Abstract
Thoracoscopic minimally invasive surgery is widely recognized for its efficacy in pain management. Nevertheless, postoperative pain control continues to pose a significant challenge in thoracic surgery. The objective of this study was to investigate the impact of bupivacaine liposomes on postoperative pain management in patients undergoing thoracoscopic lung surgery. All patients who underwent thoracoscopic surgery between March 2024 and October 2024 were retrospectively analyzed. In the patient controlled intravenous analgesia (PCIA) group, a total of 171 patients received thoracoscopic pneumonectomy without intrapleural intercostal nerve block (INB). Conversely, in the bupivacaine liposome (BL) group, another set of 171 patients underwent thoracoscopic minimally invasive surgery with intrapleural intercostal nerve infiltration anesthesia. Pain scores, measured using the Numerical Rating Scale (NRS), were recorded on the day following surgery as well as on days 1, 2, and 3 postoperatively or at the time of discharge. Additionally, we documented both postoperative analgesic consumption and any temporary emergency analgesics administered. Length of stay (LOS) and occurrences of postoperative arrhythmia were compared between the two groups. Among 342 patients undergoing thoracoscopic minimally invasive lung surgery, the LOS in the BL group was nearly half a day shorter (12.24 h) compared to the PCIA group. The consumption of postoperative analgesics in the BL group was significantly lower than that observed in the PCIA group (P = 0.038). Additionally, there were more instances of rescue analgesic use in the PCIA group than in the BL group. In patients undergoing thoracoscopic lung surgery, the administration of intrapleural intercostal nerve block utilizing bupivacaine liposome can alleviate postoperative pain and reduce the need for analgesics following the procedure. This method represents a safe adjunctive treatment for the pain management of postoperative pulmonary surgery.
Similar content being viewed by others
Introduction
Pain control after thoracic surgery is very important1. Compared with traditional thoracotomy, video-assisted thoracoscopic surgery (VATS) completes complex intrathoracic surgery with small incision and has obvious advantages in reducing postoperative pain2. Therefore, the application scope of VATS has been involved in all fields of thoracic surgery3. However, postoperative pain remains a major concern, resulting in shallow breathing and limited coughing, and in some cases, the need to remove the thoracic drainage tube prematurely, increasing the risk of re-intubation4,5. This not only prolongs the length of hospital stay but also significantly impacts both the physical and mental health of patients. Acute postoperative pain poses a barrier to safe and rapid recovery, as it adversely affects lung expansion and respiratory function, impedes physical healing, and increases the risk of respiratory infections1. Furthermore, inadequate management of acute pain may result in chronic post-thoracotomy pain syndrome (PTPS), which can severely diminish long-term quality of life6. Consequently, effective pain management is a critical component of postoperative care for patients undergoing thoracoscopic surgery.
Currently, a variety of treatments have been investigated to alleviate postoperative pain following lung surgery. These include adjunctive therapies utilizing morphine analogues and non-steroidal anti-inflammatory drugs (NSAIDs), as well as patient-controlled analgesia (PCA) and epidural blocks7. PCA represents an innovative approach to analgesic drug delivery8. Based on the patient’s level of pain and overall physical condition, medical staff pre-set the dosage of analgesics. When patients experience discomfort, they can activate the controller to administer the prescribed analgesic medication, thereby achieving effective pain relief. PCA is a widely recognized method for modern pain management and serves as an essential approach for postoperative pain relief. However, its use may be associated with certain side effects, which can include respiratory depression, circulatory depression, nausea and vomiting, abdominal distension, constipation, urinary retention, and other adverse reactions9. Furthermore, individual patients may experience incomplete analgesia due to improper usage of PCA techniques, leading to feelings of doubt or disappointment regarding their pain management. Thoracic epidural block (TEP) has emerged as one of the most effective techniques for managing pain following thoracic surgery10. While TEP is acknowledged as an efficient strategy for pain control in this context, it remains crucial to consider its application carefully to optimize patient outcomes. However, this approach may not be universally effective for all patients and is associated with a higher incidence of hypotension and local anesthetic toxicity, albeit with fewer serious complications such as intraspinal hematoma or epidural abscess11,12. Furthermore, technical challenges may contribute to an increased failure rate, potentially prolonging the duration of surgery13.
