Abstract
To investigate the effectiveness of diffusion quantitative parameters in detecting microstructural changes in the brain of patients with Alzheimer’s disease (AD) and evaluate the relationship between diffusivity and cognitive function. The study enrolled 43 patients and 16 healthy controls. All participants underwent diffusion spectrum imaging (DSI) and conventional magnetic resonance imaging (MRI). The images were further processed to obtain diffusion MRI models and multi-parameter values. Pearson correlation analysis was used to assess the relationships between diffusion parameters and clinical cognitive scores. Receiver operating characteristic (ROC) analysis was conducted to evaluate the diagnostic performance of various parameters. Significant correlations were observed between neuropsychological scores and diffusion parameters across multiple brain regions. Specifically, the diffusion metrics most strongly related to MMSE and MoCA scores included RTOP, RTAP, ICVF, and FA, with RTOP and RTAP exhibiting the strongest relationship to cognitive function. ROC analysis of DTI, NODDI, and MAP parameters for diagnosing AD indicated satisfactory performance. DTI, NODDI, and MAP-MRI diffusion models are all suitable markers for studying AD. The detailed parameters provide more information about the brain’s microstructural changes in AD patients.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD) is a significant and increasing global health concern and challenge, accounting for approximately 60-80% of patients with dementia1. Mild cognitive impairment (MCI), particularly the amnestic subtype (aMCI), represents a prodromal stage of Alzheimer’s continuum. Neuropathological studies demonstrate that over 80% of aMCI patients exhibit AD-type biomarkers (Aβ+/tau+), supporting its biological continuity with AD dementia1,2. Clinically, AD is characterized by progressive cognitive decline, initially manifesting as memory dysfunction and progressing to widespread impairment in other cognitive domains that result in functional loss. Eventually, the individual is on an inevitable course toward complete loss of independence2. Pathologically, AD is characterized by extracellular aggregation of amyloid-beta into senile plaques and hyper-phosphorylated tau protein accumulation in intraneuronal neurofibrillary tangles as well as known. However, the most direct pathological substrate of clinical symptoms is neurodegeneration, most specifically synapse, neuron loss and myelin degradation have been shown to precede volumetric changes3,4,5. Given that neurodegeneration is closely associated with cognitive dysfunction in AD, it is imperative to discover and develop reliable and sensitive in-vivo markers for neurodegeneration.
Diffusion-weighted imaging (DWI) is a modality that operates by sensitizing the magnetic resonance imaging (MRI) signal to the diffusion of water molecules in the brain. The most widely used DWI model for studying white matter (WM) changes associated with AD is diffusion tensor imaging (DTI)6,7,8,9. The application of DTI models to the study of central nervous system mechanisms of AD has advanced steadily, and several potential imaging biomarkers have been established. However, there are known limitations that DTI assumes that water molecule diffusion in the brain follows Gaussian distribution, weakening its capability to detect diffusion heterogeneity in brain tissue10,11.
Compared with conventional DTI, neurite Orientation Density and Dispersion Imaging (NODDI) is becoming an increasingly popular DWI model applied in contemporary AD research that combat these shortcomings of DTI12. NODDI is a biophysical-based model that characterizes brain changes in specific microstructural environments by assuming that the DWI signal emanates from 3 distinct tissue compartments: within neurites, outside of neurites, and free water. The primary NODDI parameters are intracellular volume fraction (ICVF), extracellular volume fraction (ECVF), isotropic volume fraction (ISOVF), and orientation dispersion index (ODI). NODDI is superior to DTI in evaluating neurodegeneration and pathological biology of AD12,13,14,15,16,17.
The mean apparent propagator magnetic resonance imaging (MAP-MRI) is a q-space-based reconstruction paradigm that fundamentally extends beyond DTI. Unlike DTI’s Gaussian diffusion assumption, MAP-MRI characterizes the full probability density function of water molecular displacements through orthogonal Hermite basis functions, enabling resolution of complex microstructure features18,19. The MAP-MRI parameters include the return-to-origin probability (RTOP), the return-to-axis probability (RTAP), the return-to-plane probability (RTPP), the mean-squared displacement (MSD), the non-Gaussianity (NG), and the q-space inverse variance (QIV)19,20. In recent years, multimodal diffusion imaging techniques (such as NODDI and MAP-MRI) have significantly advanced the analysis of the microstructure of neurodegenerative diseases21,22,23,24. For instance, MAP-MRI studies have revealed a direct association between the reduced complexity of white matter fibers and neurocognitive aging25, and have found that the degeneration of white matter microstructure occurs earlier than macroscopic structural changes during aging26. However, for AD, existing research still focuses on the DTI and NODDI models9,17, and the application of MAP-MRI in AD and its correlation with cognitive function have not been fully explored. Therefore, this study combines NODDI, MAP-MRI and DTI, aiming to reveal the specific microstructure damage patterns of AD and their association with cognitive decline.
This study aimed to preliminarily investigate AD-related microstructural changes by a broad assortment of DWI markers and assess the link between diffusivity and cognitive function. The main goals of this study were to analyze the characteristics of MAP-MRI, DTI-MRI and NODDI-MRI models for the detecting AD-related WM damage, and to assess correlations of the parameter values with Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA) scores, and Finally, to assess the diagnostic performance of different parameters via receiver operating characteristic (ROC) curve. Moreover, these diffusion MRI models could be concurrently obtained from diffusion spectral imaging (DSI), a grid acquisition model that reconstructs diverse diffusion MRI models via the raw diffusion data. The method not only saves time and cost, but also enables the comparative assessment of different models to identify the subtleties in the brain microstructure.
