Abstract
Further research is needed to investigate the association between netosis and clear cell renal cell carcinoma (ccRCC). We developed a prognostic framework for netosis using univariate, Lasso, and multivariate Cox regression analyses. The CIBERSORT algorithm was employed to compute immune infiltration metrics for The Cancer Genome Atlas (TCGA) dataset. These scores, combined with Cox regression analysis and patient survival data, contribute to the establishment of a prognostic model for the tumor microenvironment (TME). A combined prognostic model incorporating netosis and TME was then developed, stratifying patients based on median results. Further evaluation of the variations in the pathways within the model was conducted using Fast Gene Set Enrichment Analysis (FGSEA) and Weighted Correlation Network Analysis (WGCNA). Additionally, single-cell data integration allowed us to examine netosis-related genes in the context of cell communication and tumor development using the CellChat and Monocle packages. Netosis and TME scores exhibited a high degree of predictive power for patient survival, as illustrated by Kaplan-Meier (KM) curves. Gene set enrichment analysis (GSEA) revealed significant disparities in pathways associated with tumor occurrence between netosis and TME scores. A combined prognostic model incorporating both netosis and TME scores showed excellent performance in the validation set and TCGA data. FGSEA and WGCNA revealed significant differences in pathways associated with traditional tumor development and occurrence within distinct groups of the combined model. Furthermore, single-cell data analysis revealed substantial variations in intercellular communication levels among groups of netosis model genes with high and low expression. Pseudotime analysis highlighted increased expression of EREG, LYZ, S100A8, and S100A9. The combined netosis and TME prognostic model demonstrated high accuracy and efficacy, underscoring its potential value in guiding the treatment and prognosis of future ccRCC patients.
Similar content being viewed by others
Introduction
Renal cell carcinoma (RCC) is the most common type of kidney cancer in the adult population. RCC, also known as kidney cancer, originates in the renal cells. Clear cell renal cell carcinoma (ccRCC) is the most prevalent subtype, accounting for approximately 85–90% of cases, while rarer subtypes include collecting duct carcinoma, papillary carcinoma, and chromophobe carcinoma1. The exact etiology of RCC remains unclear; however, factors such as obesity, smoking, hypertension, genetic predisposition, and prolonged exposure to certain chemicals are thought to contribute to its development. RCC is often undiagnosed in its early stages, leading to treatment at more advanced stages. Common symptoms include hematuria, abdominal or flank pain, a palpable tumor or lump, fatigue, anemia, and weight loss. Diagnostic investigation is warranted when a patient presents with nonspecific symptoms. Magnetic resonance imaging (MRI) and computed tomography (CT) are commonly used for staging and treatment planning, as these techniques help characterize renal masses and assess tumor location, size, and potential invasion into adjacent tissues. The definitive diagnosis of RCC, including ccRCC, is made through histological analysis of tissue obtained via surgical resection or image-guided biopsy. Treatment strategies for RCC depend on the cancer stage, overall patient health, and individual patient needs2. Surgical removal is typically effective for early-stage patients, while advanced stages may require a combination of treatments, including immunotherapy, targeted therapy, chemotherapy, and radiotherapy3. Although advanced RCC carries a higher risk of metastasis and recurrence, the development of innovative targeted therapies and immunotherapies has offered new hope for successful treatment4.
