Abstract
This study has investigated Coxiella burnetii and HIV infection among the persons experiencing homelessness of São Paulo city, Brazil, and assessed correspondent associated risk factors. A cross-sectional study was carried out with 203 individuals performing serological tests for anti-C. burnetii and anti-HIV antibodies. A prevalence of 14.8% (30/203) was found for anti-C. burnetii IgG antibodies, with titers ranging from 64 to 1024, while anti-HIV seroprevalence was 6.4% (13/203). No statistical association was found between C. burnetii and HIV seropositivity, or between seropositivity and assessed clinical and epidemiological variables. The findings herein highlight the high homelessness exposure to Q fever, possibly influenced by environmental factors such as dust aerosols, stray animal interactions and unsanitary living conditions. To the authors knowledge, this is the first serosurvey of C. burnetii in persons experiencing homelessness to date. The study herein has emphasized the importance of public health strategies targeting vulnerable populations, particularly in Brazilian major cities. Further C. burnetii surveys should be conducted to establish whether transmission may occur in other persons experiencing homelessness worldwide.
Similar content being viewed by others
Introduction
Although the epidemiology of Q fever, caused by Coxiella burnetii, remains largely unknown and challenging to be fully understood, recent studies have shown that this pathogen has been capable of infecting a wide range of vertebrate and invertebrate hosts, including livestock, wildlife, companion animals, and arthropods such as ticks1. Vulnerable urban populations, particularly people experiencing homelessness, may be exposed and in contact with a variety of vertebrate and invertebrate animals that have been associated with transmission of zoonotic pathogens, including pigeons, rodents, mosquitoes, body lice, and fleas2. People experiencing homelessness are often in close contact with stray and unneutered cats and dogs, which may act as C. burnetii reservoirs3. Although the bacterium shedding during parturition has been well documented in ruminants, few reports have also suggested that companion animals, particularly dogs, may transmit the pathogen during their reproductive events3,4. Notably, a report of Q fever outbreak within family members was linked to the birth of an infected dog4.
As people experiencing homelessness have mostly lived and slept outdoors, such chronic environmental exposure in urban settings has included excessive sun, rain, dust, pollution, unsafe drinking and eating, and related pathogens5. During the COVID-19 pandemics, persons experiencing homelessness living in São Paulo presented 54.7% (111/203) IgG seropositivity, the highest prevalence worldwide at the time6. In addition, 47.1% (41/87) of shelter workers were also seropositive, posting airborne exposure also as professional risk. Such high SARS-CoV-2 seroprevalence indicated early and highspeed spreading of homeless people infection, associated with sociodemographic and economic vulnerability. In the case of Q fever, reports indicate that C. burnetii spores may be easily transported attached to dust particles, carried by wind and aerosolization travel more than 30 km away7. As unsafe food may be another critical factor to C. burnetii infection among people experiencing homelessness, with consumption of uninspected or improperly stored food, including discarded animal products such as unpasteurized milk and raw meat as associated risk factors for infection.
The poor homeless living conditions may include a nutritionally deficient and insufficient diet, alcohol and drug abuse, which altogether may lead to stress and immunosuppression, exacerbating infection as observed in other vulnerable populations8. In addition, seropositivity for both Q fever and HIV may be particularly alarming, as persons experiencing homelessness have reportedly shown comparative higher HIV seroprevalence and onset, mostly due to unsafe sex and drug injection sharing, leading to syphilis and hepatitis C coinfection, followed by difficult access or incompleteness of antiviral treatment9. Although social vulnerability has already been previously associated with Q fever, to the authors knowledge, no study to date has surveyed persons experiencing homelessness10.
Studying megacities in developing countries is essential to understand public health dynamics in settings of high population density, social inequalities, and adverse environmental conditions. These locations represent an environment conducive to the circulation of infectious diseases, especially in vulnerable populations, such as people experiencing homelessness, who face multiple risk factors, including exposure to zoonotic pathogens and immunosuppression11. Accordingly, the present study aimed to assess anti-C. burnetii antibodies in persons experiencing homelessness living in the city of São Paulo, along with potential HIV seropositivity and associated risk factors.
