Abstract
Health behaviors affect life expectancy, but whether disease is present can greatly impact both the individual and society. How health behavior is reflected in the utilization of health care services is yet to be investigated to support the impact of prevention efforts. Based on data from 57,053 middle-aged individuals from the Danish Diet, Cancer and Health cohort, a health score including baseline smoking status, sport activity, alcohol consumption, diet, and waist circumference was constructed as a simple measure of general health behavior. During 20 years of follow-up, healthy life expectancy among men and women aged 65 years at baseline, was 0.83 [0.74 to 0.92] and 0.86 [0.77 to 0.94] years longer on average, respectively, per one point increment in the health score. Life expectancy with disease was shorter among men (-0.18 [-0.26 to -0.09]) and women (-0.37 [-0.45 to -0.29]) with higher health scores. Among individuals with the highest scores, major chronic disease diagnosis was postponed for more than 7 years. There were fewer disability years, especially with multimorbidity, (men: -1.6 years; women: -3.3 years), and there was a clear inverse association between health score and days of hospitalization looking 20 years ahead.
Similar content being viewed by others
Introduction
With the continuous increase in the global proportion of elderly, it is crucial to focus on prevention strategies aimed at benefitting the quality of life of the individual while simultaneously addressing the mounting healthcare challenges that lie ahead. Clearly, evidence supports an association between lifestyle and risk of cardiovascular1, metabolic2,3, neurogenerative4 and respiratory diseases5,6, as well as their co-existence7,8. Less well known is the association between lifestyle and healthy aging, defined as an absence of major chronic diseases. In the current study, we use the term disease-related healthy aging, well aware that absence of disease is only one aspect of aging.
Non-communicable diseases are the main contributors to prolonged disability and early death worldwide. In 2019, ischemic heart disease, stroke, dementia, chronic obstructive pulmonary disease (COPD), and cancers of the lung and colorectum were the leading causes of death in Scandinavia, the UK, and US. Ischemic heart disease, dementia, COPD, lung cancer, and diabetes mellitus also constituted the major contributors to prolonged disability9. Multimorbidity, the co-existence of two or more chronic conditions, places substantial pressure on healthcare economies through more intensive utilization of healthcare resources10. The increased burden on hospitalizations11 constitutes one of the most costly types of health care utilization.
In Western populations, differences in disease-free life expectancy of up to 10 years have been observed with avoidance of smoking, physical inactivity, overweight, and unhealthy dietary and alcohol habits12,13,14,15,16,17. Although smoking is the single risk factor with the strongest association with loss of healthy life, ranking the remaining risk factors is relevant for prioritizing prevention strategies. By exploiting high-quality registry data, the current study investigated the association between a composite health score of common health behaviors and life expectancy with and without morbidity, as well as multimorbidity. Furthermore, associations between the health score and hospitalization load over a 20-year follow-up period from 1997 to 2018 are reported. The current results are expected to encourage health economic calculations aimed at prioritizing and tailoring prevention strategies for optimized health care in favor of both the individual and society.
Methods
The population-based “Diet, Cancer and Health” cohort includes data from 57,053 men and women aged between 50 and 64 years at their enrollment in the cohort in 1993–199718. The databank based on this cohort includes information concerning dietary habits and lifestyle obtained from self-administered questionnaires and anthropometric measurements performed by trained staff at enrollment. For the current study, we defined baseline as 1 July 1997, when the last person was enrolled in the cohort, and we included those who were alive and free of relevant diagnoses at baseline. Thus, the age range at baseline was 50 to 69 years. Follow-up was until death, emigration, or 31 December 2018, whichever came first. Establishment of the cohort was approved by the Regional Health Research Ethics Committees for the Capital Region of Denmark ((KF) 01–345/93) and by the Danish Data Protection Agency. All methods were carried out in accordance with relevant guidelines and regulations and all participants gave written informed consent.
Assessment of relevant diagnoses
Linkage with national registries was possible for all cohort members using the Danish ID number. We defined disease-related healthy aging as an absence of all cancers (ICD-10 codes: C00-C97, except C44), type 2 diabetes (E11), ischemic heart disease (I20-I25), cerebrovascular disease (I60-I64), asthma (J45), COPD (J44), and dementia (F00-F03). The specific registries are presented in the Appendix.
