Abstract
This study is targeted to explore the relationship between exposure to various air pollutants (PM1, PM2.5, PM10, O3, and NO2) and hypertension risk, and to assess the role of physical activity in this relationship among Chinese adults. The association between multiple ambient air pollutants (with separate models for each pollutant) and hypertension was explored using time-varying Cox proportional hazards regression models, adjusted for season, spatial autocorrelation, demographic, socioeconomic, and behavioral factors. The median follow-up was 4 years. The interaction tests revealed significant interactions between physical activity and exposure to PM1, PM2.5, PM10, and NO2, but not for O3 (P > 0.05). Physically active participants did not show significant increases in hypertension risk from pollutants. In contrast, inactive participants faced higher risks: PM1 (12.9%), PM2.5 (6.0%), PM10 (5.0%), NO2 (17.0%). Finally, in the multiple pollutant models, controlling for NO2 nullified the significance of PM1 and PM2.5, while adjusting for O3 increased their HRs. PM10 and O3 remained significant in all models, and adjusting for PM10 or both PM10 and O3 eliminated the significance of NO2. Higher concentrations of air pollution were linked to a heightened risk of developing hypertension among Chinese adults; however, physical activity may help mitigate this elevated risk.
Similar content being viewed by others
Introduction
Hypertension is a significant contributing factor and a key element of cardiovascular diseases. Over the past few decades, as a result of economic progress and changes in societal lifestyles, the worldwide prevalence of hypertension has doubled between 1990 and 20191. Research indicates that in 2010, 31.1% of the world’s adult population suffered from hypertension, with the prevalence steadily rising in middle and low-income nations2. Findings from the 2017 China Disease Burden Study revealed that hypertension was the primary cause of disability-adjusted life years (DALYs) loss. It resulted in 2.54 million deaths in China, with 95.7% of these deaths attributed to cardiovascular disease, imposing a substantial economic burden on the Chinese healthcare system3. Despite this, hypertension continues to be the leading preventable cause of premature death and disability globally. Hence, it is imperative to identify feasible, population-oriented, and cost-efficient methods to mitigate hypertension2,4.
Numerous investigations have established that exercise, an adaptable and acceptable lifestyle choice, is crucial in managing hypertension, which is closely tied to a sedentary lifestyle and physical activity (PA)5,6. A chronic deficiency in PA or a sedentary lifestyle is one of the contributing factors to hypertension7. Engaging in moderate PA can help reduce blood pressure and enhance cardiovascular health. Physical activity benefits heart function, inhibits insulin resistance and inflammation, encourages vasodilation, and decreases blood resistance8,9. In addition, the weight loss and reduction in anxiety and depression associated with PA can also contribute to lowering blood pressure10,11. Furthermore, some research suggests a potential link between air pollution and hypertension, though conclusions vary significantly and most studies are cross-sectional12. Air pollution primarily consists of particles and various gases13, with these tiny solid particles categorized by size: less than 1 micron (PM1), less than 10 microns (PM10), and less than 2.5 microns (PM2.5)14. Primary contributors to air pollution in the form of gaseous components are nitrogen oxides (NOX) and nitrogen dioxide (NO2), both of which are generated through the combustion of fossil fuels at elevated temperatures15. Ozone (O3) is also a significant air pollutant, and its environmental concentration has risen in recent years. In 2017, O3 pollution caused one-fourth of the global deaths attributed to it in China16. However, cohort studies specifically examining the relationship between distinct air pollutants and hypertension are limited, and the current evidence remains inadequate.
Some experimental studies have shown that the rise in cardiovascular disease burden caused by air pollutants is connected to oxidative stress and systemic inflammation17. It is speculated that moderate physical activity might alleviate the negative impacts of air pollutants. Nonetheless, some studies have suggested that increased physical activity could elevate exposure to air pollutants, given that most physical activities are typically performed outdoors, particularly by older adults18,19. The effect of physical activity on the association between air pollutants and cardiovascular disease or hypertension within the context of air pollution is a crucial topic for discussion, as it pertains to the development of public health guidelines and interventions20. If physical activity can counteract the detrimental effects of air pollutants on hypertension, then encouraging physical activity remains advantageous. Conversely, if air pollution significantly reduces the health benefits of physical activity, steps should be taken to minimize pollution exposure during outdoor activities or to enhance air quality, ensuring individuals can safely participate in physical activity21,22. To address these gaps, we aim to explore the longitudinal association between various air pollutants and the risk of hypertension and to assess the role of physical activity in this relationship, using an extensive cohort study of Chinese adults whose age were equal to or over than 45 years old.
