Abstract
The aim of this study was to explore the correlation between the parameters associated with the prevention and management of myopia and cylinder power (CP) progression in individuals who wear defocus incorporated multiple segments (DIMS) lenses. In total, 179 children (6–12 years old) prescribed DIMS lenses for 1 year were enrolled in this retrospective cohort study. Cycloplegic refraction, spherical equivalent (SE), axial length (AL), CP, and corneal astigmatism (CA) were measured. The relationship between myopia and CP progression was assessed using binary logistic regression analyses, stratified analyses, and interaction tests. These 179 DIMS lens wearers were, on average, 9.51 ± 1.48 years old, and 51.4% were male. In total, 24.02% of these participants had CP progression ≥ 0.25 D within one year. A fully-adjusted binary logistic regression analysis revealed that ΔSE (odds ratio (OR) = 1.73, 95% CI (1.32, 2.27), P < 0.001) and CA at admission (OR = 1.17, 95% CI (1, 1.36), P = 0.049) were associated with CP progression following adjustment for potential confounding factors. Interaction analysis revealed no significant interactive relationships. Our results showed a significant positive association between ΔSE and CP progression in DIMS lens wearers. Furthermore, baseline CA was also associated with ΔCP in participants over the course of the study. This suggested that myopia progression and baseline CA levels contribute to variations in CP progression. This study helps optimize astigmatism control in preventing and controlling myopia in DIMS lens wearers.
Similar content being viewed by others
Introduction
Myopia is a global public health concern. Its prevalence has increased dramatically in recent decades, particularly in East Asian countries1,2. Astigmatism, resulting from the irregular refractive power of the eyeball in children and adults, is the most common refractive error, followed by hyperopia and myopia3. Astigmatism is primarily characterized by the degree of cylinder power (CP).
Although total astigmatism is the result of a combination of corneal astigmatism (CA) and ocular residual astigmatism4 optometrists and parents are more concerned with the change in total astigmatism, expressed as a change in CP when prescribing spectacles for myopia management, especially regarding defocus incorporated multiple segments (DIMS) lens wearers.
Studies have shown that myopia-controlled lenses are the least invasive and are safe for long-term use in many myopia control strategies5. As a myopia control spectacle, DIMS is a minimally invasive therapy to slow down myopia progression and has minimal negative consequences on the quality of life throughout the entire treatment, even at a young age. Many studies have confirmed the role of DIMS lenses in myopia prevention and control6,7,8,9,10,11. However, evidence that shows specific changes in astigmatism during the correction process using DIMS lenses is lacking. The identification of CP progression patterns associated with myopia control in children would facilitate a more comprehensive understanding of myopia control, thereby offering novel insights into the management of myopia.
The aim of this study was to explore the correlation between the parameters associated with the prevention and management of myopia and CP progression in individuals who wear DIMS lenses.The study analyzed the effect of wearing DIMS on changes in spherical equivalent refraction, CYL, and CA. This study divided the participants into two groups: CP unchanged or decrease group(ΔCP ≤ 0) and CP increased group(ΔCP ≥ 0.25D).
This study is the first to investigate the factors related to CP progression in myopia prevention and control in DIMS lens wearers.
Methods
Study design
This was a retrospective observational cohort study.
The study was conducted in accordance with the tenets of the Declaration of Helsinki, and approval was obtained from the Nanjing Tongren Hospital Affiliated to Southeast University School of Medicine (Ethics approval number: 2025-03-004-K001).
Electronic patient records were retrieved in the spring of 2025 for patients prescribed with DIMS and who consented to participate in the establishment of a refractive development profile.
Children and adolescents aged 6–12 years were enrolled and prescribed DIMS lenses (Hoya MiyoSmart, Tokyo, Japan) from July 2021 to August 2023. Cycloplegic refraction and axial length (AL) were assessed at baseline and 12 months as key outcome measures.
The Strengthening the Reporting of Observational Studies in Epidemiology guidelines were used for reporting.
Inclusion and exclusion
Each patient consented to participate in establishing a refractive development profile, and follow-up examinations were completed at 6 and 12 months.
The flow diagram of inclusion and exclusion for participants is presented in Fig. 1.
The DIMS lens was replaced if there was a change of ≥ 0.50 D in the spherical equivalent (SE).
