Abstract
Patients with kyphoscoliosis can present with a variety of chief complaints, including axial back pain, concerns about cosmesis, progressively worsening respiratory function, and even neurological deficits. Correction of severe adult kyphoscoliosis remains challenging due to the severity of the deformity and poor cardiopulmonary function. Direct one-stage corrective surgery can lead to enormous complications and unsatisfactory outcomes when dealing with patients with severe kyphoscoliosis. Preoperative halo-pelvic traction (HPT) has become popular in the management of severe scoliosis. The present study aimed to summarize the efficacy and safety of the staged strategy. Patients with severe kyphoscoliosis complicated by severe pulmonary impairment who underwent staged treatment and met the inclusion and exclusion criteria from Jan 2019 to Jan 2020 were retrospectively reviewed. Data including patient demographics, major coronal curve and kyphosis, pulmonary function test results, distraction time, and complications at different stages of treatment were recorded. Twenty-three patients (16 male and 7 female) with severe kyphoscoliosis and severe pulmonary impairment were included in the study. The mean age of these patients was 26.2 ± 5.7 years. The mean duration of traction before posterior release surgery was 4.0 ± 1.0 months and 4.4 ± 1.0 months after posterior release surgery. Mean follow-up was 40.4 ± 3.9 months. The main curve and kyphosis at admission were 145 ± 11.8° and 149 ± 21.7°, respectively. After HPT, the main curve and kyphosis decreased to 114 ± 12.3° and 124 ± 22.9°, respectively. The FVC and FVC% at admission were 1.44 ± 0.63 L and 39.0 ± 16.19%, respectively. The FVC and FVC% improved significantly after HPT. According to the Nash-Moe classification, the rotation of the apical vertebrae was grade IV in all patients, and the rotation did not improve during the traction. The operative time for posterior release was 266 ± 49 min. The average bleeding of posterior release was 600 ± 242 ml. HPT was maintained after the posterior release surgery. The mean operating time of the posterior correction surgery was 588 ± 53 min, and the mean bleeding was 1605 ± 313 ml. Correction rates were 56.6% and 68.5% in the coronal and sagittal planes, respectively. Staged treatment is an effective and safe strategy to correct severe kyphoscoliosis complicated by severe pulmonary impairment. Preoperative HPT combined with posterior release surgery can significantly reduce spinal deformity and improve pulmonary function. Posterior vertebra column resection (PVCR) is an effective technique for correcting kyphoscoliosis, but it is a technically demanding procedure.
Similar content being viewed by others
Introduction
Severe scoliosis has been defined as more than 100 degree of curvature, and usually accompanied by large kyphosis and severe vertebral rotation1. The term “kyphoscoliosis” is occasionally used to describe severe scoliosis due to the presence of severe kyphosis. Patients with kyphoscoliosis may present with a variety of chief complaints including axial back pain, concerns about cosmesis, progressively worsening respiratory function, and even neurological deficit2,3. The goal of surgery in these patients is to correct the curve and to restore trunk balance while improving the patient’s quality of life and pulmonary function. Despite the advances in surgical techniques to correct spinal deformity, surgical correction of severe kyphoscoliosis remains challenging due to significant risks of mortality and morbidity, neurological injury, and even permanent paralysis3,4,5.
Posterior vertebral column resection (PVCR) is the most common osteotomy to correct severe kyphoscoliosis, with a reported success rate of over 50 degrees correction6. However, PVCR is associated with a number of significant risks, including a prolonged operative time, massive blood loss, neurological deficits, and the potential exacerbation of pulmonary compromise6. Patients with severe kyphoscoliosis, often complicated by severe pulmonary dysfunction, may not tolerate a one-stage corrective surgery such as PVCR due to the high incidence of pulmonary complications and mortality7. Therefore, preoperative distraction, such as halo-pelvic traction (HPT), has been recommended to increase the safety and correction rate of staged surgery for patients with severe kyphoscoliosis.
