Abstract
This study explored the interventional role and potential mechanism of total flavonoids from lychee seeds (TFL) on rats with liver fibrosis, focusing on the LPS/TLR2/4 signaling pathway and intestinal mucosal barrier theories. Male Sprague-Dawley (SD) rats were randomly divided into six groups: Control, Model, Silymarin (43.19 mg·kg⁻¹), TFL low dose (TFL-L, 25 mg·kg⁻¹), TFL medium dose (TFL-M, 50 mg·kg⁻¹), and TFL high dose (TFL-H, 100 mg·kg⁻¹). All groups received oral administration once daily for six weeks. Histopathological evaluations of liver tissues were conducted using HE and Masson staining, while fibrosis scores were assessed. Colon tissues were examined by HE staining for signs of inflammation and cellular infiltration. Immunohistochemistry detected the expression of tight junction proteins ZO-1, occludin, claudin 1, and claudin 4 related to the intestinal barrier. Serum levels of HA, IV-C, LN, PC-III, ALT, AST, and LPS were determined via ELISA. RT-qPCR was used to measure gene expression levels of TNF-α, IL-6, IL-1β, Ccl2, Ccl4, TLR2, TLR4 in liver tissue, and ZO-1, occludin, claudin 1, and claudin 4 in colon tissue. Compared to the Control group, the Model group exhibited significantly higher fibrosis scores, increased serum LPS, ALT, AST, LN, HA, IV-C, and PC-III levels, as well as elevated relative expression levels of Ccl2, TLR2, TLR4, IL-6, IL-1β, and TNF-α genes. After treatment with TFL, pathological scores in all TFL groups were significantly reduced, along with decreased serum levels of LPS, ALT, AST, HA, IV-C, and PC-III compared to the Model group. The relative expression levels of Ccl2, TLR2, TLR4, IL-1β, IL-6, and TNF-α genes in the TFL-H group were also notably lower than those in the Model group. No significant differences were observed in the relative expression of Ccl4 across groups. In addition, the expression of various tight junction-related proteins in the colonic mucosa of the Model group was significantly reduced, whereas the TFL-H group showed significantly richer staining compared to the Model group. TFL demonstrates a good anti-fibrotic effect, with a clear dose-response relationship, where the highest dosage produced the best results. Its anti-fibrotic effect may be associated with restoring intestinal mucosal barrier function and inhibiting the LPS/TLR2/4 signaling pathway.
Similar content being viewed by others
Introduction
Hepatic fibrosis (HF), characterized by excessive proliferation and deposition of extracellular matrix (ECM) components, leads to abnormal structural changes in liver tissue. This condition represents a critical phase in the progression of various chronic liver diseases toward cirrhosis and hepatocellular carcinoma1,2. Traditional treatments predominantly focus on alleviating local symptoms of the liver, such as using interferon to inhibit viral replication or colchicine to combat fibrosis. However, these methods often only partially slow disease progression and are unable to fundamentally block the complex pathological processes underlying hepatic fibrosis3.
In Traditional Chinese Medicine (TCM), HF is categorized under terms such as “accumulation” and “flank pain.” Key pathogenic factors include dampness, heat, phlegm, blood stasis, and toxicity. Deficiencies in qi and blood, along with diminished vital energy, are considered fundamental to its onset. Therapeutic strategies emphasize soothing the liver, reinforcing the spleen, nourishing qi and blood, promoting blood circulation, and resolving stasis4,5.
The use of lychee seeds (Litchi Chinensis Sonn) has been documented in ancient traditional Chinese medical literature. Total flavonoids from lychee seeds (TFL), an active pharmacological component extracted from lychee seeds6, is primarily used in modern clinical settings to treat various fibrotic proliferative diseases, such as hepatitis B-induced liver cirrhosis, breast hyperplasia, and uterine fibroids7,8. However, research on its mechanisms of action against hepatic fibrosis within the context of modern medicine is still in its early stages.
Modern scientific research indicates that the process of hepatic fibrosis involves complex changes at multiple cellular and molecular levels, such as hepatocyte apoptosis, release of inflammatory factors, and alterations in gut barrier function. Studies have shown that high mobility group box-1 (HMGB-1), secreted by apoptotic hepatocytes, can form complexes with single-stranded DNA, lipopolysaccharide (LPS), interleukin-1β (IL-1β), and other inflammatory factors, thereby inducing inflammatory responses9. Additionally, when LPS binds to Toll-like receptor 4 (TLR4), it further activates hepatic stellate cells (HSCs), leading to extensive deposition of ECM in liver tissue. Moreover, a high-fat diet induces low-grade inflammatory cell infiltration in the intestines of mice, accompanied by hepatic steatosis. This condition is associated with increased expression of inflammatory factors such as IL-1β, IL-6, and ICAM-1 in the gut, as well as elevated levels of triglycerides (TG) and total cholesterol (TC) in serum and liver tissues. Treatment with tauroursodeoxycholic acid (TUDCA) alleviates intestinal inflammation and consequently mitigates hepatic steatosis10. Studies have also demonstrated that varying degrees of gut barrier dysfunction are present in various chronic liver diseases11,12.
The intestinal mechanical barrier primarily consists of tight junction proteins such as occludin, claudins, and zonula occludens (ZOs), which, together with the actin cytoskeleton, connect adjacent cells to form the intestinal mucosal epithelial barrier13. Damage to these proteins can directly increase gut mucosal permeability.