Results
In overall, the prevalence of anti-C. burnetii IgG antibodies among the persons experiencing homelessness in the city of São Paulo was 14.78% (30/203) (95% CI 10.55–20.31). Among the seropositive individuals, 21 presented a titer of 64, 6 a titer of 128, 2 a titer of 256 and 1 a titer of 1024. The prevalence of HIV antibodies was 6.40% (13/203) (95% CI 3.78–10.65). Only in one individual was seropositive for both C. burnetii and HIV. Association between serological results and the variables considered as potential associated risk factors for infection was assessed and presented (Table 1). No statistically significant association was found between Q fever seropositivity and analyzed variables, including HIV seropositivity.
Discussion
To the authors knowledge, this is the first report of C. burnetii serological survey and associated risk factors in persons experiencing homelessness to date. The seroprevalence of anti-C. burnetii IgG antibodies identified herein has shown the importance of investigating vulnerable urban populations, who may be exposed to social and environmental conditions favoring infection, particularly by zoonotic pathogens, including Bartonella spp., Rickettsia spp., Leptospira spp., Toxoplasma gondii, Toxocara canis, Trypanosoma cruzi and SARS-CoV-26,12,13,14,15,16,17.
The study has identified a 14.8% prevalence of anti-C. burnetii antibodies and 6.4% of anti-HIV antibodies in the persons experiencing homelessness of São Paulo city. The seropositivity for both C. burnetii and HIV was observed in only one out of 203 individuals, with no statistical association of risk factors with C. burnetii seropositivity including age, raw meat consumption, presence of rats, drug use and stray pet ownership.
The overall seroprevalence of C. burnetii in asymptomatic populations has widely varied, influenced by country, occupation and contact with infected reservoirs17. In Brazil, epidemiological surveys indicate an average of 3% prevalence1while in Australia, an endemic country for Q fever, the prevalence may reach up to 10% 2. The prevalence has also been usually higher in rural and meatpacking workers, due to exposure risk during daily labor, and the highest prevalences recorded to date, as expected, in symptomatic populations18.
The seroprevalence herein was higher than 0.9% (8/893) indigenous individuals8 and 8% (25/309) forest rangers and zoo workers19and lower than 22% (44/200) quilombola (former Black slave) and 34% (139/413) female inmates20. Proximity to farm animals, intimate contact and isolation, and interaction with wildlife have been associated with C. burnetii exposure in Brazil.
The C. burnetii ability to survive in dust particles and be transported by wind over long distances may greatly increase the possibility of infection in such a high vulnerability scenario21as observed in the present study. In addition, the present study has focused on the human population, with no survey in stray dogs, cats and other animal species with potential homeless interaction. As animal contact may have contributed to the C. burnetii exposure22such transmission route should be further investigated.
In addition, although a previous study in southern Brazil has shown a higher Q fever prevalence in injectable drug users23statistical analysis herein has shown no association of drug use, even with immunosuppressive agents, with C. burnetii seropositivity. Although direct contact with pets has apparently not influenced Q fever seropositivity22no data was available on the pet reproductive history, and such limitation should be further investigated.
Also, molecular testing could be useful for identifying active C. burnetii infections, particularly in symptomatic individuals24. However, PCR sensitivity has been limited even in acute cases, and its use in the asymptomatic homeless population herein could be even more restricted due to the low probability of detectable bacteremia25. The current recommendation of diagnostic approach in symptomatic patients has been paired serology, as PCR may rarely detect the bacterium in blood samples26.
As a limitation, the present study has not included a control group composed of non-vulnerable individuals living in the same urban setting, that may determine whether the observed seroprevalence among people experiencing homelessness was significantly higher than general urban population. Future studies may include comparative groups to better understand potential disparities in exposure.
These findings suggest that people experiencing homelessness, due to their heightened exposure to environmental and social risk factors, may represent a neglected population that could provide early warning signs of zoonotic pathogen circulation in urban areas. This highlights the importance of including this vulnerable population in zoonotic pathogen surveillance efforts and the need to reduce social disparities.
