Abstract
Vulvovaginal candidiasis is a common fungal infection in the reproductive age group of women with an estimated 70–75% of women infected at least once in their life cycle. A chronic condition, recurrent vulvovaginal candidiasis, significantly affects the quality of life in women globally. Hydrogel-based wound dressing has emerged as effective choices for wound closure, as they can mimic the structure and physicochemical properties of the extracellular matrix. However, they are frequently linked with limited biocompatibility, and a deficiency in antifungal activities. Herein, a biocompatible composite sponge-like hydrogel with effective antifungal activities is developed for the management of such wound infections. Synthesis and characterization of a sponge-like protein based hydrogels comprising keratin, gelatin (Kr/Gel), and fluconazole (Kr/Gel@Flu) were engineered via a cryogelation process. The formulation was cross-linked by sodium alginate as a cross-linker. The physicochemical properties of the hydrogels were characterized using Fourier transform infrared spectroscopy, scanning electron microscopy, and energy-dispersive X-ray. Additional physicochemical characterizations involved its moisture content (3.70 ± 0.83% Kr/Gel@Flu), water vapor transmission rate (1438 g/m2/per day for Kr/Gel@Flu), porosity (a porosity value of 76% in the Kr/Gel@Flu), and release (21.61% release of Flu from Kr/Gel@Flu within the first 360 min) properties. The hydrogels demonstrated a fibrous structure with appropriate moisture content, indicating its potential for maintaining wound environment. The formulation exhibited significant antifungal, and antibiofilm properties also supported normal skin fibroblast and HeLa cell lines growth in vitro that confirmed their biocompatibility. In conclusion, sponge-like hydrogel combines the advantages of targeted antifungal delivery, antibiofilm activity, and biocompatibility, making it a promising candidate for biomedical applications.
Similar content being viewed by others
Introduction
Vaginitis, or vulvovaginal candidiasis, is a yeast fungal infection. This mucocutaneous fungal infection is caused most frequently by the fungus Candida albicans. It is characterized by vagina pruritus, dyspareunia, urinary pain, and abnormal vaginal discharge. It usually occurs in reproductive women. It is estimated that 70% of women develop this infection once in their lifetime1. It was previously recognized that Candida species can disrupt the microbial flora balance of the skin and mucous membranes and their barrier integrity. Therefore, infection-related inflammation in this instance can be associated with an unfavorable course of the wound2.
Fluconazole (Flu) is one of the widely used triazole antifungal agents, with the IUPAC name 2-(2,4-difluorophenyl)-1,3-bis(1 H-1,2,4-tria-zol-1-yl)-propan-2-ol]. The antifungal agent selectively inhibits the fungal enzyme lanosterol 14α-demethylase (CYP51), which is a cytochrome P450-dependent enzyme involved in the metabolism of lanosterol to ergosterol, a key component of the fungal cell membrane. By blocking this step, Flu causes toxic methylated sterols to accumulate while depleting ergosterol, thereby disrupting membrane integrity and function3,4. This leads to increased permeability, impaired fungal growth, and interference with membrane-bound enzymes, including those involved in ATP production5,6. Flu is primarily fungistatic against most fungi, particularly Candida species, but is fungicidal at higher concentrations. Its specificity for fungal CYP450 over human enzymes minimizes toxicity in mammalian cells7. Flu is broad-spectrum, active against Candida, Cryptococcus, and some dermatophytes, and is available in number of formulation and administration routes of delivery, including oral, intravenous injection, and vaginal cream preparations. Oral or systemic Flu administration exhibits a high volume of distribution, leading to adverse effects like nausea, vomiting, and abdominal discomfort, which may limit patient compliance3,8. However, both inherent and acquired resistance to Flu have been reported. This resistance can develop through CYP51 mutations, efflux pump overexpression, or altered sterol biosynthesis pathways9,10. Formulations containing Flu applied vaginally have the potential to improve drug bioavailability to target tissue and, therefore, reduce dosing frequency and enhance therapeutic outcomes in vulvovaginal candidiasis11. However, classical vaginal formulations have a short duration of action since the cervicovaginal fluid is washed out of drug products over time, necessitating frequent applications are required. This has motivated the development of new systems capable of improving efficacy and convenience in the treatment of vaginal infections10,12.
Sponge-like hydrogel are gel matrices with a macroporous three-dimensional structure. These materials are prepared by a procedure termed cryotropic gelation, which involves forming a gel in the presence of ice crystals at subzero temperature13. These platforms hold promise for revolutionizing drug delivery in treating vaginal candidiasis14,15,16. Their unique properties make them particularly well-suited for this application. These formulations boast a high absorption capacity, allowing them to encapsulate a larger dose of antifungal medication, such as Flu, and enable a controlled release of the encapsulated drug over time14,17,18. This sustained release provides longer-lasting antimicrobial activity in the vagina, overcoming the limitations of conventional treatments that may be easily washed away. Thus, the high water content in sponge-like hydrogel offers more comfort to patients by imitating the natural environment of the vagina19. The procedure of freeze-thawing and drying for the fabrication of these products could be varied to regulate the size and the level of interconnectedness of the pores. So, vaginal sponge-like hydrogels are a new drug delivery system that has many merits and is more acceptable for women compared to cream due to their small size, ease of use, leakage prevention, economic production, and easy administration without an applicator15,16. Hydrogel can be loaded with a wide range of antimicrobial agents such as antibiotics, antiseptics, and non-antibiotic antimicrobial substances, which may also include natural materials20. The drug delivery platform formulated with natural substances can help address the growing problem of antibiotic resistance to azole antifungals, particularly Flu7,20,21.
Interest in biopolymers has been increased by biocompatibility, biomimetic properties, biodegradability, low toxicity, and various biomedical applications. These are some of the proteins tried by various researchers for the preparation of different biopolymer-based formulations such as films, hydrogels, nanofibers, 3D-printed scaffolds, and drug delivery systems22,23,24,25. Nowadays, keratin (Kr) is one of the versatile biomaterials that has been of widespread interest in fabricating scaffolds for application in tissue engineering. Besides that, Kr had superior structural and functional properties: it allows attachment but also acts as an extracellular controllable matrix. According to these considerations, Kr represents a promising biomaterial to be employed in the development of tissue engineering constructs as well as wound healing applications26,27. Sodium alginate (SA) is a structural biopolymer obtained from brown algae. Recently, its application has increased commercially in hydrogel-based wound dressings28,29. SA is a linear anionic polysaccharide capable of forming gels, which are three-dimensional networks capable of encapsulating the anti-microbial agent. Its great antimicrobial property is related to its ability to absorb exudates coming out of the wound and keeping it in a moist condition, which is crucial to maintain healthy healing with prevention against infection28,30. Gelatin (Gel) is a widely used biomaterial for fabricating wound dressing due to its excellent biocompatibility, biodegradability, and ability to mimics the body’s environment for a moist healing process31,32.
