Abstract
The cortical thickness index (CTI) is a radiological measure and correlates with diminishing local bone quality in the proximal femur. The objective of this study was to assess the association between a lower CTI and the occurrence of peri- and postoperative surgical complications. A total of 228 consecutive patients treated with endomedullary nailing for trochanteric fracture (TFx) (AO/OTA 31A1.1–31A2.3) (n = 99) and hemi-/total hip arthroplasty for femoral neck fracture (AO/OTA 31B1–B3) (FNFx) (n = 129) with a mean age of 82 ± 9.9 (50–99) years were retrospectively reviewed. An evaluation of these cases was conducted to ascertain the presence of any surgery-related complications. Eighteen patients (7.9%) undergoing revision surgery were identified. Patient demographics and radiographic measurements of these groups were compared to the cases without complications (n = 210) and statistically analysed. A total of 18 patients (7.9%) with complications who underwent revision surgery were identified. Among the total number of patients, 10 (55.6%) exhibited mechanical complications. The remaining patients underwent a subsequent revision due to infection (n = 4), seroma/hematoma (n = 3), or a running wound (n = 1). The FNFx group exhibited a lack of intraoperative fractures; however, two periprosthetic fractures occurred subsequent to another fall (36 and 59 days postoperatively). A total of five incisions or extractions of the helical blade were identified in the TFx group. The following factors contributed to the necessity for revision: tractus irritation (n = 2), one intraoperative fracture, one running wound, and one seroma. Among all of the variables that were analyzed, including age, body mass index, and hemoglobin level, only the CTI of the affected side in the TFx group was found to be significantly higher in the complications group, as well as the mechanical complications group (0.51 ± 0.09, 0.58 ± 0.05, 0.58 ± 0.05; p = 0.029). Poor local bone quality, as indicated by a low CTI, is not associated with increased complication rates following surgically managed proximal femoral fractures. Instead, the predominant contributors to mechanical complications seem to emanate from alternative factors, such as insufficient fracture reduction and suboptimal blade positioning.
Similar content being viewed by others
Introduction
Due to the ongoing aging of the population, the incidence of proximal femoral fractures is rising1. These fractures can have severe consequences on the quality of life of older people and are associated with an elevated mortality rate2,3.
A primary factor contributing to the occurrence of fractures subsequent to low-energy trauma is the deterioration of bone quality4,5. Diminishing bone mineral density (BMD) has been demonstrated to be a contributing factor to elevated incidences of intra- and postoperative surgical complications6,7. Although the dual-energy x-ray absorptiometry (DEXA) is regarded as the gold standard in quantifying the BMD, several radiological measurements using plain radiographs have been proposed to assess bone quality8,9,10. Among those, the cortical thickness index (CTI) of the proximal femur has been described as a reliable tool with a moderate to strong correlation to the BMD, especially for geriatric patients10,11,12,13. An examination of demographic trends reveals a growing emphasis on the utilization of user-friendly instruments that facilitate clinicians in assessing patients’ bone quality. A paucity of research has been conducted on the correlation concerning peri- and postoperative surgery-associated complications after treatment of proximal femoral fractures with total- or hemi arthroplasty or endomedullary nailing and the CTI The aim of this study was to assess the correlation between the CTI and the rate of short- to mid-term surgical complications. The hypothesis posits, that a lower CTI is associated with a higher rate of surgery-related complications.
Materials and methods
Patients’ demographics and surgery-related information
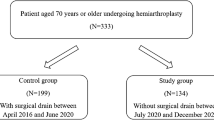
Eligible patients were consecutively enrolled between July 2022 until September 2023 and retrospectively analysed. The following inclusion criteria were applied:
(1) operative treatment of a proximal femoral fracture (femoral neck (AO/OTA 31B1-B3), trochanteric fracture (AO/OTA 31A1.1–31A2.3)) with either a total- or hemi arthroplasty of the hip or endomedullary nailing, (2) low-energy trauma, (3) preoperative conventional radiograph of the pelvis (antero-posterior (ap), (4) at least one postoperative conventional radiograph of the pelvis (ap) after mobilization, (5) present informed consent, (6) minimum 50 years of age, (7) absence of signs for a pathological fracture, (8) absence of surgery to contralateral hip, (9) full set of data (e.g. patients demographics, operation reports for primary and revision surgery). Demographic data was recorded. Patients under the age 50 years, those with preoperative surgery to the affected proximal femur, an incomplete follow-up data (including radiographs), radiographic signs for an atypical femoral fracture or absence of informed consent were excluded.