Measurements
AL and refractive status (diopter of sphere (DS); diopter of cylinder (DC); CA, and AL/CR) were measured for all participants.
Refractive development profile were established for all patients. Each participant underwent a slit-lamp examination and intraocular pressure measurement to ensure the safety of cycloplegia.
AL and AL/CR were measured using an IOL Master 500 (Carl Zeiss, Germany) before DIMS lens wear and at each review. The measurements were repeated five times for each eye and averaged, and all AL measurements were performed before cycloplegia.
CA is defined as difference in refractive power between the two principal meridians of the cornea (i.e., the flattest keratometry value K1 and the steepest keratometry value K2) as measured by the IOL MASTER 500.after inducing cycloplegia. Three measurements for each eye were obtained, and the procedure was repeated if the difference between any two records of K1 or K2 was larger than 0.50 diopter (D).
An autorefractor (Topcon RM800, Japan) was used to perform objective refraction after inducing cycloplegia combined with subjective refraction to determine the prescription.
Cycloplegic refraction and quality control
A compound tropicamide ophthalmic solution (0.5% tropicamide and 0.5% phenylephrine eye drops; zhuo bi an, xingqi, China)was administered to each eye, 1–2 drops per instillation, at 5-min intervals, for a total of three instillation. The pupillary light reflex and the diameter of the pupil were evaluated a minimum of 30 min after the final drop of the cycloplegic agent. The absence of light reflection and a pupil diameter greater than 6 mm were considered indicative of complete cycloplegia; otherwise, an additional drop of tropicamide was administered. It was imperative that the participants kept their eyes closed during the procedure to ensure completion. The longest time to complete refraction was 30–40 min after use.
An experienced optometrist conducted comprehensive optometry examination. The standard operating procedures of the refractive clinic have been implemented in our clinic at first visit. The clinician needs to perform retinoscopy, corneal topography, a slit-lamp examination and a retinal examination under small pupil.The treating ophthalmologists diagnosed keratoconus through the identification of typical clinical signs (scissors reflex, prominent corneal nerves, Vogt’s striae, corneal thinning or ectasia) and topographic findings.
All measurements were performed using the same equipment to minimize data discrepancies. A refractive development profile was established to identify and resolve problems related to myopia control. The database was reviewed by optometrists and the data management team to identify any missing or inaccurate information and to make the necessary corrections in a timely manner.
All instruments were calibrated before the examination.
Definitions
Exposure variable
Referring to the ‘Expert Consensus on the Application of Spectacle Related to Myopia Prevention and Control in Myopia Management (2023)’12 a dual classification system was devised to categorize the definitions of myopia prevention and control effect.
The SE was calculated as DS + 0.5 × DC. In terms of ΔSE (SE control effect at 12 months). Group I was defined as those with a good response to myopia control after 12 months of lens wear and significant effect (ΔSE ≤ 0.25 D). Group II displayed an insignificant effect on myopia control (0.25 D < ΔSE < 0.75 D). Group III displayed a poor effect on myopia control (ΔSE ≥ 0.75 D).
In terms of ΔAL (AL control effect at 12 months), Group I displayed a good response to myopia prevention and control effect (ΔAL ≤ 0.20 mm).Group II displayed an effect of 0.20 mm < ΔAL ≤ 0.40 mm. Group III displayed a poor response in AL control (ΔAL > 0.40 mm).
Outcome variable
A change in DC over 1 year was defined as CP progression(ΔCP).children were classified by ΔCP.Clylinder power unchanged or decrease group(ΔCP ≤ 0)and Clylinder power increased group(ΔCP ≥ 0.25D).
Covariates
The children were divided into two groups according to their baseline age, i.e., participants aged 6–9 and 10–12 years.
The children was categorized into a low (− 3.00 D < SE ≤ − 0.50 D), moderate (− 6.00 D < SE ≤ − 3.00 D), or high (SE ≤ − 6.00 D) myopia group13.
Statistical analysis
Owing to the high correlation between the right and left eyes, only data on the right eye were used for analysis in this study, and the Kolmogorov–Smirnov test was used to determine whether the variables were normally distributed. Normally distributed variables were presented as mean (standard deviation), while skewed variables were presented as median (interquartile range, 25–75%). Categorical variables were presented as proportions (%). Comparisons of continuous variables across groups were conducted using the independent samples Student’s t-test or Mann–Whitney U-test, contingent upon the normality of the distribution. Categorical data were compared using the χ2 test, as appropriate.