Exposure assessment—health behaviors
A health score was derived based on five health behaviors: smoking status, sport activity, alcohol consumption, diet, and waist circumference. The health score ranged from 0 to 9 points, with 9 points representing the healthiest behavior, hence the presumed lowest risk. Smoking status was scored as never (2 points), former (1 point), or current (0 point).
Sport activity was assessed by questions covering average weekly leisure time spent on activities such as jogging, football, and swimming during summer and winter. Activities included in this category were presumed to be of moderate to high intensity. Sport activity for a minimum of 30 min/week during the past year was considered to reflect a regular physical activity level (1 point), whereas less was considered low activity (0 point).
Both alcohol intake and dietary habits were derived from a validated food frequency questionnaire19. Alcohol consumption was estimated from intake of beer, wine, and liquor to calculate the total amount of alcohol per day (1 unit = 12 g) and scored according to former sex-specific Danish recommendations (applicable in 2010 to 2022).
Alcohol consumption was scored as maximum 7 units/week for women and 14 units/week for men as healthy intake (2 points), 7–14 or 14–21 units/week, respectively, as moderately high intake (1 point), and > 14 or > 21 units/week, respectively, for high intake (0 point). Diet was included based on four dietary recommendations with good evidence to support a role in lifestyle-related disease: whole grains, fruit and vegetables20, red meat, and processed meat21. For each item, questions containing relevant foods were summed. Whole-grain foods included oatmeal and muesli, rye bread, and whole-grain bread with the recommendation of 75 g/day (per 10 MJ/day). All fruits and vegetables (fresh and frozen), excluding juices, were summed for a daily average with the recommendation of a minimum 600 g/day regardless of the proportion between the two. For red meat (beef, pork, and lamb), the recommendation is to limit intake to a maximum 350 g/week. For processed meat, the current recommendation is to avoid or limit intake as much as possible, which we defined to be a maximum 10 g/d. The diet score ranged from 0 to 4 points, with a score of 4 given for adherence to all four recommendations: a high intake of whole grains (≥ 75 g/d/10 MJ/d) and fruits and vegetables (≥ 600 g/d), and low intake of red (≤ 350 g/w) and processed meats (≤ 10 g/d). For the composite health score, diet was grouped by scores of 3–4 (2 points), 1–2 (1 point), and 0 (0 point). Waist circumference was grouped according to official Europid sex-specific cut-off values22 for low, moderate, and high risk of cardio-metabolic diseases. Waist circumference was scored based on ≤ 80 cm or ≤ 94 cm (2 points), 80–88 cm or 94–102 cm (1 point), and > 88 cm or > 102 cm (0 point) for women and men, respectively.
Socioeconomic covariates
Information about cohabitation status and education was obtained from Statistics Denmark. Cohabitation status was based on information from household registries and defined as living with a partner or not. Education level was grouped into short (i.e., primary school), middle (i.e., high school, primary school longer than the 7 years mandatory for Danish citizens born before 1958, vocational education, supplementary education), and long (i.e., higher education).
Data on hospitalization
We quantified the hospital load by duration of hospital stays during follow-up. We identified patient entries for which the patient was physically at the hospital from among all of the patient entries in the DNPR according to algorithms from the final report of the Expert Technician Commission on Hospitalizations as appointed by the Danish National Health Data Authority23. See the Appendix for details on the definition of duration of hospital stay.
Statistical analysis
Using an illness-death multistate model, we assessed the expected length of stay in the stages “healthy” and “with disease”. The association between the health score and length of stay was estimated using pseudo-observations as the outcome in linear regression models with generalized estimating equations with a robust variance estimator24. We assumed a linear effect of health score on the length of stay, and the reported estimates are the difference in mean length of stay per 1 point increment in health score, or the per 9-point increment corresponding to comparing the most extreme health scores. As a secondary analysis, we substituted the simple health score with the five health parameters, mutually adjusted, into one multistate model. We also extended the multistate model to multimorbidity with the stages “with one disease” and “with two or more diseases” due to few observations of multimorbidity with three and more diagnoses. To illustrate these results, we predicted the mean length of stay within 20 years from baseline for 0–9 health score points for an “average person” with fixed values of cohabitation (together) and education level (middle). We carried out sensitivity analyses of the length of stay with modified versions of the simple health score by grouping the diet score into 2–4 (2 points), 1 (1 point), and 0 (0 point), allowing for a less strict definition of a healthy diet, and by substituting waist circumference with body mass index (BMI).