Methodology
Study population and procedures
The China Health and Retirement Longitudinal Study (CHARLS) is managed and directed by the National Development Institute at Peking University23. The main objective of CHARLS was to gather and analyze the health, socioeconomic, and demographic details of individuals aged 45 and above residing in various communities across China. Launched in 2011, the initial CHARLS survey was carried out through household interviews, utilizing a comprehensive approach that combined multi-stage, stratified, and clustered sampling across 150 counties in 28 provinces and cities nationwide. Subsequent surveys took place in 2013, 2015, 2018, and 2020, adding further socio-demographic data along with physical, biological, and health assessments.
In this research study, subjects were tracked using their unique ID over five distinct waves of the survey conducted in 2011, 2013, 2015, 2018, and 2020. The baseline (2011) included 13,900 participants. Exclusions were made for those who were classified as having hypertension at baseline (n = 374), as well as for participants with missing data on hypertension (n = 174), air pollutants (n = 21), and/or covariates (n = 5,702) in any of the waves. This resulted in a final sample size of 7,629 participants for analysis. During follow-up, 634 participants (8.3% of the analytical sample) were lost to follow-up, primarily due to out-migration or refusal to continue. To minimize attrition bias, CHARLS has attempted to re-contact these individuals via telephone calls, mailed reminders, and home visits conducted by local community health workers. Participants who could not be reached after these efforts were censored at the date of their last completed survey wave. Subsequently, the Last Observation Carried Forward (LOCF) imputation method was utilized to estimate partially missing covariate data. For gender and age variables, data reported in any wave were used to logically infer the corresponding data for other waves. All other covariates were filled in using the 2011 baseline data, as most conditions remained stable or showed minimal changes over time24 (Fig. 1).
Exposure: PM1, PM2.5, PM10, O3, and NO2
High-resolution, annual data on PM1, PM2.5, PM10, and O3 at a 1 km scale in China from January 2010 to December 2020, along with NO2 data from January 2019 to December 2020, and high-resolution, annual NO2 data at a 10 km scale from January 2010 to December 201825,26, were sourced from the China High Air Pollutants (CHAP) datasets (https://weijing-rs.github.io/product.html). The CHAP dataset is a robust and reliable source of air pollution data for China and has been extensively used in numerous related studies27,28. Due to the lag effect of air pollutant exposure, each individual was assigned the previous year’s annual average exposure concentration (µg/m³) for various air pollutants, based on the geocoding of their residential addresses29,30. For instance, the 2010 annual average concentrations of the five air pollutants were used to align with the 2011 wave data in CHARLS.
Outcome: hypertension
All hypertensive cases were identified exclusively via self-report, based on question DA003 in the questionnaire: “Have you ever been diagnosed with hypertension by a doctor or physician?” Participants who responded “Yes” were classified as hypertensive at the wave corresponding to their first positive report. Participants who responded “No” or whose response was missing were treated as non-hypertensive until (and unless) they subsequently reported a diagnosis in a later wave. Baseline data were gathered in 2011, and all participants were monitored for the first occurrence of hypertension until the 2020 wave or until the occurrence of a hypertension event, death, or loss of follow-up. Individuals who joined the study after 2011 were excluded from the analysis. Hypertension was identified when two or more instances were recorded, with the first documented instance marking a singular hypertension event, serving as the study’s endpoint. If this endpoint was not reached, the last follow-up date from the 2020 wave was considered the end of the follow-up period.
Interaction: physical activity
The survey designed to assess the physical activity levels of participants was based on the International Physical Activity Questionnaire (IPAQ). During the five survey waves from 2011 to 2020, participants were asked about their engagement in physical activities lasting at least 10 min each. These activities were classified into categories such as vigorous (carrying heavy loads, excavating, cultivating, doing aerobic exercises, cycling rapidly, or bicycling with cargo), moderate (carrying lighter items, cycling at a normal pace, mopping, practicing tai chi, or walking briskly), and low-intensity activities (walking at work or home, as well as walking for recreation, exercise leisurely). The survey also gathered information on the frequency of these activities, ranging from once to seven times per week, and their daily duration, categorized into segments (> 10 min but < 30 min, ≥ 30 min but < 2 h, ≥ 2 h but < 4 h, and ≥ 4 h).
For consistency in analysis and due to the absence of specific time durations in the questionnaire, we adopted a median value approach as used by other researchers31,32. Thus, the time segments were interpreted as follows: more than 10 min but less than 30 min as 20 min, over 30 min but under two hours as 75 min, between two to four hours as 180 min, and more than four hours as 240 min. The cumulative weekly duration scores for each level of physical activity were calculated by multiplying the number of days the activity was performed by the median time spent on that activity per day. The overall score for physical activity volume (PAV) was represented using the metabolic equivalent (MET)33. It was computed as follows: PAV equals 8.0 times the score for weekly vigorous physical activity duration plus 4.0 times the score for weekly moderate physical activity duration plus 3.3 times the score for weekly low-intensity physical activity duration. As per the IPAQ guidelines, a total PAV falling below 600 MET-minutes per week was classified as physical inactivity (PI)32.