We used both univariate and multivariate binary logistic regression models to investigate the association between myopia and CP progression. Stratified analyses, interaction tests, and covariate screening were also performed. A multivariate single-imputation method for missing data based on an iterative imputer was implemented using R software (version 4.2.2; R Foundation for Statistical Computing; http://www. Rproject. org), and Free Statistics software (version 2.1; Beijing Free Clinical Medical Technology Co., Ltd.) was used for the analysis. Significance was set at a two-sided P-value < 0.05 for all analyses. Data were analyzed from March to April 2025.
Results
General characteristics
The demographics and characteristics of the wearers at the time of admission and at one year are summarized in Table 1. Of these patients, 87 were male and 92 were female, with a mean age of 9.51 ± 1.48 years. Furthermore, the CP of 24.02% of these participants exceeded 0.25 DC within 1 year.
There were no significant differences in age, sex ratio, baseline SE, AL, or ΔAL between the groups with unchanged or decreased CP and those with increased CP (P > 0.05).
The SE level at admission was − 2.50 (− 3.50, − 1.75) D, and the ΔSE levels were significantly higher in wearers with increased CP than in those with unchanged or decreased CP (P < 0.001).
Multivariate binary logistic regression models
ΔSE levels were predictive of ΔCP.
As shown in Table 2, increased SE levels were associated with an increased risk of CP. This analysis revealed that ΔSE was significantly associated with the incidence of ΔCP (odds ratio (OR) = 1.73,95% CI: 1.32–2.27). Every 0.25 D increase in ΔSE was associated with a 73% increase in the odds of ΔCP in DIMS lens wearers.
Table 2 shows a graded association between ΔSE and ΔCP risk (ODDS ratio for grade 3 ΔSE [ΔR-SE > 0.75 D] vs. grade 1 ΔSE [ΔR-SE ≤ 0.25 D] in the fully adjusted model, 6.32; (95% confidence interval [CI], 2.48 to 16.07).
We also found an association between CA baseline and ΔCP risk (1.17 (1.00–1.36). Every 0.25 D increase in CA baseline was associated with a 17% increase in the odds of ΔCP in DIMS lens wearers.
However, no statistically significant relationship was observed between ΔCP and ΔAL. The crude model showed an OR of 3.17 (95% CI: 0.47–21.13, P = 0.234), indicating no significant association between change in AL and myopia progression. This finding remained non-significant across all adjusted models (P > 0.05), with ORs ranging from 1.65 to 3.17.
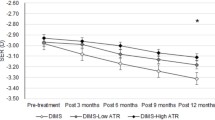
Stratified analysis
Forest plots show ORs in subgroup analyses. A stratified analysis yielded results consistent with those of our multivariate logistic regression analysis concerning the relationship between ΔSE and ΔCP incidence. In contrast, an interaction analysis detected no interactive association between ΔSE and ΔCP (Fig. 2). Also, no interactive association was detected between baseline CA and ΔCP (Fig. 3).
We conducted a subgroup analysis with baseline myopia to explore the influence of different baseline myopia groups on the association between ΔSE and ΔCP. The ORs in the two groups were similar, and no interaction was detected. In addition, the same subgroup findings were observed between baseline CA and ΔCP.
Discussion
Our analysis suggested that baseline CA and ΔSE were significant predictors of CP progression. The magnitude of ΔSE had a positive correlation with CP progression, with larger changes associated with higher odds. In contrast, ΔAL did not appear to be a significant predictor in this data set.
Effective myopia prevention and control strategies include orthokeratology, low-concentration atropine drops, multifocal soft contact lenses, specially designed myopia control frames, and increased outdoor activities. Recently, specially designed frames have been getting more attention14. These lenses are popular because of their convenience, minimal side effects, and lack of age restrictions. The myopia control mechanisms of these lenses include peripheral defocus, peripheral image dispersion design, and peripheral low-contrast design. Clinical trials have shown that newer specially designed spectacle lenses that incorporate multiple segments, lenslets, or diffusion optics have good efficacy7,15,16,17,18,19.