Surgical technique
All surgical interventions were performed using a traction table with the patient in a supine position. For the total-/hemi arthroplasties, a direct anterior approach was employed, whereas the affected leg was over-extended and externally rotated to implant the femoral component14. In fifty-seven cases (44%), a hemi- and in 72 cases (56%) total hip arthroplasties were implanted (AMIStem C/H, Medacta International SA, Castel San Pietro, Switzerland; cemented and uncemented), whereas stem fixation was performed on surgeons preference as well as taking local bone quality into account. The intramedullary nailing was performed using a 200 mm nail in all patients (TFNA, DePuy Synthes, Zuchwil, Switzerland) with the affected leg positioned in traction. The diameters of the implants were selected based on the intraoperative measurement after fracture reposition, aiming to achieve the thickest possible implant. A helical femoral blade was measured using the measuring device over the positioned guide wire. The helical femoral blade was inserted subsequent to the drilling of the lateral cortex. The blade was locked dynamically while the distal locking screw was locked statically. In none of the operated cases cement augmentation of the helical blade was performed. All patients were permitted to execute full weight bearing immediately.
The approval from the local ethics committee and informed patient consent was obtained (BASEC number 2023-01407).
Radiological measurements
Bilateral measurement of the CTI was performed in accordance to the previously described methods using plain ap-radiographs were patients were positioned supine with the lower extremity internally rotated (15°) (Fig. 1)8,9. On the day of admission, the orthopaedic consultant performed bilateral measurements. The CTI was calculated using the outer (a) and inner (b) femoral diameter 10 cm below the lesser trochanter according to the established formula: CTI = (a − b)/b. For all patients treated with endomedullary nailing, the tip-apex distance (TAD) was measured in the initial postoperative x-ray (ap and lateral) according to the method first described by Baumgaertner et al.15. Furthermore, the position of the helical blade in the femoral head and the femoral neck-shaft angle (NSA) in the first postoperative x-ray were recorded. For patients treated with an endomedullary nail, who subsequently developed a mechanical complication, the integrity of the medial femoral calcar in the postoperative radiograph was observed.
The measurements were executed using mediCAD clinical software (mediCAD Hectec GmbH, Altdorf, Germany).
Follow-up examinations and complications
Routine clinical and radiological follow-up examinations were conducted after six weeks, three months and one year.
All surgical revisions performed during the follow-up period were documented and classified as a complication. These were categorized into mechanical (e.g. lateralisation of femoral blade, blade cut-out, periprosthetic fracture) and non-mechanical complications (hematoma/seroma, revision due to running wounds or infection). Revision surgeries due to implant-associated factors were evaluated in a sub-group for further analysis.
Statistical analysis
Clinical characteristics of patients were determined using descriptive statistics. All data was assessed for normality using the Shapiro–Wilk test. Comparison of the injured proximal femoral with the healthy side was performed using the paired t-test (normal distribution) or the Wilcoxon signed-rank test (non-normal distribution). The independent t test (normal distribution) and Mann–Whitney U test (non-normal distribution) were used to compare continuous variables of the different groups. For comparison of three groups, ANOVA (normal distribution) or the Kruksal-Wallis test (non-normal distribution) were used. Pearson correlation was used to assess the relationship between radiographic measurements. According to Cohen’s assessment, a correlation of r > 0.5 is considered strong, an r value of 0.5–0.3 is considered moderate, and an r value of r < 0.3 is considered weak16. All statistical analyses were performed in SPSS for Mac (version 23.0, SPSS Inc, Chicago, Illinois). Significance was set at p < 0.05.
Results
Patients’ demographics and surgery-related information
A total of 233 patients who underwent treatment with either endomedullary nailing (trochanteric fracture (TFx)) or total-/hemi arthroplasty of the hip (femoral neck fracture (FNFx)) after a low-energy trauma from July 2022 to September 2023 were identified. Due to the absence of postoperative x-rays, five patients were excluded, leaving 228 individuals eligible for final statistical analysis. The absence of data was attributable to the fact that the patients had passed away prior to undergoing postoperative X-rays. The mean age at time of surgery was 82.4 ± 9.9 (range 50–99) years with a majority of the patients being female (n = 171, 75%). A total of 129 patients (57%) sustained a femoral neck fracture. Detailed information on patient demographics and surgery-specific data are presented in Table 1.