The primary objective of this study is to formulate the sponge-like Kr and Gel-based hydrogels incorporating Flu. The prepared hydrogels were tested for physicochemical properties and stability profile, drug release, antifungal activity, and biocompatibility. We have emphasized the rationale behind our research by discussing the limitations of current antifungal treatments, such as poor patient compliance due to side effects and short action duration of conventional formulations. The formulation can address these issues by providing a controlled release of antifungal agents, thus improving therapeutic outcomes (Fig. 1).
Schematic overview of the study rationale and workflow. This figure provides a graphical summary of the study’s conceptual framework and experimental approach. The diagram outlines the main hypothesis, key methodological steps, and anticipated outcomes. Major stages of the research process including sample preparation, experimental intervention, data collection, and analysis are depicted sequentially.
Result and discussion
FTIR analysis
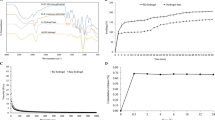
As shown in Fig. 2, in the structure of the Kr/Gel@Flu sponge-like hydrogel, the broad absorption peak around 3200 cm−1 is referred to the stretching vibration of N–H and O–H in Kr (named as Amide A)33 overlapping with the stretching vibration of N–H in Gel34, O–H in the structure of Flu35, and alcoholic O–H in crosslinking agent36. The observed peaks in the structure of the formulated sample at 2900 and 2850 cm−1 are associated with CH2 aliphatic groups and C–H methyl stretching band in Gel, Kr, and crosslinker36,37. The bands around 1600 cm−1 and 1400 cm−1 correspond to amide I and amide II (with a shift) related to the structure of Kr (for C=O stretching), which are representative of α-helical conformation33,38.
Additionally, the band at 1600 cm−1 is associated with the stretching mode of the aromatic ring39, as well as C=C, and C=N vibrations in Flu35,40. The peaks at 1400 cm−1 and 1252 cm−1 can be attributed to the vibrations of C–N and C–F, respectively, related to the Flu structure41. Moreover, the peak observed in 1400 cm−1 is related to the stretching vibrations of C–N and amide N–H in the structure of Gel (with a shift)42, which overlaps with the symmetric stretching vibration of carboxylate salt ion in the structure of SA36. The band located at 1230 cm−1 is attributed to Amide III in the structure of Kr resulting from C–N stretching and N–H bending43. The peaks located at 1280 and 950 cm−1 are attributed to an in-plane C-H triazole ring of Flu39. The FTIR spectrum of Kr/Gel@Flu hydrogel confirms the presence of components in this final matrix.
Scanning electron microscopy (SEM) and energy dispersive X-ray (EDX) studies
The morphology of three synthesized sponge-like hydrogel is displayed in Fig. 3. The SEM image of Kr/Gel sample (A) appears to be porous, fibrous, and layered. The surface seems relatively smooth with fewer irregularities. The layered and fibrous structure suggests a porous structure, which could provide a higher surface area for cell attachment, growth, and migration. The smooth surface and well-defined layers may indicate a more uniform pore size distribution, which could facilitate cell infiltration and nutrient exchange. The addition of Flu to this mixture results in a high density of fibers that are closely packed together. This dense packing can reduce the porosity of the hydrogel, as there are fewer spaces for pores to form. Since Gel and Kr can interact strongly, leading to the formation of a dense network. The strong interactions between these biopolymers can result in a more compact structure with fewer pores. The SEM image of Kr/Gel@Flu sponge-like hydrogel (B) seems more irregular and less organized compared to other samples. There are more rough surfaces. The presence of Flu seems to have disrupted the uniformity, leading to a more heterogeneous texture.
The incorporation of Flu might reduce the porosity of the final sample. The other result of cross-linking can be a more rigid, less porous structure. Elemental analysis of the samples using EDX was conducted to confirm the presence of components. As shown in Fig. 4, the presence of carbon (C), nitrogen (N), oxygen (O), sulfur (S), and phosphorus (P) in the samples is related to their components. The signals of S and P can be attributed to Kr. The EDX spectra of Kr/Gel@Flu clearly showed the presence of fluorine (F), while Kr/Gel sponge-like hydrogel did not show any F, indicating successful synthesis of hydrogels containing Flu.
Mechanical test of the hydrogels
The toughness and superfast swelling of sponge-like hydrogels allow them to better address the needs of various wound types9. Young’s modulus represents the stiffness of the materials, while the compression strength indicates the maximum stress of the material that can withstand before failing. In the current investigation, as shown in Table 1, Kr/Gel@Flu has the highest stiffness, followed by Kr/Gel representing that Flu affect the mechanical properties of the samples. Because Flu, an antifungal agent, can lead to increased interactions between the molecules and protein chains of Kr and Gel. These interactions can enhance the structural integrity of the hydrogel, resulting in improved mechanical properties, which may be helpful in biomedical applications.
Moisture content determination of hydrogel samples
The moisture content is the amount of water or volatile liquid contained within the hydrogel material. This may be altered depending on the nature or composition of the hydrogel samples, cross-linking density, or prevailing ambient surroundings. The presence of moisture at the wound site helps in preventing dehydration and accelerates the healing process. This is achieved by facilitating the migration of cells, the formation of blood vessels, and finally, collagen synthesis44. In the current study, the moisture content (%) was achieved as 4.55 ± 1.93%, and 3.70 ± 0.83%, for Kr/Gel, and Kr/Gel@Flu, respectively (Table 2). Generally, the combined effect of Flu in Kr/Gel@Flu can result in a balance between water binding and water-repelling properties. This balance can lead to a moisture content that is lower than that of the Kr/Gel hydrogel. A similar decrease in moisture content of a cryogel including was reported by Valentina Dinu et al.45.
