Abstract
The study aimed to determine the relationship between personality traits, orofacial pain (OFP), and headache. Eligible patients underwent one-night videopolysomnography and completed a series of validated questionnaires assessing sleep quality (ISS- Insomnia Severity Scale, PSQI- Pittsburgh Sleep Quality Index, ESS- Epworth Sleepiness Scale), pain intensity (McGill Pain questionnaire, GCPS- Graded Chronic Pain Scale, HIT-6- Headache Impact Test-6, MIDAS- Migraine Disability Assessment, TMD pain screener- Temporomandibular Disorder pain screener), psychoemotional state (KPS- Sense of Stress Questionnaire, PHQ-9 – Patient Health Questionnaire-9, BDI- Beck Depression Inventory, BAI- Beck Anxiety Index, PSS-10- Perceived Stress Scale-10, GAD-7- Generalized Anxiety Disorder-7), personality traits (IPIP-BFM-20 -International Personality Item Pool- Big Five Markers- 20). Patients who exhibited nervousness and hypersensitivity reported higher perceived pain and greater negative impacts on work and daily activities (p = 0,000). Furthermore, a statistically significant relationship was found between subjective sleep quality and emotional stability scales (p = 0,001 for PSQI, p = 0,000 for ISI, p = 0,001 for ESS). However, no such relationship was observed for objective sleep quality, as measured by polysomnography (p > 0,05). The correlation between the emotional stability scale and each of the questionnaires used to examine anxiety, depression, and stress was very strong and corresponded to p = 0.000.
Clinical Trial: Relationship Between Selected Parameters and Bruxism www.ClinicalTrials.gov, identifier NCT04214561.
Similar content being viewed by others
Introduction
Following the International Association for the Study of Pain (IASP) “orofacial pain (OFP) is a frequent form of pain perceived in the face and/or oral cavity. It may be caused by diseases or disorders of regional structures, nervous system dysfunction, or through referral from distant sources”1. An essential aspect of OFP is its relationship with important structures and functions, including aesthetics, psychosocial status, speech, eating, and breathing2. The etiology of OFP can be odontogenic or non-odontogenic. In the classification of OFP, we will distinguish, among others, such entities as: orofacial pain attributed to disorders of dentoalveolar and anatomically related structures, myofascial orofacial pain, temporomandibular joint (TMJ) pain, orofacial pain attributed to lesion or disease of the cranial nerves, orofacial pains resembling presentations of primary headaches, idiopathic orofacial pain and psychosocial assessment of patients with orofacial pain3.
The second most common cause of orofacial pain is TMD pain2. And it is pain that is the most common reason why patients struggling with TMD seek help. Pain is an essential part of the human experience, serving as both a physical and emotional signal of bodily harm. It can strongly motivate human behavior3. Pain can be classified as either acute or chronic. Chronic OFP, according to the International Classification of Orofacial Pain, is pain that has persisted for more than 3 months and recurs in at least 10 episodes, or remains unremitting3. Chronic headache (HA) is defined as pain occurring on more than 15 days per month for at least the past 3 months4.
However, pain is often not the only ailment these patients face. They are frequently accompanied by sleep disorders, sleep and/or awake bruxism, anxiety, chronic stress, and depression2,5,7.
The relationships between the severity of OFP, headaches, and polysomnographic sleep quality parameters were previously analyzed by the authors of this study7. We did not find statistically significant connections between pain and sleep quality in polysomnography studies. In contrast, subjective sleep quality was statistically significantly correlated with the intensity of pain experienced. Moreover, in our previous studies, pain relief was also significantly correlated with depression, anxiety, and perceived stress levels5.
Upon analyzing many available works, we have observed similar conclusions from other authors: the psychoemotional state of the patient is closely related to the level of pain experienced5,8,12, how they cope with it9,11, and the occurrence of other often subjective disorders, such as a deterioration in sleep quality5,13,15.
The question then arises, what may be related to the psychoemotional state of patients suffering from primary headache and orofacial pain? Is it possible to predict, at the diagnostic stage, that the patient may experience disorders such as depression, anxiety, or high stress levels? Can we define factors influencing the symptoms reported by the patient to be more serious, and therapeutic interventions may be less effective? This would suggest that the patient should receive psychotherapeutic support from the very beginning. The analyzed literature confirmed that the patient’s personality may be related to the level of pain experienced and the way they cope with it. We sought to answer whether a patient’s personality can influence the experience of pain or affect the quality of sleep, as measured subjectively by questionnaires and objectively assessed during a polysomnographic examination. Additionally, we examined whether a patient’s personality influences sleep bruxism (SB) and its relationship with anxiety disorders, depression, severe stress, and coping mechanisms.
The aim of our study was to determine whether a specific set of personality traits predisposes individuals with reported OFP to a more severe course and greater intensity of headache and OFP. Additionally, we sought to explore whether these traits influence the co-occurrence of sleep quality disturbances, the intensity of sleep bruxism, a deterioration in well-being, and a decline in mental health within this group.
Materials and methods
Participants
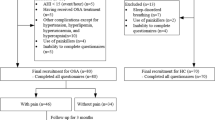
The study group consisted of 114 patients from the Outpatient Clinic for Temporomandibular Disorders at the Wroclaw Medical University, qualified for the study in 11.2019–12.2020. Patients who came to the clinic due to a reported pain localized in the face, masticatory muscles, temporomandibular joint (TMJ), or headaches were examined by a dentist with over than 5 years’ experience in OFP management. A comprehensive clinical examination was conducted according to the International Classification of Orofacial Pain, 1 st edition (ICOP) criteria for orofacial pain3. The study group included adult patients diagnosed with primary headache or orofacial pain.
Primary headaches (pain with absence of an underlying pathologic process, disease, or traumatic injury that occurs in temporal relationship to the onset of pain) include migraine, tension-type headache, and the trigeminal autonomic cephalalgias4.
Orofacial pain including myofascial orofacial pain (pain localized to the masticatory muscles, with or without functional impairment), temporomandibular joint (TMJ) pain (pain localized to the TMJ, occurring at rest or during jaw movement or palpation) and orofacial pain resembling presentations of primary headaches (pain in the orofacial area, resembling 1 of the primary headache types in pain character, duration, and intensity with or without the associated symptoms of these headache types but without concomitant headache)3.
In case of doubts as to the nature of the headache, suspicion by the examining dentist that the headache is not of a primary nature, but may be associated with the absence of an underlying pathological process, disease, or traumatic injury that occurs in temporal relation to the onset of pain, the patient was excluded from the study group and referred for additional neurological consultations. Also, patients with orofacial pain whose pain could not be clearly diagnosed by the examining dentist as myofascial orofacial pain, temporomandibular joint (TMJ) pain or orofacial pain resembling presentations of primary headaches were excluded from the study group.
