Abstract
To assess the 1-month outcomes of visual performance and positional stability of capsule-fixated intraocular lenses (IOLs) in patients with IOL-Bag complex dislocation. We enrolled 36 eyes (34 patients) with IOL-Bag complex dislocation due to pseudoexfoliation syndrome. Patients with intraoperative complications or prior posterior capsule Nd-YAG laser were excluded. Surgical intervention involved creating a superior service keratotomy and using introflective sutures for IOL fixation. Best Corrected Visual acuity (BCVA), endothelial cell counts, and tonometry were assessed at multiple postoperative time points. We also evaluated the mean spherical equivalent (SE), and the residual cylinder and sphere at each follow-up. This study has been successfully registered on ClinicalTrials.gov public (Identifier NCT06423079). The study included 36 eyes, with 22 having a one-piece IOL, 2 with a one-piece IOL plus capsular tension ring, and 12 with a three-piece IOL. Our technique demonstrates a statistically significant improvement in BCVA 1 year after surgery compared to BCVA at the time of IOL dislocation (preoperative BCVA 1.45 ± 0.81 vs 1 year 0.06 ± 0.09 logMAR; p < 0.001). There were no statistically significant differences when comparing the BCVA before the IOL dislocation with the 1-year post-operative BCVA (p > 0.13). No intraocular pressure fluctuations (preoperative IOP 15.0 ± 2.43 vs 1 year IOP 14.69 ± 2.27 p > 0.3), changes in endothelial cell counts (CC) (Preoperative CC: 1812 ± 461 cell/mm2 vs 1 year 1760 ± 329 cell/mm2; p > 0.3), or significant complications were observed. This novel surgical technique may represent a viable, economic, and durable solution to restore dislocations of IOLs accessible from the anterior chamber that respect the cornea and restores visual function without damaging ocular structures.
Similar content being viewed by others
Introduction
Displacement of the bag-IOL complex in patients undergoing cataract surgery is a postoperative complication that is rather infrequent1 in the general population, but it is accentuated in cases of pseudoexfoliation syndrome2, Marfan’s syndrome, homocystinuria, high myopia, post-vitrectomy, and combined cases of the above3. In addition, the increased frequency of this occurrence could be due to longer pseudophakia lifespan, i.e., people live longer, cataract surgery is performed at an early stage of clinical manifestation, and surgery is reserved for the most complicated and complex cases4. Changes in optic tilt and decentration can occur after implantation and affect the optical performance of IOLs5. In fact, the first symptom of this situation is a reduction of visual acuity due to the lower decentration, secondary to gravity, of the intraocular lens. In cases in which this situation is neglected for a long time, the complete dislocation of the bag-IOL complex in the vitreous chamber occurs rather frequently. Various surgical approaches to manage this complication have been proposed, including iris fixation of dislocated lenses6, anterior or posterior iris claw lens7, sutured scleral fixation of the IOL covered by scleral flaps8, glued intraocular lenses9, and removal of the implanted lens10. In many of these approaches, the surgical procedures are burdened by the need for extensive corneal incisions and are associated with inflammation and loss of endothelial cells. Furthermore, externalized sutures may erode and cause more problems, such as suture-induced inflammation, infection, IOL dislocation, or subluxation due to suture degradation or breakage11. Though rarely reported, cases of secondary endophthalmitis have been described12. Due to these challenges, we decided to investigate new approaches to scleral fixation, and we observed that the most auspicious was based on the use of introflective sutures that provided lens stability through a minimally invasive approach. In fact, this new technique was developed to reduce the need for large scleral cuts and with greater respect for corneal endothelial cells.
Materials and methods
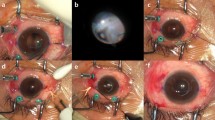
This study was designed as a prospective study to assess the outcomes of a novel surgical technique for scleral fixation of dislocated intraocular lens (IOL)-bag complexes using Siepser’s scleral sliding knots. We enrolled 36 eyes of 34 patients—19 males and 15 females, mean age 66.53 ± 8.12 years old, range 47–80 years—admitted to our clinic between 2020 and 2022 (See Fig. 1 and Table 1).
