Abstract
No study has investigated the incidence or risk factors of recurrent lumbar disc herniation (rLDH) after unilateral biportal endoscopic discectomy (UBED) in patients with lumbar disc herniation. Therefore, we aimed to construct and verify a nomogram that can predict the risk of recurrence after UBED for lumbar disc herniation and therefore help clinicians understand the recurrence rate of lumbar disc herniation before surgery and formulate corresponding interventions to improve the prognosis of patients. This is a retrospective study based on the data from all patients who underwent UBED for lumbar disc herniation in Zhoukou Central Hospital between September 2021 and December 2023. The risk factors for recurrence after UBED in patients with lumbar disc herniation were determined via stepwise regression. Finally, a nomogram was constructed on the basis of these selected variables to predict the recurrence rate of lumbar disc herniation after UBED. The receiver operating characteristic (ROC) curves and the areas under the curve (AUC) were used to evaluate the discrimination ability of the model. In addition, calibration curve and Hosmer-Lemeshow goodness of fit test (HL test) were constructed to evaluate the consistency between the predicted risk and the actual risk. Decision curve analysis (DCA) was used to evaluate the clinical net income and the clinical applicability of the nomogram. The stepwise regression analysis showed that Age, disease duration, segmental range of motion (SROM), global range of motion (GROM), Modic I changes, and Modic II changes are risk factors for the recurrence of lumbar disc herniation after UBED. The AUCs of the model on the training set and the validation set are 0.763 (95% CI: 0.648–0.879) and 0.721 (95% CI: 0.573–0.868), respectively. The results showed that our nomogram has better recognition ability. The calibration plot and goodness-of-fit test results indicated that the prediction results of our model were consistent with the actual results (training set HL test, P = 0.087; HL test of the validation set, P = 0.193). DCA showed that our model has good net clinical benefit. Our study revealed that age, disease duration, SROM, GROM, and Modic changes are risk factors for the recurrence of lumbar disc herniation after UBED. On the basis of these variables, we successfully constructed and verified a nomogram that can predict the risk of recurrence of lumbar disc herniation after UBED, which can help clinicians predict the possibility of rLDH in patients in advance and develop interventions to reduce the risk of recurrence.
Similar content being viewed by others
Introduction
Lumbar disc herniation can cause low back pain, lower limb radiation pain, numbness, weakness and other symptoms and is the most common spinal degenerative disease1,2,3. According to statistics, the incidence of natural absorption of herniated intervertebral discs is 66%, so most patients experience satisfactory results through conservative treatment, but few patients need surgical intervention after conservative treatment fails4. In recent years, with the continuous promotion of the concept of minimally invasive surgery, the unilateral biportal endoscopic technique (UBE) has been widely used to treat lumbar disc herniation. Many studies have revealed that the clinical efficacy of UBE for the treatment of lumbar disc herniation is comparable to that of percutaneous endoscopic lumbar discectomy (PELD), but UBE is advantageous owing to its association with a low recurrence rate, low residual rate of the nucleus pulposus and good visual field5,6,7.
The common complications of lumbar disc herniation surgery mainly include dural tear, recurrence, infection, epidural hematoma and deep vein thrombosis, among which recurrence and dural tear are the most common8,9,10. Lumbar disc herniation is the most common cause of reoperation. According to different studies, the recurrence rate of postoperative lumbar disc herniation is between 3.6% and 12.5%11,12,13. Recurrent lumbar disc herniation not only results in more pain but also high medical care costs for patients who experience this complication14. Therefore, it is necessary to take relevant measures to prevent the recurrence of lumbar disc herniation.
We found that no study has investigated the incidence or risk factors of recurrent lumbar disc herniation (rLDH) after unilateral biportal endoscopic discectomy (UBED) in patients with lumbar disc herniation. Therefore, we aimed to construct and verify a nomogram that can predict the risk of recurrence after UBED for lumbar disc herniation and therefore help clinicians understand the recurrence rate of lumbar disc herniation before surgery and formulate corresponding interventions to improve the prognosis of patients.