Materials and methods
Participants
The ethics committee of Zigong First People’s Hospital approved this study [Ethics (Research) No. 36, 2023], and all participants provided written informed consent. The study was conducted in accordance with the ethical standards set out in the 1964 Declaration of Helsinki and its subsequent amendments, or comparable ethical standards. Each participant underwent comprehensive cognitive evaluations. The diagnosis of cognitive impairment, including mild cognitive impairment (MCI) or dementia due to probable Alzheimer’s disease (AD), was established based on clinical and cognitive information according to the 2011 National Institute on Aging-Alzheimer’s Association (NIA-AA) diagnostic criteria. A total of 43 patients (MCI/AD) and 16 healthy controls (HC) were enrolled for the primary analysis. The inclusion criteria for the healthy controls were as follows: (1) no evidence of cognitive impairment, (2) MMSE ≥ 25, (3) MoCA ≥ 25, and (4) CDR score = 0.
MCI: Subjective cognitive complaint + objective cognitive impairment (at least one test Z value < -1.5). Retention of activities of daily living (ADL scale decrease < 20%). AD: Progressive episodic memory impairment + ≥ 1 cognitive impairment (CDR ≥ 1, FAQ ≥ 9)27,28. All cases were reviewed by a multidisciplinary consensus panel (neurologist, neuropsychologist, neuroradiologist). The exclusion criteria for all participants were: (1) severe cerebrovascular disorder, (2) severe white matter (WM) hyperintensity, (3) a history of psychiatric illness or severe injury, (4) use of medications that influence cognition, (5) left-handedness, (6) contraindications to MRI, and (7) poor-quality MRI images due to movement artifacts. Of the 43 patients (MCI/AD), 25 successfully completed both the Mini-Mental Status Examination (MMSE) and the Montreal Cognitive Assessment (MoCA).
Data acquisition
All participants underwent DSI sequence on a 3.0T MRI scanner (Skyra; Siemens Healthcare, Erlangen, Germany) equipped with a 32-channel head coil.The DSI sequence was obtained in the axial plane using a half q-space Cartesian grid sampling procedure under the following parameters: TR/TE = 4400/108 ms; FOV = 220 × 220 mm2; SMS factor = 2; slice thickness = 2.0 mm; voxel size = 2.0 × 2.0 × 2.0 mm2; number of slices = 60; b = 0 s/mm2: 0 volume, b = 200 s/mm2: 3 directions, b = 350 s/mm2: 1 directions, b = 400 s/mm2:5 directions, b = 550 s/mm2: 4 directions, b = 750 s/mm2: 3 directions, b = 950 s/mm2: 12 directions, b = 1150 s/mm2: 12 directions, b = 1500 s/mm2: 6 directions, b = 1700 s/mm2: 15 directions, b = 1850 s/mm2: 1 directions, b =1900 s/mm2: 11 directions, b = 2050 s/mm2: 12 directions, b = 2250 s/mm2: 4 directions, b = 2450 s/mm2: 12 directions, b = 2650 s/mm2: 24 directions, b =3000 s/mm2: 3 directions ; a total of 128 diffusion sampling were acquired. The total scan time was approximately 10 min and 8 s.
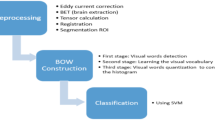
Diffusion data analysis
Multiple parameter maps of DTI, MAP-MRI and NODDI were obtained from DSI data calculated using an in-house prototype software developed by MR Station (Chengdu Zhongying Medical Technology Co., Ltd.). All raw diffusion imaging data need to be converted to NIFTI format and subjected to eddy current correction (FSL) and denoised with a gaussian filter with FWHM 3 mm. Then, three diffusion models were fitted and the related diffusion metrics were derived20,29. The maps of quantitative microstructural parameters are shown in Fig. 1.
Comparison of three diffusion MRI maps revealing brain microstructure. The top image presents DTI parameters, including axial diffusivity (AxD), fractional anisotropy (FA), mean diffusivity (MD), and radial diffusivity (RD). The middle image displays NODDI parameters: extracellular volume fraction (ECVF), intracellular volume fraction (ICVF), isotropi volume fraction (ISOVF), and orientation dispersion index (ODI). The botto image shows MAP-MRI parameters: mean squared displacement (MSD), non-Gaussianity (NG), axial non-Gaussianity (NGAx), radial Non-Gaussianity (NGRad), Q-space inverse variance (QIV), return-to-axis probability (RTAP), return-to-origin probability (RTOP), and return-to-plane probability (RTPP). Each parameter map reveals specific aspects of brain tissue microstructure.
For the DTI model, the axial and radial difusivity (AxD and RD) are the average difusivities, respectively, in the directions parallel and perpendicular to the difusion tensor (DT) eigenvector with the largest eigenvalue.Mean difusivity (MD) quantifes the mean extent of the difusion of water molecules in a voxel and refects the overall level of molecular dispersion. Fractional anisotropy (FA) represents the amount of difusion asymmetry within a voxel, which in theory should range between 0 and 1.