Porosity
The porosity of sponge-like hydrogels used for wound healing applications can differ depending on its composition and intended use. It has been demonstrated that porosity is a key factor in facilitating cell penetration, nutrient transport, and overall effectiveness of wound healing46. As presented in Table 2, a porosity value of 76% was observed for the Kr/Gel@Flu, while Kr/Gel showed porosity of about 90%. The differences in porosity between the samples can be attributed to the interactions between the components and their effects on the gelation process. In Kr/Gel, the Gel and Kr molecules interact through hydrogen bonding, creating a network that traps water, resulting in a more porous structure. This is because Gel and Kr are both hydrophilic, facilitating their interaction. The addition of Flu in Kr/Gel@Flu might change the porosity, as it is a small molecule that might affect the gelation process or the interactions between Gel and Kr. Scaffolds with a porosity range of 60–95% have been known as the most suitable for wound healing and tissue regeneration applications, as they facilitate essential cellular activities (oxygenation and nutrient exchange). For instance, Jaidev et al. developed a 3D-printed poly lactic acid scaffold with 70.2% porosity47, while Ju et al. fabricated a poly butylene succinate/cellulose scaffold with an extremely porosity (95.2%)48. Similarly, the porosity of the 3D COL-SPG (collagen sponge), COL-SPG-D (COL-SPG that has been chemically modified or crosslinked with a specific agent) and COL-SPG-CPE (COL-SPG-Coccinia grandis plant extracts) exhibited with liquid displacement method was found to be 75, 80 and 88% respectively49.
Water vapor transmission rate
The water vapor transmission rate (WVTR) is a measure of the amount of water vapor that passes through a material over a specific period. A high value of WVTR can cause the wound to dry more quickly, resulting in the formation of scars. On the other hand, a low amount of WVTR can lead to excessive exudate, which hinders the healing process and increases the risk of microbial growth20,50. In the current investigation, Kr/Gel and Kr/Gel@Flu showed WVTR of 1529.31 and 1438 g/m2/day, respectively (Table 2). This difference in WVTR can be attributed to the presence of Flu, which may have altered the structure and properties of the hydrogel matrix. These components could have contributed to a denser or more compact structure, reducing the pathways for water vapor transmission. In addition to porosity, the WVTR of wound dressings plays a crucial role in maintaining an optimal healing environment. Studies by Sobhanian et al. demonstrated that collagen grafting reduced WVTR from 1625.65 to 1575.72 g/m2/day closely matching to thepresent study51, while Letha et al. reported a lower WVTR of 1172 g/m2/day for a polyurethane-gelatin scaffold52. Together, these findings highlight the critical interplay between scaffold porosity and WVTR in effective wound healing and tissue regeneration.
Wound fluid uptake
When a hydrophilic polymeric matrix is exposed to a moist environment, it begins to swell. This happens because water molecules enter the matrix due to a concentration gradient and the increased movement of the polymer chains. This phenomenon is known as “polymer chain relaxation or hydration”53. In the current investigation, the wound fluid uptake, indicating the amount of swelling was investigated, and the results are displayed in Fig. 5. The swelling percentage of Kr/Gel@Flu increases with time, reaching a maximum of about ~ 90% after 210 min, while the Kr/Gel sample dissolve. This difference in the amount of swelling can be attributed to the combined effects of Flu and polymeric matrix. Flu is a water-soluble drug that can bind to water molecules and increase the water content of the formulated hydrogel. The Kr/Gel@Flu sponge-like hydrogel can effectively absorb excess vaginal secretions associated with infections. This absorption capacity helps alleviate discomfort and prevents wound or irritation formations in the delicate vaginal area. The hydrogel’s ability to manage the excess moisture contributes to improved treatment outcomes by creating a more favorable, healing-conducive environment within the vagina54.
Release
The release process for Kr/Gel@Flu was studied for 540 min. The graph for Kr/Gel@Flu (Fig. 6) shows a rapid increase in Flu within the first 360 min (21.61%). This indicates a significant amount of Flu is released quickly. The release process for Kr/Gel@Flu increases gradually within the first 360 min.The observed burst release can be attributed to: the presence of drug molecules on or near the surface of the sponge-like hydrogels; and rapid swelling of the sample, which facilitates the quick release of the drug. The release processes revealed that Kr/Gel@Flu shows a more prominent burst release, indicating that more Flu is readily available for immediate release. In the graph, Kr/Gel@Flu exhibit sustained release after the initial burst phase. This could be beneficial for applications requiring a more controlled and prolonged release of the drug. Encapsulation efficiency (EE) is a measure of the percentage of the initial amount of drug that is successfully loaded into the carrier system. The EE parameter for Flu at Kr/Gel@Flu was 98.42%. A EE indicates that a larger proportion of the initial drug amount is successfully loaded into the carrier, resulting in a more efficient encapsulation process. Alginate-based hydrogels can be designed to provide controlled release of the incorporated antimicrobial agent, which would ensure sustained antibacterial action. According to these results, it can be supposed that there is a great interaction between the Flu and formulated samples. The sponge-like hydrogel formulation, with its porous structure and controlled release of active components, can support wound healing and tissue regeneration in the vulvovaginal area20,55.
Antifungal activity
The antifungal activity of the produced hydrogel samples was measured using a colony count and compared with the control. The antifungal results of the Kr/Gel, and Kr/Gel@Flu are presented in Fig. 7. The Kr/Gel@Flu showed antifungal activity through a combined effect of components. Flu, as a well-established antifungal agent, which is released from the hydrogel samples under regulated conditions and inhibits the synthesis of a vital fungal cell membrane component, is the main cause of the strong antifungal effects against different species of Candida. The Kr may disrupt fungal cell membranes, while Gel acts as a carrier for sustained release and targeted delivery of these components, making the fungus more susceptible and ultimately leading to cell death. This multi-pronged attack by the hydrogel’s ingredients could potentially overcome fungal resistance and enhance the fungicidal activity of the formulations. Variability in the count reduction among Candida species may be attributed to their differing sensitivities to the synthesized components. The controlled drug release ensures a consistent Flu concentration at the wound site, effectively inhibiting fungal growth and reducing the risk of recurrence. Combining these biopolymers creates a biomimetic scaffold that supports cell growth, promotes wound healing, and delivers targeted agents for infection control. The sponge-like hydrogel formulation containing Flu exhibits potent antimicrobial activity against various Candida species. The Flu component inhibits the synthesis of vital fungal cell membrane components, while the Kr, and Gel components can disrupt fungal cell membranes and interfere with fungal metabolism. The formulated hydrogels demonstrat significant antifungal activity against clinically relevant isolate. This multi-pronged antimicrobial approach can help overcome fungal resistance and enhance the fungicidal activity. Khullar and coworkers reported that topical mefenamic emulgels formulated using clove oil demonstrated superior drug permeation, anti-inflammatory and analgesic activities56.