Our study examined the interactions between physical activity (both physically inactive and physically active) and PM1, PM2.5, PM10, O3, and NO2. We also analyzed the relationship and effect values of air pollutant exposure and the risk of hypertension under different physical activity statuses for each type of air pollutant.
Cofounders
Confounders were selected based on previous research and included the following variables: (1) demographic factors, including age group (< 70 years old, 70–80 years old, ≥ 80 years old), gender (male or female), educational level (illiterate, primary school and below, middle school and high school, technical school and above), residence (urban or rural), marital status (married or unmarried); (2) health-related behavior factors, including smoking status (still smoking, former smoking, and never smoking), alcohol consumption (current drinking, non-drinking), sleep duration (short, nighttime sleep duration < 7 h; normal, nighttime sleep duration 7–9 h; long, nighttime sleep duration > 9 h) and physical activity (physical inactivity and physically active); (3) socioeconomic variables, including medical insurance (Non-medical insurance-NMI; Urban employee medical insurance-UEMI; Urban resident medical insurance-URMI; Urban and rural resident medical insurance-URRMI; New cooperative medical insurance-NCMI), income (based on the quintiles of personal annual income for the five waves of the 10,301 participants included, specifically: Quintile 1, personal annual income of 0 to 2,880¥; Quintile 2, personal annual income of 2,880¥ to 11,000¥; Quintile 3, personal annual income of 11,000¥ to 21,900¥; Quintile 4, personal annual income of 21,900¥ to 41,000¥; Quintile 5, personal annual income of greater than 41,000¥); employment status (unemployed, agricultural job, non-agricultural job). (4) Seasonal and spatial autocorrelation factors: interactions between natural cubic splines of latitude and longitude, year, month, and city.
Statistical analysis
The baseline characteristics of study participants were described using frequency (n) and percentage (%), stratified by hypertension status (non-hypertension and hypertension). Given the large sample size in this study, the Kolmogorov-Smirnov test was employed to assess the normality of the annual average concentrations of various pollutants34. If the distribution was normal, the mean and standard deviation of the respective pollutant were reported. For skewed distributions, the median (25th percentile, 75th percentile) was presented instead. Additionally, for skewed distributions, box plots were used to display the median, quartiles, minimum value, maximum value, and any potential outliers.
Cox proportional hazard models were employed separately for each air pollutant to investigate the association between air pollutants exposure and hypertension risk, using the survey waves as the timescale. However, significant variations in the annual average concentrations of air pollutants between survey waves posed a challenge in defining consistent exposure, potentially introducing immortal time bias35. To address this, Cox regression with time-varying exposure and confounders was performed to avoid this bias24,36. Several models were constructed as follows.
Model 1: Crude (unadjusted).
Model 2: Adjusted for age group and gender.
Model 3: Adjusted for socioeconomic status (SES) factors (educational level, residence, marital status, medical insurance, income, employment status) and season and spatial autocorrelation (incorporating interaction between natural cubic splines of latitude and longitude, and year, month, city as factors to account for potential seasonality and residual confounders).
Model 4: Further adjusted Model 3 for behavioral factors (smoking status, alcohol consumption, sleep duration, and physical activity).
Hazard ratios (HR) and 95% confidence intervals (CIs) were calculated and reported. The analyses above were based on single air pollutant models. Concurrently, natural cubic splines were used to explore the relationship between air pollutants (PM1, PM2.5, PM10, O3, and NO2) and hypertension.
To evaluate the non-linearity in the relationship between air pollutant exposure and hypertension risk, two Cox proportional hazards models with time-varying exposure were fitted: one with a linear term for each air pollutant and another with a natural spline term for air pollutants, both based on Model 4. A likelihood ratio test was then performed to compare the two models, and a significant P-value from this test indicated evidence of non-linearity.
Subsequently, multiple pollutant models, including two-pollutant and three-pollutant models, were utilized, and sensitivity analyses were conducted based on Model 4, which controls for all confounding factors. Additionally, we evaluated the interactions between each air pollutant exposure and physical activity levels (physical inactivity and physically active) and conducted interaction comparisons under different models using the Wald test. Finally, subgroup analyses were performed based on these stratifications, controlling for all confounders.
All statistical analyses and figures were generated using Stata 16.0 (Stata Corporation, College Station, Texas, USA) and R software (version 4.3.2). P-value < 0.05 was deemed statistically significant.