For the NODDI model, the isotropic volume fraction (ISOVF) measures the isotropic difusion compartment in a voxel, intracellular volume fraction (ICVF), extracellular volume fraction (ECVF) represent difusion within the axons and cells, and the orientation dispersion index (ODI) measures the orientation dispersion of fibers in a voxel.
For the MAP model, the non-Gaussianity (NG) characterizes the three-dimensional difusion process and is defned as NG = sinθPG, which quantifes the dissimilarity between the propagator, P(r), and its Gaussian part, G(r). Axial non-Gaussianity (NGAx) and radial nonGaussianity (NGRad) are the derivations of NG for difusion on the axial and radial directions, respectively. The return-to-origin probability (RTOP) describes the probability of no net displacement of molecules between two difusion sensitization gradients, and the return-to-plane probability (RTPP) and return-to-axis probability (RTAP) are its variants for difusion in one- and two-dimensions. The mean squared displacement (MSD) measures the average amount of difusion in a voxel. The q-space inverse variance (QIV) measures the inverse variance of the q-signal geometric means.
Tract-based spatial statistics (TBSS) processing
The disparity between patients with AD and healthy controls (HC) was assessed by processing diffusion parameter maps via a tract-based spatial statistics pipeline within the FSL toolbox from the Oxford Centre for Functional MRI of the Brain (http://fsl.fmrib.ox.ac.uk/fsl/fslwiki/). The detailed procedural steps were as follows: Firstly, FA maps for AD and HC were nonlinearly registered to the FMRIB58_FA template. Secondly, affine align transformations were carried out for all participants from the previous stage into the 1 × 1 × 1 mm2 Montreal Neurological Institute (MNI152) standard space. Thirdly, all the aligned images were averaged, skeletonized, and a mean FA skeleton was created. Finally, FA maps and other parameter maps of each subject were projected onto the mean FA skeleton. The whole brain was separated into 50 brain regions by employing the Johns Hopkins University (JHU)-White Matter-labels as masks.
Statistical analysis
Nonparametric permutation tests were carried out using the randomize tool to analyze group differences. The number of random permutations was set to 5000. Threshold-free cluster enhancement (TFCE) was utilized for multiple comparison correction. The statistical threshold was defined as p < 0.001. Eventually, the results of the group comparison were superimposed on HU–white matter–label templates for locating major brain regions.
Statistical analyses were conducted by utilizing the IBM SPSS 23.0 software package (IBM Corp, Armonk, NY, USA). Pearson correlation analysis was implemented to assess the relationship between clinical cognitive scores and diffusion parameter values. The criterion for statistical significance was set at p < 0.05, and a false discovery rate (FDR) was used to correct for multiple comparisons.
Subsequently, we constructed regression models between diffusion parameters and AD via multivariate binary logistic regression analysis, and adjusted for the square of age, the gender and years of education.Then, diagnostic performance of various diffusion parameter values in distinguishing AD was evaluated through receiver operating characteristic curve (ROC) analysis. The sensitivity, specificity, accuracy, and area under the curve (AUC) were calculated using SPSS. A significance level of p < 0.05 was adopted, and differences reaching this criterion were considered to have statistical significance.
Results
Demographic and neuropsychologic data analyses
A total of 43 AD patients and 16 healthy volunteers were included in this study. The average age in the AD group was significantly higher than that in the HC group (p = 0.005), but the years of education (p = 0.009), MMSE scores (p < 0.001) and MoCA scores (p < 0.001) in the AD group were significantly lower than that in the HC group. There was no significant difference in gender between the AD group and the HC group (Table 1).
Diffusion quantitative parameters of DTI, NODDI and MAP-MRI
In the DTI model, the brain regions with significantly higher AxD values, MD values and RD values were mainly situated in the body of the corpus callosum, splenium of the corpus callosum, anterior corona radiata R/L in the AD group compared with the HC group ( p < 0.001). Conversely, in the AD group, the FA values of specific regions including the middle cerebellar peduncle, genu of corpus callosum, body of corpus callosum, splenium of corpus callosum, anterior corona radiata R/L, and superior longitudinal fasciculus R/L were notably decreased when compared with the HC groups. Meanwhile, there was an increase in the MD and RD values of these determined brain regions ( p < 0.001) (Fig. 2).
Diffusion parameter maps exhibiting microstructural differences between the AD and HC groups. DTI parameters: axial diffusivity (AxD), fractional anisotropy (FA), mean diffusivity (MD), and radial diffusivity (RD). NODDI parameters: extracellular volume fraction (ECVF), intracellular volume fraction (ICVF), and isotropic volume fraction (ISOVF). MAP-MRI parameters: mean-squared displacement (MSD), non-Gaussianity (NG), axial non-Gaussianity (NGAx), radial non-Gaussianity (NGRad), q-space inverse variance (QIV), return-to-origin probability (RTOP), return-to-axis probability (RTAP), and return-to-plane probability (RTPP). Each column represents axial brain slices at various Z-coordinates, indicating the spatial distribution of these parameters within the brain. Green represents the mean FA skeleton of all participants. Red–blue represent regions with significant statistical values (P < 0.001). Compared with the HC group, Red indicates an increase in the parameter values and blue indicates a decrease in the AD group.