Antifungal properties of sponge-like hydrogel samples against the tested standard Candida cells. The residual viable cells were monitored as the numbers of CFU on SDA plates after treatment. The data are exhibited as mean ± SD (n = 3). Error bars denote standard error from mean cell proliferation as determined by repeated experiments.
Antibiofilm activity
Biofilms are comprised of microorganisms within a protective matrix, and they have the tendency to be found on chronic wounds, slowing down the process of healing and causing infection57. The antibiofilm activity of hydrogels was discovered during the study to be dose dependent. The control sample (Kr/Gel) showed moderate activity with biofilm inhibition between 20% and 45%. Addition of Flu (Kr/Gel@Flu) significantly enhanced this effect, which exhibited an outstanding reduction in biofilm production of 80–95%. Flu loaded sample was evaluated for its anti-biofilm effect against Candida species involved in fungal infections. The findings confirmed a significant biofilm growth inhibition compared to control groups, illustrating the formulated hydrogel is able to inhibit the growth of biofilms (Fig. 8). This effectiveness is attributed to several factors including Flu antifungal action, sustained release of the drug by the hydrogel, and the hydrogel matrix to facilitate drug diffusion and reaction with microbes7. Flu is a well-known antifungal medication that works by disrupting fungal cell membranes. It achieves this by targeting ergosterol, an important component in the fungal cell wall1. This medication works through the inhibition of the specific fungal enzyme lanosterol 14α-demethylase. This inhibits the conversion of lanosterol into ergosterol. By blocking this step, Flu disrupts membrane integrity and ultimately leads to fungal cell death. This effect is synergistic to controlled drug release, which increases its effectiveness against biofilms. Several studies have described that the vaginal infection of Candida species is most often associated with biofilm formation on the host’s vaginal epithelium58. Here, the antibiofilm activity of Kr/Gel@Flu can be extremely effective in the local prevention and disruption of Candida biofilms to enhance the treatment and management of vulvovaginal candidiasis.
This platform holds promise for combating vaginal biofilms, minimizing systemic side effects. The Kr/Gel@Flu antibiofilm, and antimicrobial, properties make it a promising candidate for vulvovaginal applications, particularly in managing recurrent and persistent vaginal infections.
MTT assay
To evaluate the biocompatibility of the developed sponge-like hydrogel for vaginal drug delivery applications, it is crucial to assess cell viability. For the direct contact test, evaluation of the biocompatibility of Kr/Gel, and Kr/Gel@Flu to HeLa and CRL-1658 cell lines was performed using the MTT assay at different immersion periods (24 h, 48 h, and 72 h). The cell viability data (Fig. 9) indicate no significant difference in cytotoxicity of Kr/Gel and Kr/Gel@Flu and to tested cell lines (p value > 0.05). These findings highlight the biocompatibility of the formulated sponge-like hydrogel, which exhibits significant antifungal properties (Fig. 7). The cytocompatibility of the formulations make them suitable for various therapeutic applications, including vulvovaginal drug delivery systems and wound healing treatments.
Hemocompatibility assessment
Blood is typically the first tissue that comes into contact with wound dressing materials, making it essential to evaluate the blood compatibility of the applied materials in tissue engineering. In order to investigate the blood compatibility of the produced formulation, hemolysis test was performed. As shown in the Fig. 10, the hemolytic amount (%) of the Kr/Gel@Flu sponge-like hydrogel was 1.08, 3.44, and 4.66%, after 2, 6, and 12 h, respectively. These findings indicated appropriate blood compatibility.
Conclusion
In this study, a sponge-like hydrogel was developed as a promising delivery system for the treatment of vulvovaginal candidiasis. These formulations exhibited a porous, fibrous structure with suitable moisture content, wound fluid uptake ability, and low solubility in simulated wound fluid. These properties indicate its potential for maintaining a moist wound environment and providing controlled drug release. In vitro evaluations demonstrated significant antifungal and antibiofilm activity of the Kr/Gel@Flu against Candida spp., alongside cytocompatibility, highlighting its potential for combating biofilm-associated chronic infections. However, this study has limitations. First, the in vitro models, while informative, cannot fully replicate the in vivo microenvironment of vulvovaginal infections, including host immune responses and mucosal interactions. Second, the sample size in antibiofilm and cytotoxicity assays was limited; future work should include larger replicates to strengthen statistical power. To address these gaps, we propose (1) in vivo validation in a murine vulvovaginal candidiasis model to assess efficacy, safety, and pharmacokinetics, and (2) preclinical testing under dynamic conditions (e.g., flow systems mimicking vaginal fluid turnover). These steps are critical to translate this platform toward clinical application.
Materials and methods
Materials
All chemicals and reagents were of analytical grade. The Kr, edible bovine Gel, dimethyl sulfoxide (DMSO), sodium alginate (SA, medium viscosity ~ 3500 cps), glacial acetic acid, Dimethylformamide (DMF), Mueller-Hinton broth (MHB), RPMI-1640, Sabouraud Dextrose Agar (SDA), Sabouraud Dextrose Broth (SDB), and Muller-Hinton agar (MHA) were purchased from Merck Company (Darmstadt, Germany). The Flu, Menadione, XTT, Fetal Bovine Serum (FBS) and DMEM medium were purchased from Sigma-Aldrich Company. Other agents such as calcium chloride, sodium chloride, tris methylamine, Phosphate Buffer Saline (PBS), and Sodium Phosphate Buffer (SPB) were available in the laboratory. Cervical cancerous cell line (HeLa cell line) and normal skin fibroblast (CRL-1658) were obtained from Pasteur Institute of Iran.
Synthesis of the sponge-like hydrogels
To prepare the hydrogels, a specified ratio of Kr (0.3 g) and Gel (0.03 g) was dispersed in distilled water (D.W.). The polymeric mixture was stirred to create a homogeneous solution. Then, Flu (10 mg) was added to the polymeric solution and stirred for 24 h (extended stirring time aids in maximizing the interaction between Flu and the polymer matrix, despite its limited solubility). In the following, to strengthen the sponge-like hydrogels structure, the cross-linking process was performed using SA (3%) for 24 h. Different ratios that were initially ineffective were tested. However, subsequent experiments, along with our previous report20, revealed that these ratios were effective in terms of both chemical and microbial properties. According to our previous report20, a ratio of 2:1 was selected for SA and polymeric solution, respectively. Then, the homogeneous polymeric solution was transferred to Falcon tubes. To solidify the hydrogels and impart their’s unique properties, the cryogelation process was carried out. This process involved freezing the polymeric solution-filled tubes at a temperature of -80°C and allowing them to remain at this temperature for a sufficient period. After the cryogelation process was completed, we allowed the frozen hydrogels to thaw at room temperature to ensure that they returned to their’s intended state. Following the freeze-thawing step (n = 3), the hydrogels were subjected to freeze-drying at − 48 °C for two days. Finally, the prepared hydrogels were kept in a desiccator (humidity of 70%) to maintain their rigid structure. Each formulation including, Kr-Gel, and Kr-Gel@Flu were extensively analyzed to assess its physicochemical properties and potential for enhanced drug delivery applications. The sponge-like hydrogel preparation is illustrated in Fig. 11.