In addition, all qualified patients were referred for video-polysomnographic (vPSG) examination at the Sleep Laboratory in the Clinical Department of Diabetology, Hypertension, and Internal Diseases at the Wroclaw Medical University.
After a polysomnographic examination, participants were asked to complete several questionnaires related to their psychoemotional state, including validated measures of depression, anxiety, stress, and trauma. They also completed questionnaires assessing sleep quality, pain, and the International Personality Item Pool-Big Five Markers-20 (IPIP-BFM-20). The project was approved by the Ethical Committee of Wroclaw Medical University (KB 175/2024). All study participants were informed of the purpose of the examinations and had their privacy rights upheld. All participants provided written informed consent, they obtained written information about data confidentiality. The study was conducted in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The information regarding clinical trial registration can be found at www.ClinicalTrials.gov (identifier: NCT04214561).
Inclusion criteria
Patients were included for the study if they met the following criteria: age over 18 years, informed consent to participate in the study, presence of orofacial pain including myofascial orofacial pain, temporomandibular joint (TMJ) pain and orofacial pain resembling presentations of primary headaches by the ICOP3 or primary headache according to the International Classification of Headache Disorders, 3rd edition (ICHD-3)4.
Exclusion criteria
The main exclusion criteria were: patients whose pain was related to orofacial pain attributed to disorders of dentoalveolar and anatomically related structures, drug and/or alcohol addiction; use of medications that significantly affect the function of the nervous and muscular systems; neoplasms; severe systemic diseases including genetic disorders, neurological disorders, active inflammation, active malignancy, severe mental disorders, including significant mental disabilities; and refusal to participate in the study. Pregnant or breastfeeding women were also excluded from the study.
Video-polysomnography with sleep bruxism assessment
The patients in the study underwent a one-night video-polysomnographic examination with video recording, conducted in the Sleep Laboratory at Wroclaw Medical University using a Nox A1 device (Nox Medical, Iceland). The recordings took place between 10:00 p.m. and 6:00 a.m., taking into account the patient’s individual preferences and sleep habits. The elements of each polysomnographic examination included electroencephalography, electrocardiography, electrooculography, and electromyography (EMG) from the chin and bilaterally from the masseter muscles, along with motion recording of abdominal and thoracic breathing activity, body position assessment, and audio and video recordings. Additionally, a NONIN WristOx2 3150 pulse oximeter (Nonin Medical, Inc., USA) was used to record oxygen saturation, pulse, and plethysmographic data. All vPSG recordings were scored and analysed in 30-s epochs by a qualified and experienced physician, prof. Helena Martynowicz, in accordance with the AASM Manual for the Scoring of Sleep and Associated Events, Version 2.416,17.
SB was assessed using bilateral masseter EMG and audio–video evaluation during polysomnography. The Bruxism Episode Index (BEI) was scored according to the American Academy of Sleep Medicine (AASM) guidelines16. The BEI measures the number of bruxism episodes per hour of sleep (< 2: irrelevant SB; 2–4: mild/moderate SB; >4: severe SB)16. To measure electromyographic activity, electrodes were placed on the right and left masseter muscles of the study participants. EMG bursts within 3 s were considered part of the same episode. Video assessment allowed for the exclusion of events imitating sleep bruxism in EMG (e.g., coughing, swallowing saliva, or yawning) from the BEI.
Personality traits: the international personality item Pool-Big five Markers-20 (IPIP-BFM-20)
The IPIP-BFM-20 is a shortened version of the 50-item Big Five Markers Questionnaire from Goldberg’s International Personality Item Pool18. The IPIP-BFM-20 measures five traits (Extraversion, Agreeableness, Conscientiousness, Emotional Stability, and Intellect) and consists of 20 items. Respondents rate each statement on a Likert scale ranging from “strongly disagree” to “strongly agree” to indicate how well it describes them. Items are rated on a 1–5 point scale, and each trait is assessed with four items, resulting in scores for each trait ranging from 4 to 20 points. Higher scores indicate higher levels of a given trait19. The reliability of the scales (Cronbach’s alpha) ranged from 0.75 to 0.88, and the accuracy (verified through confirmatory factor analysis and correlation with other measurements of the five personality traits) is satisfactory, making the questionnaire suitable for scientific research19,20. An additional shortened version of the questionnaire ensures a low cost for the study. It reduces the time required to complete it, making the survey less tedious for participants and minimizing the risk of errors from accidental answer selection20,22. The IPIP-BFM-50 and IPIP-BFM-20 questionnaires measure the five personality traits in the traditional lexical Big Five23. A brief description of these traits, as proposed by Strus et al., is provided in Table 120,23.
Psychoemotional state assessment
KPS: sense of stress questionnaire
It measures the structure of stress sensations and consists of 27 statements. The questionnaire allows for the calculation of an overall score for generalized stress levels, as well as three results related to the following dimensions: experiencing emotional tension, intrapsychic stress (resulting from confrontation with oneself), and external stress (resulting from the individual’s confrontation with perceived burdens in the social and external world). The questionnaire also includes a scale for detecting lies24.
PHQ-9: Patient Health Questionnaire-9
The subject rates the answers on a scale from 0 to 3, based on the frequency of a given symptom in the past 2 weeks. The PHQ-9 total score for the nine items ranges from 0 to 27. A score of 10 or more indicates a high risk of a depressive episode, with the risk increasing as the score rises. A score of less than five indicates no depression, 5–9 indicates mild depression, 10–14 indicates moderate depression, 15–19 indicates moderately severe depression, and a score of more than 20 indicates severe depression25.
BDI: Beck Depression Inventory
The subject rates the answers on a scale from 0 to 3, based on the frequency of a given symptom in the past 2 weeks. The PHQ-9 total score for the nine items ranges from 0 to 27. A score of 10 or more indicates a high risk of a depressive episode, with the risk increasing as the score rises. A score of less than five indicates no depression, 5–9 indicates mild depression, 10–14 indicates moderate depression, 15–19 indicates moderately severe depression, and a score of more than 20 indicates severe depression26.
BAI: Beck Anxiety Index
The total score is calculated by summing the 21 items. The total score for all 21 symptoms can range from 0 to 63 points. A score of 0–7 is interpreted as “Minimal” anxiety, 8–15 as “Mild” anxiety, 16–25 as “Moderate” anxiety, and 26–63 as “Severe” anxiety26.