As initially reported by O’Brien, preoperative HPT has gained wide popularity as a component of a staged strategy for the treatment of severe rigid scoliosis8,9,10,11. The use of preoperative HPT has been demonstrated to enhance patients’ pulmonary and digestive function, reduce the severity of scoliosis, and improve safety and correction rate10. The application of HPT provides an effective, continuous, and adjustable correction force for patients with severe spinal deformity. Patients who undergo treatment with HPT are able to engage in exercise and breathing training, which has the capacity to enhance their overall condition12.
Since 2013, a staged strategy comprising HPT, posterior release surgery, PVCR and instrument fusion has been utilized to correct severe kyphoscoliosis (see process diagram in Fig. 1). The objective of this study is to provide a comprehensive summary of the efficacy and safety of this staged strategy.
Material and methods
Patient data
This retrospective study was approved by the Institutional Review Board of the Third People’s Hospital of Chengdu (IRB approval number: 2022-S-23). All methods were conducted in compliance with the relevant guidelines, regulations, and the Declaration of Helsinki. Informed consent was obtained from all patients. The records of patients with severe kyphoscoliosis who were treated with staged strategy including HPT, posterior release surgery, PVCR and instrument fusion in our hospital from January 2019 to January 2020 were reviewed. The radiographic parameters, clinical data and results of pulmonary function test (PFT) were collected and analyzed. The inclusion criteria were as follows: (1) older than 18-years, (2) severe kyphoscoliosis (Cobb’s angle >120 degree), (3) treated with HPT, posterior release surgery, followed by HPT until the final posterior corrective surgery. The exclusion criteria were as follows: (1) had previous spinal surgery, (2) coexisting respiratory failure, and (3) incomplete data.
HPT protocol
With the patients under general anesthesia and in lateral position, two pins were inserted into the thickest parts from the anterior superior iliac spine to the posterior superior iliac spine on each side. The process was taken in lateral position, pelvic viscera deviate downward due to gravity action, which helps to avoid visceral injuring during pelvic pins placement. The pins do not need to pass through the ilium completely, the important is the pins need to pass the anterior and posterior superior iliac spine medially, then the pins will be stable enough for traction. (Fig. 2). The halo hoop was fitted at the maximum cranial circumference of the skull with 10 skull halo pins implanted in the front and both sides of the skull. The pelvic frame was applied 5 to 7 days after the halo hoop and pelvic pins, and at the same time 4 bars were applied to connect the halo and pelvic hoop. After the frame assembly, traction was started and distraction was performed at a rate of 0.8 cm twice a week for the first 8 weeks. The rate was then reduced to 0.3–0.5 cm twice a week. A standing whole spine film was taken every two months to assess the effect and safety of the traction. If the patient had obvious pain or neurological symptoms (including cranial nerve injury, spinal cord injury, and temporary limb paresthesia or numbness), traction was stopped. Traction was resumed after the symptoms had resolved with treatment, including reduction in traction length, use of medication, and careful observation.
Posterior release surgery
Posterior release surgery was performed in patients in prone position if the large kyphoscoliosis remained with significant widening of the atlantoaxial gap and atlantooccipital gaps (Fig. 3). The HPT device was not removed at the time of surgery. Patients underwent multiple Ponte osteotomies during surgery. During the surgery, somatosensory evoked potentials and motor evoked potentials were used to monitor the status of the spinal cord. Approximately 10 days after the surgery, the patients recovered and traction was resumed.
Posterior correction surgery
Posterior correction surgery was performed in the prone position. Patients underwent PVCR and instrument fusion during surgery. Somatosensory evoked potentials and motor evoked potentials were also used to monitor the status of the spinal cord.
Radiographic parameter and pulmonary function test
Spinal parameters, including main Cobb angle and kyphosis, were assessed on the coronal and sagittal films of the standing whole spine at admission, before posterior release surgery, before final surgical correction, and after final surgery were evaluated. Apical vertebral rotation was measured according to the Nash-Moe classification13. All patients underwent PFT before and after traction PFT. PFT parameters included FVC, and the measured FVC values as a percentage of the predicted values (FVC%). Severity of pulmonary impairment was classified according to the American Thoracic Society’s guidelines, based on the forced vital capacity (FVC), as follows: FVC% >80%, no impairment; FVC% between 65% and 80%, mild impairment; FVC% between 50% and 65%, moderate impairment; and FVC% <50%, severe impairment.