In the NODDI model, the brain regions that had significantly higher ECVF values were mostly situated in the genu of corpus callosum, body of corpus callosum, splenium of corpus callosum, anterior corona radiata R/L, and superior corona radiata R/L. (p < 0.001). In the AD group, the ISOVF values of the body of corpus callosum, splenium of corpus callosum, external capsule, and cerebral peduncle were increased (Fig. 2).
In the MAP-MRI model, the MSD and QIV values of the frontal lobe, occipital parietal lobe, cerebral peduncle, and corpus callosum in the AD group were significantly higher than those in the HC group (p < 0.001). Furthermore, in the AD group, the values of NGRad, RTAP, RTOP, and RTPP of the genu of corpus callosum, body of corpus callosum, splenium of corpus callosum, anterior corona radiata R/L, and superior corona radiata R/L were lower than those in the HC group (p < 0.001). Meanwhile, the NG and NGAx values of anterior corona radiata R/L were also significantly decreased in the AD compared with the HC group (p < 0.001) (Fig. 2).
Correlations between imaging parameters and neuropsychologic scores
The correlation analyses with the maximal correlation coefficients between DTI-derived parameters (AxD, FA, MD, RD), NODDI-derived parameters (ECVF, ICVF, ISOVF), MAP-MRI-derived parameters (MSD, QIV, NG, NGAx, NGRad, RTAP, RTOP, RTPP) and neuropsychological testing scores (MMSE scores, MoCA scores) in 25 AD patients. Associations were noted between neuropsychologic scores and mangy diffusion parameters across multiple fiber tracts. Since many parameter values of multiple brain regions are correlated with cognitive scale scores, we only select some brain regions and parameter values with good cognitive correlation for display (Figs. 3 and 4).
The MMSE scores in AD patients were markedly related to the diffusion parameters in six brain regions. Each scatterplot exhibits the relationship between the MMSE scores (x-axis) and the specific diffusion imaging parameters (y-axis) for the corresponding brain area. L, Left; R, right. AD, Alzheimer’s disease; FA, fractional anisotropy; ICVF, intracellular volume fraction; MMSE, Mini-Mental State Examination; RTAP, return-to-axis probability; RTOP, return-to-origin probability.
The MoCA scores in AD patients were markedly related to the diffusion parameters in six brain regions. Each scatterplot exhibits the relationship between the MoCA scores (x-axis) and the specific diffusion imaging parameters (y-axis) for the corresponding brain area. MoCA, Montreal cognitive assessment.
For DTI-derived parameters, the FA values were positively correlated with the correlation of cognitive scale, while the AxD, MD, and RD values had a negative correlation. The FA values were significantly correlated with MMSE and MoCA scores compared with the other 3 parameter values. The FA values in the fornix (r = 0.740, p < 0.001), anterior corona radiata L (r = 0.617, p < 0.001), stria terminalis R (r = 0.715, p < 0.001) exhibited strongly correlations with MMSE scores. The FA values of fornix (r = 0.690, p < 0.001), stria terminalis R (r = 0.644, p < 0.001), and stria terminalis L (r = 0.617, p < 0.001) demonstrated strong correlations with the MoCA scores.
For NODDI-derived parameters, the ECVF values in the anterior corona radiata R (r = 0.642, p < 0.001), ICVF values in the splenium of corpus callosum (r = 0.666, p < 0.001), and ISOVF values in the stria terminalis R (r = 0.604, p < 0.001) exhibited the strongest correlations with the MMSE scores, compared with other brain regions. In addition, the ICVF values in the splenium of corpus callosum (r = 0.649, p < 0.001) were most correlated with the MoCA scores. However, no ECVF, ODI, and ISOVF values for any fiber were significantly correlated with the MoCA scores.
For MAP-derived parameters, RTAP and RTOP values were significantly correlated with the MMSE and MoCA scores. The RTAP values in the stria terminalis R (r = 0.737, p < 0.001) and the RTOP values in the stria terminalis R (r = 0.734, p < 0.001) exhibited the strongest correlation with the MMSE scores. The RTAP values in the stria terminalis R (r = 0.699, p < 0.001) and the RTOP values in the cerebral peduncle R (r = 0.717, p < 0.001) exhibited the strongest correlation with the MoCA scores.
ROC analysis for the diagnostic performance
For the diagnosis of AD or MCI, the diagnostic capabilities of diffusion parameters in six brain regions—namely, the splenium of the corpus callosum, fornix, cerebral peduncle R/L, anterior corona radiata R, and stria terminalis R—were evaluated using ROC curve analysis. The results of this analysis are presented in Table 2. This study suggests that the DTI radial diffusivity (DTI-RD) parameter exhibited the best diagnostic performance in the following brain regions: splenium of the corpus callosum [ p = 0.021, AUC = 0.86, 95% confidence interval (CI) = 0.76–0.95], fornix [ p = 0.002, AUC = 0.93, 95% CI 0.86–1.00 ], right cerebral peduncle [ p = 0.002, AUC = 0.95, 95% CI 0.91–1.00], left cerebral peduncle [ p = 0.021, AUC = 0.88, 95% CI 0.79–0.97 ], and right stria terminalis [ p = 0.004, AUC = 0.92, 95% CI 0.84–0.99 ]. Additionally, the DTI mean diffusivity (DTI-MD) parameter demonstrated the best performance in the right anterior corona radiata [ p = 0.005, AUC = 0.92, 95% CI 0.84–1.00 ]. In the NODDI model, the isotropic volume fraction (NODDI-ISOVF) parameter showed similar diagnostic performance across the same brain regions: splenium of the corpus callosum, fornix, right and left cerebral peduncles, right stria terminalis, and right anterior corona radiata. Furthermore, different parameters in the MAP model also exhibited excellent diagnostic performance in various brain regions. Finally, Delong’s test revealed that only the AUC of MAP-RTOP and NODDI-ECVF differed significantly when compared with each other ( p = 0.027 ).
