Abstract
Accurate knowledge of the root canal system is essential for successful endodontic treatment. The position of the apical foramen, which frequently deviates from the anatomical apex, impacts treatment precision. While advances like electronic apex locators have enhanced accuracy, discrepancies with radiographic readings still arise due to foramen position variations. Factors such as age, race, and ethnicity contribute to these differences. This study examines the distance and direction of deviation between the major apical foramen and the anatomical apex in an Iraqi subpopulation. It aims to highlight local anatomical variations, aiding better treatment outcomes. A total of 238 extracted permanent human teeth were examined. The teeth were sectioned transversely at the cemento-enamel junction, mounted on a calibrated microscopic slide, and analyzed to identify the location of the major apical foramen. The major foramen was defined as the largest-diameter opening at the root apex. The assessment was conducted using a dental operating microscope. The distance between the major apical foramen and the anatomical apex was calculated using Image J software. The mean distance between the major apical foramen and the anatomical apex across all teeth was 0.52 mm. This distance was consistent in both anterior and posterior teeth, with notable variations observed among different tooth types. The mandibular canine exhibited the greatest deviation, with a mean distance of 0.77 mm, followed by mandibular molars, which showed a mean distance of 0.6 mm. The most common direction of deviation was distal, with a frequency of 25.65% across all tooth types. The study’s findings indicated that in 85% of all tooth types, the major foramen deviated from the anatomical and/or radiographic apex. The distal deviation was the most frequent, with an average distance of 0.52 mm. These results underscore the importance of understanding apical anatomy for accurate endodontic treatment and highlight notable anatomical variations in this subpopulation.
Similar content being viewed by others
Introduction
The major apical foramen plays a crucial role in endodontic treatment, serving as the primary pathway for communication between the pulp and periapical tissues. Accurate knowledge of its anatomical location, shape, and size is essential for effective working length determination, optimal canal preparation, and successful obturation1,2. Considering the significance of this, the location of the anatomical root apex in relation to the apical constriction/foramen is a significant aspect for an operator to consider because it dictates the appropriate execution of the therapeutic steps and determines where the treatment should end3.
Many factors, such as age, physiologic or pathological conditions, might contribute to the variation in distance and frequency of deviation of the apical foramen4. In this regard, Kuttler5 claimed that with age, the alignment of the apical foramen to the root apex declines and the distance between them increases. The anatomical location of the apical foramina changes according to the anatomical root apex throughout tooth development; as a result of eruption, cementum apposition, and functional activity adaptation, the dimension of apical foramen increases and moves away from the central position6. The frequency and distance of deviation of the major apical foramen from the anatomical root apex in extracted teeth have been investigated using various methods, including direct observation7, scanning electron microscopy (SEM)8, and cone-beam computed tomography (CBCT)9,10.
As technology has advanced, endodontic treatments have been improved in recent years with the introduction of electronic apex locators11. They allow for the determination of the position of the root canal’s apical constriction and this innovation in the field has earned the simplicity of detecting the apical termination; however, when combining the information from the electronic apex locators and the radiographic apex, some clinicians might develop questions regarding the accuracy of the device’s readings12. In terms of using different radiographic technique to determine the working length; two studies by Shirazi et al.13, Faraj14 stated that a standardized parallel radiographic method was performed similarly to the CBCT technique and closest to its real clinical working length and it could prevent the need for further diagnostic radiographs for confirmation of working canal length. The reason behind this is that the apical foramen/apical constriction does not consistently end at the anatomical and/or radiographic apex and might deviate to the facial, palatal/lingual, mesial, or distal in respect to the radiographic apex center; however, it is also feasible to coincide with the radiographic apex15.