Statistical analysis
Data analysis was performed using SPSS software (version 27.0; IBM). Each variable is presented as the mean and the standard deviation. Pre-HPT and post-HPT values were compared using t-tests. The significance level was set at P <0.05.
Results
Twenty-three patients (16 males and 7 females) with severe kyphoscoliosis and severe pulmonary impairment were included in the study. The etiologic diagnosis included idiopathic scoliosis (n = 18), congenital scoliosis (n = 4), neurofibromatosis with scoliosis (n = 1). The mean age of these patients was 26.2 ± 5.7 years ( range, 18 to 40 years). The mean duration of traction before posterior release surgery was 4.0 ± 1.0 months ( range, 3 to 6 months), while the duration after posterior release surgery was 4.4 ± 1.0 months ( range, 3 to 6 months). The mean follow-up was 40.4 ± 3.9 months (range, 36 to 49 months).
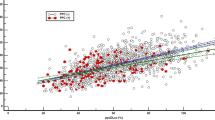
The main curve and kyphosis at admission were 145 ± 11.8° (range from 129° to 172°) and 149 ± 21.7° ( range from 103° to 178°), respectively. The main curve and kyphosis decreased to 114 ± 12.3° and 124 ± 22.9°, respectively, after HPT. The FVC and FVC% on admission were 1.44 ± 0.63 L and 39.0 ± 16.19%, respectively. The FVC and FVC% improved significantly (P<0.05) after HPT ( Table 1). According to the Nash-Moe classification, the rotation of apical vertebrae was Grade IV in all patients, and the rotation did not improve during the traction13. Posterior release surgery included soft tissue release and Ponte osteotomy around the apical vertebra. The operative time of posterior release was 266 ± 49 min. The mean bleeding of posterior release was 600 ± 242 ml. HPT was maintained after posterior release. The main curve, kyphosis, FVC and FVC% continued to improve (Table 1). PVCR was performed in the posterior correction surgery because of the obvious humpback due to the severe rotation of the apical vertebra. The mean operating time for posterior correction surgery was 588 ± 53 min, and the mean blood loss was 1605 ± 313 ml. Finally, the correction rate of was 56.6% and 68.5% on coronal and sagittal plan, respectively. Representative images are shown in Fig. 4.
A 23-year-old male patient with severe kyphoscoliosis and severe pulmonary impairment underwent staged treatment. On admission, the humpback deformity was obvious (a,b), the Cobb angle of main curve was 143° (c), and the angle of kyphosis was 150° (d); after 4 months of HPT, the humpback deformity has been improved (e,f), and the main curve reduced to 102° (g), the kyphosis reduced to 130° (h); another 5 months of HPT after posterior release surgery, the humpback deformity was still obvious (i,j), and the main curve reduced to 62° (g), the kyphosis reduced to 92° (h); after final surgical correction including PVCR and instrument fusion, the humpback deformity has been improved significantly (m,n), and the main curve reduced to 53° (o), the kyphosis reduced to 41° (p).
The incidence of HPT-related complications was approximately 21.7%. There were 2 patients who experienced pelvic pins site infection requiring antibiotic treatment. Three patients experienced new-onset intractable neck or back pain. The pain was resolved with releasing the distraction and analgesics. One patient suffered a superficial incisional infection which was successfully treated with incisional debridement. Six patients developed pleural effusions which were managed with closed drainage (Table 2). There were no neurological complications. Clinical outcome remained good at final follow-up.
Discussion
In our study, the staged treatment was useful in correcting patients with severe kyphoscoliosis and severe pulmonary impairment. All the patients in our study had severe rotation of the apical vertebra, which can cause severe kyphosis. After the first stage of HPT, the pulmonary function improved enormously. Although the main curve and kyphosis decreased significantly, but the curve and kyphosis remained at 114 ± 12.3° and 124 ± 22.9°, respectively. The rotation of the apical vertebra did not change and the humpback was still evident.To achieve a better clinical outcome of deformity correction, the second stage of treatment, defined as posterior release surgery, was performed. Traction was continued after the patients recovered from the posterior release surgery. The kyphoscoliosis continued to decrease during the traction. Finally, in the corrective surgery, PVCR was performed, which significantly decreased the kyphosis, and the hump back improved perfectly. This staged correction strategy of correction for severe kyphoscoliosis was safe and effective. The improvement in pulmonary function increased the tolerance of the patients for complex corrective surgery.