Bupivacaine liposome injection represents a novel formulation of sustained-release anesthetic, specifically designed for local anesthetic administration14. In this innovative approach, bupivacaine is encapsulated within polycystic liposomes using a specialized technique. The rupture of individual vesicles does not compromise the overall integrity of the liposomal structure. Due to the variability in rupture times among different vesicles, the release duration of bupivacaine can be significantly prolonged. Consequently, this formulation facilitates slower drug diffusion over an extended period—lasting up to 72 h—thereby providing adequate time for effective local analgesia following surgical procedures15,16. There is limited evidence to suggest that bupivacaine liposomes are superior to traditional local anesthetics for postoperative analgesia in thoracic surgery. Several retrospective studies have indicated that the use of bupivacaine liposomes in minimally invasive thoracic procedures can enhance postoperative pain management, reduce opioid consumption, and shorten hospital stays16,17,18. However, data regarding large-scale outcomes of bupivacaine liposomes in patients undergoing minimally invasive pulmonary resection remain scarce. Furthermore, few studies have incorporated quality assurance measures for intrapleural administration performed under direct visualization.
In this context, the aim of our study was to assess the efficacy of direct vision intercostal injection of bupivacaine liposomes in managing postoperative acute and chronic pain in patients undergoing video-assisted thoracoscopic lung surgery, compared to a self-controlled pain relief pump.
Methods
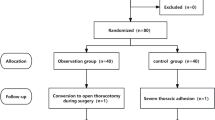
Research design
This study is a retrospective analysis of prospective clinical data. Since 2020, our institution has maintained a consistent influx of thoracic surgeons exhibiting largely uniform departmental practices. The research was conducted in accordance with the Declaration of Helsinki (revised in 2013) and received approval from our Institutional Review Board. Informed consent was obtained from all patients involved in the study. PCA is utilized for pain management in nearly all cases of thoracic surgery, with the exception of a small percentage of patients who report such severe pain that they decline to have an analgesia pump installed. A total of 342 patients (143 males and 199 females) who underwent thoracoscopic minimally invasive pneumonectomy at our institution from March 2024 to October 2024 were included in this study. Patients were categorized into two groups based on the administration of bupivacaine liposomes: the BL group (n = 171) and the PCIA group (n = 171). The inclusion criteria primarily consisted of adults aged between 18 and 80 years who were scheduled for elective video-assisted thoracoscopic single-port or porous lung surgery under bronchial intubation general anesthesia. Exclusion criteria encompassed patients with chronic pain who had been on long-term narcotic medication, individuals with a history of psychiatric disorders such as depression or anxiety, and those with known allergies to medications utilized during the study.
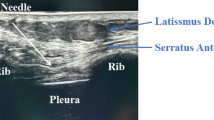
Analgesia and technique
Patients receiving BL are injected by the thoracic surgeon while awaiting frozen pathology results during surgery. This approach not only reduces the overall duration of the surgical procedure but also allows sufficient time for the BL to take effect. Patients in the PCIA group were treated with Patients controlled intravenous analgesia. In the BL group, a total of 266 mg (20 mL) of bupivacaine liposome injection was administered into the thoracic cavity under thoracoscopic guidance. A No. 7 scalp needle was carefully inserted into the thoracic cavity through the operative port to prevent premature release of the multi-capsular liposome due to damage from extrusion. The same volume of solution (approximately 4 mL per gap) was uniformly injected from the third intercostal space to the seventh intercostal space. The size of the liposome is relatively large, which hinders its ability to spread effectively. Consequently, it is seldom absorbed into the systemic circulation following local injection. Following local injection, it is infrequently absorbed into the systemic circulation. These injections result in localized infiltration between the pleural lining and the intercostal nerve. Thoracoscopic visualization confirms the subpleural depth of drug delivery, thereby minimizing the risk of missing anatomical spaces.
Postoperative management
The primary endpoint measured in this study was pain. Perioperative management remained consistent throughout the study period. Our institution did not begin implementing the postoperative Enhanced Recovery After Surgery(ERAS) pathway until the latter half of 2020, ensuring uniformity within our study population in this regard. Upon returning to the ward after surgery, standard protocols were adhered to, which included regular intravenous administration of Flurbiprofen Axetil or intramuscular injections of Tramadol or Cobratide; the majority of these administered medications were flurbiprofen. Take paracetamol and oxycodone tablets regularly to alleviate both short-term and long-term pain, as prescribed by professional nurses. Patients may also be administered a more potent opioid analgesic, Dezocine, primarily following surgical procedures, contingent upon the surgeon’s discretion. Patients are deemed fit for discharge when they can manage their pain with minimal oral opioids, tolerate a regular diet, and exhibit near-normal levels of activities of daily living. Ultimately, the decision regarding discharge preparation rests with the attending physician.
