom SFR may serve as a novel therapeutic option. For high-demand populations such as athletes and younger patients (typically presenting acute injuries without fatty infiltration), SFR combined with rotator cuff repair could be considered. This hybrid approach not only utilizes the suture-bridge configuration to restore biomechanical leverage but also effectively reduces tension on the repaired tendons, thereby optimizing functional outcomes. However, its widespread clinical implementation will depend on overcoming challenges related to surgical precision requirements and age-associated osseous adaptations. Our current findings (demonstrating robust fibrocartilage regeneration and improved collagen organization at the tendon-bone interface) support a cautiously optimistic outlook for the long-term prognosis of SFR technology. The histological evidence of mature tendon-bone integration and molecular markers indicating active remodeling suggest durable biological fixation may be achievable. However, definitive clinical validation requires long-term follow-up studies to assess functional outcomes and graft survival rates in human applications.
The study has several limitations. Firstly, the primary focus was on histological and molecular biological assessments in this study, while biomechanical testing was not incorporated. Consequently, while structural improvements were observed in histological sections, we cannot establish whether these translate into enhanced functional outcomes at the healing enthesis. To further explore the therapeutic potential of SFR for clinical application, future studies incorporating biomechanical evaluations are essential to provide robust experimental evidence supporting clinical translation. Secondly, the sample size was relatively modest, and the experimental design lacked an untreated control group representing the intrinsic healing capacity of the rabbit rotator cuff tear model. Although the direct comparison between SFR and SCR techniques offers valuable insights into their relative efficacy, the absence of a baseline control precludes establishing a definitive biological baseline for spontaneous tendon-to-bone healing. Future investigations, particularly those including biomechanical assessments, will employ larger cohorts and incorporate appropriate control groups to yield more definitive results. Thirdly, while the findings from this rabbit model suggest the potential applicability of SFR for IMRCT, the inherent biological differences between rabbits and humans necessitate caution in direct extrapolation. Further preclinical studies in higher-order species and subsequent clinical investigations are warranted to validate the efficacy and safety of SFR before its potential adoption in human clinical practice. In light of the aforementioned findings, our subsequent investigations will prioritize a multidimensional analysis64,65 of the preliminary animal tissue sections with the assistance of artificial intelligence. This will be followed by systematic exploration of differentially expressed key signaling molecules and associated pathways. Subsequently, dynamic biomechanical assessments under physiological loading conditions will be conducted to evaluate the fixation efficacy of SFR during simulated motion. These integrative approaches aim to uncover fundamental insights into SFR-mediated tendon-bone healing, thereby establishing a robust scientific foundation for its clinical translation and informing the design of long-term follow-up protocols in human trials.
Conclusion
In an IMRCT rabbit model, healing processes of SFR and SCR are different, but both repair techniques were effective. SFR outperformed SCR in collagen fiber maturity, fibrocartilage regeneration, and tendon regeneration. Therefore, we provide a new treatment idea for the clinical treatment of IMRCT, and plan to carry out the application of this study in clinical treatment and observe the clinical treatment effect. In order to improve the clinical effect of the patients with IMRCT, and further improve the satisfaction of the patients.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Peng, Y. et al. Effect of mechanical stimulation combined with platelet-rich plasma on healing of the rotator cuff in a murine model. Am. J. Sports. 50(5), 1358–1368 (2022).
Morse, K. et al. Arthroscopic versus mini-open rotator cuff repair: A comprehensive review and meta-analysis. Am. J. Sports Med. 36(9), 1824–1828 (2008).
Lee, S., Park, I., Kim, M. S. & Shin, S. J. Clinical differences between patients with early and late revision surgery for symptomatic failed arthroscopic rotator cuff repair. Knee Surg. Sports Traumatol. Arthrosc. 29(12), 3921–3928 (2021).
Lebaschi, A. H. et al. Biomechanical, histologic, and molecular evaluation of tendon healing in a new murine model of rotator cuff repair. Arthroscopy 34(4), 1173–1183 (2018).
Kim, C., Lee, Y. J., Kim, S. J., Yoon, T. H. & Chun, Y. M. Bone marrow stimulation in arthroscopic repair for large to massive rotator cuff tears with incomplete footprint coverage. Am. J. Sports Med. 48(13), 3322–3327 (2020).
Hallock, J. D., Parsell, D. E. & Field, L. D. Partial rotator cuff repair for massive tears rarely require revision surgery. Arthrosc. Sports Med. Rehabil. 3(1), e121–e126 (2020).