In view of the impressive myopia control results reported, parents and optometrists who manage myopia with specially designed spectacles are concerned about the increase in myopia and the growth of astigmatism.
Our study is a real-world observational study with retrospective inclusion of clinical data. Due to the record keeping requirements of the refractive development archive, participants underwent cycloplegic refraction both before and after one year, with a complete record of the main examination result parameters.
We observed a myopia progression in ΔSE ((IQR) 0.25 (0.00, 0.75) D) and in ΔAL ((IQR) 0.24 (0.11, 0.38)) mm in this study. Determining the treatment effect using AL and SE as criteria resembled that of another real-world study11. In that study, not all results were obtained using cycloplegic refraction. The normalized annual changes in SER and AL in DIMS wearers were significantly smaller than those in SV wearers (DIMS; SER change vs. AL changes; −0.38 ± 0.32 D vs. 0.22 ± 0.16 mm. SV; −0.45 ± 0.41 D vs. 0.29 ± 0.20 mm, P < 0.05). Average axial elongation and myopia progression after 1 year were 0.17 (95% CI 0.13–0.20) mm and − 0.27 (95% CI − 0.36 to − 0.18) D in the DIMS group and 0.30 (95% CI 0.26–0.33) mm and − 0.55 (95% CI − 0.64 to − 0.47) D in the SV group in another recently RCT study16. The small differences in these studies may arise from whether cycloplegic refraction was performed or not.
Previous studies have shown good results in myopia control, but none have examined whether CP changes significantly during myopia control with specially designed myopia control frames. While previous RCT(randomized controlled trial)s for DIMS lens and real studies were only concerned with AL and SE, our study was also concerned with ΔCP based on the needs of parents and optometrists in a real clinical work environment. The results illustrated that 73.18% of the CP remained unchanged or even decreased individually. Parents and optometrists should not be concerned about the progression of subclinical CP during myopia control.
Our findings suggested that CP progression was associated with ΔSE and baseline CA in DIMS lens wearers. Similar results have been seen in young people with myopia20. Stratified analyses showed that the results remained robust across age and sex groups and different initial refractive errors.Age groups as proxies for biologigal, developmental, psychological, and social differences21. In our study, age groups were categorised as 6–9 and 9–12 years old, corresponding to grades 1–3 and grades 4–6, respectively, for Chinese primary school students. In China, the corresponding level of academic learning stress increases for students in grades 4–6. Therefore, through this categorization, we observe whether the occurrence of this type of risk is different under different age factors.
The main predictors of astigmatic change in DIMS spectacle wearers were ΔSE (OR = 1.73,1.32–2.27), and baseline CA (OR = 1.17,1–1.36), suggesting that optometrists should consider such two main correlations when explaining the possible causes of astigmatic change to parents. Additionally, more attention was paid to the use of myopia prevention and control measures with SE as the outcome, especially the combined use of multiple myopia prevention and control methods, to avoid an increase in ΔCP. Previous studies have shown that pharmaceutical interventions22,23 and light therapy24 may be more effective when combined with DIMS. Therefore, parents should be advised to use these in combination. However, attention must be paid to ΔCP if the DIMS lens wearer has high CA during the early baseline examination, even when various myopia prevention and control methods are utilized.
Previous study have shown that DIMS spectacle lenses can bring the AL growth rate of myopic children to the level of physiological AL growth rate9. Notably, we did not observe a significant positive correlation between ΔAL and CP progression. Unlike ΔSE, ΔAL is an important objective and convenient indicator for assessing the eye development patterns of children and adolescents and predicting the occurrence and development of myopia. However, individuals of different ages and varying myopic progress show different AL. Therefore, it is speculated that this may be the reason for the lack of significant correlation between ΔCP and ΔAL in this study.
On the one hand, The increase in children’s AL is relevant to their height increases. The faster their height increases, the faster their AL increases. Guangzhou twin eye study25 also discuss this connection.on the other hand, The principle function of defocus spectacles is to create myopic defocus on the peripheral retina while concurrently providing distance vision correction in the central zone.CP mainly shows the difference between two different meridian parameters. Due to the equivalence of different meridian defocus, it is possible that the CP is not related to defocus.It is hypothesized that CP may not be related to the defocus mechanism, whereas AL is only related to the value of the measured change in data in the middle portion of the retina. Therefore, in our study, It is speculated that ΔCP was not related to ΔAL.