Methods
Ethical statement
The present research was approved by the Human Research Ethics Committee, Brazilian Ministry of Health, through the Federal University of Paraná (CAAE: 80099017.3.0000.0102, protocol number 2,512,196) and by the Human Health Ethics Committee of the Municipal Health Department of São Paulo (CAAE: 80099017.3.3004.0086, protocol number 3,366,684). All study participants were informed, voluntary signed a Free and Informed Consent Form, and received their undisclosed results, in compliance with the Brazilian General Data Protection Law.
Study area
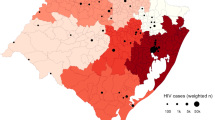
This study was conducted in the São Paulo city (23°33′1″ S, 46°38′2″ W), capital of São Paulo state, located in the southeastern Brazil, and ranked the most populous city and with the largest Gross Domestic Product (GDP) in Latin America, with over 12 million inhabitants27. São Paulo presented a high Human Development Index (HDI) (0.805) at the time of survey, with a humid subtropical climate, and average temperatures ranging from 19 °C in winter to 25 °C in summer27.
The survey was conducted in partnership with the city team as part of official duties of multi-tasking professionals at the São Paulo City Secretary of Health, known as the “street clinic”, composed by clinicians, nurses, dentists, social workers and psychologists, as part of the Brazilian Unified Health System (SUS) strategy. The street clinic official team provides continuous care to the people experiencing homelessness, keeping medical records and providing health care in a permanent follow-up approach.
The descriptive, cross-sectional study was carried out with the persons experiencing homelessness attended at the Our Lady of Good Childbirth (Nossa Senhora do Bom Parto) Shelter, a non-governmental organization located on western São Paulo, funded by the city hall, and daily receiving around 800 to 1,200 persons experiencing homelessness, providing breakfast, lunch and dinner meals, medical assistance, work activities and leisure options.
Sample collection
Blood samples from people experiencing homelessness were conveniently collected in a four-day survey in August 2020, as permitted by the City Secretary of Health. A sample size of 203 individuals was calculated using a commercial software Epi Info 7.7.7.6 28, considering an estimated 16,000 persons experiencing homelessness at the time in the city of São Paulo, an HIV infection prevalence of 4.9%, a 95% confidence level, and a precision of 5%. Participants were informed during Shelter activities and invited to voluntarily participate in the study, with blood collection performed by cephalic puncture, conducted by a certified nurse. Samples were placed into tubes without anticoagulant and kept at 25 °C until visible clot retraction. Subsequently, the serum was separated by centrifugation at 3,000 revolutions per minute for 10 min and stored at − 20 °C until processing. During the samplings, researchers ran a clothing drive donation and provided clean clothing to needed.
Epidemiological data collection
The epidemiological analyses were based on a questionnaire taken from all participants by interview, which included: (1) Demographic profile: gender, self-declared race and age; (2) Social profile: having a pet, raw meat consumption, presence of rats in the sleeping area and use of licit and illicit drugs; (3) Health profile: symptoms related to Q fever (fever, myalgia, headache, difficulty breathing, sore throat and dry cough) in the last six months and diagnosis of HIV. Refusal to partially or totally answer any question was accepted and recorded.
Coxiella burnetii serology
Human serum samples were tested by indirect immunofluorescence assay (IFA), performed with Vero cells infected by C. burnetii antigen strain At12, and serum tested in 1:64 dilutions using a conjugated anti-human IgG, based on the protocol previously described by França et al.27modified by the use of IgG-specific conjugate. Human patients previously tested at the routine laboratory were used as positive and negative controls. The positive samples were further tested to serial dilutions and titrated according to the last dilution in which luminescence was observed.