Surgery- and implant-related peri- and postoperative complications
A total of 18 patients (8%) underwent an additional surgical procedure after an average time of 61 ± 83 (0–327) days. A total of eight patients (4%) underwent revision surgery for non-mechanical issues, with an average time interval of 18 days (range: 0–44 days) between the initial procedure and the subsequent intervention. Revision interventions for mechanical complications was performed in 10 patients (4%) after a mean of 101 (14–327) days. In patients with a FNFx, no perioperative periprosthetic fracture was observed. In the FNFx cohort, eight patients (6%) underwent revision surgery. A total of six patients (75%) were revised due to hematoma/seroma or infection. In addition, two patients (25%) underwent revision surgery due to periprosthetic fractures following another fall 36 and 59 days postoperatively. In the TFx cohort, two patients (2%) were revised due to non-mechanical reasons. Eight patients (8%) required revision surgery because of close to or actual helical blade cut-through/cut-out (n = 5) (Fig. 2a,c), tractus irritation through helical blade lateralisation (n = 2) (Fig. 2b) or intraoperative fracture (n = 1). Detailed data is presented in Tables 2 and 3.
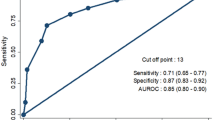
The analysis of the relationship between the bilateral CTI for the entire cohort demonstrated a strong correlation (r = 0.574) between the affected and non-affected side (see Fig. 3).
Comparison of patients with and without complications
In the group of patients with a FNFx who did not experience complications, 56 (47%) received an uncemented implant whereas five patients (63%) in the complication group were treated with an uncemented implant. In both cohorts of the TFx, a closed reduction and internal fixation (CRIF) was performed in all but two patients. The investigation revealed that no observed variables exhibited a statistically significant discrepancy between the three subsamples (Table 4).With regard to the various fixation methods, no significant differences were observed in the complication cohort of the TFx. This is due to the fact that no additional cement augmentation was utilized for any of the patients who experienced complications. In three of the eight complication cases (37.5%) treated with a hemi-/total hip arthroplasty, a cemented fixation was utilized. In the present study, a total of 12.5% of the cases underwent revision surgery due to various postoperative complications. These complications included the development of a hematoma (n = 1), a periprosthetic fracture (n = 1), and a periprosthetic infection (n = 1), each accounting for one case of revision surgery.
Analysis of radiological measurements
A significant difference was observed in the average ap CTI on the non-fractured femur among patients with trochanteric fractures, with those demonstrating no complications exhibiting a lower value compared to those experiencing complications (p = 0.006; 0.029). The TAD did not differ between the three cohorts. Results are presented in Table 5. Results for the measurements of postoperative NSA and position of the helical blade for the mechanical failures are shown in Table 3. In five out of eight patients (62.5%), the first postoperative radiograph (antero-posterior, lateral) revealed a disruption of the medial femoral calcar.
Discussion
The main finding of this study is that a lower CTI—contrary to the study’s hypothesis—is not associated with increased incidence of peri- or postoperative surgical complications after operative treatment for proximal femoral fractures. Remarkably, patients with a surgical or mechanical complication in the short- to mid-term follow up exhibited a significantly higher CTI on the non-affected side compared to those who did not experience complications.
In previous studies different radiographic parameters were described to correlate with an increased rate of periprosthetic fractures, whereas most studies investigated the association with the Dorr classification8,17. Exemplary, Griffiths et al. demonstrated a correlation with Dorr B- and C-type femora and a lower canal flare index and a higher rate of perioperative periprosthetic fractures17. Another recent study displayed a correlation of Dorr’s canal calcar ratio and the CTI in geriatric patients with trochanteric and femoral neck fractures18. Spina et al. reported, that Dorr C-femora exhibited a higher incidence of periprosthetic fractures in the first year after implantation of a total hip arthroplasty19. However in contrast to the current study with a shorter follow-up, the age of the patients of the study was younger with a mean age of 75 years. Similar results were observed by Nash et al., who described a correlation between decreased CTI values and rising Dorr grades7. Their findings indicated an increased rate of periprosthetic fractures after treatment of femoral neck fractures with a hemiarthroplasty with diminishing CTI values. These findings contrast with the current study which failed to ascertain an association of a lower CTI and the incidence of intra- or perioperative fracture in the treatment for femoral neck fractures.