Materials and methods
Study population
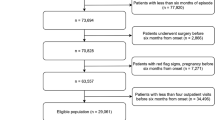
The clinical data of all patients who underwent UBED for lumbar disc herniation in Zhoukou Central Hospital between September 2021 and December 2023 were retrospectively analyzed in this study. All patients included in the study were followed up for 6 months. The study was approved by the Ethics Committee of Zhoukou Central Hospital, and all procedures were conducted following the principles outlined in the Declaration of Helsinki. After screening, a total of 274 patients were included in the study. All patients were operated on by senior spinal surgeons in our team. The inclusion criteria were as follows: (1) patients who were diagnosed with single-segment lumbar disc herniation according to clinical manifestations and imaging features; (2) patients whose conservative treatment for at least 6 weeks was ineffective or severely affected the daily life of patients; and (3) patients whose surgical method was UBED. The exclusion criteria were as follows: (1) had lumbar spondylolisthesis classified as II° or higher, or lumbar instability; (2) had a lumbar fracture, tumor, infection, or ankylosing spondylitis; (3) a history of lumbar spine surgery; (4) no lumbar spine anteroposterior or lateral radiographs, dynamic radiographs or lumbar MRI examination.
Clinical data
The demographic and surgery-related information of the patients included age, sex, smoking history, drinking history, hypertension status, diabetes status, osteoporosis status, admission method, education level, body mass index (BMI), obesity status, disease duration, and surgical segment. Imaging indicators included the segmental range of motion (SROM), global range of motion (GROM), disc height index (DHI), degree of spondylolisthesis, grade of disc degeneration, Modic changes, degree of disc herniation, direction of disc herniation, degree of fat infiltration on the affected side, and type of disc herniation.
Clinically, rLDH is characterized by symptoms of lumbar disc herniation and compression at the same level as before surgery, with no restriction on duration15,16,17,18. According to the postoperative lumbar MRI examination and clinical symptoms, we judged whether the patient experienced recurrence after UBED.
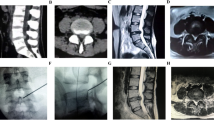
Global lordosis (GL) was defined as the Cobb angle between the upper endplates of L1 and S1. Segmental lordosis (SL) was defined as the Cobb angle between the upper and lower vertebral endplates of the operating segment. The GROM was the absolute value of the result obtained by subtracting the GL angle at buckling from the GL angle during overextension. The SROM is the absolute value of the result obtained by subtracting the SL angle at buckling from the SL angle at hyperextension19. The measurement diagram is shown in Fig. 1.
The DHI is the ratio of the sum of the anterior and posterior heights of the intervertebral disc to the sum of the depths of the upper and lower intervertebral discs during standing, and the formula is DHI = (C + D)/(A + B)20,21. The measurement diagram is shown in Fig. 2. The degree of intervertebral disc herniation was measured on the cross section of the maximum level of intervertebral disc herniation using MRI, and the internal line of the facet joint was defined as the transverse line between the medial edges of the left and right facet joints. The degree of intervertebral disc herniation was divided into 3 levels according to the internal line of the facet joint22.
Severe lumbar disc degeneration is closely related to fat infiltration of the multifidus and erector spinae23. Axial and sagittal T2W images of the corresponding segments of the patients were collected, and transverse images of the center of the herniated disc were selected. The total fat infiltration ratio of the multifidus and erector spinae on the affected side was measured using ImageJ software24. The degree of fat infiltration in muscle was evaluated using a semiquantitative grading system, that is, a simplified 4-level system: Grade 1 indicates that the muscle state is normal, and the fat infiltration area accounts for 10% of the muscle cross-sectional area; Grade 2 is mild fat infiltration, and the area of fat infiltration accounts for 10-30% of the cross-sectional area of muscle; Grade 3 is moderate fat infiltration, fat infiltration area accounted for 30-50% of the muscle cross-sectional area; Grade 4 is severe fat immersion, and the area of fat infiltration accounted for more than 50% of the cross-sectional area of muscle25. The measurement diagram is shown in Fig. 3.
Surgical procedure
All cases underwent general anesthesia and prone position surgery. Under the guidance of C-arm fluoroscopy, the surgical segment and incision surface point were determined. The initial target point of the mirror instrument is located at the junction of spinous process and vertebral lamina, which is used as a horizontal marker line, and then a vertical marker line is drawn along the inner edge of pedicle. 1.5 cm above and below the intersection point of the two lines are the body surface points of the observation incision and the operation incision respectively. 9–10 mm incision and 6–7 mm incision were made at the body surface positioning points of operation incision and observation incision respectively. Cut the skin, subcutaneous tissue and deep fascia in turn, insert a step-by-step expansion catheter and use a stripper to gradually expand the soft tissue to the bone surface of the lamina for blunt separation to establish a channel. An arthroscopic system is placed in the observation channel and saline is used for flushing. Generally, the vertical distance between the saline bag and the patient’s back is maintained at 50–70 cm, so as to keep the water flow unobstructed and make the field of vision clear.