Polymorphonuclear neutrophils (PMNs), the predominant leukocytes in the blood, play a critical role in the body’s initial immune defense by actively participating in the innate immune response against various invading pathogens, including bacteria, fungi, protozoa, and viruses5. In response to infection or inflammation, PMNs rapidly migrate from the bloodstream to sites of infection or tissue damage, where they perform phagocytosis, engulfing and eliminating invading microorganisms through various cytotoxic mechanisms. Neutrophils employ three primary mechanisms to target and neutralize these invading microorganisms: (1) the production of reactive oxygen species (ROS) inside phagolysosomes, enabling phagocytosis and destruction; (2) degranulation, which releases antimicrobial peptides to be released; and (3) the release of extracellular DNA traps, known as neutrophil extracellular traps (NETs), which trap microbes6. While the production of NETs aids in clearing infections, increasing evidence suggests that excessive NETs may contribute to the development of autoimmune disorders7. NETs function to immobilize extracellular pathogens and have the capacity to neutralize and eliminate bacteria, fungi, viruses, and parasites8. Subsequently, NETs are cleared either through macrophage-mediated endocytosis or by DNase I, an endonuclease responsible for cleaving chromatin within NETs9,10. Although NET formation aids in pathogen clearance, growing evidence suggests that an overabundance of NETs may contribute to the pathogenesis of autoimmune disorders11,12,13,14. In recent years, research on netosis and renal cancer has become quite popular. It has been confirmed that neutrophils influence tumor development by affecting the metabolic process of tumors through netosis15. However, the interaction between netosis and the tumor microenvironment (TME) still requires further investigation6. In our study, we focus on classical NETosis, which is a ROS-dependent form of NET formation characterized by cell membrane rupture, nuclear chromatin decondensation, and neutrophil death. This process is distinct from vital NETosis, which occurs without lytic cell death16.
The immune microenvironment of ccRCC consists of immune regulatory molecules, inflammatory mediators, and a complex network of immune cell components surrounding the tumor17. Understanding the immune microenvironment of ccRCC is crucial for investigating tumor development, treatment, and prognosis18,19. Various immune cell types coexist within this microenvironment, actively regulating both immune responses against the tumor and anti-tumor reactions20. Studies suggest a strong association between immune cell infiltration in RCC and patient prognosis21. Furthermore, certain netosis-related genes (NRGs) play a role in regulating immune cell activity and inflammatory responses within the ccRCC microenvironment.
Prognostic assessment of ccRCC is a complex and multidimensional process that requires consideration of various factors, including immunological elements, pathogenic and clinical characteristics, and molecular markers22,23. With the growing understanding of tumor biology and its relationship to the immune system, developing prognostic models with tailored treatment plans has the potential to enhance RCC patient outcomes. This study aims to identify new indicators associated with immunotherapy by integrating the patient’s immunological microenvironment and NRGs to create a predictive model for ccRCC treatment.
Method
Data acquisition and processing
Sixty-nine NRGs were compiled from pertinent reviews and studies6,24,25. We retrieved bulk data and matching clinical data from the TCGA and Gene Expression Omnibus (GEO) databases. GSE29609 was used for objective evaluation for model validation. We procured single-cell data for ccRCC cells from GSE171306. This study does not involve experimental animals or human participants.
Models of NETosis and immune cell infiltration
Based on differential analysis, tumor tissue and adjacent non-tumor tissue were compared in the RCC patient data. The selection criteria included a p-value < 0.01 and |logFC| > 2.0. A predictive model was developed by intersecting the identified differentially expressed genes with the NRGs. The percentage of immune cell infiltration was assessed using the CIBERSORT method to evaluate the immune cell composition.
Distinctions in pathways between NETosis and TME models
Using the median as a threshold, the NETosis and TME models were stratified into high and low-risk groups. Pathway variations between these risk groups were then compared to identify differences within the NETosis and TME models.
Construction of a risk prediction model and survival analysis
Once the NRGs were selected, the first step was to identify the prognostic NRGs. LASSO regression was employed to select predictive variables and reduce the risk of overfitting. Multivariate Cox regression analysis, combined with bootstrap optimization, was applied to identify the remaining candidates for the risk model. Use the coefficient divided by the bootstrap standard deviation to obtain the NET score. A TME infiltration score was also calculated using bootstrap-optimized multivariable Cox regression, and favorable prognostic immune cells were selected based on the optimal cutoff from the CIBERSORT findings and survival data. NETosis scores and immune scores were categorized as NET high, NET low, TME high, and TME low according to their median values. Patients were then divided into NET high-TME high, NET low-TME low, and mixed groups, and survival curves were generated for detailed analysis.
WGCNA analysis and group GSEA analysis
We aimed to identify distinct pathways within the NET and TME groups using WGCNA modules. The FGSEA approach was utilized to identify the pathways associated with each group, 20 pathways were selected for heatmap visualization. The TIP database was utilized to visualize global immunological pathway variations among these three groups, enabling a comprehensive analysis of the disparities. This comprehensive methodology facilitated a complete investigation of pathway variations within the NET high, NET low, and mixed groups.