Cryogelation involves the formation of a gel matrix at subzero temperatures, where ice crystals form within the polymeric solution. In the present formulation, Kr and Gel serve as the primary structural components. When the polymeric solution is frozen at – 80 °C, water molecules crystallize, leading to a concentration of the polymer chains in the remaining liquid phase. This process facilitates physical entanglement and hydrogen bonding between Kr and Gel molecules, which is critical for establishing a stable gel network. SA acts as a cross-linking agent in our formulation. Upon thawing, SA interacts with the Kr and Gel through ionic interactions and hydrogen bonding, further enhancing the structural integrity of the hydrogel.
Chemical and structural characterization
Fourier-transform infrared spectroscopy (FTIR) was conducted in attenuated total reflectance (FTIR-ATR) transmittance mode using (Bruker Tensor II instrument, Germany). Spectra were obtained at a resolution of 4 cm−1 with 32 scans in the range of 4000–400 cm−1. This technique verified the chemical interactions between the components and confirmed the successful formulation of the sponge-like hydrogels. The surface characteristics of the formulated hydrogel samples were documented using a TESCAN-Vega3 scanning electron microscope (Czech Republic). Before SEM analysis, the samples were coated with a thin layer of gold through sputter coating for 20 min. Energy dispersive X-ray analysis (EDX) analysis was used to identify the elemental composition of the materials present in the formulated sponge-like hydrogels.
Compression mechanical properties
Flexural strength testing
The Kr/Gel, and Kr/Gel@Flu sponge-like hydrogels were tested on a Universal Material-Testing Machine (Zwick/Roell Z020, Germany) to measure their Young’s modulus and compression strength. The fully swollen sponge-like hydrogel columns, approximately 40 mm in length and 12 mm in diameter were compressed at room temperature. The compression speed between the two parallel plates was set at 10 mm/min.
Data analysis
From the repeated measurements, the standard deviations in the modulus values were less than 5%. The compression strength was calculated by dividing the maximum force (Fmax) of the samples by their cross-sectional area. Each experiment was carried out in duplicate to ensure the reliability of the results20.
Water barrier properties
Moisture content determination
Obtained hydrogel disks were weighted first (M1), then they were incubated at a relative humidity of 20% and a temperature of 37 °C. Each disk was repeatedly weighed at specified time intervals using an electronic analytical balance until a constant weight (M2) had been achieved. Each experiment was performed in triplicate to ensure the reliability of the results59. The moisture content (%) was calculated using the following Eq. (1):
Porosity
To analyze the porosity of formulated samples, the mass of a dry sample (M1) was weighed using a balance, then immersed in the simulated wound fluid (SWF) medium, and allowed to fully swell, which took approximately 210 min. This SWF fluid comprised 0.02 M calcium chloride, 0.4 M sodium chloride, 0.08 M Tris methylamine, and 2% W/V BSA in D.W., with the pH adjusted to 7.560. Then, the swollen sample was removed and its mass was recorded (M2). The porosity was calculated using the formula, where ρs and ρd are the density of the fully swollen and dry samples, respectively, which are achieved by dividing M1 and M2 by their volumes. Finally, the porosity (P %) of the open pores in the synthesized sponge-like hydrogels was calculated by the formula given in Eq. (2):
Water vapor transmission rate
This test was measured based on ASTM E96 (37 °C, humidity: 87%). The formulated samples were cut into circular shapes and affixed to the mouths of individual bottles (13.5 mm diameter). Each bottle was filled with 10 mL of D.W. The bottles were tightly sealed with parafilm tapes to prevent water loss and weighed before incubation. The bottles were then placed in a desiccator containing a saturated solution of sodium chloride, maintained at a temperature of 37 ℃. The bottles were weighed after 24 h, and WVTR (g/m2/day) was calculated by the Eq. (3):
Where Wi (g) and Wf (g) are defined as the initial and final bottles’ weights, respectively; and A (m2) is the exposure surface of the bottle mouth.
Wound fluid uptake
The capacity for fluid absorption in the formulated samples was determined using simulated wound fluid (SWF) as the medium60. Sponge-like hydrogel pieces with dimensions of 10 × 30 mm were immersed in the SWF. At predetermined time intervals, the hydrated and expanded hydrogel samples were gently dabbed with filter paper to remove any excess SWF on their surfaces and then weighed. The variation in mass for each sample was recorded. To calculate the swelling index (Is %), the following formula (4) was used.
Where Ws and Wd are the weights of the swollen and dry samples, respectively.
In vitro release of flu from sponge-like hydrogels
The release behavior was determined using SWF as a medium60. To study the release behavior of Flu from Kr/Gel@Flu, the samples were prepared in circular disks (12 mm diameter) and weighed (n = 2). Each disk was placed in a glass tube containing 5 mL of SWF and stirred at room temperature. At various time intervals, 1 mL of each sample was replaced with a fresh SWF. After centrifugation of each sample (10,000 rpm, 3 min), the supernatant was filtered and analyzed using an Agilent Cary Series 100 UV/VIS Spectrophotometer at a wavelength of 260 nm.
The encapsulation efficiency (EE) parameter and cumulative drug release were calculated from the following Eqs. (5) and (6)9,61:
Where, MFlu and MTotal are related to the amount of Flu released at time t and total Flu loaded into the hydrogel, respectively.