In the working channel, the 90 degree radiofrequency coagulator is used to clean the soft tissue on the surface of the intervertebral space and stop bleeding, and then the lower edge of the upper lamina, the upper edge of the lower lamina, the ligamentum flavum, the root of spinous process and the inner edge of the articular process are exposed. Grind the lower edge of the lamina and the inner edge of the inferior articular process with a grinding drill, and continue to bite the lamina proximally with a lamina rongeur until the proximal end of the ligamentum flavum stops. Decompression from the upper edge of the ipsilateral lower vertebral lamina to the end of ligamentum flavum. Expose the inner edge of Corner and superior articular process, use reverse laminectomy rongeur to decompress the same Corner, remove the inner edge of superior articular process and release the outer edge of ligamentum flavum. Stripping the ligamentum flavum to expose the dural sac, nerve root and intervertebral disc. UBE retractor was used to retract the dural sac, and bipolar radiofrequency cutter was used to stop bleeding and remove adhesion on the surface of herniated intervertebral disc. Using nucleus pulposus forceps to remove the protruding nucleus pulposus tissue, loosen the nerve roots, explore the free nucleus pulposus tissue existing in the annulus fibrosus break and clean it up, and finally use 90 degree radiofrequency coagulator to shrink the annulus fibrosus break. Use bipolar radio frequency cutter to stop bleeding. After stopping bleeding completely, place a drainage tube on the surface of the vertebral lamina, fix the drainage tube, suture the incision, and cover the site with sterile dressing. The nucleus pulposus tissue resected during the operation is shown in the Fig. 9.
Statistical analysis
The Shapiro-Wilk test was used to determine whether the continuous variables were normally distributed. Continuous variables with a normal distribution are described as means ± standard deviations (x ± s), and the independent sample t test was used for comparisons between groups. If a continuous variable was not normally distributed, it was described as the median and interquartile range, and Wilcoxon’ s rank-sum test was selected for comparison between two groups. Categorical variables are expressed as frequencies/percentages, and the chi-square test or Fisher’ s exact test was used for comparisons between different groups.
The risk factors for recurrence after UBED in patients with lumbar disc herniation were determined via stepwise regression. In this study, we prioritized logistic regression over other potential models such as Lasso regression and random forest due to its clinical interpretability and suitability for our sample size. Logistic regression provides clear and interpretable coefficients that are essential for communicating risk factors to clinicians. Additionally, our relatively small sample size limits the performance of more complex models like random forest, which are more prone to overfitting. Logistic regression has been widely used and validated in similar clinical studies, ensuring consistency and comparability with previous research. The results are expressed as odds ratios (ORs) and 95% confidence intervals (CIs). Finally, a nomogram was constructed on the basis of these selected variables to predict the recurrence rate of lumbar disc herniation after UBED. ROC curves and AUCs were used to evaluate the discrimination ability of the model. The higher the AUC value, the greater the degree of discrimination of the model. In addition, we constructed a calibration curve and performed an HL test to evaluate the consistency between the predicted risk and the actual risk. DCA was used to evaluate the clinical net income and the clinical applicability of the nomogram. All the statistical analyses were performed using R software (version 4.2.2). A two-sided P value < 0.05 was considered indicative of statistical significance.
Results
Baseline characteristics of the patients
A total of 274 patients with single-segment lumbar disc herniation who underwent UBED surgery were included in this study. The overall characteristics are shown in Table 1. The patients were randomly divided into a training set (N = 191) and a validation set (N = 83) according to a ratio of 7:3. A total of 29 patients experienced recurrence after surgery, accounting for 10.6%, 19 of whom in the training set (9.95%) and 10 of whom in the validation set (12.0%). There was no significant difference in the recurrence rate between the training set and the validation set (P > 0.05).
Risk factor screening and nomogram development
Stepwise regression was used to determine the risk factors for the recurrence of lumbar disc herniation after UBED. The regression results are shown in Table 2. Age, disease duration, SROM, GROM, Modic I changes, and Modic II changes are risk factors for the recurrence of lumbar disc herniation after UBED, and Modic II changes are independent risk factors for recurrence. Age (OR: 1.03, 95% CI: 1.00–1.07), SROM (OR: 1.12, 95% CI: 0.99–1.28), Modic I (OR: 4.12, 95% CI: 0.79–17.45), and Modic II changes (OR: 3.67, 95% CI: 1.54–8.92) were positively correlated with the recurrence of lumbar disc herniation after UBED. The disease duration (OR: 0.99, 95% CI: 0.98–1.00) and GROM (OR: 0.96, 95% CI: 0.92–1.00) were negatively correlated with the recurrence of lumbar disc herniation after UBED. On the basis of the results of multivariate regression analysis, we constructed a nomogram to predict the recurrence of lumbar disc herniation after UBED (Fig. 4) and constructed a network-based prognostic calculator to facilitate the calculation of recurrence probability (Fig. 5, https://xingzhibin.shinyapps.io/DynNomapp/).