Ethical considerations
The Biomedical Ethics Review Committee at Peking University (IRB00001052-11015) granted ethical approval for CHARLS. All participants provided informed consent. During data collection, individuals who reported a new physician diagnosis of hypertension were informed of their status by trained interviewers and advised to seek medical evaluation and management at local health facilities. Interviewers also provided standardized educational materials on blood pressure control and lifestyle modification. No additional clinical intervention was conducted as part of this research beyond the CHARLS standard follow-up procedures. All methods were performed in accordance with the relevant guidelines and regulations.
Results
Table 1 presents the baseline characteristics of included participants stratified by hypertension status (non-hypertension and hypertension). Among the 7,629 eligible participants, 7,386 (96.8%) were classified as non-hypertensive, while 243 (3.2%) were identified as hypertensive. Compared to the non-hypertensive group, hypertensive participants were more likely to be female, older, have a technical school education level or higher, be unmarried, reside in urban areas, be former smokers, abstain from alcohol, have UEMI, URRMI, and URMI medical insurance, fall within the lowest income quintile of 0 to 2,880¥, be unemployed, and be physically inactive.
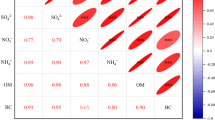
Based on the results of Kolmogorov-Smirnov test, the distributions of the annual average concentrations of all air pollutants do not follow a normal distribution (P < 0.05). Consequently, throughout the entire follow-up period, the annual average concentrations of PM1, PM2.5, PM10, O3 and NO2 were reported as medians (25th percentile, 75th percentile): 25.3 (18.3, 33.3) µg/m³, 44.1 (32.0, 59.4) µg/m³, 76.5 (53.7, 103.6) µg/m³, 88.0 (81.6, 96.8) µg/m³, and 25.8 (19.4, 33.4) µg/m³, respectively. Figure 2 further illustrates the annual average exposure concentration (µg/m³) of different air pollutants by hypertension status. It is evident that the exposure levels to the same air pollutants are generally similar among participants with different hypertension statuses. Over a median follow-up of 4 years (2 years, 7 years), a total of 243 participants (3.2%) developed hypertension. Simultaneously, after adjusting for all confounders (Model 4), for every ten unit increase in the annual average concentration of PM1, PM2.5, PM10, O3 and NO2 (10 µg/m3), the risk of hypertension increased by 14.6% (HR = 1.146, 95% CI 1.093–1.202), 7.0% (HR = 1.070, 95% CI 1.045–1.096), 5.2% (HR = 1.052, 95% CI 1.038–1.067), 4.9% (HR = 1.049, 95% CI 1.020–1.080), 18.2% (HR = 1.182, 95% CI 1.120–1.247), respectively. (Table 2). Figure 3 further shows the natural cubic splines of the annual average exposure concentration of all pollutants and the risk of hypertension. The P-nonlinearity for PM1, PM2.5, PM10, O3, and NO2 was > 0.001, > 0.001, > 0.001, 0.082, 0.010, respectively, indicating only a linear relationship between O3 and the risk of hypertension.
Dose-response relationship between exposure concentration of all pollutants and the hypertension risk among Chinese middle-aged and older individuals. (a) PM1, (b) PM2.5, (c) PM10, (d) O3 and (e) NO2. Adjusted for age group, gender, socioeconomic status (SES) factors (educational level, residence (urban or rural), marital status, medical insurance, income, employment status), season, and spatial autocorrelation, behavioral factors (smoking status, sleep duration, physical activity, and alcohol consumption).
Table 3 shows the analysis results of multiple pollutant models for sensitivity analysis. For PM1 and PM2.5, after controlling for NO2, the HRs were no longer statistically significant. However, after controlling for O3, the HRs were higher than in the single air pollutant model, while when controlling for both NO2 and O3, the HRs were lower than in the single air pollutant model. Simultaneously, for PM10 and O3, the HRs were statistically significant in any of the multiple pollutant models. However, for PM10, after controlling for NO2, the HRs were lower than in the single air pollutant model, while after controlling for other pollutants, the HRs were all higher than in the single air pollutant model. In contrast, for O3, after controlling for any other pollutants combination, the HRs were all higher than in the single air pollutant model. Lastly, for NO2, after controlling for PM10 or both PM10 and O3, the HRs were no longer statistically significant. However, except for the scenario where controlling for O3 resulted in higher HRs compared to the single air pollutant model, in all other remaining multiple pollutant combinations, the HRs were lower.