In the context of endomedullary nailing for proximal femoral fractures, various implant-related complications have been documented, often necessitating subsequent surgical interventions. The following factors have been identified as contributing to the loss of reduction and the necessity for subsequent reoperations: lateral wall comminution, reduced medullary fill, or distally unlocked nails20,21,22. Yamamoto et al. who reviewed 390 cases of intramedullary nails for treatment of trochanteric fracture for reasons of reoperation, examined the CTI and Dorr classification23. They examined a significant higher CTI in the cohort without need for reoperation (CTI 0.5 ± 0.08 vs. 0.45 ± 0.1, p = 0.033), whereas information is lacking whether the affected or unaffected femoral bone was measured. It has been established that malrotation of the fractured extremity, as depicted in the preoperative radiograph, can exert a substantial influence on the measuring results of the CTI. The present study’s findings contradict those of the aforementioned study, which observed an elevated AP CTI in both proximal femora, with a statistical significance on the non-fractured side. Another study by Fan et al., conducted a retrospective evaluation of 130 intertrochanteric fractures and risk factors for implant failure, did not see any difference in the ap CTI in their failure (0.49 ± 0.07) or control (0.5 ± 0.07; p = 0.447) group21. Unfortunately, this analysis also fails to provide information on which side they measured to calculate the ap CTI. Due to the significant heterogeneity observed in the information obtained from the affected and unaffected sides, the present study offers a substantial advantage, as it involves the bilateral scanning of the AP CTI.
Next to the above discussed CTI-related complication studies, several previously described failure modes have to be considered. As described by Baumgaertner et al. the TAD should not exceed 25 mm since higher values led to a higher risk for helical blade cut-out in their cohort15. In the present series of mechanical failures of trochanteric fractures two out of eight revised patients showed a TAD above the recommended distance, which subsequently led to a blade cut-out. Furthermore, screw positioning in the femoral head and restoration of the neck-shaft-angle (NSA) are crucial and remain significant subjects in the treatment of trochanteric fractures24,25. In two cases of the blade cut-outs (cases no.4 and 12), TAD, blade positioning and postoperative neck-shaft-angle were not conducive for fracture healing leading to varus collapse and revision surgery. Since the medial calcar integrity displays a major role to prevent structure collapse, the overall high percentage (62.5%) of failing to restore the calcar adds to the multifactorial causes for the development of construct failure26. This further underscores the importance of anatomical reduction and blade positioning.
Adding to the above mentioned, the use of cement augmentation could have potentially enhanced the construct’s stability in cases where the risk for revision surgery is dooming. Schneider et al. retrospectively reviewed 275 consecutive trochanteric fractures treated with a an endomedullary nail, whereas 68 (25%) underwent a cement augmentation and none of those revealed a postoperative cut-out/cut-through27. Nonetheless, the authors’ assertion that they elected to utilize cement in patients exhibiting suboptimal bone quality, as indicated by a mean age of 77.5 years within the cohort, appears to lack precision. Furthermore, information on postoperative weightbearing is missing, which could additionally be protective for mechanical failure. Another multicentre randomized controlled trial published earlier on confirmed those findings with smaller reoperation rates in cement augmented patients, but again finding no statistical relevance28. However, in the present study, although the number of different fixation methods in endomedullary nailing or cemented versus uncemented hemi-/total hip arthroplasties was low, no obvious correlation to any of the fixation methods could be seen.