Hereafter, expected length of stay is referred to as life expectancy, which should be interpreted as the residual restricted life expectancy, as the length of stay in a state was defined as the time spent in a state from baseline (hence, “residual”) until 20 years after (hence, “restricted”).
The association between the health score and the continuous variable days of hospitalization per year was analyzed by a quasi-Poisson model with a log-link. The effect of the health score was modeled as a third-degree polynomial due to nonlinearity; thus, the estimates do not have an easy interpretation and were not reported. Instead, we reported the predicted mean number of days of hospitalization per year calculated from the predicted median number of days obtained from the model due to the log-link for 0–9 health score points at fixed values of the adjustment variables. We conducted sensitivity analyses of the days of hospitalization using bed days instead of calendar days.
To formally assess the linearity assumptions regarding the effect of health score and age, we visually inspected the Pearson residuals and evaluated the significance of both log and second- and third-order terms using likelihood ratio tests.
The primary results were reported for the specific ages 55, 60, and 65 years at baseline, but with a focus on the 65-year-olds because they are most susceptible to being diagnosed with disease and are closest to completing follow-up until end of life.
All analyses were adjusted for age at baseline, education, and cohabitation status and carried out separately for men and women. The effect of age was modeled as a second-degree polynomial for the models of length of stay with disease, but was otherwise modeled as linear. We included interactions between adjustment variables and the health score whenever significant in a likelihood ratio test; thus, an interaction between age and health score is included in some models. Consequently, the health score estimates from these models could be reported only for specific age values.
All statistical tests were two-sided, and we considered P < 0.05 to be significant. The statistical analyses were performed in R, version 4.3.2.
Results
A total of 22,218 men and 25,119 women were followed for a median 21.5 years (Supplement Fig. 1). During follow-up, 14,647 men and 14,147 women were diagnosed with at least one disease after a median 9.9 and 10.2 years, respectively, and 5,577 men and 4,591 women were diagnosed with two or more diseases. A total of 6,632 men and 5,137 women died during follow-up, the majority with disease (85% and 88%, respectively), Supplement Fig. 2.
The distribution of the nine selected health behaviors at baseline are shown in Table 1. The health score was calculated as the total number of these health behaviors an individual had at baseline. The mean health score was 4.2 (standard deviation [SD] 1.8) for men and 5.0 (SD 1.7) for women. The vast majority, approximately 91%, presented with a score between 2 and 7.
Life expectancy with and without disease
Table 2 shows life expectancy without disease by the health score according to sex and baseline age. For 65-year-old male participants, each point increment on the health score was associated with an additional 0.83 years [95% confidence interval 0.74 to 0.92] of healthy life expectancy, resulting in 7.4 years [6.63 to 8.26] when comparing the most healthy to the least healthy on the scale from 9 to 0 points. For women aged 65 years, each increment in health score was associated with 0.86 years of longer life without disease [0.77 to 0.94], with the extreme comparison resulting in 7.7 [6.93 to 8.49] years free from disease for those scoring 9 compared to 0.
Table 2 also shows life expectancy with disease by the health score according to sex and baseline age. Among 65-year-old male participants, each additional point on the health score was associated with −0.18 years [−0.26 to −0.09] of life expectancy with disease. A score of 9 compared to 0 resulted in 1.6 years less with disease [0.81 to 2.34]. Among 65-year-old women, each increment in health score resulted in −0.37 years [−0.45 to −0.29] with disease, resulting in 3.3 years less with disease for the highest health score compared to the lowest health score [2.60–4.03] (Table 2). Applying this model for men aged 65 years with cohabitation status “living together” and education level “medium”, the disease-free life expectancy for a health score of 0 points was 7.3 years, whereas the prediction for 9 points was 14.8 years. Life expectancy with disease was 6.4 years vs. 4.8 years, respectively. For a similar woman, having a score of 0 vs. 9 points resulted in 8.6 years vs. 16.3 years without disease and 6.8 years vs. 3.5 years with disease, respectively.