Integration of single-cell data
The Seurat object for each sample was processed using the Read10x function from the Seurat package. Quality control standards were set for mitochondrial genes (≤ 10%), ribosomal genes (≤ 30%), hemoglobin genes (≤ 5%), and total gene count per cell (200–7,000). After rigorous cell quality control, we normalized the data using “NormalizeData”. For each sample, the expression of a gene was multiplied by 10,000, followed by natural logarithm transformation. To prevent taking the logarithm of 0, normalization was performed after adding 1. The identification of the 3000 most highly variable genes (HVGs) was achieved using the “FindVariableFeatures” function. After applying “ScaleData” to center and scale these HVGs, PCA was performed based on these genes. To integrate samples, the “anchor point” method with SCT correction was employed, identifying 3,000 HVGs. The “dims” parameter was set to 20, and t-SNE was utilized for dimensionality reduction. Cell clustering was conducted using the KNN approach with a resolution of 1.0. Cell annotation was performed by identifying cell surface markers with the “singleR” package (version 1.10.0). The CellChat package was employed to analyze differences in cell communication among distinct netosis model groups, assessing how NETosis influences intercellular communication in ccRCC cells. Pseudotime analysis using Monocle2 was conducted to observe changes in NRGs in tumor cells. To further evaluate the predictive performance of NETosis-related gene expression at the single-cell level, we additionally incorporated three scRNA-seq datasets: GSE131685, GSE152938, and GSE171306. After cell clustering and annotation, we focused on monocytes and endothelial cells, where NET scores were calculated for each cell. ROC curve analysis was then performed to assess the ability of NETscore to discriminate tumor vs. normal cells within these two cell populations, and AUC values were used to quantify prediction accuracy. This analysis was conducted using the pROC package in R.
A comparative analysis of immunogenic mutations and immunotherapy
Using single sample gene set enrichment analysis (ssGSEA), we examined the immunological microenvironmental features of prognostic groups in ccRCC. Additionally, we assessed the efficacy of immunotherapy across different groups using the TIDE (Tumor Immune Dysfunction and Exclusion) tool (http://tide.dfci.harvard.edu/login/).
Cell culture and transfection
Five ccRCC cell lines (786-O, 769-P, UMRC2, OSRC2 and Caki-1) and normal renal cells (HK-2) were obtained from the Cell Bank of the Chinese Academy of Sciences (Shanghai, China). All cell lines were maintained in RPMI-1640 medium (Gibco, USA). 10% fetal bovine serum (Gibco, USA), 1% penicillin and streptomycin (Gibco, USA) were added to the medium. All were cultured at 37 °C in a humidified atmosphere containing 5% CO2.
Quantitative real-time PCR (qRT-PCR)
A previous study described specific methods for total RNA extraction and quantitative real-time PCR (qRT-PCR). Table S1 showed the sequence of primers used in this study. Actin was used as an internal control. The procedures were performed three times to ensure accuracy and precision. The relative expression levels were calculated using the 2 − ΔΔCT method.
Results
Intersection of differential genes and netosis-related genes for immune cell infiltration
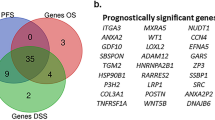
Screening was conducted to identify genes with varying expression between cancerous and adjacent non-cancerous tissues based on the criteria of |logFC| > 2.0 and p < 0.05. NRGs were employed in the design of prognostic models by intersecting with differentially expressed genes. Subsequently, univariate Cox regression analysis was performed to determine 22 prognostic NRGs with a p-value < 0.01. A heatmap was generated to illustrate the disparities in gene expression between tumor and non-tumor samples (Fig. 1A). Using Lasso and multivariate Cox regression models, we identified 7 NRGs to construct the prognostic model (Fig. 1B, C, D). Survival curves were then generated by classifying each sample into high and low-risk groups, based on the optimal model coefficients (Fig. 1E), demonstrating the model’s robust prognostic predictive power. The CIBERSORT algorithm was used to analyze immune cell infiltration proportions in ccRCC, yielding data for 22 immune cell types. After excluding low-expression cells and identifying fourteen immune cells that significantly impact patient prognosis (p < 0.05), further analysis focused on active dendritic cells, resting mast cells, activated dendritic cells, and monocytes (Fig. 1F, G, H, I). KM curves, grouped by median infiltration proportions, revealed that infiltration percentages of activated dendritic cells, resting mast cells, M2 macrophages, and monocytes can accurately predict patient prognosis (Fig. 1J). Improved survival rates were observed in the group with a high infiltration proportion (Fig. 1K). Additionally, immune infiltration scores were used in a multivariable Cox regression analysis to construct an immunological prognostic model with these four immune cell types. By employing bootstrap methods to optimize model coefficients and creating a forest plot, it is evident that patients with these three cell types generally have better prognoses. The immune infiltration model serves as a robust predictor of patient prognosis, as shown by KM curves based on model risk scores that categorize patients into high and low-risk groups. The group with higher immune infiltration score exhibited a greater chance of survival.