Discussion
In this study, advanced diffusion models (DTI, NODDI, and MAP-MRI) demonstrate that white matter (WM) microstructural changes in Alzheimer’s disease (AD) patients are significant and may be more widespread than typically recognized. These changes in WM integrity, observed on the whole-brain scale, could provide valuable insights into alternative pathological mechanisms contributing to dementia in AD. The diffusion metrics most strongly correlated with MMSE and MoCA scores were RTOP, RTAP, ICVF, and FA, with RTOP and RTAP showing the most robust relationship to cognitive function. Overall, DTI, NODDI, and MAP-MRI appear to be clinically viable tools for identifying microstructural changes associated with AD and reflecting clinical cognitive status.
Several studies indicated that Aβ deposition is one of the AD-related pathologic changes, with impacts on synapse loss, neuron loss, and myelin degradation in the WM4,5,30,31. DWI microstructural metrics, which measure these phenomena, may provide useful and complementary information related to the onset and progression of AD pathology. The NG, NGAx, and NGRad values of the genu of the corpus callosum, splenium of the corpus callosum, anterior corona radiata, and superior corona radiata were lower in the AD group compared with the HC group. Reduced NG derived from MAP-MRI suggested reduced tissue complexity and may be associated with axon loss and demyelination in AD pathology18,19,32. Meanwhile, the decrease in RTAP, RTOP, and RTPP values of the corpus callosum, corona radiata, fornix, and cerebral peduncle may be due to neuronal density reduction and impaired fiber integrity19,33. Additionally, previous studies have noted RTAP is inversely related to the apparent diameter of the axon19,20,34. Therefore, the reduction in RTAP may be associated with an increase in axonal diameter resulting from axonal swelling. Similarly, the decreased RTOP values could be linked to axonal damage to fiber bundles, accompanied by an increase in isotropic tissue18. RTPP reflects the presence of restrictive barriers in the axial orientation. The decreased RTPP value may be linked to impaired integrity of the fibers21,35. In addition, the MSD and QIV values of frontal lobe, parietal lobe, temporal lobe, cerebral peduncles, and corpus callosum were substantially higher in the AD group, reflecting enhancement of the free diffusion of water molecules due to the loss of anisotropy of water molecules caused by the impaired fiber integrity19,36,37. These findings suggest that MAP-MRI may be sensitive to microstructural signatures of AD-related pathologic neurodegeneration.
In our NODDI model, patients with AD showed higher ECVF and ISOVF values, as well as lower ICVF values compared with HCs, may be related to the extracellular accumulation of β-amyloid protein, the formation of age-related plaques, and the excessive phosphorylation of tau protein leading to the formation of neurofibrillary tangles within neurons. These pathological changes physically constrain intracellular space, expand the extracellular matrix, and disrupt axonal integrity. Consequently, these alterations indirectly modify the anisotropic pattern of diffusion4,5. ICVF, correlating with neurite density index (NDI)38, may decrease when nerve cells are destroyed or lost, leading to a smaller volume of the intracellular space. Xiuwei Fu et al. demonstrated that there were multiple significant differences in NDI and ODI values between the HC and MCI groups15. In this study, no significant difference in the ODI values was observed between the HC and AD groups at the significant threshold, which was inconsistent with previous studies. Although ODI quantifies axonal bending and fanning in WM, which is valuable for mapping brain connectivity, the lack of significance in ODI may arise from inherent limitations of the Watson distribution used in NODDI modeling39. While ODI effectively measures fanning/bending in cylindrical fibers, its accuracy diminishes in complex regions such as kissing fibers (violating cylindrical symmetry assumptions40), crossing axons (requiring higher-order spherical harmonics for accurate representation41,42), and regions with diffuse pathological changes in AD (the complexity of astrocyte reactions in AD involving both dendritic pruning which reduces ODI and neurite beading which increases ODI43). This bidirectional effect arising from diffuse pathological processes may manifest as non-significant group differences when averaged across heterogeneous subregions.
Though DTI assumes that the diffusion of water molecules in the brain follows a Gaussian distribution, limiting its ability to detect the diffusion heterogeneity of brain tissue. However, in this study, DTI still detected extensive WM microstructural abnormalities in patients with AD44.These results emphasize the advantage of DTI in identifying brain microstructural alterations in AD. In this study, a reduction in the dendrite density was observed in the temporal lobe and hippocampus of AD patients through the NODDI model, which was consistent with the decreased FA values reported in the DTI study9. MAP detected more extensive microstructural changes across brain regions compared with NODDI, consistent with findings reported in previous studies24. This may be a consequence of the fact that MAP-MRI metrics more directly correlate with the microstructural features of brain tissue and characterize non-Gaussian diffusion profiles, which reflect more complex tissue organization18,19. Therefore, these markers may be particularly sensitive to neurodegenerative changes in AD pathology, such as axonal degeneration, demyelination, inflammation, and reduced tissue cellularity45. The above results indicate that parameters from different imaging models may capture different dimensions of the pathological process, thereby complementing our understanding of the pathological mechanism of AD.