PSS-10: Perceived Stress Scale-10
Scores are obtained by reversing the values of the four positive items (e.g., 0 becomes 4, 1 becomes 3, 2 becomes 2, etc.), and then summing the scores across all 10 items. Items 4, 5, 7, and 8 are the positively worded items. The total score can range from 0 to 40. A score between 0 and 13 is considered low stress, 14–26 indicates moderate stress, and a score between 27 and 40 reflects high perceived stress27.
GAD-7: Generalized Anxiety Disorder-7
The questionnaire consists of seven items, with a total score range of 0 to 21 points. Scores of 5, 10, and 15 are used as cut-off points for mild, moderate, and severe anxiety, respectively28.
Subjective assessment of sleep quality
ISS: Insomnia Severity Scale
The minimum score is 0, and the maximum score is 28. A score of up to 10 is considered within the normal range, while a score of 8–14 indicates subliminal insomnia. A score of 15–21 reflects clinically significant moderate insomnia, and a score of 22–28 indicates severe insomnia29.
PSQI: Pittsburgh Sleep Quality Index
It assesses sleep quality over a 1-month period. The measure consists of 19 individual items, divided into 7 components of sleep quality, which produce a global score ranging from 0 to 21, with lower scores indicating better sleep quality. A total score of 5 is set as the cut-off point for poor sleep quality30.
ESS: Epworth Sleepiness Scale
The ESS is a validated eight-item questionnaire that measures subjective sleepiness. ESS scores range from 0 (unlikely to fall asleep in any situation) to 24 (high chance of falling asleep in all 8 situations). The final ESS score is classified as follows: 1–10 is considered normal, 11–14 indicates mild daytime sleepiness, 15–18 reflects average daytime sleepiness, and scores over 18 indicate severe daytime sleepiness31.
Pain assessment
McGill pain questionnaire
It consists of 78 words that describe the experience of pain. Scores range from 0 (no pain) to 78 (severe pain). Results are considered clinically significant when the total value is > 5. In their study designed to assess the multidimensional nature of the pain experience, Melzack et al. demonstrated that the SF-MPQ is a reliable, valid, and consistent measurement tool. The short-form version (SF-MPQ) is available for use in specific research settings where time to obtain information from patients is limited and when more detailed information than just the intensity of pain is needed32.
GCPS: Graded Chronic Pain Scale
The assessment consists of the Grading Chronic Pain Severity, Disability Score, and Disability Points. The classification is as follows: GRADE 0 indicates no pain in the prior 6 months; GRADE I represents low intensity, with a characteristic pain intensity < 50 and low disability (< 3 Disability Points); GRADE II refers to high intensity, with a characteristic pain intensity > 50 and low disability (< 3 Disability Points); GRADE III is characterized by high disability (3 to 4 Disability Points), moderately limiting, regardless of characteristic pain intensity; and GRADE IV represents high disability (5 to 6 Disability Points), severely limiting, regardless of characteristic pain intensity. In their study, Sharma et al. report that the reliability of the 1-month GCPS is equal to or better than the 6-month version in terms of pain intensity, days of disability, pain interference, CPG, and high-impact pain. The cited study shows that the GCPS is a reliable and valid tool that can effectively assess pain intensity and pain interference33.
HIT-6: Headache Impact Test-6
The total score ranges from 36 to 78. A score of ≤ 49 indicates no or minimal impact of the headache on daily activities, a score of 50–55 indicates a slight impact, a score of 56–59 indicates a significant impact, and a score of ≥ 60 indicates a severe impact of the headache on daily activities. The cited study shows that the HIT-6 is a reliable and valid tool for measuring the impact of headaches on daily life in both episodic and chronic migraine sufferers. In this study, the HIT-6 showed high internal consistency reliability among migraine sufferers, with values ranging from 0.82 to 0.9034.
MIDAS: Migraine Disability Assessment
Scoring is based on the total number of days from questions 1 to 5. Grading is as follows: Grade I (little or no disability) for 0–5 days, Grade II (mild disability) for 6–10 days, Grade III (moderate disability) for 11–20 days, and Grade IV (severe disability) for more than 21 days. In their publication, Stewart et al. demonstrated that the MIDAS score has moderately high test-retest reliability among headache sufferers and correlates with clinical judgment regarding the need for medical care. The MIDAS score is calculated by summing missed work or school days, missed household chores days, missed nonwork activity days, and days at work or school, plus days of household chores, where productivity was reduced by half or more over the past 3 months. The correlation between the MIDAS summary score and an equivalent daily diary score was 0.63. The group’s estimate of the MIDAS score was found to be a valid approximation of a rigorous diary-based measure of disability. The mean and median values for the MIDAS score in a population-based sample of migraine cases were similar to those from equivalent diary measures34.
TMD pain screener: Temporomandibular Disorder pain screener
A score of ≥ 3 on the TMD pain screening test (range 0–7) predicts painful TMD based on the DC/TMD (Diagnostic Criteria for Temporomandibular Disorders) criteria and is therefore considered a positive TMD pain test result. The validity of the TMD pain screener is excellent, with high levels of sensitivity and specificity. The TMD pain screener exhibited excellent validity in correctly identifying participants with pain-related TMD (sensitivity, 99%) and healthy control participants (specificity, 97%). Additionally, the screener showed excellent validity in correctly identifying participants with competing symptom conditions, such as nonpainful TMJ disorder (specificity, 95%) and headache unrelated to TMD (specificity, 96%)35.
Database
Data obtained from the medical history, completed questionnaire, and polysomnography were entered into a database created in Excel (Microsoft Office, USA). The elements of the database were then subjected to statistical analysis.
Statistical analysis
The obtained data were analyzed using the TIBCO Software Inc. (2017), Statistica (data analysis software system), version 13 (http://statistica.io). The nonparametric Tau-Kendall correlation coefficient was used to assess the relationship between the variables. This choice was based on the fact that the variables did not follow a normal distribution. A p-value for the correlation coefficient below 0.05 was considered significant. The sample size prediction (n) was performed using the power.cor function from the genefu package (https://rdrr.io/bioc/genefu/man/power.cor.html). The sample size required for determining the significance of the Kendall correlation, which was used in the statistical analysis, was calculated with an expected correlation coefficient of 0.7 and an anticipated confidence interval width of 0.05. The calculated sample size was 22 persons. Therefore, the 114 patients who participated in the study provided a sufficient sample to detect significant differences and correlations between the examined parameters.
Results
Characteristics of the studied sample
A total of 114 adult patients were included in the study (72 women and 42 men). All the patients were Caucasian, aged 21–71 years (mean age: 37.67).