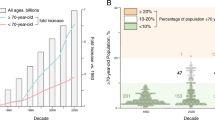
Figure 1 shows how life expectancy with and without disease was associated with each of the nine individual health behaviors. For life expectancy without disease, current smoking had the largest impact of −3.20 years for men and −3.74 years for women compared to never smoking. A high waist circumference was associated with −2.54 years and −1.90 years without disease, respectively, compared to low-risk waist circumference. The contribution to life expectancy without disease from a healthy diet (including the less strict diet score, Supplement Tables 5–6), sport activity, and alcohol consumption was less pronounced. For life expectancy with disease, the most pronounced impact was observed for women who were current smokers and had a high-risk waist circumference (as for life expectancy without disease), which did not appear to contribute to time with disease among men. Including BMI instead of waist circumference showed that the association between these two measures of obesity and disease-related healthy aging was similar (Supplement Tables 7–8).
Difference in life expectancy within 20 years of follow-up without (left) and with (right) disease for each of the nine individual health score factors by sex. The reference groups represent the healthier behavior except for diet due to very low numbers with the highest score. *Due to interactions between age and smoking (for men both with and without disease, for women only without disease), and age and waist circumference (only for life expectancy with disease), the estimates for smoking and waist, are shown for age 65 years, whereas the other estimates are valid for the entire age span. See Supplement Tables 2-4 for relevant estimates for age 60 and 55 years.
Life expectancy with multimorbidity
Table 2 also shows life expectancy with one disease and two or more diseases by the health score according to sex and baseline age. For 65-year-old men, each increment in health score was inversely associated with life expectancy with two or more diseases (−0.18 years [−0.20 to −0.16]). Among 65-year-old women, each increment in health score was associated with −0.18 years [−0.25 to −0.12] with one disease and −0.16 years [−0.18 to −0.14] with two or more diseases. Among men, predicted life expectancy with one disease was almost constant across health scores. However, for time with two or more diagnoses, there was a difference of 1.6 additional years (2.3 minus 0.7) for the score of 0 points compared to 9 points. Among women, the lowest score was associated with longer life expectancy with both one and two or more diagnoses compared to the highest score (4.8 vs. 3.1 years and 1.9 vs. 0.5 years, respectively, Fig. 2). Calculating predicted time with multimorbidity as a proportion of predicted time alive, these numbers correspond to 16.8% (2.3/13.7) and 3.6% (0.7/19.7) for lowest and highest health scores, respectively, for 65-year-old (living together, medium education level) men and 12.4% (1.9/15.3) and 2.5% (0.5/19.9), respectively, for women.
Days of hospitalization
Among the 47,112 (99.5%) participants with at least 1 year of follow-up included in these analyses, the median number of days of hospitalization per year of follow-up was 1.0 day (interquartile range [IQR]: 0.3 to 2.8) for men and 0.8 days (IQR: 0.3 to 2.1) for women; 1,206 (5.5%) men and 1,365 (5.5%) women had no history of hospitalization (Table 1). The distribution of the observed number of days of hospitalization per year for each health score is shown in Supplement Fig. 3. Predictions for 65-year-old men and women living with a partner who had a medium education level are shown in Fig. 3, with an average number of days of hospitalization per year of 6.1 and 5.5 for the lowest health score and 2.4 and 2.5 for the highest health score for men and women, respectively. The overall pattern shows a strong association for those with the lowest scores (2.5 [6.1 minus 3.6 days] and 1.7 [5.5 minus 3.8 days] days/year comparing 0 points with 4 points in men and women, respectively), whereas increase for those with the highest health score were markedly smaller (0.8 days comparing 5 with 9 points for both men and women [3.2 minus 2.4 and 3.3 minus 2.5, respectively]).
The overall pattern was the same for age 55 and 60 years (Supplement Figs. 4–5. Substituting calendar days of hospitalization with bed days defined according to Danish Health Authorities showed very similar results (Supplement Fig. 6).