Variations in the apical foramen’s anatomy may occur due to ethnic, geographic, and genetic factors, highlighting the importance of population-specific data. Despite the clinical significance of this anatomical structure, limited information exists regarding its characteristics in the Iraqi population. The current study’s aim is to further investigate the distance between the major apical foramina and the anatomical apex, as well as the direction of deviation of the apical foramen from the center of the anatomical apex on extracted maxillary and mandibular teeth from a sample of Iraqi subpopulation using dental operating microscope (DOM) and also SEM was used to assess the morphology and topography of the major apical foramen.
Materials and methods
Sample size calculation
The G*Power software (version 3.1.9.4) was used to perform an a priori sample size calculation for this study. The selected statistical test was a t-test for independent means (two groups), using a two-tailed hypothesis. An effect size of 0.5 (medium) was selected based on Cohen’s conventions16. The significance level (α error probability) was set at 0.05, with a statistical power (1 − β error probability) of 0.95. An equal allocation ratio (N2/N1 = 1) was assumed. Based on these parameters, the required total sample size was calculated to be 210 (105 samples per group), confirming that the study is adequately powered to detect medium effect size with a 5% significance level and 95% power, two-tailed.
So, the calculated minimum required sample size is 210 samples for two groups. Since the available sample size in the study 238 teeth exceeds this requirement, the study is adequately powered to detect medium effect sizes reliably.
Final sample size of 238 sound, permanent, completely developed teeth were selected to be examined for this study. Informed consent was obtained from the patients when the sampled teeth when collected. The distribution of the teeth according to tooth groups comprised 139 maxillary teeth and 99 mandibular teeth, encompassing central and lateral incisors, canines, first and second premolars, and first and second molars. This distribution ensured representation across different tooth types and arches, allowing for comprehensive analysis and insights into endodontic characteristics and variations. Fractured roots and samples with resorbed apical areas were excluded to maintain measurement accuracy, deciduous teeth were excluded due to the inability to assess physiological resorption at extraction. Third molars were also excluded due to their difficult endodontic treatment, unpredictable root anatomy. This study was approved by the ethics committee at Komar University for Science and Technology under the ethical approval code (S23-01-01-DEN) and all experiments were performed in accordance with Helsinki–ethical principles for medical research and relevant guidelines and regulations.
Before storage, the teeth were cleaned from periodontal tissues and calculus using 5% sodium hypochlorite and ultrasonic scaler (Sonic Borden 2000N, Kavo Equipaments, Joinville, Brazil). After disinfection with sodium hypochlorite (Neo Cleaner, Neo Dental, Tokyo, Japan) for 24 h, each group of teeth was kept in normal saline in a separate container labeled with a distinct code for each category of teeth until the examination. During the examination, the teeth were cut transversely at the cementoenamel junction Accutom-50 diamond cutter (Accutom Hard Tissue Microtome, Struers, Denmark). Initially, two examiners consisting of an endodontist and an experienced dentist identified the major apical foramen under the microscope, in case of disagreement a K-file size 10 (Dentsply Maillefer, Ballaigues, Switzerland) were employed in accordance with the size of the canal. The file was placed in the canal and visualized as it emerged from it while observing under the microscope. To facilitate the characterization of the foramen, the apical region of the teeth was prepared and stained with pink ink using a micro brush. In the context of identifying main foramens, the presence of two separate canals or two joined canals that separate at the end, each culminating in a distinct foramen, or the existence of any additional foramen, poses a notable anatomical variation. In such instances, the largest foramen among the identified openings was selected for the purpose of this study. Then, for each root of each tooth, an inspection was done to indicate if the main apical foramen has diverged from the root apex’s center. That being the case, the position of the foramen was recorded whether it was at the center or placed mesial, distal, buccal, or lingual to the anatomic apex.