This study has several limitations. Next to the obvious drawbacks of the retrospective design, the statistical expressiveness may be diminished by a small number of cases in both complication sub-groups. Due to the overall advanced age of the cohort and the potential cognitive impairment of certain patients, mild and subjectively irrelevant disturbing factors, such as tractus irritation, were not taken into account, whereas the focus was on those complications resulting in revision surgery. Furthermore, additional factors, including cognitive impairment and BMI, which have been associated with peri- or postoperative implant complications, were not observed and were not included in the analysis. This would have certainly increased the informative value of this study. Nonetheless, the AO/OTA classification was documented, and, for the trochanteric fractures, the TAD and integrity of the medial calcar, in case of a mechanical complication, was examined, to address at least two relevant variables as reasons for failure. Furthermore, the limited number of mechanical failures does not allow a meaningful statistical analysis. Nevertheless, the cases that have been examined can assist in the prevention of future failures. Another limitation is the absence of measured BMD to evaluate the level of osteoporosis. Furthermore, this study is subject to selection bias, as it includes solely European individuals from one medical center included. Therefore, an international multi-center study with a larger sample size would be required to confirm the presented findings. One further limitation might be the inclusion of the two mainly occurring proximal femoral fracture types in order to analyze the correlation with surgical complications. A distinctive and separate investigation of a larger cohort of either fracture type would certainly add to the scientific value. Lastly, since plain radiographic measurements are not validated and patient positioning displays a crucial role, a certain inaccuracy of the measurements have to be assumed. To address those demerits, the included x-rays where screened for extensive malpositioning. However, the applied measurement methods have displayed excellent inter- and intra-rater reliability18.
Notwithstanding the inherent limitations of the present study, its findings constitute a significant contribution to the existing body of knowledge. The study’s primary conclusion is that a smaller CTI, which is associated with a reduced BMD, does not result in an elevated incidence of surgical complications, both peri- and postoperatively, in the growing cohort of geriatric patients.
Conclusion
Poor local bone quality, as indicated by a low CTI, is not associated with increased complication rates following surgically managed proximal femoral fractures. Instead, the predominant contributors to mechanical complications seem to emanate from alternative factors, such as insufficient fracture reduction and suboptimal blade positioning.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Sambrook, P. & Cooper, C. Osteoporosis. Lancet 367(9527), 2010–2018 (2006).
Guzon-Illescas, O. et al. Mortality after osteoporotic hip fracture: Incidence, trends, and associated factors. J. Orthop. Surg. Res. 14(1), 1–9 (2019).
Dyer, S. M. et al. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. https://doi.org/10.1186/s12877-016-0332-0 (2016).
Nguyen, T. et al. Prediction of osteoporotic fractures by postural instability and bone density. Br. Med. J. 307(6912), 1111–1115 (1993).
Hui, S. L., Slemenda, C. W. & Johnston, C. C. Age and bone mass as predictors of fracture in a prospective study. J. Clin. Invest. 81(6), 1804–1809 (1988).
Liu, B. et al. Incidence, classification, and risk factors for intraoperative periprosthetic femoral fractures in patients undergoing total hip arthroplasty with a single stem: A retrospective Study. J. Arthroplast. 34(7), 1400–1411. https://doi.org/10.1016/j.arth.2019.03.031 (2019).
Nash, W. & Harris, A. The Dorr type and cortical thickness index of the proximal femur for predicting peri-operative complications during hemiarthroplasty. J. Orthop. Surg. 22(1), 92–95 (2014).
Dorr, L. D. et al. Structural and cellular assessment of bone quality of proximal femur. Bone 14(3), 231–242 (1993).
Sah, A. P., Thornhill, T. S., LeBoff, M. S. & Glowacki, J. Correlation of plain radiographic indices of the hip with quantitative bone mineral density. Osteoporos. Int. 18(8), 1119–1126 (2007).
Baumgärtner, R., Heeren, N., Quast, D., Babst, R. & Brunner, A. Is the cortical thickness index a valid parameter to assess bone mineral density in geriatric patients with hip fractures?. Arch. Orthop. Trauma Surg. 135(6), 805–810 (2015).
Faundez, J. et al. Radiographic assessment of bone quality using 4 radiographic indexes: Canal diaphysis ratio is superior. J. Arthroplast. https://doi.org/10.1016/j.arth.2023.08.037 (2023).
Ilyas, G. & Ipci, F. B. Evaluation of the Relationship between osteoporosis parameters in plain hip radiography and DXA results in 156 patients at a single center in Turkey. Diagnostics 13(15), 2519 (2023).