Disruption of the gut microbiota impairs gut barrier function, allowing bacterial products like LPS and bacterial DNA—pathogen-associated molecular patterns (PAMPs)—to enter the liver via the portal vein. This subsequently activates multiple cell types in the liver, including Kupffer cells, hepatocytes, and HSCs, particularly through Toll-like receptors (TLRs), especially TLR4. In HSCs, activation of TLR4 induces the production of various chemokines and adhesion molecules, which in turn recruit Kupffer cells14.
This study hypothesizes that TFL mitigates hepatic fibrosis progression through gut-liver crosstalk: this compound reduces gut inflammation, enhances gut barrier function, modulates the gut microbiota, and decreases the release of inflammatory factors, thereby slowing the progression of hepatic fibrosis.
Materials
Main equipment
Fluorescence Quantitative PCR Instrument: Manufactured by Beijing Analytical Instrument Co., Ltd., Beijing. Fully Automated Chemiluminescence/Fluorescence Imaging Analysis System 5200Multi: Shanghai Tianeng Life Science Co., Ltd. Benchtop Refrigerated Centrifuge Model 5430R: Eppendorf China Co., Ltd. Vortex Mixer Model XH-C: Supplied by Ronghua Experimental Equipment Co., Ltd., Jiangsu Province, China. Microplate Reader Epoch: BioTek Instruments, Inc., USA. Electrophoresis Unit DYCP-31DN: Produced by Beijing Children’s Day Biotechnology Co., Ltd.
Main drugs and reagents
TFL: Generously supplied by the College of Pharmacy at Guangxi University of Chinese Medicine. TFL extraction followed the protocol described by Feng Yu et al. [6], achieving a purity of 50%. Silymarin Capsules (Lot No.: 250703016; 30 mg silymarin per capsule): Procured from Tianjin Tasly Sainty Pharmaceutical Co., Ltd. Carbon Tetrachloride (CCl₄) (Analytical Grade): Obtained from Tianjin Hengxing Chemical Reagent Manufacturing Co., Ltd. ELISA Kits: For procollagen type III (PCIII), collagen type IV (IV-C), laminin (LN), hyaluronidase (HA), LPS, alanine aminotransferase (ALT), and aspartate aminotransferase (AST). These were purchased from Jiangsu Enzyme-Free Industry Co., Ltd. with lot numbers 202,305-M010, 202,305-M023, 202,305-M014, 202,303-M025, 202,301-M009, 202,306-M029, and 202,306-M030, respectively. Antibodies: Anti-ZO-1 (Lot No. ab276131) and anti-Occludin (Lot No. ab216327) antibodies were acquired from Abcam (Shanghai) Trading Co., Ltd. Antibodies recognizing Claudin1 (Lot No. sc-166338) and Claudin4 (Lot No. sc-376643) were sourced from Santa Cruz Biotechnology. RNA Extraction Kit (Lot No. RC112-01) and SYBR qPCR Kit (Lot No. R223-01): Both products of Nanjing Novozymes Biotech Co., Ltd.
Experimental animals
Fifty-six healthy male SPF-grade SD rats, aged 5 weeks and with an average weight of 150 g, were purchased from Hunan Nasdaq Experimental Animal Center (Animal Use Permit No.: SYXK Gui 2019-0001). All procedures were conducted in an SPF-level laboratory on the sixth floor of the Animal Experiment Center at Xianhu Campus, Guangxi University of Chinese Medicine. The rats were housed individually in SPF cages equipped with positive-pressure ventilation and filtration systems. Environmental conditions were maintained at a stable temperature range of 24 °C to 26 °C, humidity between 60% and 70%, and a day-night light cycle. Food and water were provided ad libitum, and bedding was periodically renewed by designated staff.
Methods
Grouping, modeling, and treatment
All experimental protocols were approved by the Ethics Committee of Guangxi University of Chinese Medicine (Approval No.: DW20220430-065). The study was conducted in accordance with relevant guidelines and regulations, and all methods are reported following the ARRIVE guidelines.
SD rats were adaptively fed for one week and then divided intorandomly assigned to Control (n = 8) or Model groups (n = 48) using a random number table. The hepatic fibrosis (HF) rat model was established by subcutaneous injection of carbon tetrachloride (CCl₄). The modeling group received subcutaneous injections of 40% CCl₄ (CCl₄: olive oil = 2:3) at a dose of 3.0 mg·kg⁻¹ every three days for a total of 8 weeks15. After completing the HF modeling, liver tissues from three randomly selected rats were collected and stained with Masson trichrome to evaluate the pathological morphology under a microscope to confirm the success of the model. During the modeling period, five rats died, leaving 40 rats which were subsequently divided into five groups using a random number table: Model group (Model group, 8 rats), Silybin group (SF group, 8 rats), low-dose TFL group (TFL-L group, 8 rats), medium-dose TFL group (TFL-M group, 8 rats), and high-dose TFL group (TFL-H group, 8 rats). The SF group served as the positive control for drug treatment16.