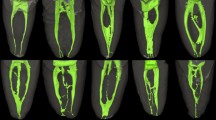
After the exploration of the opening side of the major apical foramen, the tooth was mounted on a calibration microscopic slide at the accuracy of 0.5 mm, using a softened wax to constrain movement and permit the measurement to be performed parallel to the tooth’s long axis. The mounted tooth was examined under Zumax OMS2380 DOM at 27X magnification (Zumax Medical Co., Ltd., Suzhou, China). The working distance between the optical lens of the microscope and the mounted table was set at 30 cm using a calibration ruler. In the next step, with the aid of the microscope’s digital camera, pictures of each root were captured on the side of the opening. After transferring the images into a computer and through utilizing Image J software (Ver.1.54 October 2023) program (National Institutes of Health, Bethesda, MD, USA), the distance was measured from the most coronal border of the major apical foramen to the anatomic apex17 (Fig. 1).
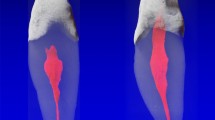
The topography and morphology of randomly selected specimens were examined under SEM after being coated with a gold sputter-coating process for qualitative analysis (Caesium, version 6.1.10, ID 634,258,760) (CS3200 Tungsten) (Fig. 2). The workflow chart of the study shown in (Fig. 3). All photographs were taken by Ubaydah Alqailani (ubaydah.falah@komar.edu.iq).
A scanning electron micrograph of the different root apices showing different locations of the major apical foramen; (A): distal root of mandibular first molar (X50), (B): hourglass shape of major apical foramen of maxillary second molar (X100), and (C): typical circular shape of major foramen of a maxillary central incisor root, located at the center of the anatomical apex (X250).
Reliability test
To assess reliability, all measurements were taken twice by the same observer, with a two-week interval between sessions. The average of the two measurements was used for analysis. Reliability was evaluated using the Intraclass Correlation Coefficient (ICC), which ranges from 0 to 1. An ICC value below 0.5 indicates poor reliability, values between 0.5 and 0.75 indicate moderate reliability, values between 0.75 and 0.9 indicate good reliability, and values above 0.9 indicate excellent reliability18.
Statistical analysis
"Using IBM SPSS 26.0 (IBM Corporation, Chicago, IL) the mean values and standard deviations of the distances and frequencies of deviation of the major apical foramen with respect to the anatomical apex were calculated for each group of specimens." (IBM Corporation, Chicago, USA).
Results
The score from analysis of intra-examiner reliability was 0.88, indicating total dependability of the study.
A total of 238 teeth with 343 root canals were investigated. The average distances between the major apical foramen, the center of the anatomical apex and the frequency of displacement from the center of the root apex are summarized in (Tables 1, 2). The mean distance between the major apical foramen and the anatomical root apex was 0.52 mm, which was comparable in both anterior and posterior. The mandibular canine group had the greatest mean distance 0.77 mm, followed by the mandibular molar group 0.60 mm, after which came the maxillary premolars 0.56 mm.
In 14.86% of the cases, the major foramen coincided with the root apex’s center, and diverged from the anatomical apex in 85.11% of the cases. The percentage of deviation in posterior teeth (86.48%) was higher than in anterior teeth (81.3%), and the most prevalent locations were in the distal (25.65%) and mesial (21.57%) surfaces, followed by lingual (19.24%) and buccal (18.65%) surfaces.
A Bland–Altman analysis was performed to evaluate the agreement between the two examiners’ measurements of the distance between major apical foramen and anatomical apex. The analysis revealed a mean difference of 0.003 mm, the standard deviation of the differences was 0.004 mm, suggesting that there is minimal variability in the differences. The limits of agreement were calculated to be between − 0.005 mm and 0.011 mm. This indicates that approximately 95% of the differences between the two examiners’ measurements lie within this range, reflecting a strong agreement in their assessments of the major apical foramen’s location. Notably, this result was achieved with the aid of Image J Software, which helped reduce the differences between examiners.
Additionally, the topography and morphology of randomly selected specimens were examined using SEM. Specimens were coated with a gold sputter-coating process for qualitative analysis. Various shapes and morphologies of the apical foramen were observed, with the most typical shapes being ovoid or circular. Some specimens exhibited asymmetries and irregularities in the foramen’s structure. For example, the SEM images revealed distinct morphologies: Fig. 2C illustrates the typical circular form of the major foramen in a maxillary central incisor, while Fig. 2B shows an hourglass-shaped foramen in a maxillary second molar.