Postoperative pain evaluation
Postoperative pain is routinely assessed by nursing staff using the Numeric Rating Scale (NRS), which is consistently employed across our institution. In this scale, a score of 0 indicates “no pain,” scores ranging from 1 to 3 signify mild pain (which does not interfere with sleep), scores between 4 and 6 represent moderate pain (resulting in shallow sleep), scores from 7 to 9 denote severe pain (leading to significantly disturbed sleep), and a score of 10 reflects extreme pain, characterized as “the pain is intense and uncontrollable.” The initial score was documented upon the patient’s return to thoracic surgery in the Post-Anesthesia Care Unit (PACU). Pain scores were subsequently recorded and compiled at 24, 48, and 72 h post-surgery. It is important to note that some patients who were discharged from the hospital on postoperative day three had their pain scores recorded at the same time point; therefore, these data could be included in the analysis for the 72-hour mark. Both groups received temporary rescue analgesics based on their subjective reports of pain. The medications primarily consist of Flurbiprofen Axetil, Oxycodone-Acetaminophen Tablets, and Tramadol injections. We documented the daily dosage and total dosage of each analgesic administered. Furthermore, we summarized the dosages utilized by each patient on the day following surgery, as well as on the first day post-surgery, the second day post-surgery, and within a 72-hour period after surgery.
Data collection
All data points utilized for analysis were extracted from electronic medical records, specifically through hospital physician system programs or nurse care system medical records. Demographic information was obtained from admission records, while the duration of hospitalization was calculated as the time difference between the date of discharge and the date of admission. LOS was subsequently determined. Specific surgical modalities and types of incisions were sourced from surgical records. Pain scores (NRS) are systematically and reliably documented by nursing staff at our facility. Nurses are instructed to encourage patients to ambulate within 12 h post-surgery and to expectorate sputum in order to promote effective coughing. Additionally, data regarding the administration of all analgesics were extracted from the doctor’s order management records, with a comprehensive tally of oral, intramuscular, or intravenous (IV) medications conducted for subsequent analysis.
Statistical analysis
Two-tailed Fisher’s exact test, Chi-square test, or independent sample t-test were employed for the comparison of categorical variables. The Mann-Whitney U test was utilized for comparing non-normally distributed continuous variables. A multivariate linear regression model was established to evaluate the dependence of hospital length of stay on age, postoperative arrhythmia, and type of operation. The threshold for statistical significance was set at P < 0.05.
Results
Population characteristics
From March 2024 to October 2024, a total of 342 patients were enrolled in the study. Among these, there were 114 cases (33%) of wedge-shaped resection, 105 cases (31%) of segmentectomy, and 123 cases (36%) of lobectomy. Additionally, a total of 171 patients underwent intrapleural injection of bupivacaine liposomes during the procedure. The median age at surgery for the entire cohort was 58 years (range: 19–78 years). Notably, the median age for patients receiving patient-controlled intravenous analgesia was slightly higher at 58 years (range: 25–77 years), compared to those receiving bilateral procedures who had a median age of 56 years (range: 19–78 years) with a statistically significant difference observed (P = 0.016). A total of 328 patients (96%) underwent surgical resection for space-occupying lung disease, while 14 patients were treated for other types of lung diseases. Within the PCIA group, 167 patients underwent pulmonary resection, three patients had bullotomy procedures, and one patient received surgery for pulmonary sequestration. In the BL group, 159 patients (93%) also underwent pulmonary resection. Additionally, seven patients in this group underwent bullotomy, two had bronchodilation surgery, two received resections for pulmonary abscesses, and one patient was treated for a pulmonary aspergillus infection. The demographic, clinical, and surgical characteristics were similar between the two groups (Table 1).
Main result
Pain score
The pain scores of certain patients who were discharged from the hospital on the third day post-surgery may be documented for analysis at 72 h following the surgical procedure. Consequently, all patients fulfilled the criteria for pain score analysis. No significant differences in Numeric Rating Scale (NRS) pain scores were observed between groups on both the day of surgery (P = 0.371) and two days post-surgery (P = 0.764) (Table 1). At 24 h following surgery, patients in the BL group reported a mean pain score of 2.16 (2.16 ± 0.430), compared to a mean score of 2.08 (2.08 ± 0.307) in the PCIA group (P = 0.026). By 72 h after surgery, patients in the BL group exhibited a mean pain score of 1.63(1.63 ± 0.702), while those in the PCIA group reported a mean pain score of 1.36(1.36 ± 0.816) (P < 0.001). One possible explanation for the observed outcomes is that a small quantity of bupivacaine liposomes may not have fully entered the pleural cavity when administered using a #7 scalp needle. Another potential explanation is that the analgesic effect of bupivacaine liposome injection might be somewhat limited to a duration of 72 h.