Nguyen, B. N. T., Hoshino, H., Togawa, D. & Matsuyama, Y. Cortical thickness index of the proximal femur: A radiographic parameter for preliminary assessment of bone mineral density and osteoporosis status in the age 50 years and over population. CiOS Clin. Orthop. Surg. 10(2), 149–156 (2018).
Paillard, P. Hip replacement by a minimal anterior approach. Int. Orthop. 31(SUPPL. 1), 13–15 (2007).
Baumgaertner, M. R., Curtin, S. L., Lindskog, D. M. & Keggi, J. M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Jt. Surg. 77(7), 1058–1064 (1995).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences (Academic Press, 2013).
Griffiths, S. Z. et al. Predictors of perioperative vancouver B periprosthetic femoral fractures associated with the direct anterior approach to total hip arthroplasty. J. Arthroplast. 35(5), 1407–1411 (2020).
Guyan, F., Gianduzzo, E., Waltenspül, M., Dietrich, M. & Kabelitz, M. Cortical thickness index and canal calcar ratio: A comparison of proximal femoral fractures and non-fractured femora in octogenarians to centenarians. J. Clin. Med. 13(4), 981 (2024).
Spina, M. & Scalvi, A. Periprosthetic fractures of the proximal femur within first year of the index hip prosthesis. Acta Biomed. 91(3), e2020060 (2020).
Tisherman, R. T., Hankins, M. L., Moloney, G. B. & Tarkin, I. S. Distal locking of short cephalomedullary nails decreases varus collapse in unstable intertrochanteric fractures: A biomechanical analysis. Injury 52(3), 414–418. https://doi.org/10.1016/j.injury.2021.02.007 (2021).
Fan, J. et al. Risk factors for implant failure of intertrochanteric fractures with lateral femoral wall fracture after intramedullary nail fixation. Injury 52(11), 3397–3403. https://doi.org/10.1016/j.injury.2021.07.025 (2021).
Durusoy, S., Paksoy, A. E., Korkmaz, M., Dağlar, B. & Elibol, F. K. E. The effect of medullary fill on varus collapse in AO 31A3 intertrochanteric (reverse obliquity) fracture treated with cephalomedullary nails. Orthop. Traumatol. Surg. Res. 107(3), 102804 (2021).
Yamamoto, N. et al. Reduction quality and nail fixation ratio as bone-implant stability factors associated with reoperation for trochanteric fractures. Injury 52(7), 1813–1818 (2021).
De Bruijn, K., den Hartog, D., Tuinebreijer, W. & Roukema, G. Reliability of predictors for screw cutout in intertrochanteric hip fractures. J. Bone Jt. Surg. 94(14), 1266–1272 (2012).
Kristan, A., Benulič, Č & Jaklič, M. Reduction of trochanteric fractures in lateral view is significant predictor for radiological and functional result after six months. Injury 52(10), 3036–3041 (2021).
Mei, J., Pang, L. & Jiang, Z. Strategies for managing the destruction of calcar femorale. BMC Musculoskelet. Disord. 22(1), 1–9 (2021).
Schneider, F. et al. Retrospective evaluation of radiological and clinical outcomes after surgical treatment of proximal femur fractures utilizing TFNA. Arch. Orthop. Trauma Surg. 143(7), 4165–4171. https://doi.org/10.1007/s00402-022-04704-x (2023).
Kammerlander, C. et al. Cement augmentation of the proximal femoral nail antirotation (PFNA): A multicentre randomized controlled trial. Injury 49(8), 1436–1444. https://doi.org/10.1016/j.injury.2018.04.022 (2018).
Funding
There were no fundings received for this study.
Author information
Authors and Affiliations
Contributions
M.K. collected the data. M.W. performed data analysis. M.W. and M.K. wrote the manuscript. M.D. critically reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was obtained by the local ethical committee and all procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was given by all the patients. Ethics approval was given by the local ethics committee (Kantonale Ethikkommission Zürich, Switzerland, BASEC-Nr. 2023-01407).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kabelitz, M., Waltenspül, M. & Dietrich, M. Lower cortical thickness index does not correlate with increased surgical complications in proximal femoral fractures: a clinical and radiological study. Sci Rep 15, 24115 (2025). https://doi.org/10.1038/s41598-025-09362-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09362-8