Verification of the nomogram
The AUCs of the model on the training set and the validation set are 0.763 (95% CI: 0.648–0.879) and 0.721 (95% CI: 0.573–0.868), respectively (Fig. 6). The results showed that our nomogram has better recognition ability. The calibration plot and goodness-of-fit test results indicated that the prediction results of our model were consistent with the actual results (training set HL test, P = 0.087; HL test of the validation set, P = 0.193) (Fig. 7). Finally, we plotted the DCA curve to illustrate the clinical applicability of the nomogram, where the x-axis represents the threshold probability of recurrence after UBED, and the y-axis represents the clinical net benefit of stratifying patient risk. As shown in the Fig. 8, our model has good net clinical benefit.
Discussion
To our knowledge, no scholars have developed nor validated a nomogram to predict the risk of recurrence of lumbar disc herniation after UBED. Our study fills this gap. In this study, the recurrence rate of lumbar disc herniation after UBED was 10.6%. Previous studies have shown that the recurrence rate of lumbar disc herniation after percutaneous endoscopic lumbar discectomy is 9.1%26. One study compared the efficacy of the unilateral biportal endoscopic technique and the unilateral transforaminal endoscopic technique in the treatment of severe lumbar disc herniation. The UBE group was significantly superior to the unilateral transforaminal endoscopic group in terms of the postoperative nucleus pulposus residual rate and postoperative recurrence rate6. After analysis, we considered that the reasons for the relatively high recurrence rate of lumbar disc herniation after UBED in this study are as follows. First, some patients were excluded from the study because of our inability to obtain imaging data due to preoperative lumbar magnetic resonance imaging in other hospitals, resulting in a reduction in sample size. Second, we found that most of the patients who experienced recurrence after UBED experienced recurrence in the early stage after the operation, and the lack of surgeon skill may have led to a higher recurrence rate (Fig. 9).
By integrating potential risk factors, nomograms have been proven to be intuitive and easy-to-use clinical personalized risk assessment tools that are widely used in medical research and clinical practice27. Our study revealed that age, disease course, SROM, GROM, and Modic changes were risk factors for the recurrence of lumbar disc herniation after UBED. On the basis of these results, we constructed a nomogram to predict the risk of recurrence of lumbar disc herniation after UBED and verified the validity of the nomogram using ROC curves, AUCs, calibration curves, HL tests, DCA curves and other indicators.
There is controversy about the relationship between age and the recurrence of lumbar disc herniation. In this study, age was positively correlated with the recurrence of lumbar disc herniation after UBED (OR: 1.03, 95% CI: 1.00–1.07). The older the patient is, the higher the risk of recurrence. This may be because with increasing age, the repair ability of the annulus fibrosus weakens, and the nucleus pulposus can easily protrude from the rupture site of the annulus fibrosus. A meta-analysis of the risk factors for the recurrence of lumbar disc herniation after percutaneous endoscopic lumbar discectomy revealed that postoperative recurrence of lumbar disc herniation was significantly associated with advanced age, which is consistent with our findings28. Another study on the relationship between age and the incidence and duration of recurrence after microdiscectomy revealed that age had no effect on the incidence of recurrence of lumbar disc herniation29. The reason for these inconsistent results may be that there are differences in the age distribution of the study population. Studies have shown that the risk of postoperative recurrence of lumbar disc herniation is higher in patients older than 60 years of age than in patients younger than 60 years of age30.
The symptoms of low back pain caused by lumbar disc herniation are related mainly to lumbar disc degeneration31. Lumbar disc herniation changes the original direction of stress transmission of the lumbar spine to a some extent, exacerbating degeneration of the intervertebral disc. In the late stage, pathological changes such as intervertebral space stenosis and osteophyte formation at the upper and lower edges of the vertebral body may occur. It has been reported that osteophyte formation is an adaptive process that reduces lumbar instability32. Owing to the increasing degree of disc degeneration, the lumbar spine becomes increasingly unstable as a result of frequent movement and finally enters the rigidity stage, which is characterized by increased stability33. The study revealed that the lumbar segment with grade III and grade IV disc degeneration showed greater range of motion; however, the disc space collapsed, and osteophyte formation in grade V stabilized the motion segment34. Our study revealed that a long course of disease can reduce the risk of recurrence after lumbar disc herniation, which may be related to osteophyte formation caused by severe degeneration. Studies have shown that early disc degeneration may make patients prone to recurrence of lumbar disc herniation, but more severe degeneration may reduce segmental motion and reduce the risk of recurrence35.