Discussion
Using different markers of health behavior, we report a strong association between the utilized health score and subsequent disease-related healthy aging within a 20-year time frame in the population-based Danish cohort “Diet, Cancer and Health”. Thus, individuals with high scores lived longer; importantly, they lived twice as long without major chronic disease than those with low health scores. Furthermore, high scores were associated with a lower proportion of life expectancy with multimorbidity. We also report novel results of a strong association between the health score and days of hospitalization.
We used data from a large population-based cohort with detailed information on lifestyle and habitual diet. National registries in Denmark provide a unique resource for valid disease endpoint assessment with limited loss to follow-up25. However, unmeasured confounding can never be ruled out, and four out of five exposure variables were based on self-reporting. In contrast, trained personnel measured waist circumference at the study center visit, and education and cohabitation status were obtained from national registries. An obvious weakness was that information on health behaviors was obtained only at study entry. However, the aim was to study the association between health behaviors in midlife and disease-related healthy aging. The score based on these five health-related factors, assuming equal effects on disease-related healthy aging, is a simplified measure of a complex risk factor pattern. To address this, we conducted an analysis with a specific contribution of disease-free life expectancy from each health factor. Our results do not imply that all of the included markers of healthy behavior have an equal effect on disease-related healthy aging, but our health score can be used as a simple way of conveying the potential impact of healthy behavior on disease-related healthy aging.
Other studies have investigated differences in disease-free life expectancy according to composite scores based on health-related risk factors12,14,15. However, these studies are difficult to compare to our study due to different scores and disease outcomes. Our results are in concordance with those of Nyberg et al., as the healthiest participants based on smoking, BMI, physical activity, and alcohol (combined score of 0 to 8 points) lived 9 to 10 years more without type 2 diabetes, CHD, stroke, cancer, asthma, or COPD than the unhealthiest12. They found that a 1-point higher score was associated with almost 1 year longer without any major disease diagnosis. We reported 0.8 years per 1 point increment based on 20 years of follow-up. Thus, the true gain in healthy life years is most likely even larger.
This study illustrates that healthy behavior is not only associated with additional disease-free life, but also with a reduction of the relative life expectancy spent with disease in a 20-year time frame. However, by end of follow-up in 2018, 64% of the oldest participants aged 60–69 years at baseline were still alive, and we cannot conclude whether this pattern persists beyond the 20 years. By end of follow-up in 2018, 64% of the oldest participants aged 60–69 years at baseline were still alive, and we cannot conclude whether those who were disease-free and survived beyond end of follow-up will stay free of disease. The association between health behaviors and life expectancy with multimorbidity is not well studied. However, Licher et al. reported that absence of smoking, hypertension, and overweight was associated with a 9-year delay in a broad spectrum of diagnoses17, similar to those included in the current study. Furthermore, a difference of 10% in remaining lifetime (equal to a compression of 2 years) spent with one or more diseases was observed between the healthiest and least healthy participants. In line with this study, we found that high scores were associated with a lower proportion of life expectancy with multimorbidity; 65-year-old male participants with the highest health score could expect to spend 3% of their total life expectancy within 20 years with two or more diagnoses compared to 16% in the group with the lowest health score. Our study suggests that, when investigating the impact of healthy behavior, a broad range of morbidity measures is needed.
Healthy behavior has not previously been linked with subsequent days of hospitalization. Using this alternative morbidity measure, we found a strong association between our health score and days of hospitalization. For example, among 65-year-old men, the expected number of days of hospitalization decreased approximately 0.6 days/year per 1-point increment in the health score for scores of 0 to 4 points, after which the effect attenuated gradually. Days of hospitalization are among the most expensive services in healthcare and can be viewed as a marker of health care utilization11. Increasing pressure on health care systems forecasts a serious lack of health care personnel to treat the growing number of elderly with chronic disease, which requires solutions. The analyses of the hospitalization load with more pronounced effects in the lower half of the health score interval highlights that, from a health economic perspective, there is extra benefit of initiatives to support high-risk groups. In theory, the potential of moving a population from a score of 2 to a score of 4, which would lead to a reduction in the average number of days of hospitalization per year, may be realistic. Roughly translating this to health economy, assuming a tariff per bed day of 1,108€26, a decrease of 1 bed day per year for the Danish population of 65-year-olds (n = 61,264 in 2022) would correspond to savings of 67.9 million €/year, or 61,264 fewer hospital beds in use per year. The approach of simply summing the total number of days for each individual and dividing by years of follow-up may be a simplified approach to analyzing the association between health score and days of hospitalization. However, our results underline the importance of sophisticated cost–benefit analyses for implementing prevention efforts.