Discussion
Anatomical understanding of the root apex is crucial for accurate measurement of root canal working length because it contains the major apical foramen, which is frequently used as the reference point for root canal treatment. In this study, 238 teeth with 343 root canals using the DOM with an integrated camera to capture precise images of the apical portion of the teeth, followed by the use of Image J software program was used to measure the distance from the most coronal border of the major foramen to the anatomical apex. The results revealed that in Iraqi subpopulation 85% mismatch between the major foramen’s location and the anatomical apex, indicating that the major apical foramen usually does not align with the anatomical or radiographical apex. This contrasts with a Brazilian study’s lower 19% incompatibility rate in 634 root canals, possibly due to racial and geographical variations19.
In the present study, average distance from major apical foramen border to anatomical apex was 0.52 mm for all teeth. This aligns with previous study, showing mean distances not exceed 1.0 mm7. However, Sayao Maia et al20 found a mean distance of 1.20 mm between the apical foramen and the radiographic apex for all tooth types, this difference might be due to the use of intraoral periapical radiography instead of magnification microscopes for measurements as well as racial differences. The present study’s findings regarding the distance between the apical foramen and the anatomical apex are consistent with those reported by Wolf et al.21, who utilized micro-CT analysis to evaluate this distance in maxillary and mandibular molars. Additionally, Akhlaghi et al22 found the maximum distance of 1.45 mm in mesiolingual roots of mandibular second molars similar to the current study in which the maximum distance was also observed in the mesiolingual roots of mandibular second molars. Additionally, In the present study, the average distance in maxillary premolars is 0.56 mm (ranging from 0 mm to 2.132 mm) and 0.48 mm in mandibular premolars (ranging from 0 mm to 1.259 mm), indicating that both types have similar means; however, it reports slightly lower results as a study by Awawdeh et al.4, in which the mean distance is 0.638 mm in the premolars, with a range of (0.070 mm to 2.180 mm). While, both studies again suggest significant anatomical diversity that may complicate endodontic procedure, the different results can be referred to different measuring methods.
Furthermore, the present study finds distal surface as the common deviation, consistent with Sayao Maia et al.20 and Swathika et al.6 followed by mesial (21.57%), lingual (19.24%), and buccal (18.65%) deviations. In Fig. 1C, an example of lower lateral incisor from the present study can be seen which exhibits a buccal deviation with 0.849 mm distance from the anatomical apex in the microscopic view.
Various shapes and morphology of the apical foramen was observed under SEM, most typical being ovoid or circular as well as presence of asymmetry and irregularities. For example, Fig. 2C shows the foramen of maxillary central incisor with the typical circular form of the major foramen while Fig. 2B shows the foramen of an upper second molar exhibiting an hourglass shape, and this is consistent with a study done by Martos et al.23.
These findings provide support to previous doubts about the precision of periapical radiograph and advocate the use of additional tools like electronic apex locator, an operating microscope, and CBCT scanning2.
Conclusions
The findings from this study on an Iraqi subpopulation indicate that the major apical foramen deviates from the anatomical and/or radiographic root apex in 85% of all examined tooth types. The deviation was most frequently observed on the distal aspect, with an average distance of 0.58 mm. Additionally, various shapes and morphologies of the apical foramen were observed under SEM, with the most typical shapes being ovoid or circular. These results highlight the importance of considering anatomical variations specific to different populations during endodontic procedures to enhance treatment accuracy. Future studies should explore these deviations in broader populations and further assess their clinical implications.