However, most studies investigating WM hyperintensities in AD have focused on frontal and temporal regions, which are associated with memory and executive function46. In the present study, compared with the HC group, WM changes in AD were found to be more widespread than generally recognized, including alterations in the brain stem and cerebellum hemispheres, which were consistent with a study by Moody JF et al.24. The WM damage on a whole-brain scale probably plays a vital role in the clinical manifestation of AD, and an in-depth understanding of these changes may provide insight into alternative pathologic mechanisms contributing to dementia in AD.
Associations were observed between neuropsychologic scores and multiple diffusion parameters across various fiber tracts. Overall, MAP-MRI parameters outperformed NODDI and DTI parameters in their association with cognitive function. Specifically, the diffusion metrics meaningfully related to MMSE and MoCA scores included RTOP, RTAP, ICVF, and FA, with RTOP and RTAP exhibiting the most robust correlations with cognitive function. Reductions in RTOP, RTAP, ICVF, and FA in multiple brain regions of patients with AD indicate axonal degeneration, demyelination, and neuronal loss in AD pathology19,32,38,44. The findings in this study revealed that poor cognitive outcomes were associated with substantial decreases in RTOP, RTAP, ICVF, and FA, thereby highlighting the high sensitivity of these DWI metrics in detecting these such pathological processes. These results further suggest that the decline in cognitive function was associated with the pathologic changes in AD. In the AD groups, diffusion parameters in the splenium of the corpus callosum, fornix, right/left cerebral peduncle, left anterior corona radiata, and right stria terminalis showed strong correlations with cognitive function. The brain regions associated with cognition were broadly consistent with those identified in previous studies15,24,47. These relationships were particularly evident in the limbic pathways, cortico-cortical association tracts, interhemispheric tracts, and corticospinal tracts in AD. These fiber bundles play a crucial role in the interhemispheric communication and ascending and descending pathways in the brain, participating in most of the cognitive pathways24,48.
ROC analysis revealed that the AUC values of DTI-derived RD/MD and NODDI-derived ISOVF/ECVF parameters showed a relatively consistent trend in multiple brain regions. Overall, there was no significant statistical difference in AUC between the parameters after DeLong’s test, suggesting that the NODDI model is not inferior to the DTI model with traditional advantages. Furthermore, although the NODDI model did not demonstrate outstanding AUC values in multiple brain regions, it provided critical insights into neurite density and orientation dispersion, thereby complementing the findings of DTI and MAP-MRI. For the MAP model, the DeLong’s test results provided robust statistical support for the superiority of MAP-derived RTOP over NOODI-derived ECVF in the right anterior corona radiata. In this study, the RTOP, QIV, MSD, and NGAx parameters of MAP-MRI performed well in detecting AD pathology and neurodegenerative changes, consistent with previous study results24. This result may be due to the fact that MAP-MRI parameters more directly correlate with brain tissue microstructure and characterize non-Gaussian diffusion profiles that reflect more complex tissue organization19.
Although the diffusion parameters might be useful markers for evaluating the microstructural changes of AD, this study had certain limitations. First, the study lacked positron emission tomography (PET) examinations or pathologic verification confirming tau protein deposition in participants with AD and MCI. Second, the AD groups were not divided into various subtypes due to the relatively small sample size, limiting the wide applicability of the results. Third, we did not consider the presence of WM hyperintensities (WMH) in our analysis. Since previous studies have shown that DTI49 and NODDI50 parameters are associated with the presence of WMH, and the majority of individuals older than 60 years exhibit WMH, we cannot exclude the possibility that some of our results may have been influenced by heterogeneous macrostructural WM impairments across participants.
Conclusion
In summary, this study demonstrates that DTI, NODDI, and MAP models are all effective markers for studying Alzheimer’s disease (AD), with different parameters offering valuable insights into brain microstructural changes in AD patients. Future studies should aim to further expand and validate their applicability.
Data availability
The datasets used and/or analysed during this study are available from the corresponding author on reasonable request.
References
Nichols, E. et al. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: An analysis for the global burden of disease study 2019. Lancet Public. Health 7(2), e105–e125 (2022).
Nichols, E. et al. Global, regional, and national burden of alzheimer’s disease and other dementias, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet Neurol. 18(1), 88–106 (2019).
Savva, G. M. et al. Age, neuropathology, and dementia. N. Engl. J. Med. 360(22), 2302–2309 (2009).
Nasrabady, S. E., Rizvi, B., Goldman, J. E. & Brickman, A. M. White matter changes in alzheimer’s disease: A focus on myelin and oligodendrocytes. Acta Neuropathol. Commun. 6, 1–10 (2018).
Papuć, E. & Rejdak, K. The role of Myelin damage in alzheimer’s disease pathology. Archives Med. Sci. 16(2), 345–341 (2018).