The Control group was maintained under normal conditions. The Model group received daily intragastric administration of 0.5 ml·kg⁻¹ of physiological saline. Dosage references were based on our research group’s previous studies17: the SF group received daily silybin at 43.19 mg·kg⁻¹; the TFL-L group received daily TFL at 25 mg·kg⁻¹; the TFL-M group received daily TFL at 50 mg·kg⁻¹; and the TFL-H group received daily TFL at 100 mg·kg⁻¹. All drugs were administered via oral gavage for a total of 6 weeks.
Sample harvesting
Twenty-four hours after the final treatment, rats were anesthetized with 2% sodium pentobarbital (50 mg/kg) intraperitoneally. Blood was drawn from the abdominal aorta, allowed to clot, and centrifuged at 1500 rpm for 15 min at 4 °C. The serum was stored at 4 °C for subsequent assays. Liver tissues were fixed in 4% paraformaldehyde, while additional pieces were snap-frozen in liquid nitrogen after placement in non-enzymatic tubes. The colon was excised, flushed with a non-enzymatic solution, segmented for fixation in 4% paraformaldehyde, and excess tissue was cryopreserved in liquid nitrogen.
Histopathological assessment
Liver and colon tissues underwent dehydration, clearing, embedding, sectioning, and staining with Hematoxylin and Eosin (HE) for histopathological evaluation. Separate sections were stained with Masson’s trichrome for assessing liver fibrosis, graded using the Ishak scoring system18 (detailed in Table 1). The colon tissues were also HE-stained for histomorphological assessment, and crypt damage and inflammatory infiltrate were scored according to seven categories (refer to Table 2).
Detection of ZO-1, occludin, Claudin-1, and Claudin-4
Immunohistochemical analysis was conducted to detect protein expression levels. Colon tissue sections from each group underwent dewaxing, hydration, blocking with hydrogen peroxide, rinsing, and antigen retrieval in citrate buffer. Subsequently, goat serum blocking solution was applied and incubated at room temperature for 1 h. The supernatant was discarded, and primary antibodies specific to ZO-1 (1:500), Occludin (1:200), Claudin-1 (1:100), and Claudin-4 (1:100) were added, followed by an overnight incubation at 4 °C. Afterward, corresponding HRP-conjugated goat anti-rabbit/mouse secondary antibodies (1:100) were introduced and incubated for 30 min at 37 °C. DAB was used for color development, with positive signals appearing brown to dark brown under microscopic examination. Post-washing, slides were counterstained with Harris’ hematoxylin for 2 min, differentiated with 1% acidic alcohol, and re-stained with a blue retrieval solution. Following dehydration, clarification, and mounting, slides were visually inspected and photographed under a microscope.
Quantification of LPS, ALT, AST
Serum levels of hyaluronidase (HA), collagen type IV (IV-C), laminin (LN), procollagen type III (PC-III), alanine aminotransferase (ALT), aspartate aminotransferase (AST), and lipopolysaccharide (LPS) were quantified using Enzyme-Linked Immunosorbent Assays (ELISAs). An appropriate volume of serum from each group was processed according to the respective kit protocols, and measurements were performed using a microplate reader.
RT-qPCR analysis
Real-time fluorescent quantitative PCR (RT-qPCR) was used to analyze the expression of TNF-α, IL-6, IL-1β, CCL2, CCL4, TLR2, TLR4, ZO-1, Occludin, Claudin-1, and Claudin-4 in rat liver and colon tissues. Frozen tissue samples were thawed on ice, and 10 mg of tissue was combined with 500 µL of buffer RL in a 1 mL centrifuge tube. Samples were thoroughly homogenized for RNA extraction and purity evaluation. cDNA synthesis was performed according to the kit instructions, and PCR amplification was carried out using this cDNA as the template. The reaction mixture (total volume 15 µL) consisted of 2 µL of cDNA template, 1.5 µL of combined forward and reverse primers, 7.5 µL of 2× qPCR Mix, and 4 µL of nuclease-free water. Amplification conditions included an initial denaturation at 95 °C for 30 s, followed by 40 cycles of denaturation at 95 °C for 10 s and annealing/extension at 60 °C for 30 s. Post-amplification, results were evaluated based on amplification and melting curves, with glyceraldehyde-3-phosphate dehydrogenase (GAPDH) serving as the internal control. Relative gene expression was calculated using the 2-ΔΔCt method, normalized to the Control group. Primer sequences and expected product sizes are detailed in Table 3.
Statistical analyses
Quantitative data from this study were presented as mean ± standard deviation (SD). SPSS software (version 26.0) facilitated statistical analyses, where independent samples were compared using a t-test, and ANOVA or rank-sum tests were employed for multiple independent samples in cases of unequal variance. A significance level of P < 0.05 was adopted.
Results
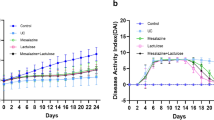
Histopathological findings in liver tissue
Liver tissues were examined for inflammatory lesions via HE staining and fibrosis via Masson staining. Control group specimens exhibited intact lobular architecture, intact central veins, and radiating hepatic cords, devoid of necrosis, inflammation, or fibrous deposits. In contrast, the Model group demonstrated disorganized hepatocyte patterns, lobular structure disruption, conspicuous infiltration by inflammatory cells, and widespread hepatocyte fat vacuolization. Masson staining disclosed prominent blue-purple staining indicative of fibrosis around portal tracts, reflecting fibrous septum formation without complete lobular encapsulation, typical of liver fibrosis. The fibrosis score of the Model group was significantly elevated compared to the Control group (P < 0.01). Relative to the Model group, the SF and TFL-H groups exhibited significantly lowered fibrosis scores (P < 0.05), with TFL-H showing the most pronounced improvement. TFL-L and TFL-M did not yield statistically significant variations in pathology scores compared to the Model group (refer to Figs. 1 and 2, and Table 4 for further details).