Thirty-one out of 34 patients were in treatment with topical hypotonizing therapy with one or more active ingredients. All the patients were affected by pseudoexfoliation syndrome, with inferior dislocation of the bag-IOL complex. We excluded patients who underwent intraoperative complications, dislocation in the vitreous chamber of the bag-IOL complex, and those who had already undergone posterior capsule Nd-YAG laser. Of the 36 eyes, 22 had an AAB00 one-piece IOL (Johnson & Johnson Vision), one an AAB00 with capsular tension ring (CTR), one a SA60AT (Alcon) with CTR, and 12 a three-piece AR40E (Johnson & Johnson Vision).
Patients’ best corrected visual acuity (BCVA) documented following cataract surgery (Historical BCVA) was compared with BCVA at the time of dislocation (Pre-operative BCVA) and following IOL-fixation surgery at 1 day, 1 month, 3 months, 6 months, and 1 year. The mean spherical equivalent (SE) and residual cylinder and sphere were also evaluated at each follow-up.
In addition, all patients underwent anterior biomicroscopy with preoperative and postoperative endothelial cell count Perseus Specular Microscope (CSO, Florence, Italy), and tonometry with a Goldman applanation tonometer during the follow-up period. No anticoagulation therapy was suspended before surgery, and informed consent was obtained from all subjects.
The surgery (Figs. 2, 3), performed under retrobulbar anesthesia by a single surgeon, consisted of the creation of a superior service keratotomy (the side of major dislocation of the bag-IOL complex) in correspondence with the terminal quarter of the superior loop and a conjunctival sliding incision superior to it. About 0.3 ccs of IAL-f were injected into the anterior chamber, and a preparatory incision at 180° was realized, identified using the Mendez ring. The rectus needle of a double-armed 10/0 Prolene suture was inserted through the sclera at a distance of 2 mm from the limbus in the conjunctival incision; tilting it forward, the needle, from below the proximal loop, pierced the posterior capsule and was recaptured from the opposite service keratotomy. Figure 4 shows how the conjunctiva is opened at the point where the needles pass through during the procedure and how it spontaneously closes over the suture within a few hours, ensuring complete coverage and minimizing the risk of suture exposure. The other straight needle of the double-armed suture was introduced on the same meridian as the previous one, at 1.5 mm from the limbus, and passed anteriorly to the bag-IOL complex and was thus captured by the opposite service keratotomy. Traction of the Prolene suture was performed until the loop was strongly adherent to the sclera, covered by the sliding conjunctiva. In cases where transconjunctival sutures were used, follow-up observations revealed that the sutures were spontaneously covered by conjunctival tissue within a week, likely due to conjunctival proliferation At this point, needles were removed and a Siepser’s sliding knot was created outside of the eye, then introduced into the anterior chamber and, by applying bimanual tension, tightened until the IOL was well-fixed to the scleral wall. We repeated the procedure for two more Siepser’s knots, then cut the excess from the service keratotomy and observed the iris covering the stumps (Figs. 2, 3). Figure 5 shows the final position of the suture under the conjunctiva, demonstrating complete coverage by conjunctival tissue.
Demonstration of conjunctival behavior during the surgical procedure. The image shows how the conjunctiva is initially opened at the point where the needles pass through and then spontaneously closes over the suture within a few hours postoperatively. This natural closure ensures complete suture coverage and minimizes the risk of suture exposure or associated complications.
In cases where the IOL was sufficiently centered (11 out of 36 eyes), further suturing was not needed; in other cases, the same contralateral procedure was performed (Fig. 2). Finally, residual viscoelastic was removed, hydrosuture of the keratotomies was performed by hydrating the corneal incisions with balanced salt solution (BSS) to promote proper wound sealing, and irrigation of the anterior chamber with cefuroxime sodium solution was carried out.
To further aid in understanding the surgical technique, we have provided supplementary surgical videos, which can be accessed at the following links: Video 1 and Video 2.
Patients were administered acetazolamide 250 mg, one tablet twice a day, for 3 days. A combination of netilmicin and dexamethasone eye drops five times daily for the first seven postoperative days, then three times daily for another 20 days, was prescribed. Any hypotonizing medications were discontinued while acetazolamide was taken.
The study was approved by the institution’s review board (Comitato Etico Campania Centro—Asl Napoli 1, aut. n. 1269/2020) and was conducted in accordance with the tenets of the Helsinki Declaration. Written informed consent was obtained from all subjects before any study procedures were undertaken. This study has been successfully registered on ClinicalTrials.gov public on May 2024 (Identifier NCT06423079).