John, R., Coady, C. M. & Wong, I. Revision of a failed latissimus dorsi transfer for a massive rotator cuff tear with arthroscopic anatomic bridging reconstruction using an acellular human dermal matrix allograft. Arthrosc. Tech. 8(10), e1171–e1179 (2019).
Osti, L. et al. Arthroscopic-assisted latissimus dorsi transfer for massive rotator cuff tear: A systematic review. Br. Med. Bull. 128(1), 23–35 (2018).
Sanchez, G. et al. Arthroscopic superior capsule reconstruction technique in the setting of a massive, irreparable rotator cuff tear. Arthrosc. Tech. 6(4), e1399–e1404 (2017).
Kobayashi, E. F. et al. Treatment of massive rotator cuff tears with reverse shoulder arthroplasty. Clin. Sports Med. 42(1), 157–173 (2023).
Moroder, P. et al. Long-term outcome after pectoralis major transfer for irreparable anterosuperior rotator cuff tears. J. Bone Joint Surg. Am. 99(3), 239–245 (2017).
Mihata, T. et al. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: A biomechanical cadaveric study. Am. J. Sports Med. 40, 2248–2255 (2012).
Denard, P. J. et al. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy 34, 93–99 (2018).
Woodmass, J. M. et al. Superior capsule reconstruction using dermal allograft: early outcomes and survival. J. Shoulder Elbow Surg. 28, 100–109 (2019).
Ding, S. et al. Arthroscopic superior capsular reconstruction using “sandwich” patch technique for irreparable rotator cuff tears. Arthrosc. Tech. 8(9), e953–e959 (2019).
Lin, J. et al. Outcome comparison of graft bridging and superior capsule reconstruction for large to massive rotator cuff tears: A systematic review. Am. J. Sports Med. 11, 2828–2838 (2020).
Azevedo, C. I. et al. Clinical importance of graft integrity in arthroscopic superior capsular reconstruction using a minimally invasively harvested midthigh fascia lata autograft: 3-year clinical and magnetic resonance imaging outcomes. Am. J. Sports Med. 48, 2115–2128 (2020).
Li, H. et al. Arthroscopic rotator cuff repair with superior fulcrum reconstruction using autologous ipsilateral peroneus longus tendon for irreparable massive rotator cuff tears. Arthrosc, Tech. 12(11), e2035–e2040 (2023).
Li, H., Fang, R. & Ning, R. Early effectiveness of arthroscopic superior fulcrum reconstruction in treatment of irreparable massive rotator cuff tear. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 37(12), 1453–1458 (2023) (Chinese).
Wang, K. et al. Modified superior capsule reconstruction using the peroneus longus for irreparable massive rotator-cuff tears: A cadaveric study. J. Back Musculoskelet. Rehabil. 38(2), 352–363 (2025).
Korth, K. et al. Histological and radiographic evaluation of three common tendon transfer techniques in an un-ossified bone porcine model: Implications for early anterior tibialis tendon transfers in children with clubfeet. J. Child. Orthop. 15(5), 443–450 (2021).
Zhao, F. et al. A more flattened bone tunnel has a positive effect on tendon-bone healing in the early period after ACL reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 27(11), 3543–3551 (2019).
Zhang, Q. et al. Arthroscopic reconstruction of the medial patellofemoral ligament in skeletally immature patients using the modified sling procedure: A novel technique for MPFL reconstruction. J. Orthop. Surg. Res. 18(1), 334 (2023).
Kim, H. N., Dong, Q., Hong, D. Y., Yoon, Y. H. & Park, Y. W. Percutaneous lateral ankle ligament reconstruction using a split peroneus longus tendon free graft: Technical tip. Foot Ankle Int. 35(10), 1082–1086 (2014).
Lui, T. H. Technical tips: reconstruction of deep and superficial deltoid ligaments by peroneus longus tendon in stage 4 posterior tibial tendon dysfunction. Foot Ankle Surg. 20(4), 295–297 (2014).
Xu, J. et al. Biceps augmentation outperforms tear completion repair or in situ repair for bursal-sided partial-thickness rotator cuff tears in a rabbit model. Am. J. Sports Med. 50(1), 195–207 (2022).
Li, X., Shen, P., Su, W., Zhao, S. & Zhao, J. Into-tunnel repair versus onto-surface repair for rotator cuff tears in a rabbit model. Am. J. Sports Med. 46(7), 1711–1719 (2018).
Yildiz, F. et al. Comparison of two different superior capsule reconstruction methods in the treatment of chronic irreparable rotator cuff tears: A biomechanical and histologic study in rabbit models. J. Shoulder Elbow Surg. 28(3), 530–538 (2019).