Histopathological findings in colon tissue
Rat colon tissues underwent HE staining. Upon evaluation, no substantial differences in pathological outcomes were detected among the groups, The crypt structure did not show significant changes, with intestinal inflammatory injury and inflammatory cell infiltration scores uniformly at zero across all groups. Representative illustrations of HE-stained sections are provided in Fig. 3.
Immunohistochemical outcomes for colon tissue
Under light microscopy, proteins ZO-1, Occludin, Claudin-1, and Claudin-4 appeared stained in a brownish hue. The Control group displayed ample brownish staining across the colonic mucosal surface, indicating that the Control group has the highest protein expression among all groups. Conversely, the Model group showed a pronounced decline in the expression of these tight junction-associated proteins in the colonic mucosa, exhibiting minimal brown staining. In the SF group and TFL low, medium, and high dosage groups, the positive expression of ZO-1, Occludin, Claudin-1, and Claudin-4 proteins in the intestinal epithelium was augmented to variable extents compared to the Model group, with the SF and TFL-H groups showcasing the most remarkable enhancements (depicted in Fig. 4).
Serum analysis of LPS, ALT, AST, and indices of liver fibrosis in rats
Enzyme-Linked Immunosorbent Assays (ELISAs) were implemented to quantify LPS, ALT, AST, LN, HA, Collagen Type IV (IV-C), and Procollagen Type III (PC-III) in rat sera across groups. Levels of LPS, ALT, AST, LN, HA, IV-C, and PC-III in the Model group were found to be significantly higher than those in the Control group (P < 0.05). Post-intervention with silymarin or various dosages of TFL, reductions in LPS, ALT, AST, HA, LH, IV-C, and PC-III levels in rat sera were statistically significant when compared to the Model group (P < 0.05) (Refer to Figs. 5 and 6), No significant crypt damage observed across groups.
RT-qPCR findings
Expression profiles of inflammatory-linked genes in rat liver
RT-qPCR was employed to evaluate the expression of Ccl2, Ccl4, TLR2, TLR4, IL-6, IL-1β, and TNF-α in the liver of rats across groups. It was discovered that the relative expression levels of Ccl2, TLR2, TLR4, IL-6, IL-1β, and TNF-α genes were significantly heightened in the Model group versus the Control group (P < 0.05), whereas Ccl4 expression remained unaltered (P > 0.05). Following interventions with silymarin, the SF group significantly curtailed the relative expression of Ccl2, TLR2, TLR4, IL-6, IL-1β, and TNF-α genes compared to the Model group (P < 0.05). Following interventions with different doses of TFL, the TFL-L group, Ccl2, Ccl4, and IL-6 showed significant declines (P < 0.05), no significant differences for TLR2, TLR4, IL-1β, and TNF-α (P > 0.05); The TFL-M group experienced significant reductions in Ccl2, TLR4, and IL-6 (P < 0.05), but no significant alterations in Ccl4, TLR2, IL-1β, and TNF-α (P > 0.05); Compared to the Model group, the TFL-H group significantly reduced the expression level of Ccl2, TLR2, TLR4, IL-1β, and IL-6 (P < 0.05), with Ccl4 showing no significant difference (P > 0.05) (Refer to Figs. 7 and 8).
Expression patterns of tight junction protein genes in rat colon
RT-qPCR was used to ascertain the expression levels of ZO-1, Occludin, Claudin-1, and Claudin-4 in the colon of rats across groups. The results indicated that the relative expression levels of ZO-1, Occludin, Claudin-1, and Claudin-4 genes were significantly depressed in the Model group compared to the Control group (P < 0.05).
After intervention with silymarin and different doses of TFL, specific trends in gene expression were observed. Compared to the Control group:
In the SF group, the relative expression levels of ZO-1, claudin-1, and claudin-4 genes were significantly downregulated (P < 0.05), while there was no significant difference in Occludin gene expression (P > 0.05).
Compared to the Model group, the SF group showed no significant differences in ZO-1, claudin-1, and claudin-4 genes (P > 0.05), but Occludin gene expression was significantly upregulated (P < 0.05).
For the low-dose TFL group (TFL-L): Compared to the Control group, the relative expression levels of ZO-1, claudin-1, and claudin-4 genes were significantly downregulated (P < 0.05), while there was no significant difference in Occludin gene expression (P > 0.05). Compared to the Model group, there were no significant differences in ZO-1, claudin-1, and claudin-4 genes (P > 0.05), but Occludin gene expression was significantly upregulated (P < 0.05).
For the medium-dose TFL group (TFL-M): Compared to the Control group, the relative expression levels of ZO-1 and claudin-4 genes were significantly downregulated (P < 0.05), while there were no significant differences in Occludin and claudin-1 gene expressions (P > 0.05). Compared to the Model group, there were no significant differences in ZO-1 and claudin-4 genes (P > 0.05), but Occludin and claudin-1 gene expressions were significantly upregulated (P < 0.05).