Alm, K. H. & Bakker, A. Relationships between diffusion tensor imaging and cerebrospinal fluid metrics in early stages of the alzheimer’s disease continuum. J. Alzheimer’s Dis. 70(4), 965–981 (2019).
Ukmar, M. et al. Evaluation of white matter damage in patients with alzheimer’s disease and in patients with mild cognitive impairment by using diffusion tensor imaging. Radiol. Med. 113(6), 915–922 (2008).
Teipel, S. J., Meindl, T., Grinberg, L., Heinsen, H. & Hampel, H. Novel MRI techniques in the assessment of dementia. Eur. J. Nucl. Med. Mol. Imaging 35, 58–69 (2008).
Rose, S. E., Janke Phd, A. L. & Chalk, J. B. Gray and white matter changes in Alzheimer’s disease: a diffusion tensor imaging study. J. Magn. Reson. Imaging: Official J. Int. Soc. Magn. Reson. Med. 27(1), 20–26 (2008).
Jones, D. K., Knösche, T. R. & Turner, R. White matter integrity, fiber count, and other fallacies: the do’s and don’ts of diffusion MRI. Neuroimage 73, 239–254 (2013).
AL A. Diffusion tensor imaging of the brain. Neurotherapeutics 4, 316–329 (2007).
Zhang, H., Schneider, T., Wheeler-Kingshott, C. A. & Alexander, D. C. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage 61(4), 1000–1016 (2012).
Vogt, N. M. et al. Cortical microstructural alterations in mild cognitive impairment and Alzheimer’s disease dementia. Cereb. Cortex. 30(5), 2948–2960 (2020).
Parker, T. D. et al. Cortical microstructure in young onset Alzheimer’s disease using neurite orientation dispersion and density imaging. Hum. Brain. Mapp. 39(7), 3005–3017 (2018).
Fu, X. et al. Microstructural white matter alterations in mild cognitive impairment and alzheimer’s disease: study based on neurite orientation dispersion and density imaging (NODDI). Clin. Neuroradiol. 30, 569–579 (2020).
Parker, D. M. et al. NODDI-derived measures of microstructural integrity in medial temporal lobe white matter pathways are associated with Alzheimer’s disease pathology and cognitive outcomes. bioRxiv (2023).
Vogt, N. M. et al. Interaction of amyloid and Tau on cortical microstructure in cognitively unimpaired adults. Alzheimer’s Dement. 18(1), 65–76 (2022).
Avram, A. V. et al. Clinical feasibility of using mean apparent propagator (MAP) MRI to characterize brain tissue microstructure. Neuroimage 127, 422–434 (2016).
Özarslan, E. et al. Mean apparent propagator (MAP) MRI: a novel diffusion imaging method for mapping tissue microstructure. NeuroImage 78, 16–32 (2013).
Fick, R. H., Wassermann, D., Caruyer, E. & Deriche, R. MAPL: Tissue microstructure estimation using Laplacian-regularized MAP-MRI and its application to HCP data. NeuroImage 134, 365–385 (2016).
Ma, K. et al. Mean apparent propagator-MRI: A new diffusion model which improves temporal lobe epilepsy lateralization. Eur. J. Radiol. 126, 108914 (2020).
Chen, H-J. et al. White matter microstructural impairments in amyotrophic lateral sclerosis: A mean apparent propagator MRI study. NeuroImage: Clin. 32, 102863 (2021).
Le, H. et al. Mean apparent propagator MRI is better than conventional diffusion tensor imaging for the evaluation of parkinson’s disease: A prospective pilot study. Front. Aging Neurosci. 12, 563595 (2020).
MoodyJF et al. Associations between diffusion MRI microstructure and cerebrospinal fluid markers of alzheimer’s disease pathology and neurodegeneration along the alzheimer’s disease continuum. Alzheimer’s Dementia: Diagnosis Assess. Dis. Monit. 14(1), e12381 (2022).
Singh, K. et al. Neuronal microstructural changes in the human brain are associated with neurocognitive aging. Aging Cell. 23 (7), e14166 (2024).
Bouhrara, M., Avram, A. V., Kiely, M., Trivedi, A. & Benjamini, D. Adult lifespan maturation and degeneration patterns in Gray and white matter: A mean apparent propagator (MAP) MRI study. Neurobiol. Aging 124, 104 (2022).
McKhann, G. M. et al. The diagnosis of dementia due to alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s association workgroups on diagnostic guidelines for alzheimer’s disease. Alzheimer’s Dement. 7(3), 263–269 (2011).
Albert, M. S. et al. The diagnosis of mild cognitive impairment due to alzheimer’s disease: Recommendations from the National Institute on Aging-Alzheimer’s association workgroups on diagnostic guidelines for alzheimer’s disease. Alzheimer’s Dement. 7(3), 270–279 (2011).
Kodiweera, C., Alexander, A. L., Harezlak, J., McAllister, T. W. & Wu, Y-C. Age effects and sex differences in human brain white matter of young to middle-aged adults: A DTI, NODDI, and q-space study. Neuroimage 128, 180–192 (2016).
Bellucci, A. et al. Cholinergic dysfunction, neuronal damage and axonal loss in TgCRND8 mice. Neurobiol. Dis. 23(2), 260–272 (2006).
Sun, S-W., Liang, H-F., Mei, J., Xu, D. & Shi, W-X. In vivo diffusion tensor imaging of amyloid-β-induced white matter damage in mice. J. Alzheimer’s Dis. 38(1), 93–101 (2013).