Ide, J. et al. Reconstruction of large rotator-cuff tears with acellular dermal matrix grafts in rats. J. Shoulder Elbow Surg. 18(2), 288–295 (2009).
Watkins, J. P., Auer, J. A., Gay, S. & Morgan, S. J. Healing of surgically created defects in the equine superficial digital flexor tendon: Collagen-type transformation and tissue morphologic reorganization. Am. J. Vet. Res. 46(10), 2091–2096 (1985).
Guo, J. et al. H-loop knotless double-row repair versus knotted suture bridge for rotator cuff tears: A biomechanical and histological study in an animal model. Am. J. Sports Med. 50(7), 1948–1959 (2022).
Shajib, M. S. et al. Method for manufacture and cryopreservation of cartilage microtissues. J. Tissue Eng. 14, 20417314231176900 (2023).
Rhee, S. M. et al. Allogeneic dermal fibroblasts improve tendon-to-bone healing in a rabbit model of chronic rotator cuff tear compared with platelet-rich plasma. Arthroscopy 38(7), 2118–2128 (2022).
Yang, B. H., Liu, B. S. & Chen, Z. L. DNA extraction with TRIzol reagent using a silica column. Anal. Sci. 37(7), 1033–1037 (2021).
Dornan, G. J. et al. Cost-effectiveness of arthroscopic rotator cuff repair versus reverse total shoulder arthroplasty for the treatment of massive rotator cuff tears in patients with pseudoparalysis and nonarthritic shoulders. Arthroscopy 33(4), 716–725 (2017).
Bockmann, B. et al. Bone tunnel placement influences shear stresses at the coracoid process after coracoclavicular ligament reconstruction: A finite element study and radiological analysis. Arch. Orthop. Trauma Surg. 143(2), 959–965 (2023).
Wolfson, T. et al. Arthroscopic reduction and internal fixation of tibial eminence fractures with transosseous suture bridge fixation. Arthrosc. Tech. 10(4), e1039–e1046 (2021).
Takayama, K., Yamada, S., Kobori, Y. & Shiode, H. Association between the postoperative condition of the subscapularis tendon and clinical outcomes after superior capsular reconstruction using autologous tensor fascia lata in patients with pseudoparalytic shoulder. Am. J. Sports Med. 48(8), 1812–1817 (2020).
Suh, D. S. et al. Atelocollagen enhances the healing of rotator cuff tendon in rabbit model. Am. J. Sports Med. 45, 2019–2027 (2017).
Consigliere, P. et al. Preliminary results of a consecutive series of large & massive rotator cuff tears treated with arthroscopic rotator cuff repairs augmented with extracellular matrix. Arch. Bone Jt. Surg. 5(1), 14–21 (2017).
Shuaib, A. et al. Heterogeneity in the mechanical properties of integrins determines mechanotransduction dynamics in bone osteoblasts. Sci. Rep. 9(1), 13113 (2019).
Sheehy, E. J., Kelly, D. J. & O’Brien, F. J. Biomaterial-based endochondral bone regeneration: A shift from traditional tissue engineering paradigms to developmentally inspired strategies. Mater. Today Bio. 3, 100009 (2019).
Schweitzer, R. et al. Analysis of the tendon cell fate 37 using Scleraxis, a specific marker for tendons and ligaments. Development 128, 3855–3866 (2001).
Nishimura, R. et al. Regulation of bone and cartilage development by network between BMP signalling and transcription factors. J. Biochem. 151, 247–254 (2012).
Liu, H. et al. Crucial transcription factors in tendon development and differentiation: Their potential for tendon regeneration. Cell Tissue Res. 356, 287–298 (2014).
Soeda, T. et al. Sox9-expressing precursors are the cellular origin of the cruciate ligament of the knee joint and the limb tendons. Genesis 48, 635–644 (2010).
Kubo, H. et al. Histologic examination of the shoulder capsule shows new layer of elastic fibres between synovial and fibrous membrane. J. Orthop. 22, 251–255 (2020).
Ebrahimi, A. S. et al. Evaluation of conventional MR imaging of the shoulder in the diagnosis of lesions of the biceps pulley. Acad. Radiol. 31(8), 3327–3335 (2024).
Encalada-Diaz, I. et al. Rotator cuff repair augmentation using a novel polycarbonate polyurethane patch: preliminary results at 12 months’ follow-up. J. Shoulder Elbow Surg. 20(5), 788–794 (2011).
Hinz, M. et al. Superior capsular reconstruction using an acellular dermal xenograft or allograft improves shoulder function but is associated with a high graft failure rate. J. Clin. Med. 13(16), 4646 (2024).