Biological properties
Antifungal activity of the formulated sponge-like hydrogels
Tested microorganisms In this research, 6 American Type Culture Collection (ATCC) and CentraalBureau voor Schimmel cultures (CBS) strains of yeast fungi, including Candida albicans (CBS562), C. dubliniensis (CBS 8501), C. tropicalis (ATCC 750), C. glabrata (ATCC 90030), C. parapsilosis (ATCC 4344), C. krusei (ATCC 6258), and one clinical isolates of C. albicans were also examined in this study. The antifungal activities of the produced hydrogels were assessed against standard strains of Candida species, according to the standard AATCC 100 test method62. In brief, the produced hydrogels including, Kr/Gel@Flu, and Kr/Gel were cut into circular shapes (13.5 mm in diameter) and sterilized under UV light (30 min). After that, 1000 µl of Candida species suspension at cell densities of 0.5 McFarland was added into Falcon tubes containing the hydrogel samples incubated (32 °C, 24 h). After that, 10 ml of PBS was added to the Falcon tubes and shaken (60 s). Following this, 10 µl of the solution was cultured on SDA medium and incubated at 32 °C for 24 h. Pure Flu was also used for control (10 mg/mL). This process was repeated in triplicate. The viable colonies were counted, and the reduction percentage of Candida species was determined using the following Eq. (7):
Where A is the number of Candida species that grew on the agar plates for untreated control, and B is the number of Candida species recovered from the inoculated formulated samples after 24 h20.
Quantitative investigation of the antibiofilm activity
To conduct a quantitative investigation of the antibiofilm activity of the hydrogel samples (Kr/Gel@Flu, and Kr/Gel), the XTT reduction assay was used. The specified standard Candida species were initially cultured on SDA plates. Following a 24 h incubation period, a single loopful of colonies was transferred into 20 mL of SDB and incubated at 32 °C with continuous agitation (100 rounds/min) for 24 h. Subsequently, the Candida species were washed twice with sterile PBS and then re-suspended in RPMI 1640 medium. The cell concentrations were adjusted to 1.0 × 106 cells/mL, measured at a wavelength of 530 nm. Then, the mentioned produced hydrogel samples were cut into circular shapes (6 mm in diameter, sterilized under UV light for 30 min), inserted into the 48-well cell culture plate, and incubated for 24 h to allow interaction. Following the removal of sample residues and gentle washing of the biofilms with PBS to remove non-adherent cells, apply the XTT-menadione solution, ensuring complete coverage of the biofilms. Incubate the plates in the dark at 32 °C for 4 h, allowing sufficient time for color development from the formazan product, which is measured using a spectrophotometer at 490 nm. Furthermore, media containing Candida strains but lacking samples were considered positive controls, and media alone, without cultures and sponge-like hydrogels, were considered negative controls63. This assay was repeated in triplicate. The Candida biofilm inhibition percentage was calculated using Eq. (8)42,59.
Cytotoxicity assessment
The cell viability for biocompatibility evaluation was performed using the HeLa and CRL-1658 cell lines by MTT assay. The sponge-like hydrogels were placed on sterile 48-well cell culture plates and exposed to ultraviolet (UV) light for 45 min to ensure their suitability for use in the cell culture experiments. The cells were cultured in high-glucose DMEM medium supplemented with 10% FBS and 1% (v/v) penicillin-streptomycin, in a humidified incubator with 5% CO2. In brief, a cell density of 1.0 × 104 cells per well was seeded in a 48-well cell culture plate and incubated for 16 h. After incubation, the formulated hydrogel samples were cut into circular shapes (6 mm in diameter), introduced into the fresh cell culture medium and incubated for 24, 48, and 72 h. Then, fresh MTT solution (0.50 mg/mL) was added to each well and incubated (4 h). To measure cell viability, the culture media was removed, and 100 µL of DMSO (100%) was added for dissolving the formazan crystals. The absorbance of the samples was measured by a BMG SpectroNano plate reader (570 and 630 nm). Cell viability was calculated as a percentage using the formula (9):
Where the A is referred to the absorbance20,64,65.
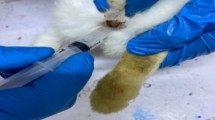
Hemocompatibility assessment
Hemolysis test was done based on ASTM F 756-00 by some modifications20,59. First, 5 mL of venous blood was collected from a healthy volunteer, stabilized with sodium citrate (3.8%), centrifuged (8 min at 2000 rpm), then obtained pellet was washed with PBS (3 times, centrifuged 5 min at 1500 rpm). The sponge-like hydrogel samples (Kr/Gel@Flu, and Kr/Gel), were cut into 2 cm2 square-shaped, and kept in 3.5 mL of PBS; after incubating at 37 °C for 24 h, then 500 µL of blood (diluted with PBS in 1:9 ratio) was added to each sample and kept at 37 °C for 2, 6 and 12 h. Positive and negative controls were prepared by the same procedure by adding the blood to 3.5 mL of water and PBS, respectively. After incubation, each fluid was transferred into a suitable tube and centrifuged for 15 min at 1000 rpm. The hemoglobin released in the supernatant was read by the BMG Spectro Nano plate reader at a wavelength of 545 nm. The percentage of hemolysis was calculated according to the formula (10):
Statistical analyses
The analysis of the obtained data was performed using GraphPad Prism. The results are reported as mean ± standard deviation (SD). The One-way ANOVA method and t test were employed to compare the effects of the formulations against different Candida strains. Statistical differences were considered significant when p value < 0.05 which provided a 95% confidence interval for the results. All tests were carried out in triplicate.
Data availability
The data used to support the findings of this study were supplied by Vice-Chancellor for Research of Shiraz University of Medical Sciences under license. Requests for data access should be made to Zahra Zareshahrabadi, zare_shahrabadi@sums.ac.ir.
Change history
24 August 2025
The original online version of this Article was revised: In the original version of this Article the Funding section was incomplete. The Funding section now reads: “This study was extracted from the thesis of Ali Radmanesh [Grant No. 29853] and financially supported by the Vice-Chancellor for Research of Shiraz University of Medical Sciences and Iran National Science Foundation (INSF) [grant number: 4031162]”.
References
Farr, A. et al. Guideline: vulvovaginal candidosis (AWMF 015/072, level S2k). Mycoses 64 (6), 583–602 (2021).
Rodríguez-Cerdeira, C. et al. Pathogenesis and clinical relevance of Candida biofilms in vulvovaginal candidiasis. Front. Microbiol. 11, 544480 (2020).
Bergin, S. et al. Analysis of clinical Candida parapsilosis isolates reveals copy number variation in key fluconazole resistance genes. Antimicrob. Agents Chemother. 68 (6), e01619–e01623 (2024).
Arastehfar, A. et al. Low level of antifungal resistance in Iranian isolates of Candida glabrata recovered from blood samples in a multicenter study from 2015 to 2018 and potential prognostic values of genotyping and sequencing of PDR1. Antimicrob. Agents Chemother. 63 (7), 02503–02518. https://doi.org/10.1128/aac (2019).