For the high-dose TFL group (TFL-H): Compared to the Control group, the relative expression levels of ZO-1 and claudin-4 genes were significantly downregulated (P < 0.05), while there were no significant differences in Occludin and claudin-1 gene expressions (P > 0.05). Compared to the Model group, there was no significant difference in claudin-4 gene expression (P > 0.05), but ZO-1, Occludin, and claudin-1 gene expressions were significantly upregulated (P < 0.05).
Detailed data are shown in Fig. 9.
Discussion
HF represents a critical pathophysiological process in the progression of various chronic liver diseases. Interventions targeting HF are essential for managing these conditions and halting their advancement to cirrhosis and hepatocellular carcinoma. Our study findings illustrate that following the induction of HF via subcutaneous CCl4 injection, hepatocellular damage in Model group rats was evident, as demonstrated by significantly raised ALT and AST levels, indicative of active hepatic inflammation. Notably, the expression of inflammatory cytokines—IL-6, TNF-α, and IL-1β—was significantly higher in the Model group compared to the Control group. Marked fibrotic changes in the liver were observed, with Masson staining revealing extensive fibrous accumulation. ELISA results further verified significantly increased serum concentrations of HA, LH, type IV-C collagen, and PC-III in Model group rats compared to Control group, along with a pronounced elevation in the HF score. Administration of TFL at different doses demonstrated its ability to reduce hepatic inflammatory cytokine expression, suppressing the inflammatory response and significantly lowering ALT and AST levels, thereby alleviating liver damage. Moreover, TFL reduced the serum content of collagen components, including HA, LH, type IV-C, and PC-III, effectively reversing fibrosis, as evidenced by a significantly lower HF score in the TFL-H group compared to the Model group. Prior studies21,22,23 have implicated TFL in modulating Bcl-2/Bax to HSCs apoptosis and MMPs and TIMPs in HSCs, thereby influencing ECM metabolism in the liver and exerting an anti-fibrotic effect.
In the colonic tissues of HF rats, disruptions to the intestinal barrier integrity were detected. While HE staining showed no overt inter-group differences, RT-qPCR analysis revealed a significant downregulation of genes associated with the intestinal barrier (ZO-1, Occludin, Claudin-1, Claudin-4) in the Model group compared to the Control group.
In the study of colon tissue, H&E staining did not reveal significant damage, indicating that the overall structure remained intact. However, immunohistochemical (IHC) analysis showed a reduction in tight junction proteins in the model group, suggesting microscopic damage to intercellular connections. This discrepancy may indicate early subcellular changes in the disease process, which, although not affecting macroscopic morphology, could potentially impact gut function and provide clues for future research. Damage to the tight junction structures in the gut can trigger leaky gut mechanisms. In various liver diseases, alterations in tight junction proteins increase intestinal permeability, allowing harmful substances to enter the bloodstream and affect the liver. Changes in tight junction proteins often influence the morphology of gut tissues, potentially compromising structural integrity, but this is not always inevitable and depends on factors such as the extent and duration of damage24. Excessive expression of inflammatory cytokines in vivo can disrupt tight junctions (TJs). Physiological concentrations of IL-1β and TNF-α are sufficient to cause a significant increase in intestinal epithelial TJ permeability25.
Wu et al.26 showed in mice with acute liver failure (ALF) that TNF-α and IL-6 signaling increase myosin light chain kinase (MLCK) and Rho-associated kinase (ROCK) activity, leading to cytoskeleton alterations and barrier dysfunction. Oxidative stress also impairs tight junctions; studies have reported imbalances in lipid peroxidation, protein oxidation, and glutathione redox status in cirrhotic patients, and oxidative stress disrupts tight junctions by altering protein dynamics. Unhealthy diets, such as those high in fat, can induce oxidative stress, damaging tight junctions and altering bile acid secretion, increasing hydrophobic bile acids, and ultimately leading to ROS accumulation and oxidative stress in intestinal epithelial cells.
Oxidative stress can also damage tight junctions (TJs). Studies have found that in patients with liver cirrhosis, there is an imbalance in lipid peroxidation, protein oxidation, and glutathione redox status27– 28. Oxidative stress disrupts TJs by affecting the assembly, localization, expression, and function of related proteins29. Poor dietary habits, such as prolonged excessive fat intake, can induce oxidative stress. This not only damages the normal structure of TJs but also leads to abnormal bile acid secretion, increasing the hydrophobic components in bile acids. Ultimately, this induces an abnormal increase in reactive oxygen species (ROS) within intestinal epithelial cells, leading to oxidative stress30.
The results of this study show that compared to the Control group, the Model group exhibited significantly elevated levels of inflammatory factors, resulting in increased concentrations of these factors in the bloodstream of HF rats, which in turn induced TJ dysfunction. Moreover, the olive oil used for subcutaneous injection in the modeling process for HF rats involves a high intake of fats, which also contributes to oxidative stress in the gut, further impacting gut barrier function.
This study also demonstrated that the Model group exhibited significantly greater inflammatory cytokine expression compared to the Control group, elevating systemic cytokine concentrations and impairing tight junction function. Furthermore, the high-fat olive oil regimen used in the Model group contributed to intestinal oxidative stress and further barrier impairment.