NET model and TME model. (A) Heatmap of gene expression after intersecting Univariate Cox regression analysis and differentially expressed genes. (B, C) LASSO-selected feature variables. (D) Multivariable Cox regression of netosis model. (E) Survival curve of high- and low-score groups in the netosis model. (F–I) Survival curves of four immune cell infiltration groups (high and low). (J) Multivariable Cox regression of four immune cell types. (K) Survival curve of immune infiltration model groups.
GSEA analysis in groups
First, we assessed GSEA pathways among groups with high and low TME scores, as well as those with high and low NET scores. Pathways such as adherens junction, tight junction, and TGF-beta signaling pathway in the NET model demonstrated a declining trend as the risk decreased (Fig. 2A, B, C). This aligns with our finding that the high-risk group experienced poorer patient survival. Improved prognosis was associated with higher immune-related scores in our immune-related model. Results from the GSEA analysis of the immunological score groups supported our hypothesis, showing that the activation levels of tight junction, adherens junction, and TGF-beta signaling pathways decreased as immunological scores increased (Fig. 2D, E, F). Our finding that individuals with higher immunological ratings fared better in our survival curves is reinforced by this consistency. Notably, the NET score model and the immunological score model exhibited opposing patterns for these pathways, which are associated with the invasion and progression of ccRCC. Combining the NET score algorithm with the immune infiltration model may enhance the reliability of prognosis predictions for patients.
Creation of a model for risk prediction and survival analysis for different groups
Subsequently, the two models were integrated, resulting in the categorization of samples into four groups: NET high TME low, NET high TME high, NET low TME low, and NET low TME high. Based on Kaplan-Meier survival trends, the NET high–TME high and NET low–TME low groups exhibited intermediate and overlapping prognostic behavior, lacking clear prognostic divergence. Therefore, these two groups were merged to form a “Mixed” group. This decision enabled us to emphasize the biologically distinct and prognostically contrasting patterns observed in the NET high–TME low and NET low–TME high groups, improving the clarity and interpretability of the overall risk stratification model. A combined risk prediction model was developed, and its validity was assessed through ROC analysis and survival curves (Fig. 3A, B). The independence of this model from additional clinical factors is demonstrated by univariate and multivariate independent prognostic assessments (Fig. 3C, D). Furthermore, the model was applied to the GSE29609 dataset, confirming its robust predictive ability through ROC analysis and survival curves (Fig. 3E, F). Subpopulation analyses for prognosis revealed statistically significant differences in prognostic outcomes for both male and female patients, as well as for those aged over 65 and those under 65 (Fig. 3G, H, I, J). It can be observed that there are significant differences in the prognostic model across different subgroups, whether in males or females, and whether individuals are below or above 65 years of age. The NET-low TME-high group shows the best prognosis, while the NET-high TME-low group has the worst prognosis. This indicates that our model holds prognostic significance across all genders and age groups. Notably, the prognostic model exhibited distinct variations among patients at different tumor stages, with a more pronounced effect observed in those with advanced stages (Fig. 3K, L, M, N, O, P).