HIV serology
HIV detection was conducted using a chemiluminescent microparticle immunoassay (CMIA) method, employing a commercially available HIV Ag/Ab Combo Reagent Kit (Alinity, Abbott Laboratories, Chicago, IL, USA). Such assay has enabled the simultaneous qualitative detection of HIV p24 antigen and antibodies against HIV type 1 (HIV-1 groups M and O) and/or type 2 (HIV-2) in human serum. The resulting chemiluminescent reaction was quantified in relative light units (RLU). Reactive serology cases were confirmed with a commercially available rapid immunoblot assay (DPP HIV1/2, Fiocruz, Rio de Janeiro, Brazil). Additionally, samples from pregnant women and individuals with HIV were tested for T. gondii IgM using CMIA with a commercial Toxoplasmosis IgM Reagent Kit (Alinity Abbott Laboratories, Chicago, IL, USA).
Data analysis
Epidemiological questionnaire and HIV seropositivity data were gathered and tested as associated risk factors to C. burnetii seropositivity. Univariate analyses were performed using Pearson’s chi-square test to estimate crude prevalence ratios (PRs) and 95% confidence intervals. Variables also were included in a multivariate Poisson regression model with robust variance to calculate adjusted PRs. The most suitable model was selected based on variables with statistically significant associations (p < 0.05). All statistical analyses were conducted using SAS Studio 3.81 (SAS Institute Inc., Cary, NC, USA).
The initial missing data in the epidemiological questionnaires were later fully completed by researchers on a specific visit, with daycare shelter database accessed, some persons reinterviewed, information and analyzed variables carefully reviewed. Thus, all participants included in the study herein provided complete responses for the considered variables, used in the statistical analysis for Q fever.
Potential sources of biased and confounding factors were also considered. Multivariate analyses using Poisson regression with robust variance were performed. Thus, potential confounding factors were adjusted in the estimation of adjusted prevalence ratios (PRs).
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
França, D. A. et al. Overview of Q fever in Brazil: An underestimated zoonosis. Rev. Inst. Med. Trop. Sao Paulo. 65, e39 (2023).
Eldin, C. et al. From Q fever to Coxiella burnetii infection: A paradigm change. Clin. Microbiol. Rev. 30, 115–190 (2017).
de França, D. A. et al. Serosurvey of Coxiella burnetii in police officers and working dogs in Brazil: Case report and one health implications. Trop. Med. Infect. Dis. 9, 78 (2024).
Dog-Related Outbreak of Q Fever | Clinical Infectious Diseases | Oxford Academic. https://academic.oup.com/cid/article-abstract/23/4/753/290020?redirectedFrom=fulltext&login=false
Fazel, S., Geddes, J. R. & Kushel, M. The health of homeless people in high-income countries: Descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet 384, 1529–1540 (2014).
do Couto, A. C. et al. High SARS-CoV-2 Seroprevalence in persons experiencing homelessness and shelter workers from a day-shelter in São Paulo, Brazil. PLoS Negl. Trop. Dis. 15, e0009754 (2021).
Tissot-Dupont, H. & Raoult, D. Q fever. Infect. Dis. Clin. North Am. 22, 505–514 (2008). ix.
Farinhas, J. H. et al. One health approach to Coxiella burnetii in Brazilian Indigenous communities. Sci. Rep. 14, 10142 (2024).
Pinheiro, R. S. et al. Human immunodeficiency virus infection and syphilis among homeless people in a large City of Central-Western Brazil: Prevalence, risk factors, human immunodeficiency virus-1 genetic diversity, and drug resistance mutations. Braz. J. Infect. Dis. 25, 101036 (2021).
Montes, M., Cilla, G., Marimon, J. M., Diaz de Tuesta, J. L. & Perez-Trallero, E. Coxiella burnetii infection in subjects with HIV infection and HIV infection in patients with Q fever. Scand. J. Infect. Dis. 27, 344–346 (1995).
Felipetto, L. G. et al. Serosurvey of Anti-Toxoplasma gondii antibodies in homeless persons of São Paulo city, southeastern Brazil. Front. Public. Health 8, 580637 (2020).
Kmetiuk, L. B., Gonçalves, G., Do Couto, C., Biondo, A., Figueiredo, F. B. & A. W. & Serosurvey of trypanosoma Cruzi in persons experiencing homelessness and shelter workers of Brazil. Front. Public Health 11, 1125028 (2023).