Chronic use of timing and rescue analgesic medications
The average consumption of regular analgesics in the BL group was found to be lower than that in the PCIA group (6.98 vs. 7.03, P = 0.801). Additionally, the average amount of rescue injection analgesics utilized by the BL group constituted 52.2% of that used by the PCIA group (0.12 vs. 0.23, P = 0.012), with 14 cases in the BL group requiring rescue analgesia compared to 30 cases in the PCIA group; among these, one patient required up to three doses. In comparison to the PCIA group, the average dosage of routine long-term oral analgesics administered post-surgery was lower in the BL group (5.90 vs. 6.04, P = 0.194). Furthermore, the average dosage of oral rescue analgesia for patients in the BL group represented only 55.6% of that observed in the PCIA cohort (0.05 vs. 0.09, P = 0.613), with eight cases from the BL group necessitating rescue analgesia as opposed to ten cases from the PCIA group. Notably, one patient in the latter group necessitated four sessions of oral analgesia.
Both groups were administered similar analgesics
Flurbiprofen ester injection and oxycodone tablets emerged as the most frequently administered analgesics. Notably, all but two patients (0.6%) required at least two non-narcotic analgesics. Among these patients, 303 (88.6%) were treated with only two medications, 34 (9.9%) received three different drugs, and 3 (0.9%) were prescribed all four non-narcotic analgesic adjuncts. There was no significant difference observed between the two groups.
Length of stay
The mean length of stay in the BL group was approximately half a day shorter than that in the PCIA group, measuring 12.24 h (P = 0.122). In multiple linear regression analysis, surgical method [β = 0.242; 95% confidence interval (CI): 0.351–1.357; P < 0.001], postoperative arrhythmia (β = 0.143; 95% CI: 0.059–3.254; P = 0.042), age (β = 0.264; 95% CI: 0.029–0.096; P < 0.001) was independently associated with a longer hospital stay, as detailed in Table 2.
Postoperative complications
Overall, 16 patients (4.7%) developed arrhythmias following surgery: 12 patients (7.0%) in the BL group and 4 patients (2.3%) in the PCIA group. Within the BL cohort, five patients experienced sinus tachycardia, while seven patients exhibited atrial fibrillation with a rapid ventricular rate. In the PCIA cohort, three patients presented with sinus tachycardia and one patient demonstrated atrial fibrillation with a rapid ventricular rate. The classification of arrhythmias is detailed in Table 3.
Discussion
Compared to the traditional surgical field of view, the thoracoscopic surgical field can be enlarged as needed to reveal fine tissue structures with greater clarity and flexibility. This enhanced visualization provides thoracic surgeons with a more intuitive opportunity to observe the intercostal nerves within the chest. During surgical procedures, some degree of tissue damage is unavoidable, which may stimulate the release of pain-inducing substances that act on pain receptors—free nerve endings distributed in the skin, mucous membranes, muscles, and internal organs—resulting in an unpleasant subjective experience19,20. In the rapid recovery phase following pulmonary surgery, we encourage patients to engage in active coughing, facilitate sputum clearance, minimize the risk of lung infections, and enhance postoperative recovery. However, it is important to note that postoperative coughing may lead to alterations in thoracic cavity stability, increased vibration at the surgical incision site, and exacerbation of pain21,22. These factors can adversely affect patients’ sleep quality, resulting in low mood and decreased appetite—conditions that are not conducive to optimal lung recovery post-surgery. Therefore, effective management of postoperative pulmonary pain is crucial for promoting patient outcomes.