Combined prognostic model. (A) Survival curve of the combined model. (B) ROC curve of the combined model. (C) Univariate independent prognostic analysis of the combined model. (D) Multivariate independent prognostic analysis of the combined model. (E) Survival curve of the validation set. (F) ROC curve of the validation set. (G–P) Survival curve of different sub-groups.
WGCNA analysis and TIP analysis
The outcomes of the WGCNA analysis revealed that each risk category was associated with distinct modules, with the gray module showing significant divergence (Fig. 4A, B). Subsequently, we isolated this module and examined the enriched genes in traditional pathways related to tumor formation using KEGG pathway analysis26,27,28. Pathways such as the PI3K-Akt signaling pathway, focal adhesion, TNF signaling pathway, proteoglycans in cancer, PPAR signaling pathway, cell adhesion molecules, NF-kappa B signaling pathway, MAPK signaling pathway, TGF-beta signaling pathway, and Hippo signaling pathway exhibited significant enrichment, indicating that these module genes may play a crucial role in tumor formation (Fig. 4C). Furthermore, each risk group’s pathways were identified using FGSEA, and the top 20 pathways were selected for the figure (Fig. 4D). Notably, pathways such as the phospholipid metabolic process, the signaling pathway of vascular endothelial growth factor, endothelial cell proliferation, and the regulation of multicellular organism development were significantly downregulated in the NET high TME low group. Conversely, mechanisms including the regulation of the Wnt signaling pathway, endothelial cell differentiation, assembly of cell-cell junctions, and artery morphogenesis were markedly upregulated in the NET low TME high group. Significant variations were observed between the three groups through FGSEA analysis. Lastly, we utilized the TIP database to illustrate the variations in global immunological pathways across the three risk groups. The monocyte recruiting pathways in the NET low TME high and NET high TME low groups exhibited notable differences, indicating a significant divergence in the immunological milieu of these two groups (Fig. 4E). This further elucidates the close correlation between macrophages and immune processes, highlighting significant implications within the model.
Single-cell data-based immunological microenvironment analysis
We obtained single-cell expression data for ccRCC, considering the notable variations in the immunological milieu across the netosis score categories, the distinct degrees of pathway activation, and the observed relationship between NRGs expression and immune cell distribution. Integration of single-cell data from six ccRCC samples was conducted (Fig. 5A). Quality control measures were implemented for these specimens, focusing on mitochondrial and red blood cell proportions. Through PCA for dimensionality reduction and tSNE visualization, along with cell annotation using singleR, we identified cell populations exhibiting a protective effect against netosis (Fig. 5B). The NET-score measurements revealed noteworthy score differences for macrophages and monocytes, suggesting their potential protective role. An examination of netosis model gene expression levels within these clusters was performed, and the differences were statistically significant (Fig. 5C). Tumor cells were categorized into NET high (cluster 18), NET low (cluster 14), and NET mid (clusters 0, 8) (Fig. 5D). Subsequently, the CellChat package was employed to demonstrate cell-to-cell contact between the various tumor clusters. The results revealed distinct cell communication patterns among these groups, particularly between the NET high and NET low clusters, reflecting significant variations in communication intensity (Fig. 5E, F). It can be observed that the NET high group exhibits the highest number and degree of communication in monocytes, with macrophages and other cells also showing significant communication. This is consistent with our previous research. Figure 5E shows the global cell-cell communication network within the TME in the NET high and NET low groups, as inferred using the CellChat package. In this diagram, nodes represent different cell types, with node size corresponding to the total amount of signaling input and output (i.e., communication activity of that cell type). Edges represent the strength of ligand-receptor–based interactions between cell types, with thicker lines indicating stronger communication. In the NET high group, we observed a greater number and strength of communication pathways, especially involving monocytes and macrophages, suggesting these cells play a central role in the immune crosstalk under NETosis-dominant conditions. In contrast, the NET low group displayed weaker and sparser interactions, indicating a relatively quiescent immune communication network. This enhanced signaling network in the NET high group highlights the potential of NETosis to restructure the immune landscape and modulate the behavior of immune effector cells in ccRCC. Figure 5F illustrates how different cell types, especially macrophages and monocytes, are involved in MIF signaling within the NET high and NET low groups. Global communication of each NET group and other cells was also