Influence of the patient’s personality on the perception of pain and its intensity
The distribution of point values achieved by the examined patients, ranging from 4 to 20 for individual personality traits in the IPIP BFM-20 questionnaire, is presented in Fig. 1-5.
We note that 93 participants in the study achieved a high score in the Agreeableness component of the IPIP BFM-20 questionnaire. This indicates that most of the surveyed patients can be described as trusting, tactful, cordial, and willing to cooperate and assist others. However, high scores in Intellect on the IPIP BFM-20 questionnaire were achieved by 84 respondents. These people can be characterized as creative, reflective, and possessing a rich imagination and a wide range of interests. Furthermore, 81 respondents achieved high scores in the Conscientiousness component of the IPIP BFM-20 questionnaire. This suggests that such people can be considered organized, careful, precise, effective in their tasks, as well as systematic and responsible. Scores of 12 or more on the Extraversion scale were achieved by 60 patients surveyed with the questionnaire. This indicates that these people are active, energetic, sociable, talkative, bold, and assertive. An interesting observation arises when analyzing the Emotional Stability scale, as only 38 of the examined patients obtained a score above 12. This suggests they are calm, balanced, and not easily affected by negative emotional states. The remaining respondents achieved relatively low scores on the Emotional Stability scale, which may indicate that the studied group was largely anxious, nervous, prone to mood changes, and inclined to worry. They were also likely hypersensitive, jealous, irritable, and prone to anger and irritation.
Using Kendall’s Tau correlation, the statistical relationship between individual personality traits in the IPIP BFM-20 questionnaire and the level of pain reported by patients in the questionnaire was examined. Statistically significant relationships were found between the Agreeableness scale and the intensity of pain reported in the GCPS questionnaire (Ƭ=0,166; p = 0,012), as well as between the Conscientiousness scale and pain reported in the TMD pain screener questionnaire (Ƭ=0.186; p = 0,012). However, no statistically significant correlation was observed between these scales and pain defined using other questionnaires. The value of the Tau coefficient in both dependencies takes on slightly positive values, indicating a not very strong directly proportional relationship.
Notably, a statistically significant relationship was observed between the Emotional Stability scale and pain across all five questionnaires. Patients displaying a nervous, anxious attitude, with changeable moods, prone to worrying, hypersensitive, irritable, and prone to anger and irritation in all five questionnaires reported increased pain perception and a negative impact on work or daily activities (GCPS (Ƭ=−0,23; p = 0,00), HIT-6 (Ƭ= −0,262; p = 0,00), MIDAS (Ƭ=−0,266; p = 0,00), McGill pain questionnaire (Ƭ=−0,293; p = 0,00), and TMD Pain Screener (Ƭ=−0,244; p = 0,00)). We can see that the correlation strength has higher values for all five questionnaire studies for pain assessment and in each case takes negative values, indicating an inversely proportional relationship. The statistical relationships between personality traits and reported pain are shown in Table 2.
Patient’s personality traits influence the occurrence and intensity of sleep Bruxism
Using Kendall’s Tau correlation for statistical analysis, the relationship between the patient’s personality and the occurrence of bruxism episodes was examined. No statistically significant relationship was found between the severity of bruxism and the Agreeableness, Conscientiousness, or Intellect scales. However, patients with higher values on the Extraversion scale—active, assertive, bold, sociable, and talkative people—were more likely to have a higher BEI index (Ƭ=0,138; p = 0.043). What also seems unusual is the fact that the relationship between the severity of bruxism and the Emotional Stability scale is directly proportional. In other words, patients with high scores on the Emotional Stability scale—those who are calm, balanced, and not easily affected by negative emotional states—were also people with higher BEI values (Ƭ=0,151; p = 0.028). For these dependencies the correlation strength is quite low.
However, when examining this relationship, it is important to consider that the causes of bruxism should be viewed through a multifactorial model36,38. Currently, bruxism is understood to be caused by three main groups of factors. The first group includes biological factors such as neurotransmitters, particularly dopamine, genetic factors, and cortical stimulation39,40. The second group comprises psychological factors, which were addressed in our study. These include sensitivity to stress, individual personality traits, and anxiety states41. The third group consists of exogenous factors such as nicotine, caffeine, alcohol, drugs, and certain medications38. The impact of systemic diseases should not be overlooked either, including thyroid disorders, digestive system disorders, sleep disorders, and circulatory system diseases36,38,42. Therefore, a study that focuses solely on the emotional component influenced by the patient’s personality may not fully capture the true relationship (Table 3).
Influence of the patient’s personality traits on the quality of sleep measured subjectively in questionnaire studies and objectively in a polysomnographic study
During the study, all patients were asked to complete questionnaires assessing their subjective sleep quality. The results obtained from these questionnaires reflected the patients’ opinions on the duration, efficiency, and quality of their sleep, as well as any disorders related to poor sleep quality, such as severe daytime sleepiness.
A comparison of the parameters regarding subjective sleep quality reported by patients and those obtained through polysomnography was the subject of a previous publication7. In this study, we aimed to focus on identifying the relationship between sleep quality and personality traits. Statistical analysis of the relationship between objective sleep quality and personality traits was conducted using parameters from the polysomnographic examination, including TST (total sleep time)—the total time spent asleep in minutes; WASO (wake after sleep onset)—the time spent awake after initially falling asleep; SL (sleep latency)—the time from turning off the light to falling asleep (defined as the first occurrence of NREM stage 2); and SE (sleep efficiency)—TST/TBT×100% (total sleep time/total bedtime).
Using of Kendall’s Tau correlation in the statistical analysis of the relationship between subjective sleep quality and patients’ personality traits showed a statistically significant association with the emotional stability scale. This relationship was inversely proportional; that is, the lower the emotional stability, as measured by the IPIP-BFM questionnaire, the worse the sleep quality. Specifically, in the group of anxious, nervous patients with fluctuating moods, prone to worry, hypersensitivity, jealousy, irritability, and anger, sleep quality, as assessed through subjective questionnaires, was poorer. The strength of correlation measured by the Tau coefficient was moderate for each of the sleep quality questionnaires used in the study (PSQI (Ƭ=−0,0224; p = 0,000); ISI (Ƭ=−0,282; p = 0,000); ESS (Ƭ=−0,230; p = 0,001). The remaining scales—extraversion, agreeableness, conscientiousness, and intellect—did not show any statistically significant correlation with subjective sleep quality (Table 4).