Although bupivacaine liposomes have established a significant role in pain management within the realm of thoracic surgery, it remains uncertain whether this novel formulation of bupivacaine is beneficial across all pulmonary procedures in this field. The objective of the present study was to assess the efficacy of bupivacaine liposomes for postoperative pain management in patients undergoing lung surgery via VATS. In our preliminary analysis, results indicated that intercostal local infiltration anesthesia with bupivacaine liposomes effectively reduced the requirement for postoperative analgesics, particularly rescue analgesics, during the first 72 h following surgery. In addition, the study demonstrated an association with fewer early postoperative extubations and shorter LOS. Notably, the mean pain score in the BL group was higher at 72 h post-surgery, which may be explained by the duration of sustained analgesia provided by bupivacaine liposomes—specifically, some portion of the pleural injection is inevitably lost, however, the analgesic effect of bupivacaine liposomes lasts for a duration of 72 h23. Furthermore, there was a higher incidence of postoperative tachycardia observed in the BL group, which can be attributed to the cardiotoxic effects associated with bupivacaine. Our study represents a larger comparative analysis between PCIA and BL following pulmonary resection via VATS. Additionally, it serves as an evaluation of postoperative pain management efficacy across multiple surgical procedures involving various types of incisions.
In recent years, an increasing number of studies have reported on the outcomes of BL administration during or after thoracic surgery. In a study examining pulmonary lobectomy performed via video-assisted thoracoscopic surgery, Liao et al.24, demonstrated that preoperative ultrasound-guided injection of liposomal bupivacaine(LB) at the erector spinalis spinal plane was more effective than traditional bupivacaine hydrochloride in managing postoperative pain. Additionally, in the study conducted by Banks et al.14, intercostal nerve block utilizing bupivacaine liposomes resulted in reduced hospital stays following video-assisted thoracic surgery for lobectomy, along with a notable difference in opioid consumption. Three years later, Singh et al., reported that the direct vision lateral block of the intercostal nerves significantly reduced morphine consumption 48 h post-thoracic surgery when compared to thoracic epidural analgesia17. Additionally, this technique was associated with fewer postoperative complications and a shorter LOS in the hospital. In their study on pneumonectomy performed via video-assisted thoracoscopic surgery, Patel et al., found that intercostal nerve block using liposome bupivacaine resulted in lower opioid usage and a reduced LOS compared to traditional intercostal nerve block utilizing standard bupivacaine25. For intercostal nerve blocks, the advantages of liposomal bupivacaine over standard bupivacaine are particularly significant in the context of robot-assisted thoracic surgery (RATS) and video-assisted thoracic surgery (VATS). In the study conducted by NeMoyer et al.26, involving patients undergoing VATS, LB paravertebral block demonstrated a substantial improvement in postoperative pain management compared to 0.25% bupivacaine epidural (BE) block. Additionally, LB paravertebral block has been shown to provide effective analgesia for patients undergoing thoracotomy. The comparative analysis and examination of LB data across various parameters in these studies further corroborate that liposomal bupivacaine is a more efficacious analgesic agent following pulmonary surgery, thereby reinforcing the consistency of our findings.
In our study, an intriguing finding was that on the day of surgery, as well as on the first and second days post-surgery and at 72 h after surgery, the pain scores in both the BL group and PCIA group exhibited a gradual decrease. Correspondingly, patients’ subjective perception of pain also diminished. Notably, there were differences in pain scores within the PCIA group at 24 h post-surgery. Early activity may contribute to increased discomfort. Another possible explanation is that the BL does not achieve its full therapeutic effect within the first 24 h, whereas PCIA can provide a rapid analgesic effect via intravenous administration. There were notable differences in pain scores observed between 24 h and 72 h post-surgery, indicating that the prolonged analgesic effect of BL may not significantly influence the pain score27. The bupivacaine liposome group demonstrated a shorter mean postoperative hospital stay compared to the PCIA group; however, this difference did not achieve statistical significance. We could not attribute the observed variation in length of stay to improved pain control with bupivacaine liposome, as pain scores were not significantly different between the two groups, with the PCIA group showing a notable advantage. Adequate pain control is merely one criterion that patients must meet prior to discharge, and there are additional factors that may influence discharge timing. Furthermore, patients in the BL group exhibited a lower mean usage of conventional long-term injections and oral analgesics. Additionally, as the number of enrolled cases increased, it was observed that the frequency of pain relief in the BL group decreased from three times per day to two times per day, while no such change occurred in the PCIA group; moreover, there was no significant increase in pain scores for the BL group. One possible explanation for the observed outcomes is that we may underestimate the analgesic effects of bupivacaine liposomes. Notably, our findings indicated that the use of rescue injections and oral analgesics in the BL group post-surgery was significantly lower than that in the PCIA group, with a marked difference in injectable analgesia. Furthermore, compared to the PCIA group, fewer patients in the BL group required early removal of drainage tube due to severe pain associated with drainage tube stimulation. These observations underscore bupivacaine liposomes is a long-acting sustained-release preparations. Utilizing the proprietary DepoFoam technology, bupivacaine is encapsulated within multicystic liposomes. Upon administration, bupivacaine is released only from ruptured vesicles, while the integrity of the overall vesicle structure is maintained. Owing to the varied timing of vesicle rupture, the release duration of bupivacaine is extended, thereby maintaining a safe concentration and providing analgesia for up to 72 h, which significantly surpasses the efficacy duration of current local anesthetics (6–8 h). Additionally, a single injection can ensure prolonged pain relief, eliminating the necessity for supplementary equipment such as catheters and analgesia pumps. This not only streamlines the operational procedures for medical workers but also enhances patient comfort and compliance while reducing equipment-related expenses23,28.