Pfaller, M. & Diekema, D. Progress in antifungal susceptibility testing of Candida spp. By use of clinical and laboratory standards Institute broth microdilution methods, 2010 to 2012. J. Clin. Microbiol. 50 (9), 2846–2856 (2012).
Mollazadeh-Narestan, Z. et al. Comparing the effect of probiotic and fluconazole on treatment and recurrence of vulvovaginal candidiasis: a triple-blinded randomized controlled trial. Probiotics Antimicrob. Proteins. 15 (5), 1436–1446 (2023).
Berkow, E. L. & Lockhart, S. R. Fluconazole resistance in Candida species: a current perspective. Infect. Drug Resist. 10, 237–245 (2017).
Wang, Y. et al. A mechanism study on the synergistic effects of rifapentine and fluconazole against fluconazole-resistant Candida albicans in vitro. Heliyon 10(6), e27346. https://doi.org/10.1016/j.heliyon.2024.e27346 (2024).
El Rabey, H. A. et al. Augmented control of drug-resistant Candida spp. via fluconazole loading into fungal Chitosan nanoparticles. Int. J. Biol. Macromol. 141, 511–516 (2019).
Ogedengbe, O. T. & Kolawole, O. M. Formulation and evaluation of fluconazole emulgels for potential treatment of vaginal candidiasis. Heliyon, 10(6). (2024).
Conte, J. et al. Development of biopolymer films loaded with fluconazole and thymol for resistant vaginal candidiasis. Int. J. Biol. Macromol. 275, 133356 (2024).
Phillips, N. A. et al. Topical treatment of recurrent vulvovaginal candidiasis: an expert consensus. Womens Health Rep. 3 (1), 38–42 (2022).
Selvaraj, S. et al. Cerium oxide nanoparticles and their polymeric composites: advancements in biomedical applications. J. Inorg. Organomet. Polym. Mater. 1–27. (2024).
Savina, I. N., Zoughaib, M. & Yergeshov, A. A. Design and assessment of biodegradable macroporous cryogels as advanced tissue engineering and drug carrying materials. Gels 7 (3), 79 (2021).
Dubashynskaya, N. V. et al. Carrageenan/chitin nanowhiskers cryogels for vaginal delivery of metronidazole. Polymers 15 (10), 2362 (2023).
Selvaraj, S. et al. A state-of-the-art review on plant-derived cellulose-based green hydrogels and their multifunctional role in advanced biomedical applications. Int. J. Biol. Macromol. 130991 (2024).
Pandey, M. et al. Promising drug delivery approaches to treat microbial infections in the vagina: a recent update. Polymers 13 (1), 26 (2020).
Selvaraj, S. et al. Biomedical potential of hydrogels: a multifaceted approach to innovative medication delivery. Emerg. Mater. 7 (3), 721–763 (2024).
Al-Musawi, M. H. et al. Localized delivery of healing stimulator medicines for enhanced wound treatment. J. Drug Deliv. Sci. Technol. 106212 (2024).
Hashempur, M. H. et al. Enrichment of creatine-gelatin cryogel with Zataria multiflora essential oil and titanium dioxide nanoparticles as a potential wound dressing. Mater. Today Chem. 38, 102069 (2024).
Selvaraj, S. et al. Multifunctional biomedical applications of MXene-based hydrogels: a review. Inorg. Chem. Commun. 164, 112457 (2024).
Memic, A. et al. Latest advances in cryogel technology for biomedical applications. Adv. Ther. 2 (4), 1800114 (2019).
Biswas, M. C. et al. Recent advancement of biopolymers and their potential biomedical applications. J. Polym. Environ. 1–24. (2022).
Mitura, S., Sionkowska, A. & Jaiswal, A. Biopolymers for hydrogels in cosmetics. J. Mater. Sci. Mater. Med. 31, 1–14 (2020).
Selvaraj, S. et al. Unveiling the role of nanogels as an innovative drug delivery in hepatocellular carcinoma therapy: an updated review. BioNanoScience 15 (3), 1–28 (2025).
Feroz, S. et al. Keratin-Based materials for biomedical applications. Bioact. Mater. 5 (3), 496–509 (2020).
Al-Sudani, B. T. et al. Vasculo-osteogenic keratin-based nanofibers containing merwinite nanoparticles and sildenafil for bone tissue regeneration. Int. J. Pharm. 667, 124875 (2024).
Straccia, M. C. et al. Crosslinker effects on functional properties of alginate/N-succinylchitosan based hydrogels. Carbohydr. Polym. 108, 321–330 (2014).
Zhou, Q. et al. Influence of different divalent ions cross-linking sodium alginate-polyacrylamide hydrogels on antibacterial properties and wound healing. Carbohydr. Polym. 197, 292–304 (2018).
Goh, C. H., Heng, P. W. S. & Chan, L. W. Cross-linker and non-gelling Na + effects on multi-functional alginate dressings. Carbohydr. Polym. 87 (2), 1796–1802 (2012).
Ndlovu, S. P. et al. Gelatin-based hybrid scaffolds: promising wound dressings. Polymers 13 (17), 2959 (2021).
Al-Sudani, B. T. et al. Highly porous 3D printed scaffold incorporated with graphene oxide-Merwinite and coated with IGF1 loaded nanofibers for calvarial defect repair. J. Polym. Environ. 32 (10), 5330–5343 (2024).
Husain, M., Gupta, A. & Alashwal, B. Development of keratin based hydrogels for biomedical applications. in: IOP Conference Series: Materials Science and Engineering. IOP Publishing. (2019).
Bukhari, S. M. H. et al. Synthesis and characterization of chemically cross-linked acrylic acid/gelatin hydrogels: effect of pH and composition on swelling and drug release. Int. J. Polym. Sci. 2015, p187961 (2015).
Monfared, A. A. et al. Design and antifungal activity of fluconazole and nystatin loaded onto silica mesoporous. Pharm. Chem. J. 57, 965–974 (2023).
Daemi, H. & Barikani, M. Synthesis and characterization of calcium alginate nanoparticles, sodium homopolymannuronate salt and its calcium nanoparticles. Sci. Iran.. 19 (6), 2023–2028 (2012).
Bölgen, N. et al. Development of Hypericum perforatum oil incorporated antimicrobial and antioxidant Chitosan cryogel as a wound dressing material. Int. J. Biol. Macromol. 161, 1581–1590 (2020).
Kakkar, P., Madhan, B. & Shanmugam, G. Extraction and characterization of keratin from bovine hoof: a potential material for biomedical applications. SpringerPlus 3 (1), 596 (2014).