This study revealed that excessive lumbar segmental range of motion (SROM) can easily lead to the recurrence of lumbar disc herniation after UBED, which is consistent with the results of previous research36. Excessive range of motion of the lumbar spine has been reported to be related to lumbar instability. At present, the diagnosis of lumbar instability is mainly based on manifestations of lumbar hyperextension and flexion on X-ray films, but there is still no consensus on the imaging criteria for the diagnosis of lumbar instability. White and Panjabi described lumbar instability as follows: a sagittal translation distance of the vertebral body relative to the lower vertebral body greater than 4.5 mm; a sagittal activity range of L1/L2, L2/L3, and L3/L4 greater than 15°; sagittal activity of L4/L5 greater than 20°; and sagittal activity of L5/S1 greater than 25°37. Some scholars also believe that the critical values of the segmental sagittal activity angle and translation distance for evaluating lumbar instability are 10° and 4 mm, respectively38. The critical value of lumbar translation motion reported by Dvorak et al. was 3 mm39. In conclusion, the boundary between normal and abnormal lumbar motion is difficult to determine. The sagittal range of motion is reported to be up to 25° in young healthy volunteers40. Finally, we classified lumbar instability as lumbar hyperextension and flexion on X-ray films showing intervertebral displacement greater than 3 mm or an angle change greater than 20°. In this study, the patient’s SROM was 8.31°± 3.76°. In addition, studies have shown that when the SROM is greater than 10°, the recurrence rate after microlumbar discectomy is 26.5%, whereas when the SROM is less than 10°, the recurrence rate is 4.1%41. Kong et al. also confirmed that patients with lumbar intervertebral disc extrusion are more likely to have lumbar instability than patients with lumbar disc herniation42. Therefore, we need to pay more attention to patients with greater SROM.
A review of the literature revealed that no research has focused on the relationship between the global range of motion (GROM) and the recurrence of lumbar disc herniation. In this study, the lumbar range of motion of patients with lumbar disc herniation was 34.1° ± 13.4°, and unlike the SROM, the GROM was negatively correlated with the recurrence of lumbar disc herniation. This seems to be inconsistent with our understanding. The possible reasons for this result are as follows: First, patients may have protective spasms of muscles due to fear of low back pain, which in turn reduces the overall range of motion of the lumbar spine. Some patients even need to use painkillers to prior to the acquisition of lumbar dynamic radiographs. Therefore, a decrease in the GROM of the lumbar spine may manifest as low back pain in patients; second, the reduced global range of motion (GROM) of the lumbar spine implies diminished flexibility. During daily activities and movements, this reduction may alter the movement patterns of the lumbar spine, causing stress to become more concentrated on specific intervertebral disc segments. The intervertebral discs in these segments are subjected to prolonged excessive pressure, which can readily lead to further damage of the annulus fibrosus and consequently increase the risk of recurrence.
To date, the pathogenesis of Modic changes has not been clarified. There are two main theories for its etiology. One hypothesis is that low-toxicity anaerobic bacteria enter the injured intervertebral disc, leading to occult discitis. The most common bacteria are Propionibacterium acnes43,44,45. Another view is that after the formation of the embryonic intervertebral disc, the nucleus pulposus no longer has any contact with the systemic circulation and is therefore isolated from white blood cells, whereas an injured intervertebral disc exposes the nucleus pulposus to the immune system, which in turn leads to an autoimmune response46,47,48. These two hypotheses are based on structural damage to the intervertebral disc, such as disc herniation or endplate injury. The final occurrence of Modic type I or Modic type II changes may depend on the intensity and duration of inflammatory stimulation and the composition and metabolic status of the vertebral bone marrow49. In our study, Modic type I (OR: 4.12, 95% CI: 0.79–17.45) and Modic type II (OR: 3.67, 95% CI: 1.54–8.92) changes were positively correlated with the recurrence of lumbar disc herniation, and Modic type II changes were independent risk factors for the recurrence of lumbar disc herniation (P = 0.003). Previous studies have confirmed that patients with Modic changes are more likely to experience postoperative recurrence of lumbar disc herniation50,51,52.