visualized (Fig. 5G). This panel compares the intercellular communication patterns between the NET high and NET low groups, particularly focusing on the interactions involving immune cells like monocytes, macrophages, NK cells, and T cells. The findings from Figs. 5E-G collectively suggest that NETosis not only affects individual immune cells but also modulates the broader network of intercellular communication within the TME. The enhanced communication observed in the NET high group, especially involving macrophages and monocytes, highlights the complex role of NETosis in shaping an environment that could support tumor progression. In addition, pseudotime trajectories for monocyte cells were inferred using the Monocle2 program. Significant alterations in the expression levels of specific genes were observed during the development and differentiation process of tumor cells (Fig. 5H, I). This panel displays the pseudotime trajectory of monocyte cells using Monocle2. Pseudotime analysis is used to infer the developmental and differentiation pathways of cells over a continuous trajectory. Pseudotime analysis in our study showed that these genes exhibited significant expression changes along the differentiation trajectory of monocytes and tumor cells, suggesting their involvement in key functional processes in the TME. Further functional annotation and pathway enrichment analysis supported their roles in pathways related to tumor invasion, immune modulation, and cell survival. Notably, EREG, LYZ, S100A8, and S100A9 exhibited high expression levels throughout development, indicating their possible functions in the early phases of expansion (Fig. 5J). Their expression patterns suggested a potential involvement in the differentiation and functional states of monocytes in the TME of ccRCC. These genes were originally identified among our NRGs and are supported by previous literature as functional markers of neutrophil activity and modulators of inflammatory responses. Notably, S100A8 and S100A9 are involved in NET formation, while LYZ reflects antimicrobial neutrophil function, and EREG has been linked to NET-induced tumor-promoting inflammation. Their progressive expression changes along the pseudotime trajectory suggest their active involvement in shaping the immune microenvironment, possibly through modulation of NETosis-related processes in ccRCC. EREG is known to play a role in modulating inflammatory responses and has been implicated in the progression of various cancers. Its expression can be influenced by the release of NETs, making it relevant to NETosis and its impact on the TME29. LYZ is an antimicrobial protein that is often associated with neutrophil activity, including NETosis. Its expression can reflect the functional state of immune cells in the TME, particularly monocytes and macrophages30. S100A8 and S100A9 encode proteins that are crucial components of the S100 family, which are involved in inflammation and the immune response. S100A8 and S100A9 have been linked to NET formation and the regulation of immune cell activity within the TME, thus serving as markers for NETosis-related processes31. The extent of alterations in different genes during the branch analysis is illustrated in Fig. 5K. In light of the earlier findings on cell communication, the expression of EREG, LYZ, S100A8, and S100A9 may influence the interaction between tumor cells and immune cells, thereby promoting tumor invasion and development (Fig. 5L). During the pseudotime analysis of monocyte differentiation, EREG, LYZ, S100A8, and S100A9 were among the genes that exhibited dynamic expression changes. Their expression patterns suggested a potential involvement in the differentiation and functional states of monocytes in the TME of ccRCC. Additionally, the elevated expression of NRGs in Monocytes suggests a protective role. The GOS2 gene potentially correlates with pathways inducing apoptosis and activating anti-cancer genes, while the IL1B gene is linked to immune-related processes (Fig. 5M). Studying these genes may have further positive implications for future research on kidney cancer. GOS2 is reported to be involved in the regulation of apoptosis and cellular energy metabolism. It is known to influence the balance between cell survival and cell death, playing a role in the suppression of tumor growth. IL1B is a pro-inflammatory cytokine that can either promote tumor progression or facilitate anti-tumor immune responses, depending on the context. It is involved in modulating the immune response within the TME32. These figures illustrate their differential expression patterns, but do not directly prove their functional roles33,34. To validate the predictive performance of NETscore at the single-cell level, we conducted ROC curve analysis in monocytes and endothelial cells, based on three independent scRNA-seq datasets (GSE131685, GSE152938, GSE171306). As shown in Fig. 5N, the NETscore achieved an AUC of 0.773 in monocytes and 0.729 in endothelial cells, indicating good classification power for distinguishing tumor versus normal cell states. These results support the discriminatory utility of NRGs in specific immune and stromal populations and further reinforce the applicability of our NETscore model across different data platforms.