Early postoperative activity has been shown to reduce the risk of venous thromboembolism (VTE), enhance lung function, and decrease pulmonary complications29. This may elucidate the observed reduction in cardiovascular and pulmonary events among patients following pulmonary surgery. Patient-controlled analgesia is an infusion control device utilized by patients themselves. When a patient experiences pain, they can administer a single dose of analgesic medication through this device, thereby achieving effective pain relief. Patient-controlled intravenous analgesia represents a significant advancement in the management of postoperative pulmonary pain due to its ease of use, rapid onset of action, and broad applicability. However, it is important to note that PCIA involves systemic administration of drugs that are associated with considerable side effects; many patients report experiencing nausea, vomiting, dizziness, or urinary retention. These adverse effects can significantly impact the overall hospitalization experience for patients30. Bupivacaine liposomes can be considered to effectively mitigate these adverse reactions. Although the peak blood concentration of bupivacaine liposomes is lower than that of bupivacaine hydrochloride, which may reduce the risk of central nervous system and cardiovascular toxicity to some extent, there remains a potential for postoperative complications31. Our study revealed that, in comparison to the PCIA group, the BL group experienced a higher incidence of postoperative arrhythmias; however, individual patients did not report symptoms such as palpitations or other related manifestations. The symptoms experienced by these patients were completely alleviated following treatment with anti-arrhythmic drugs, and no recurrence was observed within 72 h after the cessation of the drug’s efficacy. There is reason to believe that adverse reactions associated with bupivacaine liposomes are unavoidable, however, arrhythmias did not reappear after the conclusion of drug treatment or its effects, indicating a certain degree of safety. This finding aligns with the hypothesis proposed by Chenung et al.32. Although no statistically significant differences were observed in the specific arrhythmias, there was a noted tendency towards an increased incidence of these events among patients receiving BL. This trend may contribute to a rise in adverse events, which, as demonstrated by multivariate analysis, serves as a surrogate factor for prolonging length of stay.
Our study not only surpasses the size of previous investigations but also specifically examines the application of bupivacaine liposomes in VATS pneumonectomy across various surgical procedures and incisions. Our retrospective analysis yielded findings that align with our initial hypothesis, alongside several unexpected results. Our analysis indicates that, across the board, there are consistent benefits associated with BL compared to PCIA. Interestingly, among patients receiving both PCIA and BL, the BL group did not demonstrate any advantage in postoperative intergroup pain scores. One potential explanation for this finding is that the BL group utilized a long-term, slow-release analgesic mechanism characterized by gradual release, in contrast to the immediate intravenous effects of PCIA. Nevertheless, the trend observed in pain scores remained consistent. It is important to note that the dosages of BL varied between our study and others conducted in this field; such variations could influence some of these findings. Furthermore, it should be acknowledged that optimal dosing may differ from one facility to another.
Limitation
Including our study, the current high degree of subjectivity in pain perception and measurement represents an inherent limitation across all pain research. Several limitations were identified in this study. First, it is an empirical investigation conducted at a single academic institution, which may limit the generalizability of the results. Second, adverse events were recorded solely for arrhythmias, with no follow-up on additional adverse events. Furthermore, this study was not a randomized controlled trial; rather, we included a continuum of patients within each group who met the inclusion criteria. Consequently, as anticipated in observational studies such as ours, there exists some lack of standardization. For instance, nurses’ cautious approach to postoperative pain management may have introduced selection bias. Lastly, various types of injectable analgesics could potentially influence pain scores. As previously mentioned, pain is a highly subjective measure; therefore, we employed a numerical rating scale that is commonly utilized across diverse disciplines nationwide.