Conclusions
Healthy living, as reflected in a health score based on smoking, regular sport activity, alcohol intake, diet, and waist circumference in midlife, was associated with disease-free living and inversely associated with life expectancy with morbidity (i.e., ischemic heart disease, stroke, type 2 diabetes, cancer, dementia, COPD, and asthma) looking 20 years ahead. Healthy living was also inversely associated with multimorbidity and days of hospitalization, reflecting the impact on health care systems. Our results add to the mounting evidence supporting a substantial delay in, or even absence of, disease among individuals with low-risk lifestyle behaviors.
Data availability
The data underlying the findings of this study are restricted by the Danish Diet, Cancer and Health Review Board. Data can be made available from the Danish Cancer Society by following the Data Access Procedures for researchers who meet the criteria for access to sensitive data (contact: ake@cancer.dk). The application form can be obtained by contacting DCHdata@cancer.dk.
References
Yu, E. et al. Diet, lifestyle, biomarkers, genetic factors, and risk of cardiovascular disease in the nurses’ health studies. Am. J. Pub. Health 106, 1616–1623. https://doi.org/10.2105/ajph.2016.303316 (2016).
Ardisson Korat, A. V., Willett, W. C. & Hu, F. B. Diet, lifestyle, and genetic risk factors for type 2 diabetes: a review from the Nurses’ Health Study, Nurses’ Health Study 2, and Health Professionals’ Follow-up Study. Curr. Nutr. Rep. 3, 345–354. https://doi.org/10.1007/s13668-014-0103-5 (2014).
Tran, K. B. et al. The global burden of cancer attributable to risk factors, 2010–19: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 400, 563–591. https://doi.org/10.1016/S0140-6736(22)01438-6 (2022).
Kip, E. & Parr-Brownlie, L. C. Healthy lifestyles and wellbeing reduce neuroinflammation and prevent neurodegenerative and psychiatric disorders. Front. Neurosci. 17, 1092537. https://doi.org/10.3389/fnins.2023.1092537 (2023).
Stanaway, J. D. et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392, 1923–1994. https://doi.org/10.1016/S0140-6736(18)32225-6 (2018).
Ambrosino, N. & Bertella, E. Lifestyle interventions in prevention and comprehensive management of COPD. Breathe (Sheff) 14, 186–194. https://doi.org/10.1183/20734735.018618 (2018).
Freisling, H. et al. Lifestyle factors and risk of multimorbidity of cancer and cardiometabolic diseases: A multinational cohort study. BMC Med. 18, 5. https://doi.org/10.1186/s12916-019-1474-7 (2020).
Wikström, K., Lindström, J., Harald, K., Peltonen, M. & Laatikainen, T. Clinical and lifestyle-related risk factors for incident multimorbidity: 10-year follow-up of Finnish population-based cohorts 1982–2012. Eur. J. Intern. Med. 26, 211–216. https://doi.org/10.1016/j.ejim.2015.02.012 (2015).
World Health Organization (WHO). Global Health Estimates 2020: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2019 [Internet]. 2020 [cited 18–08–2022].
Tran, P. B. et al. Costs of multimorbidity: A systematic review and meta-analyses. BMC Med. 20, 234. https://doi.org/10.1186/s12916-022-02427-9 (2022).
Frølich, A., Ghith, N., Schiøtz, M., Jacobsen, R. & Stockmarr, A. Multimorbidity, healthcare utilization and socioeconomic status: A register-based study in Denmark. PLoS ONE 14, e0214183. https://doi.org/10.1371/journal.pone.0214183 (2019).
Nyberg, S. T. et al. Association of healthy lifestyle with years lived without major chronic diseases. JAMA Intern. Med. 180, 760–768. https://doi.org/10.1001/jamainternmed.2020.0618 (2020).