However, when examining the results of polysomnographic studies, we do not observe a relationship between personality traits and the deterioration of sleep quality. The only statistical relationship found was between the intellect scale and sleep latency (Ƭ=0,202; p = 0.003). The relationship is directly proportional, i.e., the more the patient’s personality can be described as intellectually active and cognitively open, creative and retrospective, the longer it takes to fall asleep, from turning off the light to falling asleep. However, statistical analysis did not show any correlation between the intellect scale and other sleep parameters measured in the polysomnographic study. (Table 5).
Influence of the patient’s personality traits on the increase in anxiety, stress levels, and the increase in the risk of depression
Among all personality traits, low emotional stability was the most significant factor predisposed to the occurrence of stress, anxiety, and depression. Interestingly, however, patients with higher intellectual scores were more likely to experience increased anxiety, depression, and higher levels of stress. The individual relationships between personality traits and the levels of stress, anxiety, and the severity of depression are presented in Table 6.
Stress
Kendall’s Tau correlation test showed a statistically significant relationship between personality traits such as conscientiousness, intellect, emotional stability, and stress.
For conscientiousness, patients who described themselves as unsystematic, inconsistent, unconcerned with order and planning, careless, and unreliable exhibited higher stress levels according to the KPS questionnaire. However, this relationship is not very strong because the Tau coefficient value is not high. (Ƭ=−0,164 p = 0.01238). Relationship between the conscientiousness scale and the stress level is not visible in the case of the stress levels measured by the PSS-10 questionnaire (Ƭ=−0,01; p = 0.1278).
In the case of intellect, this relationship was found only in the level of stress measured by the KPS questionnaire (Ƭ=−0,242; p = 0.000), and no such relationship was observed between intellect and stress measured by the PSS-10 questionnaire (Ƭ=−0,123; p = 0.060). The relationship between intellect and the level of stress is inversely proportional, meaning that the more patients described themselves as unintellectual, uninquiring, unimaginative, simple, unsophisticated, unreflective, and uncreative, the higher their stress levels as measured by the KPS questionnaire. However, the correlation strength of this relationship is not high (Ƭ=−0,242).
The relationship between emotional stability and the level of stress, as measured by the Kendall Tau correlation test, is evident for both the KPS (Ƭ=−0,547; p = 0.0000) and PSS-10 (Ƭ=−0,553; p = 0.0000) questionnaires. The Tau coefficient value for both questionnaires used is high, which indicates a strong correlation between low emotional stability and high stress levels. Patients who characterize themselves as anxious, nervous, moody, prone to worry, oversensitive, envious, touchy, and prone to anger and irritation exhibit significantly higher levels of stress compared to patients without these personality traits.
Anxiety
Using the Kendall Tau correlation test, we obtained a statistically significant relationship between the intensity of anxiety, as measured by the GAD-7 questionnaire, and the level of intellect, as measured by the IPIP-BFM-20 questionnaire (Ƭ=−0,135; p = 0.041). However, this relationship was inversely proportional, meaning that the more unintellectual, uninquiring, unimaginative, simple, unsophisticated, unreflective, and uncreative patients described themselves, the greater their tendency to experience increased anxiety, according to the GAD-7 questionnaire. A small value of the Tau coefficient indicates a low strength of correlation between these two variables. There was no statistically significant relationship between intellect and anxiety intensity, as measured by the BAI anxiety scale (Ƭ=−0,101; p = 0.1268).
A strong, statistically significant relationship was found between the level of anxiety intensity and emotional stability, as measured by the IPIP-BFM-20. This relationship is also inversely proportional (negative values in the Kendall Tau correlation coefficient), meaning that the more anxious, nervous, moody, prone to worry and hypersensitivity, as well as jealous, irritable, and prone to anger and irritation patients described themselves, the stronger their feelings of anxiety, as measured both by the GAD-7 questionnaire (Ƭ=−0,57; p = 0.000) and the BAI questionnaire (Ƭ=- 0,474; p = 0.000). A high Tau coefficient value indicates a high correlation between these two variables for both questionnaires used to measure anxiety.
Depression
During statistical analysis using the Kendall Tau correlation test, a statistically significant relationship was found between personality traits such as extraversion, conscientiousness, emotional stability, and intellect, and the degree of depression severity.
In the case of both extraversion and conscientiousness, this relationship was observed only in the severity of depression measured by the BDI questionnaire. No such relationship was found with the PHQ-9 questionnaire. The more a patient is characterized as introverted, reserved, quiet, and socially inhibited, the stronger the relationship with the severity of depression (Ƭ=−0,172; p = 0.008). Similarly, the more unsystematic and inconsistent a patient is, neglecting order and planning, being careless and uncertain, the more severe their depression symptoms (Ƭ=−0,157; p = 0.0161). As indicated by the Tau coefficient value, the correlation strength is not high in both cases.
For the intellect personality trait, a statistically significant relationship with the degree of depression severity was observed using both questionnaires. The more a patient can be characterized as unintellectual, uninquisitive, unimaginative, simple, unrefined, unreflective, and uncreative, the more severe their depressive symptoms are, as measured by the BDI questionnaire (Ƭ=−0,169; p = 0.01) and the PHQ-9 questionnaire (Ƭ=−0,153; p = 0.019). As indicated by the Tau coefficient value, the correlation strength is not high in both cases.
A strong statistical relationship is also found between emotional stability and depression symptoms. Specifically, the more anxious, nervous, prone to worry, and hypersensitive individuals are, along with being more jealous, irritable, and prone to anger and irritation, the more severe their depression symptoms tend to be. This is demonstrated by the statistical analysis of the BDI questionnaire (Ƭ=−0,501; p = 0.000) and the PHQ-9 questionnaire (Ƭ=−0,536; p = 0.000), respectively. Thus, high Tau coefficient values show that the relationship between low emotional stability and increased sense of depression measured in both questionnaire studies (BDI, PHQ-9) is related with a high correlation strength.
Discussion
From a clinical perspective, how patients cope with pain or report the co-occurrence of symptoms such as sleep disorders, heightened anxiety, stress, or depression is extremely important. All of these accompanying symptoms undoubtedly influence the treatment process and the alleviation of the patient’s symptoms. This raises the question of whether there is a specific trait or set of personality traits that predisposes patients to a worse disease progression or the co-occurrence of other conditions. Therefore, perhaps as doctors, we should be more attuned to certain personality types in patients, as these may predispose them to a more severe course of illness and a weaker response to prescribed treatments.