One-stage correction of severe kyphoscoliosis remains a major challenge. This is because severe kyphoscoliosis is usually complicated by poor cardiopulmonary function and digestive function, especially in patients with severe thoracic scoliosis3. Severe scoliosis can reduce respiratory compliance by affecting the thoracic cage and muscle and diaphragm function14. When the Cobb angle was greater than 100 degrees, airway compliance decreased to levels comparable to adult respiratory distress syndrome15. Patients with poor cardiopulmonary function could not tolerate a complex surgery which can result in long operation times, massive blood loss and a high incidence of morbidity and mortality6,7. Song et al.16 reported a total of 84 patients with severe kyphoscoliosis who underwent PVCR, the incidence of major non-neurological complications was 23.0%, including respiratory complications, cardiovascular adverse events or refractory hypotension, malignant hyperthermia, wound infection, and visual deficit.
As direct one-stage orthopedic surgery for severe kyphoscoliosis has been recognized as highly risky and demanding, preoperative HPT has been widely used to increase the safety and correction rate of staged surgery10,17. Qi et al.18 treated thirty patients with severe spinal deformities complicated with respiratory dysfunction with short-term preoperative HPT. The major coronal curve scoliosis and major kyphosis were reduced significantly. And a significantly increased FVC was observed after HPT (p < 0.001), with a significantly improved FVC% in their study. Zhao et al.12 reported the same excellent clinical outcome as well as Qi, while dealing with 18 cases of severe rigid scoliosis and type I respiratory failure treated with preoperative HPT.
Staged treatment including surgical release, preoperative traction and posterior surgical fusion has been reported as an effective strategy to correct severe and rigid scoliosis19,20,21. Hsu et al.19 treated eight patients with severe rigid scoliosis by uniportal video-assisted thoracoscopic surgery for anterior release, and followed by posterior instrumentation and fusion. The mean coronal and sagittal correction rates were 70 ± 19% and 71 ± 23%, respectively. Deng et al.20 introduced a novel posterior surgical release to treat moderate to severe rigid scoliosis, and better clinical results were achieved with posterior intervertebral release combined with posterior column osteotomy than with posterior column osteotomy alone. Yan et al.21 reported that staged posterior surgery with intervening halo-femoral traction is a viable option for severe and rigid scoliosis. And compared with anterior release, posterior release allows superior correction of the major thoracic curves without compromising pulmonary function.
Preoperative traction including HPT and halo-gravity traction (HGT), supplies a safe method for severe scoliosis with severe pulmonary impairment to improve their pulmonary function and reduce the severity of scoliosis before surgical correction10,12,18,22,23,24. Bao et al.24 reported a series cases indicated that the Cobb angel reduced from 131°to 107°after HGT, with FVC significantly increased. Koller et al.25 has reported a significant improvement in pulmonary function after HGT, and the average change of FVC% was 7 ± 8% (n = 24). In our series of cases, we used HPT as preoperative traction to improve their pulmonary function and reduce the degree of scoliosis. We think HPT has advantages over HGT on reducing spinal deformity and improving pulmonary function. The reasons might be the following: (1) the corrective force is much stronger than HGT, the persistent and gradual distraction is more powerful than HGT; (2) the distraction persists 24-hours with freely daily activity, patients can take assist respiratory training including deep respiration and balloon exercise, and physical exercises with the halo pelvic apparatus freely.
In our study posterior release was performed after 4 months of HPT, followed by another period of HPT to achieve more correction. Although the deformity was greatly reduced, the apical vertebral rotation did not improve after the HPT and posterior release surgery(Fig. 4). PVCR was performed in these patients, because of the obvious humpback due to the severe apical vertebra rotation. It has been reported that PVCR is an effective technique to correct severe spinal deformity, because it is a spinal column shortening procedure and it allows correction to be performed in the same session26. Lenke et al.6. reported that their team performed PVCR in 52 cases of kyphoscoliosis to correct the deformity, and the correction rate was 51% and 55% in coronal and sagittal plan, respectively.