O’Doherty, M. G. et al. Effect of major lifestyle risk factors, independent and jointly, on life expectancy with and without cardiovascular disease: Results from the Consortium on Health and Ageing Network of Cohorts in Europe and the United States (CHANCES). Eur. J. Epidemiol. 31, 455–468. https://doi.org/10.1007/s10654-015-0112-8 (2016).
Li, Y. et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ (Clinical research ed.) 368, l6669. https://doi.org/10.1136/bmj.l6669 (2020).
May, A. M. et al. The impact of a healthy lifestyle on Disability-Adjusted Life Years: A prospective cohort study. BMC Med. 13, 39. https://doi.org/10.1186/s12916-015-0287-6 (2015).
Stenholm, S. et al. Smoking, physical inactivity and obesity as predictors of healthy and disease-free life expectancy between ages 50 and 75: A multicohort study. Int. J. Epidemiol. 45, 1260–1270. https://doi.org/10.1093/ije/dyw126 (2016).
Licher, S. et al. Lifetime risk and multimorbidity of non-communicable diseases and disease-free life expectancy in the general population: A population-based cohort study. PLoS Med. 16, e1002741. https://doi.org/10.1371/journal.pmed.1002741 (2019).
Tjonneland, A. et al. Study design, exposure variables, and socioeconomic determinants of participation in Diet, Cancer and Health: A population-based prospective cohort study of 57,053 men and women in Denmark. Scand J. Pub. Health 35, 432–441. https://doi.org/10.1080/14034940601047986 (2007).
Tjonneland, A. et al. Validation of a semiquantitative food frequency questionnaire developed in Denmark. Int. J. Epidemiol. 20, 906–912 (1991).
Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (London, England) 393, 1958–1972 (2019). https://doi.org/10.1016/s0140-6736(19)30041-8
Shi, W., Huang, X., Schooling, C. M. & Zhao, J. V. Red meat consumption, cardiovascular diseases, and diabetes: A systematic review and meta-analysis. Eur. Heart J. 44, 2626–2635. https://doi.org/10.1093/eurheartj/ehad336 (2023).
World Health Organization (WHO). Waist Circumference and Waist-Hip Ratio. Report of a WHO Expert Consultation, Geneva: World Health Organization, 2011.
Danish National Health Data Authority, Afrapportering fra teknikergruppe om opgørelse af indlæggelsesforløb baseret på Landspatientregisteret, 2017.
Grand, M. K. & Putter, H. Regression models for expected length of stay. Stat. Med. 35, 1178–1192. https://doi.org/10.1002/sim.6771 (2016).
Thygesen, L. C., Daasnes, C., Thaulow, I. & Bronnum-Hansen, H. Introduction to Danish (nationwide) registers on health and social issues: Structure, access, legislation, and archiving. Scand J. Pub. Health 39, 12–16. https://doi.org/10.1177/1403494811399956 (2011).
Dehlholm-Lambertsen, E. et al. Cost savings following faecal microbiota transplantation for recurrent Clostridium difficile infection. Therap. Adv. Gastroenterol. 12, 1756284819843002. https://doi.org/10.1177/1756284819843002 (2019).
Acknowledgements
We thank all the participants and staff who contributed to the Diet, Cancer and Helth cohort.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception. AKE wrote the original draft, while all contributed to editing and review in the process towards the final version. AKE and KG was responsible for the methods and data interpretation, while KG conducted all data analyses, made the figures and wrote the statistical methods section. PFH was data manager on the project and contributed to methods on hospitalization. JW and AO contributed to methods, data interpretation, and supervision. AT was responsible for cohort data collection and validation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Establishment of the Diet, Cancer and Health cohort study was approved by relevant scientific ethics committees ((KF) 01–345/93) and by the Danish Data Protection Agency. All participants gave written informed consent. The Danish authorities approved registry linkage and all analyses were conducted through Statistics Denmark.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Eriksen, A.K., Grell, K., Hendriksen, P.F. et al. Healthy lifestyle and life expectancy with and without major chronic disease – a cohort study. Sci Rep 15, 27691 (2025). https://doi.org/10.1038/s41598-025-11093-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-11093-9