Results
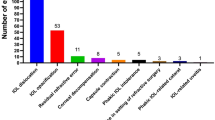
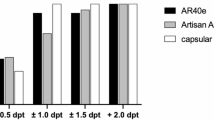
The mean Historical BCVA was 0.05 ± 0.07 logMAR. At the time of IOL dislocation, the mean BCVA was 1.45 ± 0.81 logMAR, and 1 year after surgery, it was 0.06 ± 0.09 logMAR. A statistically significant improvement in BCVA was observed between the pre-operative and 1-year post-operative BCVA (p < 0.001). In contrast, no statistically significant differences were found when comparing Historical BCVA with the 1-year post-operative BCVA (p > 0.13) (See Fig. 6).
The mean SE, as well as the residual cylinder and the residual sphere, showed no statistically significant differences between the historical and 1-year post-operative measurements (respectively p > 0.7; p > 0.59; p > 0.92) (See Figs. 7, 8).
There were no statistically significant changes in endothelial cell counts. The mean value before suspension surgery was 1812 ± 461 cell/mm2, and at the end of the follow-up period, it was 1760 ± 329 cell/mm2 (p > 0.3). No fluctuations in intraocular pressure (p > 0.3) or other complications were observed during the entire follow-up (See Table 2).
Of the 36 eyes, none developed visible intraocular hemorrhage (hypohema/vitreous hemorrhage), but almost all developed moderate conjunctival hemorrhage that was reabsorbed over the first 3 weeks.
One eye with superior and inferior suspension developed another inferior luxation of the IOL 1 week later; during the second operation, knot rupture/dislodgement was observed, and we proceeded to repeat Siepser’s suture, then verified effectiveness.
The other 35 cases had no intraoperative or postoperative complications.
Discussion
In this prospective study, we describe a new technique for scleral fixation in patients with luxation of the bag-IOL complex.
Of the 36 eyes that underwent this procedure, 11 received only hemi-suspension because of the coincidence of the point of fixation chosen for the IOL with the axis of major dislocation (always at 12 o’clock) to achieve good centration with inferior stabilization by the residual zonular fibers. During the 12 months of follow-up, no alteration of IOL position was found in those cases, demonstrating that the inferior zonular fibers, if not stressed further through superior stabilization, do not deteriorate.
The lens stabilization achieved by this technique proved to be 1 year durable, as evidenced by the stability of postoperative refraction and the lack of corneal complications affecting the endothelium and the postoperative astigmatism. Unlike other techniques, no iris lesions or pupillary changes were found. No patient developed uveitis, probably due to the absence of inflammation in the ciliary body. No significant alteration in ocular tone was observed.
Although Prolene sutures are known to degrade over time, our technique minimizes this risk by ensuring the sutures are covered by conjunctival tissue, which prevents direct exposure to light and reduces the chance of degradation13. The literature on this topic primarily discusses exposed sutures, and further research could focus on chemical mechanisms of Prolene degradation in different surgical contexts13. Collaboration with engineering departments to create in vitro models for studying ophthalmic suture degradation would be valuable.
The BCVA gain from preoperative to postoperative appears particularly high because of the severe visual disturbance caused by capsular remnants in the pupillary field and IOL tilting.
We found it much more significant to note that there is a strong correlation between “historical” visus after primary phaco + IOL surgery and after fixation surgery: this relationship indicates that the method restores good visual acuity with minimal stress on ocular structures.
We observed a small mean myopic variation, which was not statistically significant, and we attributed it to a slightly more anterior position of the lens.
In addition, compared with other fixation techniques with scleral flaps, this technique is not subject to the risk of suture exposure, infection, or thinning of the implantation site. Chronic irritation induced by excess of suture, possibly covered by scleral flaps and conjunctiva, is not verifiable in this type of surgery, since the knot is introflective and well-hidden posteriorly to the iris plane. Unlike other solutions using Prolene, which tends to degenerate under exposure to light, this method circumvents that tendency by covering the sutures under the conjunctiva and eyelids.