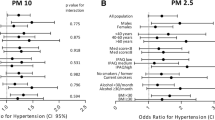
To quantify the independent effect of physical activity, we also fitted a Cox model adjusting for all confounders with Model IV. Compared with physically inactive participants, physically active participants had a significantly 11.4% lower risk of incident hypertension (HR = 0.886, 95% CI 0.858–0.916, P < 0.001). Simultaneously, the interaction tests for PM1, PM2.5, PM10, and NO2 with physical activity were significant (P for interaction: 0.003, 0.039, 0.011, and 0.001, respectively), and only O3 was not significant (P for interaction: 0.075). Further subgroup analysis showed that for physically active participants, the association between PM1, PM2.5, PM10, and NO2 exposure and the hypertension risk was not significant (P > 0.05). In contrast, for the physically inactive subgroup, PM1, PM2.5, PM10 and NO2 exposure significantly increased the risk of hypertension by 12.9% (HR = 1.129, 95% CI 1.071–1.189), 6.0% (HR = 1.060, 95% CI 1.032–1.088), 5.0% (HR = 1.050, 95% CI 1.034–1.066), 17.0% (HR = 1.170, 95% CI 1.103–1.241) (Fig. 4).
Subgroup analysis of the relationship of PM1, PM2.5, PM10, O3, and NO2 exposure (10 µg/m3) with the risk of hypertension in different physical activity among 7629 participants: the results of time-varying Cox regression analysis. Separate analyses were performed for each one of the pollutants and each analysis was adjusted for age group, gender, SES factors (educational level, residence, marital status, medical insurance, income, employment status), season and spatial autocorrelation, behavioural factors (smoking status, alcohol consumption, sleep duration and physical activity).
Discussion
As far as we are aware, this is the inaugural study to examine the relationship between exposure to multiple air pollutants and the hypertension risk, while also assessing the influence of physical activity on this association. This research is based on a large, long-term longitudinal cohort study of Chinese middle-aged and older individuals. Our findings demonstrate that increased exposure to numerous air pollutants such as PM1, PM2.5, PM10, O3, and NO2 is significantly correlated with a heightened risk of hypertension. After accounting for all confounding factors, NO2 was found to have the most pronounced effect on hypertension risk, followed by PM1, PM2.5, PM10, and O3, underscoring their individual contributions to the onset of hypertension. However, when compared to physical inactivity, engaging in physical activity notably reduces this risk across all the aforementioned air pollutants, including NO2, which has the most significant impact.
Our findings align with the results of numerous cross-sectional and cohort studies. For example, Wu et al. was based on 18,496 UK Biobank participants, suggested that air pollution exposure was a key factor in the development and progression of hypertension, diabetes, and chronic kidney disease37. A meta-analysis demonstrated that exposure to various ambient air pollutants was positively associated with hypertension. Specifically, brief exposure to air pollutants such as NO2, O3, and CO, as well as prolonged exposure to NOx, PM2.5, and SO2, were linked to an increased risk of hypertension38. Furthermore, a prospective cohort study of 39,259 individuals from rural Henan, China, showed that air pollutants and obesity metrics had an additive effect on hypertension39. We extend the available evidence while reporting novel results on the association between other pollutants such as PM1, PM10, O3, and NO2 and hypertension in middle-aged and older populations in China, and also further indicate the role of physical activity in this relationship. We observed that NO2 has the highest impact on the risk of developing hypertension, whereas O3 appears to have the lowest impact by comparison. A cross-sectional study involving 11,866 adults from the Korean National Health and Nutrition Examination Survey also supports our conclusion40. Data from 2,552 participants aged 31–72 from the Augsburg region of Germany indicate a stronger correlation between nitrogen dioxide and hypertension or diastolic blood pressure in men and diabetic patients41.
Although the exact mechanism linking air pollutants and hypertension remains unclear, one widely suggested hypothesis is that air pollutants can trigger the release of various inflammatory factors into the systemic circulation. This process can then induce systemic inflammation and oxidative stress, resulting in endothelial dysfunction, autonomic imbalance, and the progression of atherosclerosis42,43. However, engaging in moderate physical activity has the potential to mitigate this process to some extent. Hypertension was primarily attributed to vascular abnormalities such as endothelial dysfunction and impaired vascular smooth muscle function, along with autonomic nervous system dysfunction characterized by sympathetic overactivity. Physical activity was recognized to modulate blood pressure by engaging in these underlying mechanisms44,45. In a study involving middle-aged and elderly hypertensive individuals in China, the relationship between physical exercise and oxidative stress biomarkers was investigated. The research found that exercise reduced oxidative stress markers such as malondialdehyde and 4-hydroxy-2-nonenal, while enhancing the activity of superoxide dismutase, thereby lowering blood pressure46. However, high-intensity exercise may exacerbate oxidative stress. Another study by Ye et al. demonstrated that moderate-intensity aerobic training improved endothelial function and vasodilation by reducing oxidative stress and increasing NO levels in spontaneously hypertensive rats47. In contrast, high-intensity exercise increased ROS and decreased NO, worsening endothelial dysfunction and leading to vasoconstriction. Additionally, a meta-analysis of 27 randomized controlled trials has shown that regular moderate to high-intensity aerobic exercise can lead to an average reduction in blood pressure of 11/5 mm Hg (evidence level 3+)48.