In this study, the serum endotoxin (LPS) levels in the Model group rats were significantly higher than those in the Control group, clearly indicating impaired gut barrier function and increased mucosal permeability, which led to LPS leakage from the gut into the systemic circulation. After intervention with different doses of TFL, the levels of inflammatory cytokines in each treatment group showed varying degrees of reduction compared to the Model group. Additionally, the expression of tight junction-related proteins in the colon tissues of the rats was significantly enhanced, and the gene expression of ZO-1, Occludin, and Claudin-1 was partially restored. Moreover, the LPS content in the serum was significantly lower compared to the Model group. These findings suggest that TFL not only possesses anti-inflammatory properties but also likely repairs gut barrier function, effectively reducing the translocation of pathogenic gut microbiota and endotoxins. This mechanism may play a crucial role in combating hepatic fibrosis.
Consistent with our findings, Koizumi et al. demonstrated through in vivo and in vitro experiments that elafibranor (a dual PPARα/δ agonist) prevents alcohol-induced liver fibrosis and cirrhosis by activating PPARα to enhance lipolysis and β-oxidation; augmenting hepatocyte autophagy and antioxidant capacity; suppressing Kupffer cell-mediated inflammatory responses; and blocking the LPS/TLR-4/NF-κB signaling pathway to restore tight junction protein expression, thereby reducing intestinal LPS translocation. In parallel, other studies confirm that tight junction proteins serve as critical therapeutic targets for natural compounds derived from Chinese herbal medicines in combating liver fibrosis31. For instance, Forsythiaside A (FTA)—a hepatoprotective phytochemical isolated from Forsythia suspensa—was shown by Fu et al. in animal studies to: Alleviate intestinal inflammation and edema; Significantly upregulate protein expression of ZO-1, claudin-1, and occludin in ileal tissues, mirroring our experimental outcomes32.
Microbial-associated molecular patterns (MAMPs), conserved components of pathogens including bacteria, viruses, fungi, and parasites, are rapidly recognized by pattern recognition receptors (PRRs), notably Toll-like receptor 4 (TLR4), triggering a rapid nonspecific immune response and inflammation)33. TLR4 is a key receptor for lipopolysaccharide (LPS)34– 35. LPS-induced TLR4 activation on cell surfaces initiates two signaling cascades: one through TIRAP and MyD88 and another through TRAM and TRIF, leading to the internalization of the TLR4-LPS complex. This internalization negatively regulates MyD88-dependent signaling, while the maturation of TLR4 endosomes and lysosomal degradation modulate TRIF-dependent signaling)36. LPS, bacterial DNA, and peptidoglycan, particularly from Gram-negative bacteria, can elicit inflammatory responses that may lead to fatal septic shock, with LPS being a primary mediator. The outer membrane of these bacteria contains LPS, phospholipids, lipoproteins, and surface proteins, with the toxic effects of LPS attributed to its lipid A component, which can elicit a strong innate immune response even at low doses, priming the immune system against infection)37. Kupffer cells (KC), the liver’s resident macrophages, play a critical role in non-specific immunity by phagocytosing pathogens entering through the portal or arterial circulation, serving as the first line of defense against gut-originating immunoreactive substances passing through the portal system and mediating anti-inflammatory actions in the liver. LPS activates KCs, and TLRs on their surface specifically recognize LPS38. In C3H/HeJ mice, mutations in TLR4 prevent LPS responses despite high lipopolysaccharide-binding protein (LBP) levels39. In the context of HF, a dysfunctional intestinal barrier permits LPS to enter the bloodstream, reach the liver, and bind to TLR2 and TLR4 on Kupffer cells, amplifying hepatic inflammation and promoting fibrosis.
The study results showed that, under the stimulation of CCl₄ and inflammatory conditions, the expression levels of TLR2 and TLR4 genes in the Model group were significantly higher compared to the Control group. After intervention with different doses of TFL, varying effects were observed. Specifically, in the high-dose TFL (TFL-H) group, the expression levels of TLR2 and TLR4 genes were downregulated to different extents compared to the Model group. While the low- and medium-dose groups also exhibited significant downregulation, the trend was most pronounced in the high-dose group. This suggests that high-dose TFL may effectively block LPS/TLR2/4 inflammatory signaling by downregulating the expression of LPS, TLR2, and TLR4 in rats. Consequently, this can reduce liver inflammation and decrease the secretion of ECM, ultimately contributing to the treatment of HF. The differential effects of various TFL doses provide important evidence for further investigation into its anti-HF mechanisms and for determining the optimal dosage.
Substantial evidence confirms TLR4 as a therapeutic target for liver cirrhosis and fibrosis. Clinical studies by Patel et al. demonstrated that rifaximin-α significantly reduced serum TLR4 expression in cirrhosis patients by Day 30, concomitantly improving hepatic encephalopathy40. Complementarily, Weber et al.41generated ABCB4 deficient (spontaneously developing biliary fibrosis mimicking human sclerosing cholangitis) with TLR4-deficient mice—and revealed that TLR4 deficiency protected against diethylnitrosamine (DEN)-induced liver injury and attenuated HF. These findings collectively validate TLR4 as a pivotal anti-fibrotic target, closely aligned with our experimental results.