The HPT-related complications including, pin infections, cervical stifness and neurological symptoms, were reported with an incidence of 6.6-27.6%10. In our study, five patients suffered HPT-related complications including pin infections and intractable neck or back pain. The complications rate was approximately 21.7%, which remains at a relatively high level. The reason may be that patients in this study had more severe conditions and prolonged traction duration, which could increase the occurrence of traction-related complications. However, no severe complications (such as nerve damage) were observed, demonstrating that the procedure remains relatively safe.
Limitations
This study had several limitations. Firstly, it was a retrospective review with a small sample size. This is because there were rare cases of extremely severe kyphoscoliosis complicated by severe pulmonary impairment in the current medical environment. Second, the images reconstructed by 3D CT of the entire spine will better represent vertebral rotation, but patients lack 3D CT image data for the entire treatment process, so we use radiographs to express it. Thirdly, the duration of the treatment was long and required good patient tolerance and cooperation.
Conclusions
In conclusion, the treatment of severe kyphoscoliosis with severe apical vertebra rotation and severe pulmonary impairment remains a challenge. Staged treatment is an effective and safe strategy to correct severe kyphoscoliosis complicated by severe pulmonary impairment. Preoperative HPT combined with posterior release surgery can significantly reduce spinal deformity and improve pulmonary function. Posterior vertebra column resection (PVCR) is an effective technique for correcting kyphoscoliosis, but it is a technically demanding procedure.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Kandwal, P., Vijayaraghavan, G. P., Nagaraja, U. B. & Jayaswal, A. Severe rigid scoliosis: review of management strategies and role of spinal osteotomies. Asian Spine J. 11 (3), 494–503 (2017).
Sheehan, D. D. & Grayhack, J. Pediatric scoliosis and kyphosis: an overview of diagnosis, management, and surgical treatment. Pediatr. Ann. 46 (12), e472–e480 (2017).
Kempen, D. et al. Pulmonary function in children and adolescents with untreated idiopathic scoliosis: a systematic review with meta-regression analysis. Spine J. 22 (7), 1178–1190 (2022).
Bouchoucha, S. et al. Progressive correction of severe spinal deformities with halo-gravity traction. Acta Orthop. Belg. 77 (4), 529–534 (2011).
Sucato, D. J. Management of severe spinal deformity: scoliosis and kyphosis. Spine (Phila Pa. 1976). 35 (25), 2186–2192 (2010).
Lenke, L. G. et al. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine (Phila Pa. 1976). 38 (2), 119–132 (2013).
Shimizu, T. et al. Preoperative halo-gravity traction for treatment of severe adult kyphosis and scoliosis. Spine Deform. 8 (1), 85–95 (2020).
Wang, Y., Li, C., Liu, L., Li, H. & Yi, X. Presurgical Short-Term Halo-Pelvic traction for severe rigid scoliosis (Cobb Angle > 120°): A 2-Year Follow-up Review of 62 Patients. Spine (Phila Pa. 1976). 46 (2), E95–E104 (2021).
Chen, J. et al. The radiographic, pulmonary, and clinical outcomes of patients with severe rigid spinal deformities treated via halo-pelvic traction. BMC Musculoskelet. Disord. 22 (1), 106 (2021).
Sun, Y., Zhang, Y., Ma, H., Tan, M. & Zhang, Z. Halo-pelvic traction in the treatment of severe scoliosis: a meta-analysis. Eur. Spine J. 32 (3), 874–882 (2023).
Qi, L., Zhao, Y., Xu, B., Li, C. & Wang, Y. Two-stage treatment for severe spinal kyphotic deformity secondary to tuberculosis: halo-pelvic traction followed by a posterior-only approach correction. BMC Musculoskelet. Disord. 23 (1), 991 (2022).
Zhao, D., Wang, F., Hu, Z., Zhong, R. & Liang, Y. Pulmonary and clinical outcomes of patients with severe rigid scoliosis and type I respiratory failure treated with halo-pelvic distraction. J. Orthop. Surg. Res. 18 (1), 710 (2023).