The influence of the patient’s personality on reported pain was also the subject of research by Manfredini et al.43. They included two groups of patients with chronic TMJ pain in their study. The first group consisted of patients showing symptoms of TMJ effusion on magnetic resonance imaging (MRI), while the second group included patients with TMJ pain that was unjustified, due to the absence of disorders detected on MRI. A third group of pain-free people was selected as the comparison group. All patients completed a personality assessment using the Minnesota Multiphasic Personality Inventory-2 (MMPI-2)43. The authors examined the psychological profiles of patients with TMJ pain and effusion visible on MRI, those with TMJ pain but no effusion on MRI, and a control group of patients without TMJ pain. The study hypothesis was that patients without other potential causes of pain in the TMJ area might have a distinct personality profile. The results supported this hypothesis, showing that patients with chronic TMJ pain and no effusion had a personality profile characterized by significant concern about physical health and physical symptoms. Similar to our research team, the authors recognize this relationship as an important clinical implication, suggesting that it is essential to consider the potential existence of a psychologically modulated condition in patients who report TMJ pain without signs of effusion43.
OFP is often classified as chronic pain. It should be emphasized that chronic pain is frequently associated with high levels of psychological distress, as described in the literature44,45. Therefore, the psychoemotional state of our patients is crucial at both the diagnostic and therapeutic levels. This aligns with the conclusions drawn from our work and provides additional important insights for dentists treating patients with chronic OFP or headaches.
In their work, Rerrando et al. report that patients with TMD of muscular etiology exhibit higher levels of anxiety, fear, and depression, as well as less use of positive reinterpretation and humor as coping strategies46. The group of patients with TMD of articular etiology showed higher distress, less pain-related positive reinterpretation, and lower interest in seeking instrumental social support compared to the control group. According to the researchers, a lack of behavioral engagement was a predictor of stress in both temporomandibular groups. In the muscle group, neuroticism and depression were observed, while in the joint group, conscientiousness and self-discipline were identified. Thus, the researchers presented the relationship between specific personality traits and the occurrence of TMD, whether of muscular or joint origin46.
Yap et al. also distinguished patients based on the origin of TMD, emphasizing the importance of psychological factors, especially in patients with the muscular form of TMD47. Their research concluded that patients diagnosed with myofascial pain and other joint conditions had significantly higher levels of depression and somatization compared to those diagnosed solely with disk displacements47. These findings are consistent with research by Meldolesi et al.48, which explored the relationship between emotional dysfunction and TMJ dysfunction. Their study suggests that psychological factors play a more significant role in muscle pain48. Auerbach et al. found similar results, highlighting the relationship between emotions and TMD. Their findings confirm that psychological factors have a greater influence in cases of pain of muscular origin49. However, research by Nifosi et al. indicated that while TMD patients showed increased levels of depression, somatization, and anxiety, these traits did not significantly differ between patients with myofascial pain and those with joint pain50.
Based on the findings from previous authors and our research, conclusions can be drawn that contribute to improving the quality of life for patients with TMD. This is particularly significant for the early diagnosis of mental health issues, such as the development of depression and anxiety. Early detection of mental disorders should be a focus of preventive mental health screenings in patients with chronic OFP and headaches, especially in those with myogenous TMD.
Hekmati et al., in their study, focused on the association between TMD and personality profiles using the Minnesota Multiphasic Personality Inventory-2-Reconstructed (MMPI-2-RF) form50. The authors identified personality characteristics that were more prevalent in the TMD patient group compared to the control group. These characteristics include emotional/internalizing dysfunction (EID), behavioral/externalizing dysfunction (BXD), demoralization, somatic complaints, low positive emotions, antisocial behavior, ideas of persecution, and dysfunctional negative emotions51.
In the study by Yap et al., conducted on two groups of patients—one with TMD and the other a healthy control group—significantly higher levels of negative affectivity, anxiety, and stress were found in patients with TMD compared to those without TMD symptoms. The researchers used the Big Five Inventory-10 (BFI-10) questionnaire. Moreover, patients with TMD showed significantly greater somatization and more oral behaviors than the group without TMD symptoms52.
Study limitations
We consider the lack of a control group of healthy participants to be the biggest limitation of this study. Our future work will focus on assessing the impact of the patient’s personality on the pain experienced, with an extension of the analysis to include a control group. The limitations of this study are also related to the use of questionnaires to assess OFP and headache characteristics. The study does not include a tool to objectively measure pain intensity in patients. We also consider the lack of DC/TMD protocol (Diagnostic Criteria for Temporomandibular Disorders)12 to make a specific diagnosis of temporomandibular joints and masticatory muscle disorders as a limitation of this study. The lack of analysis of the examined relationships by gender can also be considered a limitation. The use of scales recommended by the psychiatrist was performed by different researchers, which can also be considered a limitation of this study. Another important limitation of this study is the fact that the relationship between pain and the patient’s psycho-emotional state and personality traits may be bidirectional. As the studies cited in the discussion show, chronic pain can lead to high levels of psychological distress. Therefore, the patient’s personality traits may also be moderated by the level of chronic pain that accompanies it. Limitations related to the polysomnographic examination include the use of a one-night recording. Additionally, it should be noted that the conditions in the sleep laboratory differ from those in which the examined person usually sleeps, and the negative impact of the new environment on sleep quality is most evident during the first night spent in the sleep laboratory.
Nevertheless, our study has several advantages, making it important in exploring this topic. To our knowledge, an objective diagnostic method of sleep quality and sleep breathing disorders - polysomnography (avPSG) is not often used to assess sleep quality in patients complaining of primary headache or orofacial pain, so this is undoubtedly a strong advantage of the research we conducted. In addition, a large group of participants took part in this study (n = 114), which is extremely important in light of obtaining valuable results. Another advantage of this study is the fact that we used many validated questionnaires, selected by a specialist psychiatrist, which reliably allowed for the assessment of such items as anxiety, depression, stress level, personality traits, and subjective sleep quality in a wide group of patients. Thanks to these advantages, the results of this study show great potential for further research and clinical purposes.
Conclusion
The results of our study revealed that emotional stability had the strongest relationship and influence on the pain complaints experienced by patients and the deterioration of the patient’s psycho-emotional state. Patients who were characterized as anxious, nervous, moody, prone to worry, and oversensitive, as well as envious, touchy, and prone to anger and irritation, are patients who report stronger pain complaints and in whom pain has the strongest negative impact on daily functioning and is most strongly associated with limitation and exclusion from professional, family or social activity. The study shows a strong link between lower emotional stability and feelings of anxiety, depression, and stress. Low emotional stability may indicate that the patient’s treatment process will be more challenging, that the symptoms will be more severe, often accompanied by issues such as sleep disorders, and that the patient may show a weaker response to the proposed therapeutic tools. By identifying these traits early, we can promptly provide the patient with psychotherapeutic care, use known relaxation techniques, and refer them to a mental health clinic to prevent the onset of depression and anxiety, which could worsen the patient’s condition and their response to therapy.