The multiple pollutant models reveal that adjusting for NO2 negated the significance of PM1 and PM2.5, whereas controlling for O3 increased their HRs. PM10 and O3 remained significant across all models, and adjusting for PM10, or both PM10 and O3, eliminated the significance of NO2. This suggests potential collinearity between PM1, PM2.5, and NO2. A prior study examining the link between air pollution and emergency hospital admissions for hypertension in China reported similar findings49.
The strengths of this study include its longitudinal design, large and nationally representative sample from 28 provinces across mainland China, and relatively long follow-up period (median follow-up of 4 years, IQR 2–7 years). Additionally, the study explores the effects of multiple air pollutants on the risk of hypertension. However, there are also several limitations. Due to the lack of specific addresses, exposure to air pollutants was assessed at the city level, which may have resulted in exposure misclassification by ignoring within-city variations in air pollution. Although this oversight may not have changed the direction of the association between various air pollutants and hypertension, it could have introduced bias into the point estimate of the association and widened its uncertainty range. Previous evidence has indicated that city-level exposure assessments often lead to an underestimated association50. Moreover, all behavioral and health-related variables, including physical activity, smoking status, alcohol consumption, sleep duration, and hypertension diagnosis, were self-reported, which are inherently constrained by the potential for overestimation or underestimation due to social desirability, recall bias, and other influencing factors. However, to minimize subjective bias, CHARLS used validated instruments (IPAQ for physical activity), implemented standardized, staff-conducted interviews, and performed cross-wave consistency checks to flag implausible responses. Lastly, although a wide range of putative confounders have been adjusted for, residual confounding may still be present.
Our findings have significant implications for health policy and future research. Policymakers should consider the distinct effects of various air pollutants on hypertension when setting air quality standards and public health strategies. Targeted interventions to reduce exposure to harmful pollutants like NO2, PM1, PM2.5, and PM10 in vulnerable populations could help mitigate the risk of hypertension. Additionally, promoting moderate physical activity among middle-aged and older individuals is crucial, fostering a societal culture that values physical fitness. Even in the presence of air pollution, moderate physical activity can reduce the risk of hypertension associated with air pollutant exposure. In conclusion, managing air pollutant concentrations and encouraging moderate physical activity as modifiable risk factors for hypertension have substantial public health implications, potentially extending lifespan and promoting healthy aging.
Conclusion
Our study reveals a significant positive association between exposure to PM1, PM2.5, PM10, O3, and NO2 and the risk of hypertension in Chinese middle-aged and older adults. Notably, NO2 had the greatest impact on increasing the risk of hypertension, while O3 had the least effect. However, physical activity was found to mitigate this increased risk, reducing the effect of numerous air pollutant exposures on hypertension. Implementing targeted policies and interventions to reduce air pollution, along with encouraging regular physical activity, can potentially decrease the risk of hypertension, improve health outcomes, and promote healthy aging.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 398 (10304), 957–980 (2021).
MILLS K T et al. Global disparities of hypertension prevalence and control: A systematic analysis of Population-Based studies from 90 Countries. Circulation 134 (6), 441–450 (2016).
ZHOU, M. et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 394 (10204), 1145–1158 (2019).
MATHERS C D, K. O. N. T. I. S. V. et al. Contribution of six risk factors to achieving the 25×25 non-communicable disease mortality reduction target: a modelling study. Lancet 384 (9941), 427–437 (2014).
BADR H E, R. A. O. S. & MANEE, F. Gender differences in quality of life, physical activity, and risk of hypertension among sedentary occupation workers. Qual. Life Res. 30 (5), 1365–1377 (2021).
CAMõES, M. et al. Role of physical activity and diet in incidence of hypertension: a population-based study in Portuguese adults. Eur. J. Clin. Nutr. 64 (12), 1441–1449 (2010).
DIAZ K M, S. H. I. M. B. O. D. Physical activity and the prevention of hypertension. Curr. Hypertens. Rep. 15 (6), 659–668 (2013).
PEDRALLI M et al. Different exercise training modalities produce similar endothelial function improvements in individuals with prehypertension or hypertension: a randomized clinical trial exercise, endothelium and blood pressure. Sci. Rep. 10 (1), 7628 (2020).