Nash, C. L. Jr & Moe, J. H. A study of vertebral rotation. J. Bone Joint Surg. Am. 51 (2), 223–229 (1969).
Smiljanić, I., Kovac, V. & Cimić, M. Changes in pulmonary functional parameters after surgical treatment of idiopathic scoliosis. Coll. Antropol. 33 (Suppl 2), 145–152 (2009).
Quanjer, P. H. et al. Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, European community for steel and coal. Official statement of the European respiratory society. Eur. Respir J. Suppl. 16, 5–40 (1993).
Song, Z. et al. Posterior vertebral column resection for severe spinal deformity correction: comparison of pediatric, adolescent, and adult groups. Comput. Intell. Neurosci. 2022, 5730856 (2022).
Xia, L., Li, P., Wang, D., Bao, D. & Xu, J. Spinal osteotomy techniques in management of severe pediatric spinal deformity and analysis of postoperative complications. Spine (Phila Pa. 1976). 40 (5), E286–292 (2015).
Qi, L., Xu, B., Li, C. & Wang, Y. Clinical efficacy of short-term pre-operative halo-pelvic traction in the treatment of severe spinal deformities complicated with respiratory dysfunction. BMC Musculoskelet. Disord. 21 (1), 665 (2020).
Hsu, C. M. et al. Pioneering experience of uniportal Video-Assisted thoracoscopic surgery for anterior release of severe thoracic scoliosis. Sci. Rep. 10 (1), 841 (2020).
Deng, Z. et al. The comparison of posterior intervertebral release combined with posterior column osteotomy and posterior column osteotomy alone for the treatment of Moderate-to-Severe rigid scoliosis: A prospective controlled study. Orthop. Surg. 16 (3), 594–603 (2024).
Yan, H. et al. Surgical releasing for severe and rigid scoliosis: posterior approach is better than anterior approach. Clin. Spine Surg. 35 (5), 190–195 (2022).
Liu, D. et al. Efficacy of Halo-Gravity traction in the perioperative treatment of severe scoliosis and kyphosis: A comparison of adolescent and adult patients. World Neurosurg. 166, e70–e76 (2022).
Rinella, A. et al. Perioperative halo-gravity traction in the treatment of severe scoliosis and kyphosis. Spine (Phila Pa. 1976). 30 (4), 475–482 (2005).
Bao, H. et al. Halo-gravity traction combined with assisted ventilation: an effective pre-operative management for severe adult scoliosis complicated with respiratory dysfunction. Eur. Spine J. 25 (8), 2416–2422 (2016).
Koller, H. et al. The impact of halo-gravity traction on curve rigidity and pulmonary function in the treatment of severe and rigid scoliosis and kyphoscoliosis: a clinical study and narrative review of the literature. Eur. Spine J. 21 (3), 514–529 (2012).
Hamzaoglu, A. et al. Posterior vertebral column resection in severe spinal deformities: a total of 102 cases. Spine (Phila Pa. 1976). 36 (5), E340–E344 (2011).
Acknowledgements
We appreciate the contribution of all patients, their families, the investigators and the medical staff. We are grateful to all authors.
Author information
Authors and Affiliations
Contributions
D.Z and Z.Z: Conceptualization, Investigation, Writing - original draft & review. Z.J.H,R.Z and D.X.J: Investigation, Conceptualization, Resources. F.Y.Y, Y.X.L and Y.L.Y: Formal analysis, prepared Figs. 1, 2, 3, and 4. Y.J.L: Conceptualization, Writing - review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study protocol was approved by the ethics committee of the Third People’s Hospital of Chengdu (IRB approval number: 2022-S-23). All methods were conducted in compliance with relevant guidelines, regulations, and the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent has been submitted to this journal.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhao, D., Zhang, Z., Hu, Z. et al. Multistage correction of severe kyphoscoliosis and pulmonary compromise in adults through combined halo-pelvic traction and posterior spinal techniques. Sci Rep 15, 24318 (2025). https://doi.org/10.1038/s41598-025-10307-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-10307-4