We provided some recovery suggestions for patients after UBED and discussed how to reduce the risk of recurrence of lumbar disc herniation after surgery. First of all, patients should stay in bed in the early postoperative period (1 to 3 days after surgery) and avoid strenuous exercise. Ankle pump exercise can be properly performed to prevent deep venous thrombosis of both lower limbs. In the middle of the postoperative period (3 days to 6 weeks after surgery), the patient can wear a waist brace to get out of bed, but it is necessary to avoid bending and twisting. In addition, patients can exercise their back muscles properly and avoid sitting and standing for a long time. Within 6 weeks to 3 months after surgery, patients need to strengthen the back muscle exercise, can gradually return to normal life and work, but need to avoid heavy physical labor and bad posture. Patients with a higher risk of postoperative recurrence predicted by our model can appropriately reduce the resection range of the facet joint according to the specific conditions during the operation. Postoperative bed rest as far as possible, appropriate back muscle exercise, avoid heavy physical labor and bad posture can reduce the risk of postoperative recurrence.
In addition, we illustrated how the nomogram can be integrated into clinical decision-making processes. To facilitate clinicians’prediction, we developed a web-based calculator at https://xingzhibin.shinyapps.io/DynNomapp/. Dynamic Nomogram is displayed on the left side of the page. We only need to adjust the patient ‘s age, disease duration, SROM, GROM, and Modic changes on the scale, and then click the’Predict’button, the patient ‘s postoperative recurrence rate of lumbar disc herniation will be displayed.However, our research also has several limitations. First, this study is a single-center retrospective study with only internal validation results, so external validation of data from different medical institutions is needed. Second, owing to the lack of preoperative data, some patients were excluded from the study, resulting in a small sample size, which may have caused bias in the reporting results. In addition, we identified only 24 influencing factors that may be related to the recurrence of lumbar disc herniation. There may be other variables that affect the results. For example, the degree of resection of the lumbar intervertebral disc and the range of decompression of the facet joint may be related to postoperative recurrence. In the future, more samples and variables may need to be collected to study the factors affecting the occurrence of rLDH.
Conclusion
Our study revealed that age, disease duration, SROM, GROM, and Modic changes are risk factors for the recurrence of lumbar disc herniation after UBED. On the basis of these variables, we successfully constructed and verified a nomogram that can predict the risk of recurrence of lumbar disc herniation after UBED, which can help clinicians predict the possibility of rLDH in patients in advance and develop interventions to reduce the risk of recurrence.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Benzakour, T. et al. Current concepts for lumbar disc herniation [J]. Int. Orthop. 43 (4), 841–851 (2019).
Kreiner, D. S. et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy [J]. Spine J. 14 (1), 180–191 (2014).
Zhang, A. S. et al. Lumbar disc herniation: diagnosis and management [J]. Am. J. Med. 136 (7), 645–651 (2023).
Zhong, M. et al. Incidence of spontaneous resorption of lumbar disc herniation: A Meta-Analysis [J]. Pain Physician. 20 (1), E45–E52 (2017).
Jiang, H. W. et al. Unilateral biportal endoscopic discectomy versus percutaneous endoscopic lumbar discectomy in the treatment of lumbar disc herniation: a retrospective study [J]. J. Orthop. Surg, Res. 17 (1), 30 (2022).
Yuan, C. H., Wen, B. J. & Lin, H. K. Clinical Analysis of Minimally Invasive Percutaneous Treatment of Severe Lumbar Disc Herniation with UBE Two-Channel Endoscopy and Foraminal Single-Channel Endoscopy Technique [J]. Oxidative Medicine and Cellular Longevity, 2022: 9264852. (2022).
Zuo, R. J. et al. The clinical efficacy of biportal endoscopy is comparable to that of uniportal endoscopy via the interlaminar approach for the treatment of L5/S1 lumbar disc herniation [J]. Front. Surg. 9, 1014033 (2022).
Cheng, J. W. et al. Reoperation after lumbar disc surgery in two hundred and seven patients [J]. Int. Orthop. 37 (8), 1511–1517 (2013).
Lin, G. X. et al. A systematic review of unilateral biportal endoscopic spinal surgery: preliminary clinical results and complications [J]. World Neurosurg. 125, 425–432 (2019).
Nubukpo-Guménu, A. A. et al. Endospine surgery complications in lumbar herniated disc [J]. World Neurosurg. 119, E78–E79 (2018).