NYBERG, M., GLIEMANN, L. & HELLSTEN, Y. Vascular function in health, hypertension, and diabetes: effect of physical activity on skeletal muscle microcirculation. Scand. J. Med. Sci. Sports. 25 (Suppl 4), 60–73 (2015).
Denche-Zamorano, A. et al. A Cross-Sectional study on the associations between depression and anxiety, medication use for these diseases and physical activity level in Spanish people with Hypertension. Int. J. Environ. Res. Public. Health 20 (3) (2023).
HALL M E, COHEN J B, ARD, J. D. et al. Weight-Loss strategies for prevention and treatment of hypertension: A scientific statement from the American heart Association. Hypertension 78 (5), e38–e50 (2021).
QIN, P. et al. Long-term association of ambient air pollution and hypertension in adults and in children: A systematic review and meta-analysis. Sci. Total Environ. 796, 148620 (2021).
BROOK, R. D., RAJAGOPALAN, S., POPE C, A. & 3RD. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American heart Association. Circulation 121 (21), 2331–2378 (2010).
RAJAGOPALAN, S. & AL-KINDI S G, BROOK, R. D. Air pollution and cardiovascular disease: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 72 (17), 2054–2070 (2018).
WOLF, K. et al. Long-term exposure to low-level ambient air pollution and incidence of stroke and coronary heart disease: a pooled analysis of six European cohorts within the ELAPSE project. Lancet Planet. Health. 5 (9), e620–e632 (2021).
Global National disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet 392 (10159), 1859–1922 (2018).
DE BONT, J. et al. Ambient air pollution and cardiovascular diseases: an umbrella review of systematic reviews and meta-analyses. J. Intern. Med. 291 (6), 779–800 (2022).
BONANNI L J, NEWMAN, J. D. Personal strategies to reduce the cardiovascular impacts of environmental Exposures. Circ. Res. 134 (9), 1197–1217 (2024).
BRANKSTON, G. et al. Increased weekly mean PM(2.5), and NO(2) are associated with increased proportions of lower airway granulocytes in Ontario Horses. Front. Vet. Sci. 7, 185 (2020).
CAI, C. et al. Long-term exposure to PM(2.5) chemical constituents and diabesity: evidence from a multi-center cohort study in China. Lancet Reg. Health West. Pac. 47, 101100 (2024).
LI, S. et al. Association between green space and multiple ambient air pollutants with depressive and anxiety symptoms among Chinese adolescents: the role of physical activity. Environ. Int. 189, 108796 (2024).
LIU, M. et al. Impact of green space exposure on blood pressure in guangzhou, china: mediation by air pollution, mental health, physical activity, and weight status. Environ. Pollut. 356, 124251 (2024).
FANCOURT, D. & NOGUCHI, T. Moderating effect of country-level health determinants on the association between hobby engagement and mental health: cross-cohort multi-level models, meta-analyses, and meta-regressions. Lancet 402 (Suppl 1), S41 (2023).
SUN, J. et al. Does social participation decrease the risk of frailty? Impacts of diversity in frequency and types of social participation on frailty in middle-aged and older populations. BMC Geriatr. 22 (1), 553 (2022).
WEI, J. et al. Ground-level gaseous pollutants (NO2, SO2, and CO) in china: daily seamless mapping and Spatiotemporal variations. Atmos. Chem. Phys. 23 (2), 1511–1532 (2023).
CHEN, Y. et al. Air pollution increases the risk of frailty: China health and retirement longitudinal study (CHARLS). J. Hazard. Mater. 492, 138105 (2025).
CHEN, N. et al. Association of household solid fuel use and long-term exposure to ambient air pollution with estimated 10-year high cardiovascular disease risk among postmenopausal women. Environ. Pollut. 342, 123091 (2024).
JIANG, H. et al. Does physical activity attenuate the association between ambient PM(2.5) and physical function?. Sci. Total Environ. 874, 162501 (2023).
ALEXEEFF, S. E. et al. Association of Long-term exposure to particulate air pollution with cardiovascular events in California. JAMA Netw. Open. 6 (2), e230561 (2023).
WANG, F. & YUAN, Z. The effects of meteorological factors and air pollutants on the incidence of tuberculosis in people living with HIV/AIDS in subtropical guangxi, China. BMC Public. Health. 24 (1), 1333 (2024).
Ding, M. et al. The Dose-Response relationships of different dimensions of physical activity with daily physical function and cognitive function in Chinese adults with hypertension: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 18 (23) (2021).
Tian, Y. & Shi, Z. Effects of physical activity on daily physical function in Chinese middle-aged and older adults: A longitudinal study from CHARLS. J. Clin. Med. 11 (21) (2022).