A major limitation of this technique is that a high level of manual dexterity is required, compared to other scleral suspension techniques; however, it enables a satisfactory and long-lasting refractive result due to the stability and centering of the IOL achieved through the adjustment of the introflex sutures. It also guarantees a saving of endothelial cells because replacement of the IOL is not required, thus making it a rather economical procedure. In addition, the absence of adverse reactions and the stability of postoperative visual acuity 1 year after surgery confirms the potential value of the widespread use of this technique for clinical practice. Our study reports a follow-up period of 1 year, during which no late complications such as IOL dislocation, cystoid macular edema, or suture degradation were observed. While the absence of complications in this timeframe is encouraging, we acknowledge that longer-term studies are necessary to confirm the durability of our technique. Potential complications such as infection, suture degradation, or retinal detachment may arise in scleral fixation procedures over extended periods and should be monitored in future studies.
Data availability
The raw datasets generated and analyzed during the current study have been deposited in the Mendeley Data repository and are publicly available at the following link https://data.mendeley.com/datasets/xbp5nmppg2/1. DOI: https://doi.org/10.17632/xbp5nmppg2.1.
References
Ascaso, F. J., Huerva, V. & Grzybowski, A. Epidemiology, etiology, and prevention of late IOL-capsular bag complex dislocation: Review of the literature. J. Ophthalmol. 2015, 805–706 (2015).
Jehan, F. S., Mamalis, N. & Crandall, A. S. Spontaneous late dislocation of intraocular lens within the capsular bag in pseudoexfoliation patients. Ophthalmology 108(10), 1727–1731 (2001).
Hayashi, K., Hirata, A. & Hayashi, H. Possible predisposing factors for in-the-bag and out-of-the-bag intraocular lens dislocation and outcomes of intraocular lens exchange surgery. Ophthalmology 114(5), 969–975 (2007).
Ton, Y. et al. Management of subluxated capsular bag-fixated intraocular lenses using a capsular anchor. J. Cataract Refract. Surg. 42(5), 653–658 (2016).
Lane, S. et al. Evaluation of intraocular lens mechanical stability. J. Cataract Refract. Surg. 45(4), 501–506 (2019).
Yazdani-Abyaneh, A., Djalilian, A. R. & Fard, M. A. Iris fixation of posterior chamber intraocular lenses. J. Cataract Refract. Surg. 42(12), 1707–1712 (2016).
Liang, I. C. et al. Iris-Claw intraocular lens: Anterior chamber or retropupillary implantation? A systematic review and meta-analysis. Medicina (Kaunas). 57(8), 785 (2021).
Jacob, S., Kumar, D. A. & Rao, N. K. Scleral fixation of intraocular lenses. Curr. Opin. Ophthalmol. 31(1), 50–60 (2020).
Kumar, D. A. et al. Glued intraocular lens in eyes with deficient capsules: retrospective analysis of long-term effects. J. Cataract Refract. Surg. 47(4), 496–503 (2021).
Kristianslund, O. et al. Late in-the-bag intraocular lens dislocation: A randomized clinical trial comparing lens repositioning and lens exchange. Ophthalmology 124(2), 151–159 (2017).
Karadag, R. et al. Sutureless intrascleral fixated intraocular lens implantation. J. Refract. Surg. 32(9), 586–597 (2016).
Armonaite, L., Löfgren, S. & Behndig, A. Iris suture fixation of out-of-the-bag dislocated three-piece intraocular lenses. Acta Ophthalmol. 97(6), 583–588 (2019).
Clayman, H. M. Polypropylene. Ophthalmology 88(9), 959–964. https://doi.org/10.1016/s0161-6420(81)80012-7 (1981).
Author information
Authors and Affiliations
Contributions
Study conception and design: L.D.A., P.G., D.F.; collection and interpretation of data: L.D.A., P.G.; statistical analysis: P.G.; manuscript drafting: L.D.A., P.G.; manuscript editing: L.D.A.; supervision: L.D.A., M.R., C.C.; approval to submit: L.D.A., P.G., D.F., M.R., C.C
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Video S1.
Supplementary Video S2.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Furgiuele, D., Giunta, P., Rinaldi, M. et al. Innovative approach to IOL-bag complex fixation with Siepser’s scleral sliding knots in pseudoexfoliation syndrome. Sci Rep 15, 28522 (2025). https://doi.org/10.1038/s41598-025-10542-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10542-9