In conclusion, TFL displays a promising anti-fibrotic effect with a dose-dependent correlation, with the highest dose exhibiting the greatest efficacy. Its anti-fibrotic mechanism appears to involve the restoration of intestinal mucosal barrier function and the inhibition of the LPS/TLR2/4 signaling pathway.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Kisseleva, T. & Brenner, D. Molecular and cellular mechanisms of liver fibrosis and its regression. Nat. Rev. Gastroenterol. Hepatol. 18 (3), 151–166 (2021).
Batudeleergeen, X. et al. Influence of Dedu Honghua-Qiwei San on apoptosis protein expression in rats with chronic liver injury induced by carbon tetrachloride. Chin. J. Clin. Pharmacol. 38 (11), 1215–1218 (2022).
Zhang Jingbo, C. & Pingping, Y. Exploring the mechanisms underlying the Anti-Hepatic fibrosis effects of various Huangqin-Chishao proportions in rats. China J. Experimental Traditional Med. Formulas. 28 (12), 69–77 (2022).
Wei Dandan, L. & Shanshan, Z. Interventional effect and mechanism of Dengzhanhua extract on rat liver fibrosis. China Pharm. 35 (6), 671–677 (2024).
Li, L. & Jing, Y. Early therapeutic efficacy of Ganshuo granules for liver fibrosis (S1-S2) with liver Qi stagnation, spleen deficiency, and blood stasis in chronic hepatitis B. China J. Experimental Traditional Med. Formulas. 28 (11), 132–138 (2022).
Feng, Y. et al. Optimizing the purification process of lychee seed total flavones using macroporous resins. Chin. J. Traditional Herb. Drugs. 50 (9), 2087–2093 (2019).
Cheng Wenhui, Z. & Liuying, H. X. Clinical assessment of lychee seed granules in the treatment of mammary hyperplasia. Clin. Med. Eng. 20 (1), 25–26 (2013).
Liu Guangqiao, L. & Weisheng Illustrative clinical cases: professor Luo weisheng’s approach to treating chronic liver disease from a deficiency perspective. J. Integr. Traditional Chin. Western Med. Liver Dis. 31 (12), 1134–1135 (2021).
Yang, H., Wang, H. & Andersson, U. Targeting inflammation driven by HMGB1[J]. Front. Immunol. 11, 484 (2020).
Wang, W. et al. Tauroursodeoxycholic acid inhibits intestinal inflammation and barrier disruption in mice with non-alcoholic fatty liver disease. Br. J. Pharmacol. 175 (3), 469–484 (2018).
Camilleri, M. Leaky gut: mechanisms, measurement and clinical implications in humans. Gut 68 (8), 1516–1526 (2019).
Tripathi, A. et al. The gut-liver axis and the intersection with the Microbiome. Nat. Rev. Gastroenterol. Hepatol. 15 (7), 397–411 (2018).
Heinemann, U. & Schuetz, A. Structural features of Tight-Junction proteins. Int. J. Mol. Sci., 20(23). (2019).
Chen, Y. H., Wu, W. K. & Wu, M. S. Microbiota-associated therapy for non-alcoholic steatohepatitis-induced liver cancer: A review. Int. J. Mol. Sci., 21(17). (2020).
Li, Z. et al. The effect of RhCygb on CCl4-Induced hepatic fibrogenesis in rat. Sci. Rep. 6, 23508. https://doi.org/10.1038/srep23508 (2016).
Zhang, T. et al. Water extract of earthworms mitigates mouse liver fibrosis by potentiating hepatic LKB1/Nrf2 axis to inhibit HSC activation and hepatocyte death. J. Ethnopharmacol. 1, 321117495. https://doi.org/10.1016/j.jep.2023.117495 (2024).
Yan, J. et al. Anti-liver fibrosis effects of the total flavonoids of litchi semen on CCl4-induced liver fibrosis in rats associated with the upregulation of retinol metabolism. Pharm. Biol. 60 (1), 1264–1277. https://doi.org/10.1080/13880209.2022.2086584 (2022).
Chowdhury, A. B. & Mehta, K. J. Liver biopsy for assessment of chronic liver diseases: a synopsis. Clin. Exp. Med. 23 (2), 273–285. https://doi.org/10.1007/s10238-022-00799-z (2023).
Deng, F. et al. YAP triggers the Wnt/β-catenin signalling pathway and promotes enterocyte self-renewal, regeneration and tumorigenesis after DSS-induced injury. Cell. Death Dis. 9 (2), 153 (2018).
Chen Shengbo. PBLD Suppresses Intestinal Epithelial Inflammation and Reinforces Barrier Function by Inhibition of the NF-κB Pathway [D]. (2021).
Feng Yinyi, Y. et al. Effects, mechanisms, and potential Q-marker prediction of lychee seed total flavones on carbon Tetrachloride-Induced liver fibrosis in rats. China J. Chin. Materia Med. 45 (23), 5722–5731 (2020).
Qin, Y. et al. Influence of lychee seed total flavones on the TGF-β/Smad signaling pathway in rats with liver fibrosis. China J. Experimental Traditional Med. Formulas. 19 (18), 223–227 (2013).
Ou Shiyu, L. et al. Effect of lychee seed total flavones on MMP-2 expression in liver tissues of rats with liver fibrosis. China J. Experimental Traditional Med. Formulas. 18 (13), 209–213 (2012).