Data availability
Data availabilityAll data supporting the findings of this study are available within the article and can be obtained from the corresponding authors upon reasonable request.
References
https://www.iasp-pain.org/advocacy/global-year/orofacial-pain/
Seweryn, P. et al. Relationship between pain severity, satisfaction with life and the quality of sleep in Polish adults with temporomandibular disorders. Dent. Med. Probl. 60 (4), 609–617. https://doi.org/10.17219/dmp/171894 (2023).
International Classification of Orofacial Pain. 1st edition (ICOP). Cephalalgia 40 (2), 129–221. https://doi.org/10.1177/0333102419893823 (2020).
Headache Classification Committee of the International Headache Society (IHS) The international classification of headache disorders, 3rd edition. Cephalalgia 38 (1), 1–211. https://doi.org/10.1177/0333102417738202 (2018).
Wieckiewicz, M. et al. Determination of pain intensity, pain-related disability, anxiety, depression, and perceived stress in Polish adults with temporomandibular disorders: A prospective cohort study. Front. Integr. Neurosci. 16, 1026781. https://doi.org/10.3389/fnint.2022.1026781 (2022). PMID: 36407294; PMCID: PMC9668250.
Martynowicz, H. et al. A case-control study on the effect of rhythmic masticatory muscle activity (RMMA) clusters on sleep fragmentation and severity of orofacial muscle pain in sleep Bruxism. J. Sleep. Res. 33 (4), e14072. https://doi.org/10.1111/jsr.14072 (2024).
Orzeszek, S. et al. Assessment of sleep quality in patients with orofacial pain and headache complaints: A polysomnographic study. Dent. Med. Probl. 61 (4), 549–562. https://doi.org/10.17219/dmp/177008 (2024).
Wieckiewicz, M. et al. Prevalence and overlaps of headaches and painrelated temporomandibular disorders among the Polish urban Popula Tion. J. Oral Facial Pain Headache. 34 (1), 31–39 (2020).
Manfredini D, Borella L, Favero L, Ferronato G, Guarda-Nardini L. Chronic pain severity and depression/somatization levels in TMD patients. Int J Prosthodont. 23(6), 529–34.
Manfredini, D. et al. Axis II psychosocial findings predict effectiveness of TMJ hyaluronic acid injections. Int. J. Oral Maxillofac. Surg. 42, 364–368. https://doi.org/10.1016/j.ijom.2012.10.033 (2013).
Manfredini, D., Marini, M., Pavan, C., Pavan, L. & Guarda-Nardini, L. Psychosocial profiles of painful TMD patients. J. Oral Rehabil. 36, 193–198. https://doi.org/10.1111/j.1365-2842.2008.01926.x (2009).
Schiffman, E. et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network** and orofacial pain special interest group†. J. Oral Facial Pain Headache. 28 (1), 6–27. https://doi.org/10.11607/jop.1151 (2014).
Klasser, G. D., Almoznino, G. & Fortuna, G. Sleep and orofacial pain. Dental Clin. N. Am. https://doi.org/10.1016/j.cden.2018.06.005 (2018).
Ananthan, S. & Benoliel, R. Chronic orofacial pain. J Neural Transm (Vienna). ;127(4):575–588. (2020). https://doi.org/10.1007/s00702-020-02157-3. Epub 2020 Mar 4. PMID: 32130516.
Dreweck, F. D. S. et al. Association between painful temporomandibular disorders and sleep quality: A systematic review. J. Rehabil. https://doi.org/10.1111/joor.12993 (2020).
American Academy of Sleep Medicine (Ed.). International Classification of Sleep Disorders 3rd edn p. 303e11 (American Academy of Sleep Medicine, 2014).
Berry, R. B. et al. AASM scoring manual updates for 2017 (Version 24). J. Clin. Sleep. Med. 13 (5), 665–666. https://doi.org/10.5664/jcsm.6576 (2017).
Goldberg, L. R. et al. The international personality item pool and the future of Public-Domain personality measures. J. Res. Personal. 40, 84–96. https://doi.org/10.1016/j.jrp.2005.08.007 (2006).
Cieślik, B., Kuligowski, T., Cacciante, L. & Kiper, P. The impact of personality traits on patient satisfaction after telerehabilitation: A comparative study of remote and Face-to-Face musculoskeletal rehabilitation during COVID-19 lockdown. Int. J. Environ. Res. Public. Health. 20 (6), 5019. https://doi.org/10.3390/ijerph20065019 (2023). PMID: 36981927; PMCID: PMC10049300.
Topolewska, E., Skimina, E., Strus, W. & Cieciuch, J. Rowiński T. Krótki Kwestionariusz do Pomiaru Wielkiej Piątki IPIP-BFM-20. Rocz Psychol. 17, 367–402 (2014).
Thalmayer, A. G. & Saucier, G. Comparative validity of brief to medium length big five and big six personality questionnaires. Psychol. Assess. 23 (4), 995–1009 (2011).
Gosling, S. D., Rentfrow, P. J. & i Swann, W. B. A very brief measure of the Big-Five personality (2003).
Strus, W., Cieciuch, J. & Rowiński, T. Polish version of Big Five Aspects Scales from International Personality Item Pool. Poster for the 16th European Conference on Personality, Triest, July 10–14, 2012. (2012).
Plopa, M. & Makarowski, R. in Sense of Stress Questionnaire. 1st edn (eds Wizja) (Warszawa, Poland,, 2010), 62-89.
Spitzer, R. L., Kroenke, K. & Williams, J. B. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA 282, 1737–1744 (1999).
Beck, A. T., Ward, C. H., Mendelson, M., Mock, J. & Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry. 4, 561–571 (1961).
Bastianon, C. D. et al. Perceived stress scale (PSS-10) psychometric properties in migrants and native Germans. BMC Psychiatry. 20 (1). https://doi.org/10.1186/s12888-020-02851-2 (2020).
Williams, N. & Medicine, O. The GAD-7 questionnaire, Volume 64, Issue 3, April Page 224, (2014). https://doi.org/10.1093/occmed/kqt161
Bastien, C. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2 (4), 297–307. https://doi.org/10.1016/s1389-9457(00)00065-4 (2001).