DENG, Y. The relationships between depressive symptoms, functional health status, physical activity, and the availability of recreational facilities: a Rural-Urban comparison in Middle-Aged and older Chinese Adults. Int. J. Behav. Med. 25 (3), 322–330 (2018).
MUMCU A K, KURNAZ, S. et al. Comparative effects of 17% Ethylenediaminetetraacetic acid and 9% etidronic acid applied with different irrigant activation techniques on the release of growth factors from dentin: in vitro study. BMC Oral Health. 24 (1), 612 (2024).
SUISSA S. Immortal time bias in pharmaco-epidemiology. Am. J. Epidemiol. 167 (4), 492–499 (2008).
ZHANG, Z. et al. Time-varying covariates and coefficients in Cox regression models. Ann. Transl Med. 6 (7), 121 (2018).
WU, G. et al. Ambient air pollution and incidence, progression to Multimorbidity and death of hypertension, diabetes, and chronic kidney disease: A National prospective cohort. Sci. Total Environ. 881, 163406 (2023).
CAI, Y. et al. Associations of Short-Term and Long-Term exposure to ambient air pollutants with hypertension: A systematic review and Meta-Analysis. Hypertension 68 (1), 62–70 (2016).
HOU, J. et al. Long-term exposure to air pollutants enhanced associations of obesity with blood pressure and hypertension. Clin. Nutr. 40 (4), 1442–1450 (2021).
KWAK, J. H. & KIM, H. J. The association between air pollutants exposure with Pre- and hypertension by vitamin C intakes in Korean adults: A Cross-Sectional study from the 2013–2016 Korea National health and nutrition Examination. J. Nutr. Health Aging. 27 (1), 21–29 (2023).
PITCHIKA, A. et al. Long-term associations of modeled and self-reported measures of exposure to air pollution and noise at residence on prevalent hypertension and blood pressure. Sci. Total Environ. 593–594, 337–346 (2017).
SONG, J. et al. Acute effect of ambient air pollution on hospitalization in patients with hypertension: A time-series study in shijiazhuang, China. Ecotoxicol. Environ. Saf. 170, 286–292 (2019).
CHEN, Z. et al. The underlying mechanism of PM2.5-induced ischemic stroke. Environ. Pollut. 310, 119827 (2022).
SABBAHI, A. et al. Exercise and hypertension: Uncovering the mechanisms of vascular Control. Prog Cardiovasc. Dis. 59 (3), 226–234 (2016).
MORAES-SILVA I C et al. Hypertension and exercise training: evidence from clinical Studies. Adv. Exp. Med. Biol. 1000, 65–84 (2017).
YU, Y. et al. Association between physical exercise and biomarkers of oxidative stress among middle-aged and elderly community residents with essential hypertension in China. Biomed. Res. Int. 2018, 4135104 (2018).
YE, F. et al. Impact of moderate- and high-intensity exercise on the endothelial ultrastructure and function in mesenteric arteries from hypertensive rats. Life Sci. 222, 36–45 (2019).
BöRJESSON, M. et al. Physical activity and exercise lower blood pressure in individuals with hypertension: narrative review of 27 RCTs. Br. J. Sports Med. 50 (6), 356–361 (2016).
GUO, Y. et al. Gaseous air pollution and emergency hospital visits for hypertension in beijing, china: a time-stratified case-crossover study. Environ. Health. 9, 57 (2010).
XUE, T. et al. Long-term PM(2.5) exposure and depressive symptoms in china: A quasi-experimental study. Lancet Reg. Health West. Pac. 6, 100079 (2021).
Funding
This work was funded by the following sources: (I) Natural Science Foundation of Hunan Province, China (Grant No. 2022JJ70059, 2025JJ70010); (II) Fundamental Research Funds for the Central Universities of Central South University (Grant No. 2022ZZTS0952); and (III) Horizontal project (Grant No. FW20230556).
Author information
Authors and Affiliations
Contributions
Conceptualization and writing—Yuquan Chen; original draft preparation—Yuquan Chen, Yanwei You and Jiarong He. Methodology and data analysis—Yuquan Chen, Yanwei You and Jiarong He. Material search—Yuquan Chen, Yanwei You and Yuechuan Zhang. Data extraction— Yuquan Chen, Yanwei You, Jiarong He, Yuechuan Zhang and Qi Zhang. Writing, review and editing: Yuquan Chen, Yanwei You, Jiarong He, Qi Zhang, Fan Yang and Mingming Zhang. Supervision, project administration, and funding acquisition: Mingming Zhang. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Y., You, Y., He, J. et al. Physical activity in the relationship between multiple air pollutants exposure and risk of hypertension: a prospective cohort study in China. Sci Rep 15, 24625 (2025). https://doi.org/10.1038/s41598-025-09341-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09341-z