Conclusions
In summary, this clinical trial aimed to evaluate the effects of bupivacaine liposomes and patient-controlled analgesia on postoperative pain following thoracoscopic lung surgery. The administration of bupivacaine liposomes under direct visualization during thoracoscopic procedures is straightforward, safe, and reproducible. To a certain extent, the use of bupivacaine liposomes contributes to effective postoperative pain management and reduced length of hospital stay.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- PCIA:
-
Patient controlled intravenous analgesia
- INB:
-
Intercostal nerve block
- BL:
-
Bupivacaine liposome
- NRS:
-
Numerical Rating Scale
- LOS:
-
Length of stay
- VATS:
-
Video-assisted thoracoscopic surgery
- PTPS:
-
Post-thoracotomy pain syndrome
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- PCA:
-
Patient-controlled analgesia
- TEP:
-
Thoracic epidural block
- ERAS:
-
Enhanced Recovery After Surgery
- PACU:
-
Post-Anesthesia Care Unit
- IV:
-
Intravenous
- LB:
-
Liposomal bupivacaine
- RATS:
-
Robot-assisted thoracic surgery
- BE:
-
Bupivacaine epidural
- VTE:
-
Venous thromboembolism
References
Marshall, K. & McLaughlin, K. Pain management in thoracic surgery. Torac. Surg. Clin. 30 (3), 339–346 (2020).
Mangiameli, G., Cioffi, U. & Testori, A. Lung Cancer treatment: from tradition to innovation. Front. Oncol.12, 858242 (2022).
Yim, A. P. C. et al. Place of Video-thoracoscopy in thoracic surgical practice. World J. Surg. 25 (2), 157–161 (2014).
Stamenovic, D. et al. A randomized controlled trial: comparison of 14 and 24 French thoracic drainage after minimally invasive lobectomy – MZ 14–24 study. Heliyon. 9 (12), e22049 (2023).
Hallifax, R. J., Psallidas, I. & Rahman, N. M. Chest drain size: the debate continues. Curr. Pulmonol. Rep. 6 (1), 26–29 (2017).
Miyazaki, T., Doi, R. & Matsumoto, K. Post-thoracotomy pain syndrome in the era of minimally invasive thoracic surgery. J. Thorac. Disease. 16 (5), 3422–3430 (2024).
Maxwell, C. & Nicoara, A. New developments in the treatment of acute pain after thoracic surgery. Curr. Opin. Anaesthesiol. 27 (1), 6–11 (2014).
Grass, J. A. Patient-controlled analgesia. Anesth. Analg. 101 (5 Suppl), S44–S61 (2005).
Palmer, P. P. & Miller, R. D. Current and developing methods of Patient-Controlled analgesia. Anesthesiol. Clin. 28 (4), 587–599 (2010).
Huang, Q. W. et al. A comparison of analgesia after a thoracoscopic lung Cancer operation with a sustained epidural block and a sustained paravertebral block: A randomized controlled study. Adv. Therapy. 37 (9), 4000–4014 (2020).
Daly, D. J. & Myles, P. S. Update on the role of paravertebral blocks for thoracic surgery: are they worth it? Curr. Opin. Anaesthesiol. 22 (1), 38–43 (2009).
Dhole, S. et al. Comparison of continuous thoracic epidural and paravertebral blocks for postoperative analgesia after minimally invasive direct coronary artery bypass surgery. J. Cardiothorac. Vasc. Anesth. 15 (3), 288–292 (2001).
Davies, R. G., Myles, P. S. & Graham, J. M. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural Blockade for thoracotomy—a systematic review and meta-analysis of randomized trials. Br. J. Anaesth. 96 (4), 418–426 (2006).
Banks, K. et al. Intercostal nerve Blockade with liposomal bupivacaine reduces length of stay after video assisted thoracic surgery (VATS) lobectomy. J. Thorac. Disease. 14 (1), 18–25 (2022).
Hu, D. et al. Pharmacokinetic profile of liposome bupivacaine injection following a single administration at the surgical site. Clin. Drug Investig. 33 (2), 109–115 (2012).
Khalil, K. G. et al. Operative intercostal nerve blocks with Long-Acting bupivacaine liposome for pain control after thoracotomy. Ann. Thorac. Surg. 100 (6), 2013–2018 (2015).
Singh, A. et al. Liposomal bupivacaine intercostal block placed under direct vision reduces morphine use in thoracic surgery. J. Thorac. Disease. 16 (2), 1161–1170 (2024).