Cyr, T. D. et al. Spectral characterization of fluconazole. J. Pharm. Biomed. Anal. 14, 247–255 (1996).
Kumar, L. et al. Preparation and characterisation of fluconazole vaginal films for the treatment of vaginal candidiasis. Indian J. Pharm. Sci. 75 (5), 585–590 (2013).
Asadi Shahi, S. et al. A new formulation of graphene oxide/fluconazole compound as a promising agent against Candida albicans. Prog. Biomater. 8 (1), 43–50 (2019).
Torabiardekani, N. et al. Encapsulation of Zataria multiflora essential oil in Polyvinyl alcohol/chitosan/gelatin thermo-responsive hydrogel: synthesis, physico-chemical properties, and biological investigations. Int. J. Biol. Macromol. 243, 125073 (2023).
Kamarudin, N. B. et al. Statistical investigation of extraction parameters of keratin from chicken feather using Design-Expert. 3 Biotech, 7(2): p. 127. (2017).
Singh, B., Sharma, S. & Dhiman, A. Design of antibiotic containing hydrogel wound dressings: biomedical properties and histological study of wound healing. Int. J. Pharm. 457 (1), 82–91 (2013).
Dinu, M. V. et al. Physically cross-linked chitosan/dextrin cryogels entrapping Thymus vulgaris essential oil with enhanced mechanical, antioxidant and antifungal properties. Int. J. Biol. Macromol. 184, 898–908 (2021).
Gun’ko, V. M., Savina, I. N. & Mikhalovsky, S. V. Cryogels: morphological, structural and adsorption characterisation. Adv. Colloid Interface Sci. 187–188, 1–46. (2013).
Jaidev, L. & Chatterjee, K. Surface functionalization of 3D printed polymer scaffolds to augment stem cell response. Mater. Des. 161, 44–54 (2019).
Ju, J. et al. Fabrication of bimodal open-porous Poly (butylene succinate)/cellulose nanocrystals composite scaffolds for tissue engineering application. Int. J. Biol. Macromol. 147, 1164–1173 (2020).
Ramanathan, G. et al. Design and characterization of 3D hybrid collagen matrixes as a dermal substitute in skin tissue engineering. Mater. Sci. Eng. C. 72, 359–370 (2017).
Sung, J. H. et al. Gel characterisation and in vivo evaluation of minocycline-loaded wound dressing with enhanced wound healing using Polyvinyl alcohol and Chitosan. Int. J. Pharm. 392 (1–2), 232–240 (2010).
Sobhanian, P. et al. Development of nanofibrous collagen-grafted Poly (vinyl alcohol)/gelatin/alginate scaffolds as potential skin substitute. Int. J. Biol. Macromol. 130, 977–987 (2019).
Letha, S. S. et al. Electrospun polyurethane-gelatin artificial skin scaffold for wound healing. J. Text. Inst. 113 (3), 378–387 (2022).
Kianfar, F., Ayensu, I. & Boateng, J. S. Development and physico-mechanical characterization of Carrageenan and poloxamer-based lyophilized matrix as a potential buccal drug delivery system. Drug Dev. Ind. Pharm. 40 (3), 361–369 (2014).
Denning, D. W. et al. Global burden of recurrent vulvovaginal candidiasis: a systematic review. Lancet. Infect. Dis. 18 (11), e339–e347 (2018).
Selvaraj, S. et al. Role of degrading hydrogels in hepatocellular carcinoma drug delivery applications: a review. J. Drug Deliv. Sci. Technol. 105628 (2024).
Khullar, R. et al. Formulation and evaluation of mefenamic acid emulgel for topical delivery. Saudi Pharm. J. 20 (1), 63–67 (2012).
Omar, A. et al. Microbial biofilms and chronic wounds. Microorganisms 5 (1), 9 (2017).
Hussain, D. A. & Hussain, M. M. Nigella sativa (black seed) is an effective herbal remedy for every disease except death-a prophetic statement which modern scientists confirm unanimously: a review. Adv. Med. Plant. Res. 4 (2), 27–57 (2016).
Karami, F. et al. Chitosan-based emulgel and xerogel film containing Thymus pubescens essential oil as a potential wound dressing. Carbohydr. Polym. 318, 121156 (2023).
Rezvanian, M. et al. Optimization, characterization, and in vitro assessment of alginate-pectin ionic cross-linked hydrogel film for wound dressing applications. Int. J. Biol. Macromol. 97, 131–140 (2017).
Damiri, F. et al. Synthesis and characterization of lyophilized Chitosan-Based hydrogels Cross-Linked with benzaldehyde for controlled drug release. J. Chem. 2020 (1), 8747639 (2020).
Barzegar, S. et al. Core-shell chitosan/PVA-based nanofibrous scaffolds loaded with Satureja mutica or Oliveria decumbens essential oils as enhanced antimicrobial wound dressing. Int. J. Pharm. 597, 120288 (2021).
Hejazi, M. et al. Characterization and physical and biological properties of tissue conditioner incorporated with Carum copticum L. BioMed Res. Int. 2021 (2021).
Zareshahrabadi, Z. et al. Magnetic Chitosan nanoparticles loaded with amphotericin B: synthesis, properties and potentiation of antifungal activity against common human pathogenic fungal strains. Int. J. Biol. Macromol. 222, 1619–1631 (2022).
Su, J. et al. Hydrogel preparation methods and biomaterials for wound dressing. Life 11 (10), 1016 (2021).
Funding
This study was extracted from the thesis of Ali Radmanesh [Grant No. 29853] and financially supported by the Vice-Chancellor for Research of Shiraz University of Medical Sciences and Iran National Science Foundation (INSF) [grant number: 4031162].
Author information
Authors and Affiliations
Contributions
M.H. H.: Investigation, Methodology, Visualisation, Writing - Review & Editing. A. R.: Methodology & Investigation. F.K.: Formal analysis, Methodology, Writing - Review & Editing. K. Z., & N. A.: Investigation & Writing - Review & Editing. S. Sh.: Methodology & Validation. Z.ZSH: Conceptualisation, Software, Validation, Formal analysis, Data Curation, Writing Original Draft, Writing- Review & Editing, Resources & Project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hashempur, M.H., Radmanesh, A., Karami, F. et al. Fabrication of a sponge-like protein based hydrogel incorporating fluconazole against Candida species as a potential treatment for vulvovaginal candidiasis infection. Sci Rep 15, 24364 (2025). https://doi.org/10.1038/s41598-025-09457-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09457-2