Strength and limitations of the study
This study has some limitations, including a small sample size due to strict criteria and a decline in available cases from previous endodontic treatments. Unlike CBCT scans, the samples couldn’t be examined with a microscope from multiple angles, which increased the chance of errors. Variations in root anatomy also made it hard to align the main foramina correctly and keep the specimens parallel. Despite these challenges, this research provides valuable insights into the anatomical features of the major apical foramen in an Iraqi subpopulation, filling an important gap in the field of endodontics in this region. Additionally, using advanced imaging techniques like digital microscopy and Image J software improved measurement accuracy and consistency.
Data availability
All data of current research is available upon resealable request from the corresponding author.
References
Estrela, C. et al. Apical foramen position in relation to proximal root surfaces of human permanent teeth determined by using a new cone-beam computed tomographic software. J. Endod. 44(11), 1741–1748 (2018).
Saeed, M. S. Apical foramen position in relation to proximal root surfaces of the premolar teeth in Kurdistan region of Iraq: A retrospective CBCT assessment. Turk. Endod. J. 8(3), 116–122 (2023).
Nekoofar, M. H. Advances in working length determination. Endodontic Adv. Evid. Based Clin. Guidelines. 218–242 (2022).
Awawdeh, L., Abu Fadaleh, M. & Al-Qudah, A. Mandibular first premolar apical morphology: A stereomicroscopic study. Aust. Endod. J. 45(2), 233–240 (2019).
Kuttler, Y. Microscopic investigation of root apexes. J. Am. Dent. Assoc. 89(1), 20–28 (1955).
Swathika B, Ullah MK, Ganesan S, Muthusamy P, Vuyyuru P, Kalita K, Swarnalatha C, Babu SJ, Nayyar AS. Variations in Canal Morphology, Shapes, and Positions of Major Foramen in Maxillary and Mandibular Teeth. J. Microsc. Ultrastruct. Nov 6;9(4):190–195 (2021).
Manva, M. Z., Alroomy, R., Sheereen, S., Hans, M. K. & Mallineni, S. K. Location and shape of the apical foramina in posterior teeth: An in-vitro analysis. Surg. Radiol. Anat. 43(2), 275–281 (2021).
Silva, J. M., Brandão, G. A., Silva, E. J. & Zaia, A. A. Influence of working length and foraminal enlargement on foramen morphology and sealing ability. Indian. J. Dent. Res. 27(1), 66 (2016).
Arsari, F., Abesi, F., Gholinia, H. & Soleymani, A. Evaluation of apical foramen position and distance from the anatomical apex of roots in anterior maxillary teeth by cone-beam computed tomography (CBCT) in a selected Iranian population. Caspian J. Dent. Res. 10, 20–29 (2021).
Sadri, A., Moudi, E., Khafri, S. & Soleymani, A. Evaluation of apical foramen distance in relation to the anatomical apex of mandibular molars by cone-beam computed tomography (CBCT) in a selected Iranian population. Caspian J. Dent. Res. 8(1), 55–59 (2019).
Kishen, A., Peters, O. A., Zehnder, M., Diogenes, A. R. & Nair, M. K. Advances in endodontics: Potential applications in clinical practice. J. Conserv. Dent. 19(3), 199 (2016).
Sameye, M. R., Bahalkeh, A. M., Izadi, A. & Jafaryan, A. Comparison of digital radiography, conventional film and self-developing film for working length determination. Iran. Endod. J. 13(3), 381 (2018).
Shirazi, Z., Al-Jadaa, A. & Saleh, A. R. Electronic apex locators and their implications in contemporary clinical practice: A review. Open Dent. J. 17(1) (2023).
Faraj, B. M. Preoperative estimation of endodontic working length with cone-beam computed tomography and standardized paralleling technique in comparison to its real length. BioMed Res. Int. 2020(1), 7890127 (2020).
da Silva Schimtz, M., Pagliarin, C. M., Londero, A., Montagner, F. & Morgental, R. Unusual foraminal position in a mandibular molar: Case report. Stomatos. 22(43), (2016).