Quinn, M. et al. Peroneus longus tendon autograft may present a viable alternative for anterior cruciate ligament reconstruction: A systematic review. Arthroscopy 40(4), 1366–1376 (2024).
Omid, R. et al. Biomechanical comparison between the trapezius transfer and latissimus transfer for irreparable posterosuperior rotator cuff tears. J. Shoulder Elbow Surg. 24(10), 1635–1643 (2015).
Shi, F. D. et al. Peroneus longus tendon autograft is a safe and effective alternative for anterior cruciate ligament reconstruction. J. Knee Surg. 32(8), 804–811 (2019).
Sommer, M. C. et al. Complications of superior capsule reconstruction for the treatment of functionally irreparable rotator cuff tears: A systematic review. Arthroscopy 37(9), 2960–2972 (2021).
Berthold, D. P. et al. A new approach to superior capsular reconstruction with hamstring allograft for irreparable posterosuperior rotator cuff tears: A dynamic biomechanical evaluation. J. Shoulder Elbow Surg. 30(7s), S38-s47 (2021).
Malahias, M. A. et al. Arthroscopic partial repair for massive rotator cuff tears: Does it work? A systematic review. Sports Med. Open. 5(1), 13 (2019).
StPierre, P. et al. Consensus statement on the treatment of massive irreparable rotator cuff tears: A Delphi approach by the Neer Circle of the American Shoulder and Elbow Surgeons. J. Shoulder Elbow Surg. 30(9), 1977–1989 (2021).
Wall, B. et al. Reverse total shoulder arthroplasty: A review of results according to etiology. J. Bone Joint Surg. Am. 89(7), 1476–1485 (2007).
Velasquez, G. A. et al. Mid- to long-term outcomes of latissimus dorsi tendon transfer for massive irreparable posterosuperior rotator cuff tears: A systematic review and meta-analysis. J. Shoulder Elbow Surg. 33(4), 959–974 (2024).
Elhassan, B. T., Wagner, E. R. & Werthel, J. D. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J. Shoulder Elbow Surg. 25(8), 1346–1353 (2016).
Resch, H. et al. Transfer of the pectoralis major muscle for the treatment of irreparable rupture of the subscapularis tendon. J. Bone Jt. Surg. Am. 82(3), 372–382 (2000).
Luo, Z. et al. Outcome comparison of latissimus dorsi transfer and pectoralis major transfer for irreparable subscapularis tendon tear: A systematic review. Am. J. Sports Med. 50(7), 2032–2041 (2022).
Ernstbrunner, L. et al. Long-term outcomes of pectoralis major transfer for the treatment of irreparable subscapularis tears: Results after a mean follow-up of 20 years. J. Bone Jt. Surg. Am. 101(23), 2091–2100 (2019).
Zhang, X., Wang, T., Luo, W. & Huang, P. Multi-level fusion and attention-guided CNN for image dehazing. IEEE Trans. Circuits Syst. Video Technol. 31, 4162–4173 (2021).
Liu, W. et al. Pair-based uncertainty and diversity promoting early active learning for person re-identification. ACM Trans. Intell. Syst. Technol. 11(2), 21 (2020).
Acknowledgements
The authors would like to thank all staff members in the participating departments.
Funding
This study was funded by Hefei Science and Technology Bureau 202104j01- Population Health special Project and the Health Research Project of Health Commission of Anhui Province (No. AHWJ2024Aa30021).
Author information
Authors and Affiliations
Contributions
RDN and LCK designed and directed the study. CP conducted the study and wrote the manuscript. HYL and KHW collected and analyzed the data. LCK and GC reviewed and edited the manuscript. All authors read and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All the methods and experiments of this study were carried out in accordance with the relevant guidelines and regulations of Anhui Medical University. Moreover, the present animal study was performed in accordance with the guidelines and approval of the Institutional Animal Care and Use Committees (IACUCs) of Anhui Medical University. This study was conducted in accordance with the ethical standards set forth in the Declaration of Helsinki and its later amendments or comparable ethical standards. Moreover, our study is reported in accordance with ARRIVE guidelines. All procedures involving animal participants were approved by the Ethics Committee of The First People’s Hospital of Hefei (LLSC-YY2019-54).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Peng, C., Li, H., Wang, K. et al. Superior fulcrum reconstruction improve tendon-to-bone healing in irreparable massive rotator cuff tears compared with superior capsule reconstruction. Sci Rep 15, 21285 (2025). https://doi.org/10.1038/s41598-025-09329-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09329-9