Manzar, M. D. et al. Dimensionality of the Pittsburgh sleep quality index: a systematic review. Health Qual. Life Outcomes. 16 (1). https://doi.org/10.1186/s12955-018-0915-x (2018).
Silva, G. E., Vana, K. D., Goodwin, J. L., Sherrill, D. L. & Quan, S. F. Identification of patients with sleep disordered breathing: comparing the Four-Variable screening tool, STOP, STOP-Bang, and Epworth sleepiness scales. J. Clin. Sleep Med. 07 (05), 467–472. https://doi.org/10.5664/jcsm.1308 (2011).
Melzack, R. The short-form McGill pain questionnaire. Pain 30 (2), 191–197. https://doi.org/10.1016/0304-3959(87)91074-8 (1987).
Von Korff, M. et al. Graded chronic pain scale revised. PAIN 1. https://doi.org/10.1097/j.pain.0000000000001758 (2019).
Yang, M., Rendas-Baum, R., Varon, S. F. & Kosinski, M. Validation of the headache impact test (HIT-6™) across episodic and chronic migraine. Cephalalgia 31 (3), 357–367. https://doi.org/10.1177/0333102410379890 (2010).
Gonzalez, Y. M. et al. Development of a brief and effective temporomandibular disorder pain screening questionnaire. J. Am. Dent. Association. 142 (10), 1183–1191 (2011).
Manfredini, D., Serra-Negra, J., Carboncini, F. & Lobbezoo, F. Current concepts of Bruxism. Int. J. Prosthodont. 30, 437–438. https://doi.org/10.11607/ijp.5210 (2017). [PubMed] [CrossRef] [Google Scholar].
Lobbezoo, F. et al. International consensus on the assessment of bruxism: report of a work in progress. J. Oral Rehabil. 45, 837–844. https://doi.org/10.1111/joor.12663 (2018). [PMC free article] [PubMed] [CrossRef] [Google Scholar].
Lobbezoo, F. et al. Bruxism defined and graded: an international consensus. J. Oral Rehabil. 40, 2–4. https://doi.org/10.1111/joor.12011 (2013).
Wieckiewicz, M. et al. Genetic basis of sleep Bruxism and sleep apnea-response to a medical puzzle. Sci. Rep. 10 (1), 7497. https://doi.org/10.1038/s41598-020-64615-y (2020).
Smardz, J. et al. Lower serotonin levels in severe sleep Bruxism and its association with sleep, heart rate, and body mass index. J. Oral Rehabil. 49 (4), 422–429. https://doi.org/10.1111/joor.13295 (2022).
Chemelo, V. D. S. et al. Is there association between stress and bruxism?? A systematic review and Meta-Analysis. Front. Neurol. 11, 590779. https://doi.org/10.3389/fneur.2020.590779 (2020).
Więckiewicz, M., Lavigne, G. & Martynowicz, H. Decrypting the putative interrelation between sleep bruxism, masticatory muscle pain and sleep breathing disorders: nosology and the role of hypoxia. Dent. Med. Probl. 61 (2), 165–167. https://doi.org/10.17219/dmp/175686 (2024).
Manfredini, D., Cerea, S., Pavan, C. & Guarda-Nardini, L. Personality traits are potentially associated with the presence of chronic temporomandibular joint pain in patients without effusion as determined by T-2 weighted magnetic resonance. Cranio 36 (2), 91–97 (2018). Epub 2017 Mar 20. PMID: 28317450.
Suvinen, T. I. et al. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur. J. Pain. 9, 613–613 (2005).
Manfredini, D. et al. Psychosocial profiles of painful TMD patients. J. Oral Rehabil. 36, 193–198 (2009).
Ferrando, M. et al. Psychological variables and temporomandibular disorders: distress, coping, and personality. oral surgery, oral medicine, oral pathology. Oral Radiol. Endodontology. 98 (2), 153–160. https://doi.org/10.1016/j.tripleo.2003.12.030 (2004).
Yap, A. U. J., Tan, K. B. C., Prosthodont, C., Chua, E. K. & Tan, H. H. Depression and somatization in patients with temporomandibular disorders. J. Prosthet. Dent. 88 (5), 479–484. https://doi.org/10.1067/mpr.2002.129375 (2002).
Meldolesi, G., Picardi, A., Accivile, E., Toraldo di Francia, R. & Biondi, M. Personality and psychopathology in patients with temporomandibular joint pain-dysfunction syndrome. A controlled investigation. Psychother Psychosom. (2000). Nov-Dec;69(6):322-8 https://doi.org/10.1159/000012415. PMID: 11070445.
Auerbach, S. M., Laskin, D. M., Frantsve, L. M. E. & Orr, T. Depression, pain, exposure to stressful life events, and long-term outcomes in temporomandibular disorder patients. J. Oral Maxillofac. Surg. 59 (6), 628–633. https://doi.org/10.1053/joms.2001.23371 (2001).
Nifosi, F., Violato, E., Pavan, C., Sifari, L., Novello, G., Nardini, L. G., … Marini,M. (2007). Psychopathology and Clinical Features in an Italian Sample of Patients with Myofascial and Temporomandibular Joint Pain: Preliminary Data. The International Journal of Psychiatry in Medicine, 37(3), 283–300. doi:10.2190/pm.37.3.f.
Hekmati, A., Mortazavi, N., Ozouni-Davaji, R. B. & Vakili, M. Personality traits and anxiety in patients with temporomandibular disorders. BMC Psychol. 10 (1), 86. https://doi.org/10.1186/s40359-022-00795-8 (2022). PMID: 35379356; PMCID: PMC8978430.
Yap, A. U. & Marpaung, C. Personality, psychosocial and oral behavioural risk factors for temporomandibular disorder symptoms in Asian young adults. J. Oral Rehabil. 50 (10), 931–939. https://doi.org/10.1111/joor.13527 (2023). Epub 2023 Jun 6. PMID: 37256928.
Funding
The study is part of a project funded by Wroclaw Medical University (grant number SUBK.B160.24.030).
Author information
Authors and Affiliations
Contributions
SO analyzed the data and wrote the manuscript. MW and HM developed the research concept and edited the manuscript. WB performed the statistical analysis. MW, JS, and SO recruited patients for the study. HM and AW conducted the polysomnography. SO collected the references. SO and MW managed the funding. MW, AJ, and HM revised the manuscript prior to final submission. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Orzeszek, S., Martynowicz, H., Smardz, J. et al. Relationship between pain, quality of sleep, sleep bruxism and patients’ personality among individuals with reported orofacial pain. Sci Rep 15, 25009 (2025). https://doi.org/10.1038/s41598-025-09978-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-09978-w