Cohen, J. Statistical power analysis for the behavioral science 2nd edn. (Lawrence erlbaum Associates, 1988).
Burch, J. G. & Hulen, S. The relationship of the apical foramen to the anatomic apex of the tooth root. Oral Surg. Oral. Med. Oral. Pathol. 34(2), 262–268 (1972).
Abdul, R. J., Abdulateef, D. S., Fattah, A. O. & Talabani, R. M. Analysis of the sagittal root position of the maxillary and mandibular anterior teeth in the alveolar bone using cone-beam computed tomography. Diagnostics (Basel) 14(23), 2756 (2024).
de Brito, L. F., Sá Nogueira, S. J., Ferreira, C. M., Gomes, F. D. & de Sousa, B. C. Prevalence of major apical foramen mismatching the root apex in root canals of human permanent teeth. RSBO 13(3), 188–193 (2016).
Sayao Maia, S. M., Costa, A. P., Lemos, A. T., Torrao, V. R. J. & Vilela, A. V. S. Study of foramen openings and their concurrence with root apexes. RSBO 2(1), 7–11 (2005).
Wolf, T. G., Paqué, F., Sven Patyna, M., Willershausen, B. & Briseño-Marroquín, B. Three-dimensional analysis of the physiological foramen geometry of maxillary and mandibular molars by means of micro-CT. Int. J. Oral. Sci. 9(3), 151–157 (2017).
Akhlaghi, N. M. et al. Radicular anatomy of permanent mandibular second molars in an Iranian population: A preliminary study. Dent. Res. J. (Isfahan) 13(4), 362366 (2016).
Martos, J., Ferrer-Luque, C. M., González-Rodríguez, M. P. & Castro, L. A. Topographical evaluation of the major apical foramen in permanent human teeth. Int. Endod. J. 42(4), 329–334 (2009).
Acknowledgements
The authors are grateful for the contributions of Dr Berekat Mola for his invaluable assistance with statistical analysis.
Author information
Authors and Affiliations
Contributions
1. Dr. Ubaydah Falah Algailani, Komar University of Science and Technology, Sulaymaniyah, Iraq, Email: ubaydah.falah@komar.edu.iq Contribution: Conception 2. Dr. Abdulsalam Rashid Khudid, University of Sulaimani, Conservative Department. Sulaymaniyah Iraq. Email: abdulsalam.kudid@univsul.edu.iq Contribution: Supervision 3. Dr. Ranjdar Mahmood Talabani, University of Sulaimani, Conservative Department, Sulaymaniyah, Iraq. Email: ranjdar.osman@univsul.edu.iq Contribution: Analysis and interpretation 4.*Dr. Hawzhen Masoud Mohammed Saeed , Assistant professor ( Corresponding author) University of Sulaimani College of Dentistry, Conservative department, Sulaymaniyah post code 46,001, Iraq. Email: hawzhen.mohammed@univsul.edu.iq Contribution: Critical review and Corresponding author 5.Dr. Dya Dlshad, Komar University of Science and Technology Sulaymaniyah Iraq, Email: dya.dlshadf18@komar.edu.iq Contribution: Literature review 6.Dr. Sazho Nawzad, Komar University of Science and Technology Sulaymaniyah Iraq, Email: sazho.nawzadf18@komar.edu.iq Contribution: Fundings 7. Dr. Sewa Ali, Komar University of Science and Technology, Sulaimani Sulaymania Contribution: Materials.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Algailani, U.F., Khudid, A.R., Talabani, R.M. et al. Anatomical evaluation of the major apical foramen of extracted maxillary and mandibular human teeth in an Iraqi subpopulation: a cross-sectional study. Sci Rep 15, 24747 (2025). https://doi.org/10.1038/s41598-025-09382-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09382-4
Keywords
This article is cited by
-
Patient perceptions regarding endodontic treatment in an Iraqi sub-population
Discover Social Science and Health (2025)