Choi, K. C. et al. Unsuccessful percutaneous endoscopic lumbar discectomy: A Single-Center experience of 10 228 cases [J]. Neurosurgery 76 (4), 372–380 (2015).
Sigmundsson, F. G., Joelson, A. & Strömqvist, F. Additional operations after surgery for lumbar disc prolapse indications, type of surgery, and long-term follow-up of primary operations performed from 2007 to 2008 [J]. Bone Joint J. 104B (5), 627–632 (2022).
Yin, S. et al. Prevalence of recurrent herniation following percutaneous endoscopic lumbar discectomy: A Meta-Analysis [J]. Pain Physician. 21 (4), 337–350 (2018).
Ambrossi, G. L. et al. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis [J]. Neurosurgery 65 (3), 574–578 (2009).
Swartz, K. R. & Trost, G. R. Recurrent lumbar disc herniation [J]. NeuroSurg. Focus. 15 (3), E10 (2003).
Cunha, M. et al. Long-term outcome of Redo discectomy for recurrent lumbar disc herniations [J]. Eur. Spine J. 32 (2), 534–541 (2023).
Jang, I-T. et al. Comparison of percutaneous endoscopic lumbar diskectomy and open lumbar microdiskectomy for recurrent lumbar disk herniation [J]. J. Neurol. Surg. Part. A: Cent. Eur. Neurosurg. 79 (06), 447–452 (2017).
Wang, Y. et al. Surgical strategy and outcomes of full endoscopic lumbar discectomy for recurrent lumbar disk herniation following a previous full endoscopic lumbar discectomy [J]. Orthop. Surg. 15 (10), 2602–2611 (2023).
Cho, H. S. et al. Radiological outcomes of unilateral laminotomy for bilateral decompression in lumbar spinal stenosis with and without discectomy [J]. World Neurosurg. 175, E1307–E1314 (2023).
Akeda, K. et al. Risk factors for lumbar intervertebral disc height narrowing: a population-based longitudinal study in the elderly [J]. BMC Musculoskelet. Disord. 16, 344 (2015).
Chen, X. L. et al. Radiographic evaluation of lumbar intervertebral disc height index: an intra and inter-rater agreement and reliability study [J]. J. Clin. Neurosci. 103, 153–162 (2022).
Mysliwiec, L. W. et al. MSU classification for herniated lumbar discs on MRI: toward developing objective criteria for surgical selection [J]. Eur. Spine J. 19 (7), 1087–1093 (2010).
Özcan-Eksi, E. E., Eksi, M. S. & Akçal, M. A. Severe lumbar intervertebral disc degeneration is associated with modic changes and fatty infiltration in the paraspinal muscles at all lumbar levels, except for L1-L2: A Cross-Sectional analysis of 50 symptomatic women and 50 Age-Matched symptomatic men [J]. World Neurosurg. 122, E1069–E1077 (2019).
Zhao, X. et al. The morphological characteristics of paraspinal muscles in young patients with unilateral neurological symptoms of lumbar disc herniation [J]. BMC Musculoskelet. Disord. 23 (1), 994 (2022).
Wen, G., Hou, W. M. & Xu, G. W. Enhanced grading methods for lumbar paraspinal fat infiltration and its prognostic value in predicting lumbar disc herniation [J]. J. Orthop. Surg, Res. 18 (1), 752 (2023).
He, H. et al. Development and validation of a nomogram to predict the risk of lumbar disk reherniation within 2 years after percutaneous endoscopic lumbar discectomy [J]. World Neurosurg. 172, E349–E356 (2023).
Li, H. J. et al. The nomogram model predicting overall survival and guiding clinical decision in patients with glioblastoma based on the SEER database [J]. Front. Oncol. 10, 1051 (2020).
Luo, M. J. et al. Risk factors for lumbar disc herniation recurrence after percutaneous endoscopic lumbar discectomy: a meta-analysis of 58 cohort studies [J]. Neurosurg. Rev. 46 (1), 159 (2023).
Siccoli, A., Schröder, M. L. & Staartjes, V. E. Association of age with incidence and timing of recurrence after microdiscectomy for lumbar disc herniation [J]. Eur. Spine J. 30 (4), 893–898 (2021).
Li, H. L. et al. Factors related to the postoperative recurrence of lumbar disc herniation treated by percutaneous transforaminal endoscopy: A meta-analysis [J]. Front. Surg. 9, 1049779 (2023).
Takatalo, J. et al. Does lumbar disc degeneration on magnetic resonance imaging associate with low back symptom severity in young Finnish adults?? [J]. Spine 36 (25), 2180–2189 (2011).