Astigmatism is a refractive error that must be focused on in clinical practice. Total astigmatism results from the combined effect of corneal astigmatism and residual astigmatism of the eye. Optometrists and parents are always more concerned with CP progression in terms of astigmatism assessment, mainly because this relates to the lens form and appearance of edge thickness. Since there is the potential for offsetting or synergistic increases in AL and corneal astigmatism13 change in astigmatism should more often only consider ΔCP. This could also explain why ΔAL was not correlated with ΔCP in our study.
Previous studies have mainly focused on ΔSE and ΔAL as the main endpoints, but our study suggests that ΔCP can also be one of the main research objectives. The effects of myopia prevention and control can be quantitatively and qualitatively calibrated in the astigmatism dimension if better explored.A latest reference also suggests that spectacle lenses with a peripheral defocus design may increase astigmatism in myopic children26. Use of CP progression as a Focused Assessment Indicator.
Conclusion
Parents and optometrists need not be concerned about the progression of subclinical CP in myopia control when using defocus incorporated multiple segments lenses.
In myopia management, corneal astigmatism (CA) measurement should be a routine examination for children and adolescents, especially those with large initial CA.
Follow-up is required for those diagnosed with myopia, and a large change in spherical equivalent (SE) is usually indicative of a large change in CP.
CP progression can be used as a secondary endpoint and observational indicator in studies on the effectiveness of clinically related myopia prevention and control of spectacle lenses.
Limitations
Our study had several limitations. First, this was a single-center retrospective study, and it is thus susceptible to potential selection bias. Secondly, the small sample of CP progression and no control group in singer vision group of this study are key limitations.
Another limitation is the duration of the wear time. Although we found statistically significant effects after just one year of DIMS lens wear. A longer study would enable us to comment on the cumulative effects of the DIMS lens.
There was some confounding bias and selection bias in our study. We recognize it and will improve them in the future through Multi-center and prospective trials.
Data availability
The current study are available from the corresponding author on reasonable request.
References
Holden, B. A. et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042 (2016).
Resnikoff, S. et al. Myopia - a 21st century public health issue. Invest. Ophthalmol. Vis. Sci. 60, Mi–Mii (2019).
Hashemi, H. et al. Global and regional estimates of prevalence of refractive errors: systematic review and meta-analysis. J. Curr. Ophthalmol. 30, 3–22 (2018).
Chen, Z. et al. Ocular residual and corneal astigmatism in a clinical population of high school students. PloS One. 13, e0194513 (2018).
Zhang, X. J. et al. Advances in myopia control strategies for children. Br. J. Ophthalmol. 109, 165–176 (2025).
Lam, C. S. Y. et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br. J. Ophthalmol. 104, 363–368 (2020).
Lam, C. S. Y. et al. Long-term myopia control effect and safety in children wearing DIMS spectacle lenses for 6 years. Sci. Rep. 13, 5475 (2023).
Zhang, H. Y., Lam, C. S. Y., Tang, W. C., Leung, M. & To, C. H. Defocus incorporated multiple segments spectacle lenses changed the relative peripheral refraction: A 2-Year randomized clinical trial. Invest. Ophthalmol. Vis. Sci. 61, 53 (2020).
Graff, B., Lam, C. S. Y., Vlasak, N. & Kaymak, H. Age-matched analysis of axial length growth in myopic children wearing defocus incorporated multiple segments spectacle lenses. Br. J. Ophthalmol. 108, 1060–1066 (2024).
Lembo, A., Schiavetti, I., Serafino, M., Caputo, R. & Nucci, P. Comparison of the performance of myopia control in European children and adolescents with defocus incorporated multiple segments (DIMS) and highly aspherical lenslets (HAL) spectacles. BMJ Paediatr. Open. 8, e003187 (2024).
Chun, R. K. M. et al. Real-world outcomes of defocus incorporated multiple segments lenses on retarding axial elongation in myopic children and adolescents. Front. Med. 11, 1416286 (2025).