Faccini-Martínez, Á. A. et al. Bartonella spp. and typhus group rickettsiae among persons experiencing homelessness, São paulo, Brazil. Emerg. Infect. Dis. 29, 418–421 (2023).
do Couto, A. C. et al. One health approach on serosurvey of anti-Leptospira spp. In homeless persons and their dogs In South Brazil. One Health 15, 100421 (2022).
Santarém, V. A. et al. Serosurvey of anti-Toxocara canis antibodies in people experiencing homelessness and shelter workers from São Paulo, Brazil. Parasites Vectors 15, 373 (2022).
Felipetto, L. G. et al. Serosurvey of anti-Treponema pallidum (syphilis), anti-hepatitis C virus and anti-HIV antibodies in homeless persons of São Paulo city, southeastern Brazil. Braz. J. Infect. Dis. 25, 101602 (2021).
Anderson, A. et al. Diagnosis and management of Q fever–United States, 2013: Recommendations from CDC and the Q Fever Working Group. MMWR Recomm Rep. 62, 1–30 (2013).
França, D. A. et al. Seropositivity for Coxiella burnetii in suspected patients with dengue in São Paulo state, Brazil. PLoS Negl. Trop. Dis. 16, e0010392 (2022).
de França, D. A. et al. Coxiella burnetii (Q fever) exposure in wildlife professionals. Front. Public Health 12, 1466981 (2024).
Serosurvey of Coxiella burnetii in Descendants of Former Black Slaves. (Quilombola Communities) of Southern Brazil. https://www.mdpi.com/2076-2607/12/1/92
Clark, N. J. & Soares Magalhães, R. J. Airborne geographical dispersal of Q fever from livestock holdings to human communities: A systematic review and critical appraisal of evidence. BMC Infect. Dis. 18, 218 (2018).
Celina, S. S. & Cerný, J. Coxiella burnetii in ticks, livestock, pets and wildlife: A mini-review. Front. Vet. Sci. 9, 1068129 (2022).
Rozental, T. et al. Seroprevalence of Bartonella spp., Coxiella burnetii, and hantavirus among people who inject drugs in Rio de Janeiro, Brazil: A retrospective assessment of a biobank. Rev. Inst. Med. Trop. Sao Paulo. 60, e31 (2018).
Ghanem-Zoubi, N. et al. The integration of Coxiella burnetii PCR testing in serum into the diagnostic algorithm of suspected acute Q fever in an endemic setting. J Clin. Microbiol. 62, e01703–e01723 .
Cherry, C. C., Nichols Heitman, K., Bestul, N. C. & Kersh, G. J. Acute and chronic Q fever National surveillance—United states, 2008–2017. Zoonoses Public. Health 69, 73–82 (2022).
CDC. Clinical and laboratory diagnosis for Q fever. Q Fever (2025). https://www.cdc.gov/q-fever/hcp/diagnosis-testing/index.html
de França, D. A. et al. Comparison of three serologic tests for the detection of anti-Coxiella burnetii antibodies in patients with Q fever. Pathogens 12, 873 (2023).
Epi Info™ 7 User Guide.
Acknowledgements
We would like to thank Sandro Ricardo Ruys, Father Júlio Renato Lancellotti and the São Martinho de Lima Community Center for helping with the collection, sampling, epidemiological questionnaires and follow-up information.
Author information
Authors and Affiliations
Contributions
L.B.K., A.W.B., made substantial contributions to the conception; D.A.F., L.B.K., A.C.C., H.L., A.W.B. designed the study; D.A.F., H.L. conducted the analysis, D.A.F., H.L., interpreted the data; D.A.F., A.W.B. drafted the article. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de França, D.A., Kmetiuk, L.B., do Couto, A.C. et al. Coxiella burnetii and HIV infection in people experiencing homelessness. Sci Rep 15, 28312 (2025). https://doi.org/10.1038/s41598-025-09422-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-09422-z