Chopyk, D. M. & Grakoui, A. Contribution of the intestinal Microbiome and gut barrier to hepatic disorders. Gastroenterology 159 (3), 849–863 (2020).
Al-Sadi, R. et al. TNF-α modulation of intestinal tight junction permeability is mediated by NIK/IKK-α Axis activation of the canonical NF-κB pathway. Am. J. Pathol. 186 (5), 1151–1165 (2016).
Wu, F. et al. Phosphorylated–myosin light chain mediates the destruction of small intestinal epithelial tight junctions in mice with acute liver failure. Mol. Med. Rep., 23(5). (2021).
Spahr, L. et al. Allopurinol, oxidative stress and intestinal permeability in patients with cirrhosis: an open-label pilot study. Liver Int. 27 (1), 54–60 (2007).
Natarajan, S. K. et al. Intestinal mucosal alterations in rats with carbon tetrachloride-induced cirrhosis: changes in glycosylation and luminal bacteria. Hepatology 43 (4), 837–846 (2006).
Rao, R. K. et al. Tyrosine phosphorylation and dissociation of occludin-ZO-1 and E-cadherin-beta-catenin complexes from the cytoskeleton by oxidative stress. Biochem. J. 368 (Pt 2), 471–481 (2002).
Rohr, M. W. et al. Negative effects of a High-Fat diet on intestinal permeability: A review. Adv. Nutr. 11 (1), 77–91 (2020).
Koizumi, A. et al. Effects of Elafibranor on liver fibrosis and gut barrier function in a mouse model of alcohol-associated liver disease. World J. Gastroenterol. 30 (28), 3428–3446. https://doi.org/10.3748/wjg.v30.i28.3428 (2024).
Fu, K. et al. Forsythiaside A alleviated carbon tetrachloride-induced liver fibrosis by modulating gut microbiota composition to increase short-chain fatty acids and restoring bile acids metabolism disorder. Biomed. Pharmacother. 151, 113185. https://doi.org/10.1016/j.biopha.2022.113185 (2022).
Fitzgerald, K. A. & Kagan, J. C. Toll-like receptors and the control of immunity. Cell 180 (6), 1044–1066 (2020).
Zhang, Y. et al. Toll-like receptor 4 (TLR4) inhibitors: current research and prospective. Eur. J. Med. Chem. 235, 114291 (2022).
Olona, A. et al. Sphingolipid metabolism during Toll-like receptor 4 (TLR4)-mediated macrophage activation. Br. J. Pharmacol. 178 (23), 4575–4587 (2021).
Ciesielska, A., Matyjek, M. & Kwiatkowska, K. TLR4 and CD14 trafficking and its influence on LPS-induced pro-inflammatory signaling. Cell. Mol. Life Sci. 78 (4), 1233–1261 (2021).
Izadparast, F. et al. Protective effect of Berberine against LPS-induced injury in the intestine: a review. Cell. Cycle. 21 (22), 2365–2378 (2022).
Chen, S. N. et al. Deletion of TLR4 attenuates lipopolysaccharide-induced acute liver injury by inhibiting inflammation and apoptosis. Acta Pharmacol. Sin. 42 (10), 1610–1619 (2021).
Su, G. L. et al. Kupffer cell activation by lipopolysaccharide in rats: role for lipopolysaccharide binding protein and toll-like receptor. Hepatology 31 (4), 932–936 (2000).
Patel, V. C. et al. Rifaximin-α reduces gut-derived inflammation and mucin degradation in cirrhosis and encephalopathy: RIFSYS randomised controlled trial. J. Hepatol. 76 (2), 332–342. https://doi.org/10.1016/j.jhep.2021.09.010 (2022).
Weber, S. N., Bohner, A., Dapito, D. H., Schwabe, R. F. & Lammert, F. TLR4 deficiency protects against hepatic fibrosis and Diethylnitrosamine-Induced Pre-Carcinogenic liver injury in fibrotic liver. PLoS One. 11 (7), e0158819. https://doi.org/10.1371/journal.pone.0158819 (2016).
Funding
National Natural Science Foundation of China (82160834); Guangxi University of Chinese Medicine 2022 Doctoral Research Startup Fund Project (2022BS024); Guangxi Graduate Education Innovation Plan Project (YCBZ2022124); Integrated Chinese and Western Medicine prominent discipline in Guangxi ([2022] No. 1); National Renowned Traditional Chinese Medicine Experts Heritage Studio Construction Project ([20212] No. 75); Guangxi Famous Traditional Chinese Medicine Experts Heritage Studio Construction Project ([2021] No. 6).
Author information
Authors and Affiliations
Contributions
Tis study was completed in collaboration among all authors. X.J.C. and H.G.C. conceived, designed and coordinated the study. C.Y.H., Z.Y., Z.X. and Y.J.Y. performed the study. T. M.W., L.W.S. and M.X.C. carried out the date analyses. H.G.C., X.J.C. and L.M.H. drafed the manuscript. X.J.C. and H.G.C. contributed equally to this work and were therefore co-frst authors. All authors have contributed to, seen and approved the fnal manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiacheng, X., Guochu, H., Minhang, L. et al. The interventional role and mechanism of total flavonoids in lychee seeds on rats with liver fibrosis. Sci Rep 15, 24320 (2025). https://doi.org/10.1038/s41598-025-10007-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-10007-z