Optometry Group of Ophthalmology Branch of Chinese Medical Association, Ophthalmology and Optometry Committee of Ophthalmologist Association of Chinese Doctor Association. Expert consensus on the application of spectacle related to myopia prevention and control in myopia management (2023). Chin. J. Optometry Ophthalmol. Visual Sci. 25, 801–808 (2023).
Wu, Z. et al. Characteristics of full compensation and its association with total astigmatism: A cross-sectional study. Front. Public. Health. 11, 1119654 (2023).
Lupon, M., Nolla, C. & Cardona, G. New designs of spectacle lenses for the control of myopia progression: A scoping review. J. Clin. Med. 13, 1157 (2024).
Sankaridurg, P. et al. IMI 2023 digest. Invest. Ophthalmol. Vis. Sci. 64, 7 (2023).
Li, X., Ma, W., Song, Y., Yap, M. & Liu, L. Comparison of myopic progression and quality of life wearing either DIMs lenses or single-vision myopia correcting spectacles. J. Ophthalmol. 9959251 (2025). (2025).
Bao, J. et al. Spectacle lenses with aspherical lenslets for myopia control vs single-vision spectacle lenses: A randomized clinical trial. JAMA Ophthalmol. 140, 472–478 (2022).
Rappon, J. et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS). Br. J. Ophthalmol. 107, 1709–1715 (2023).
Liu, J. et al. The efficacy of defocus incorporated multiple segments lenses in slowing myopia progression: results from diverse clinical circumstances. Ophthalmology 130, 542–550 (2023).
Manoharan, M. K., Tivari, U. P., Reddy, J. C. & Verkicharla, P. K. Myopia progression in young adults: insights from real-world clinical data. Clin. Exp. Optom. 1–7. https://doi.org/10.1080/08164622.2025.2475200 (2025).
Williams, K. et al. Standard 6: age groups for pediatric trials. Pediatrics 129 (Suppl 3), S153–160 (2012).
Guimarães, S., Barros da Silva, P., Oliveiros, B. & Silva, E. Myopia control: short-term effect of 0.01% Atropine vs. defocus incorporated multiple segment lenses-a retrospective study in European children. Int. Ophthalmol. 43, 3777–3784 (2023).
Huang, Z., Chen, X. F., He, T., Tang, Y. & Du, C. X. Synergistic effects of defocus-incorporated multiple segments and Atropine in slowing the progression of myopia. Sci. Rep. 12, 22311 (2022).
Yang, Y. et al. Synergistic effect of defocus incorporated multiple segment glasses and repeated low level red light therapy against myopia progression. Sci. Rep. 15, 3996 (2025).
Wang, D., Zhao, C., Huang, S., Huang, W. & He, M. Longitudinal relationship between axial length and height in Chinese children: Guangzhou twin eye study. Eye Sci. 30 (1–6), 12 (2015).
Xu, W. et al. The peripheral defocus designed spectacle lenses might increase astigmatism in myopic children. Transl Vis. Sci. Technol. 14, 8 (2025).
Acknowledgements
We thank our colleagues for their assistance during the inspection and data collection process. We also appreciate the support from the Nanjing Tongren Hospital, School of Medicine, Southeast University.This research was funded by Modern Education Technology Project of Jiangsu Province (2022-R-106149).
Funding
Modern Education Technology Project of Jiangsu Province (2022-R-106149).
Author information
Authors and Affiliations
Contributions
Ling Wang and Qing Zhang designed the study and gave guidance in writing. Ling Wang completed the statistical analysis. Ling Wang and Qing Zhang was major contributors in writing the manuscript. Tingting Zhou, Wenli Yu, Jincheng Wang, Ran Li, Qin Chen.Qingbo Que. Xiaomin Gao prepared treatment protocol, monitoring of protocol execution, data collection and data verification. All authors contributed to writing of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
from the institutional review board of Nanjing Tongren Hospital, School of Medicine, Southeast University. (Ethics approval number:2025-03-004-K001)
Consent to participate
The study protocol was explained to the participants, and all participants indicated their understanding of the protocol, and oral consent was obtained. Written informed consent forms were obtained from their parents or legal guardians.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, L., Zhang, Q., Zhou, T. et al. Association between myopia progression and cylinder power progression in defocus incorporated multiple segments lens wearers. Sci Rep 15, 24143 (2025). https://doi.org/10.1038/s41598-025-10099-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10099-7