Hsu, D. S. et al. Reduced opioid utilization and post-operative pain in Asian vs. Caucasian populations after video-assisted thoracoscopic surgery lobectomy with liposomal bupivacaine-based intercostal nerve Blockade. Annals Palliat. Med. 11 (5), 1635–1643 (2022).
Kehlet, H. Postoperative pain, analgesia, and recovery—bedfellows that cannot be ignored. Pain 159 (1), S11–S16 (2018).
Ræder, J. Postoperative pain–underestimated and undertreated. Tidsskr Nor. Laegeforen. 131 (18), 1740. https://doi.org/10.4045/tidsskr.11.0849 (2011). English, Norwegian.
Chen, S. et al. Optimal dose of ropivacaine for relieving cough-pain after video-assisted thoracoscopic lobectomy by single intrapleural injection: A randomized, double-blind, controlled study. Int. J. Surg. 69, 132–138 (2019).
Perttunen, K., Nilsson, E. & Kalso, E. I.v. Diclofenac and ketorolac for pain after thoracoscopic surgery. Br. J. Anaesth. 82 (2), 221–227 (1999).
Viscusi, E. R. et al. The pharmacokinetics and pharmacodynamics of liposome bupivacaine administered via a single epidural injection to healthy volunteers. Reg. Anesth. Pain Med. 37 (6), 616–622 (2012).
Liao, D. et al. Effect of liposomal bupivacaine for preoperative erector spinae plane block on postoperative pain following video-assisted thoracoscopic lung surgery: a protocol for a multicenter, randomized, double-blind, clinical trial. Front. Med. 11, 1359878 (2024).
Patel, K. M. et al. Liposomal bupivacaine versus bupivacaine for intercostal nerve blocks in thoracic surgery: A retrospective analysis. Pain Physician. 23 (3), E251–E258 (2020).
NeMoyer, R. E. et al. Paravertebral nerve block with liposomal bupivacaine for pain control following Video-Assisted thoracoscopic surgery and thoracotomy. J. Surg. Res. 246, 19–25 (2020).
Kendall, M. C., Castro Alves, L. J. & De Oliveira, G. Liposome Bupivacaine Compared to Plain Local Anesthetics to Reduce Postsurgical Pain: An Updated Meta-Analysis of Randomized Controlled Trials. Pain Research and Treatment, 2018: pp. 1–10. (2018).
Manna, S. et al. Probing the mechanism of bupivacaine drug release from multivesicular liposomes. J. Controlled Release. 294, 279–287 (2019).
Yin, H. Enhanced recovery after surgery (ERAS) in postoperative lung Cancer patients: A novel perioperative strategy for preventing venous thromboembolism and improving quality of life. Tohoku J. Exp. Med. 262 (3), 201–209 (2024).
Doty, R. et al. Evaluation of a Proximal Block Site and the Use of Nerve-Stimulator-Guided Needle Placement for Posterior Tibial Nerve Block103p. 1300–1305 (Anesthesia & Analgesia, 2006). 5.
Rice, D., Heil, J. W. & Biernat, L. Pharmacokinetic profile and tolerability of liposomal bupivacaine following a repeated dose via local subcutaneous infiltration in healthy volunteers. Clin. Drug Investig. 37 (3), 249–257 (2017).
Cheung, B. M. Y. et al. Pharmacokinetics and safety of liposomal bupivacaine after local infiltration in healthy Chinese adults: a phase 1 study. BMC Anesthesiol. 21 (1), 197 (2021).
Acknowledgements
We acknowledge the Guangxi Natural Science Foundation(2023GXNSFAA026129),Guangxi Medical and Health Appropriate Technology Development and Promotion Application Project(S2024013), Nanning Qingxiu District Science and Technology Project (S2020029)for support.
Author information
Authors and Affiliations
Contributions
JQ Qin, ZN Lei, and RL Li proposed the direction of this research and completed the article. JQ Qin , YF Zhou completed the post-article revision and table layout. YL Zhong was responsible for the analysis of the results and overall article revision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Human ethics and consent to participate
The studies involving humans were approved by The People’s Hospital of Guangxi Zhuang Autonomous Region. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qin, J., Lei, Z., Li, R. et al. Intrapleural injection of bupivacaine liposome for pain management after thoracoscopic surgery. Sci Rep 15, 24433 (2025). https://doi.org/10.1038/s41598-025-10616-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10616-8