Al-Rawahi, M. et al. Mechanical function of vertebral body osteophytes, as revealed by experiments on cadaveric spines [J]. Spine 36 (10), 770–777 (2011).
Lao, L. F. et al. Effect of disc degeneration on lumbar segmental mobility analyzed by kinetic magnetic resonance imaging [J]. Spine 40 (5), 316–322 (2015).
Tanaka, N. et al. The relationship between disc degeneration and flexibility of the lumbar spine [J]. Spine Journal: Official J. North. Am. Spine Soc. 1 (1), 47–56 (2001).
Brooks, M. et al. Radiological predictors of recurrent lumbar disc herniation: a systematic review and meta-analysis [J]. J. Neurosurgery-Spine. 34 (3), 481–491 (2021).
Shin, E. H. et al. Risk factors for recurrent lumbar disc herniation after discectomy [J]. Int. Orthop. 43 (4), 963–967 (2019).
Sengupta, D. K. Clinical biomechanics of the spine [J]. Spine 42 (7), S3–S3 (2017).
Dupuis, P. R. et al. Radiologic diagnosis of degenerative lumbar spinal instability [J]. Spine 10 (3), 262–276 (1985).
Dvorak, J. et al. Functional radiographic diagnosis of the lumbar spine. Flexion-extension Lateral Bending [J] Spine. 16 (5), 562–571 (1991).
Hayes, M. A. et al. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals [J]. Spine 14 (3), 327–331 (1989).
Kim, K. T., Park, S. W. & Kim, Y. B. Disc height and segmental motion as risk factors for recurrent lumbar disc herniation [J]. Spine 34 (24), 2674–2678 (2009).
Kong, M. H. et al. Lumbar segmental mobility according to the grade of the disc, the facet joint, the muscle, and the ligament pathology by using kinetic magnetic resonance imaging [J]. Spine 34 (23), 2537–2544 (2009).
Albert, H. B. et al. Modic changes, possible causes and relation to low back pain [J]. Med. Hypotheses. 70 (2), 361–368 (2008).
Stirling, A. et al. Association between sciatica and Propionibacterium acnes [J]. Lancet 357 (9273), 2024–2025 (2001).
Urquhart, D. M. et al. Could low grade bacterial infection contribute to low back pain? A systematic review [J]. BMC Med. 13, 13 (2015).
Geiss, A. et al. Autologous nucleus pulposus primes T cells to develop into Interleukin-4-Producing effector cells: an experimental study on the autoimmune properties of nucleus pulposus [J]. J. Orthop. Res. 27 (1), 97–103 (2009).
Ma, X. L. et al. Possible role of autoimmune reaction in modic type I changes [J]. Med. Hypotheses. 76 (5), 692–694 (2011).
Virri, J. et al. Comparison of the prevalence of inflammatory cells in subtypes of disc herniations and associations with straight leg Raising [J]. Spine 26 (21), 2311–2315 (2001).
Dudli, S. et al. Pathobiology of modic changes [J]. Eur. Spine J. 25 (11), 3723–3734 (2016).
Hao, L. et al. Recurrent disc herniation following percutaneous endoscopic lumbar discectomy preferentially occurs when modic changes are present [J]. J. Orthop. Surg, Res. 15 (1), 176 (2020).
Jiang, L. et al. Analysis of risk factors for post-operative recurrence after percutaneous endoscopic lumbar discectomy in patients with lumbar disc herniation: a meta-analysis [J]. J. Orthop. Surg, Res. 18 (1), 935 (2023).
Shan, Z. M. et al. Machine learning prediction model and risk factor analysis of reoperation in recurrent lumbar disc herniation patients after percutaneous endoscopic lumbar discectomy [J]. Global Spine J. 14 (8), 2240-2251 (2023).
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
ZbX, YpS, and HyG contributed to conception and design; ZbX, LlC contributed to data analysis and interpretation; ZbX contributed to drafting the manuscript for intellectual content; RhZ and MmZ contributed to revision of the manuscript. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The requirement for informed consent was waived by the Ethics Committee of Zhoukou Central Hospital due to the retrospective design of our study. The study was approved by the Ethics Committee of Zhoukou Central Hospital.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xing, Z., Guo, H., Song, Y. et al. Development and validation of a nomogram for predicting postoperative recurrent lumbar disc herniation after unilateral biportal endoscopic discectomy. Sci Rep 15, 26336 (2025). https://doi.org/10.1038/s41598-025-10943-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-10943-w