Olson, D. V., Arpinar, V. E. & Muftuler, L. T. Optimization of q-space sampling for mean apparent propagator MRI metrics using a genetic algorithm. Neuroimage 199, 237–244 (2019).
Zucchelli, M. et al. What lies beneath? Diffusion EAP-based study of brain tissue microstructure. Med. Image. Anal. 32, 145–156 (2016).
Ong, H. H. et al. Indirect measurement of regional axon diameter in excised mouse spinal cord with q-space imaging: Simulation and experimental studies. Neuroimage 40 (4), 1619–1632 (2008).
Anderson, A. W. Measurement of fiber orientation distributions using high angular resolution diffusion imaging. Magn. Reson. Medicine: Official J. Int. Soc. Magn. Reson. Med. 54(5), 1194–1206 (2005).
Assaf, Y., Blumenfeld-Katzir, T., Yovel, Y. & Basser, P. J. AxCaliber: A method for measuring axon diameter distribution from diffusion MRI. Magn. Reson. Medicine: Official J. Int. Soc. Magn. Reson. Med. 59(6), 1347–1354 (2008).
Ning, L., Westin, C-F. & Rathi, Y. Estimating diffusion propagator and its moments using directional radial basis functions. IEEE Trans. Med. Imaging. 34(10), 2058–2078 (2015).
Adluru, G. et al. Assessment of white matter microstructure in stroke patients using NODDI. in 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (IEEE, 2014).
Kaden, E., Knösche, T. R. & Anwander, A. Parametric spherical deconvolution: Inferring anatomical connectivity using diffusion MR imaging. NeuroImage 37(2), 474–488 (2007).
Pereira, C. T. et al. Synchronous nonmonotonic changes in functional connectivity and white matter integrity in a rat model of sporadic alzheimer’s disease. Neuroimage 225, 117498 (2021).
Reisert, M., Kellner, E., Dhital, B., Hennig, J. & Kiselev, V. G. Disentangling micro from mesostructure by diffusion MRI: A Bayesian approach. NeuroImage 147, 964–975 (2017).
Geng, X. et al. Diffeomorphic image registration of diffusion MRI using spherical harmonics. IEEE Trans. Med. Imaging. 30(3), 747–758 (2010).
Viejo, L. et al. Systematic review of human post‐mortem immunohistochemical studies and bioinformatics analyses unveil the complexity of astrocyte reaction in Alzheimer’s disease. Neuropathol. Appl. Neurobiol. 48 (1), e12753 (2022).
Zhang, Y-Z., Chang, C., Wei, X., Fu, J-L. & Li, W-B. Comparison of diffusion tensor image study in association fiber tracts among normal, amnestic mild cognitive impairment, and Alzheimer’s patients. Neurol. India. 59(2), 168–173 (2011).
Song, S-K. et al. Demyelination increases radial diffusivity in corpus callosum of mouse brain. Neuroimage 26(1), 132–140 (2005).
Mayo, C. D. et al. Relationship between DTI metrics and cognitive function in alzheimer’s disease. Front. Aging Neurosci. 10, 436 (2019).
Canu, E. et al. Microstructural diffusion changes are independent of macrostructural volume loss in moderate to severe alzheimer’s disease. J. Alzheimer’s Disease. 19 (3), 963–976 (2010).
Li, Y. et al. Cognition-related white matter integrity dysfunction in Alzheimer’s disease with diffusion tensor image. Brain Res. Bull. 143, 207–216 (2018).
Svärd, D. et al. The effect of white matter hyperintensities on statistical analysis of diffusion tensor imaging in cognitively healthy elderly and prodromal alzheimer’s disease. PloS One 12(9), e0185239 (2017).
Raghavan, S. et al. Diffusion models reveal white matter microstructural changes with ageing, pathology and cognition. Brain Commun. 3(2), fcab106 (2021).
Acknowledgements
I would like to thank all members of the Department of Radiology and Department of Neurology of Zigong First People’s Hospital.
Funding
This work is funded by grants from the Zigong City Key Science and Technology Plan Project (No. 2022ZCNKY04) and the Zigong Public Hospital Reform and High-Quality Development Demonstration Project in 2023 (No. ZG-KY-2023-008).
Author information
Authors and Affiliations
Contributions
In this project, JQ. Z. provided the overall conceptualization and team management. ML. L., J. Y., KC. Z., H. F., XY. X. and Y. L. collectively conducted the data collection. J. Y. was responsible for data organization and statistical analysis. ML. L. and J. Y. are responsible for the revision of the article together. All authors contributed to the article and agreed to the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
The patients/participants provided their written consent to participate in this study.
Institutional review board statement
The research involving human subjects was examined and approved by the Ethics Committee of Zigong First People’s Hospital (protocol number: Ethics(Reseach) No. 36, 2023).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lv, M., Zhan, K., Yang, J. et al. Analysis of advanced diffusion models assessing white matter microstructure in Alzheimer’s disease. Sci Rep 15, 26266 (2025). https://doi.org/10.1038/s41598-025-09412-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09412-1
Keywords
This article is cited by
-
Insights into the molecular mechanism of neurological diseases and their pathophysiological responses
Archives of Toxicology (2025)