Single-cell analysis. (A) Quality control plot for single-cell data. (B) UMAP single-cell dimensionality reduction clustering, displaying Seurat_cluster. (C) NET scores of different cell types. (D) Feature plot showing the expression levels of NET model genes in chosed clusters. (E) Global cell communication. (F) MIF signaling pathway network. (G) Cell communication between the high and low NET groups and immune model cells. (H, I) Pseudotime analysis trajectory plot. (J) Variation of GPR genes along the pseudotime. (K) Heatmap of branch analysis. (L)Feature plot of high expression genes. (M) Feature plot of high expression netosis-related genes. (N) ROC curve of NET score in single cell analysis.
Mutation burden analysis, immune checkpoint analysis, and TIDE immune therapy prediction
Utilizing downloaded tumor mutation data and conducting further investigations based on the joint prognosis group, along with the previously established NET-TME classification, we observed a negative impact of tumor mutations on patient prognosis. Figure 6A illustrates the prognostic performance among different subgroups, while Fig. 6B reveals the varying prognostic performances between different levels of TME. Figure 6C and D depict the gene mutation levels of the NET high TME low group and NET low TME high group, highlighting a significantly lower mutation level in the NET high TME low group. Numerous immune checkpoint genes, including PDCD1 (PD-1), CTLA4, LAG3, TIGIT, CD80, and BTLA, were found to be significantly upregulated in the NET high–TME low group, whereas the NET low–TME high group exhibited the lowest expression levels (Fig. 6E). These checkpoints are known to inhibit T cell activation and promote immune tolerance within the TME. The elevated expression of these inhibitory molecules suggests that the NET high–TME low group may harbor an immunosuppressive phenotype, often associated with T cell exhaustion. However, such a phenotype is also potentially more responsive to immune checkpoint inhibitor (ICI) therapy, which works by reactivating suppressed T cells through blockade of these pathways. Therefore, despite the poor baseline prognosis, patients in this subgroup may derive greater benefit from ICI treatments, highlighting an important clinical implication of our NET–TME stratification. Moreover, the expression levels of checkpoint genes gradually increase from the NET low TME high group to the mixed group and then to the NET high TME low group. This suggests that the activity of checkpoints in the protective group is relatively low, accompanied by reduced immune suppression. This condition is associated with a lower degree of immune inhibition, leading to a more robust immune response. Consequently, it is plausible that individuals in this group may exhibit enhanced immune efficacy and potentially experience a better prognosis.
Analysis of gene mutations and immunotherapy. (A) Survival curve of the combined groups. (B) Survival curve of different TME groups. (C, D) Genetic mutation analysis of two groups. (E) Differential immune checkpoint expression among GPR + TME groups. (F) Differential TIDE response rate among GPR + TME groups. (G, H) Differential response rate among GPR + TME groups. (I,J) Downregulated genes in response group and NET-low TME-high group.
Expanding upon the immunological distinctions between the two cohorts, our aim was to comprehend the fluctuations in response to immune intervention (Fig. 6F). We assessed the sensitivity of the two patient groups to immune therapy using the TIDE website, and the results revealed significant differences in sensitivity. The NET high TME low group exhibited a higher response rate, while the NET low TME high group showed a lower response rate (Fig. 6G, H). Moreover, a noteworthy difference exists in the response rates between the NET low group and the NET high group. However, when examined separately, there is no apparent difference, indicating that the individual NET score, to some extent, reflects immune response rates and treatment efficacy.
Moving on to the proteomaps analysis, we focused specifically on downregulated genes in the TIDE-predicted immune responders. These genes were selected because their reduced expression may indicate suppression of tumor-promoting or immune-evasive pathways, which can facilitate more effective immune responses. We hypothesized that such downregulation creates a tumor microenvironment more favorable for immunotherapy efficacy. When we compared this gene set to those downregulated in the NET low–TME high group, which was previously characterized by low checkpoint expression and active immune features, we observed striking transcriptomic overlap. As shown in Fig. 6I and J, proteomaps revealed a shared landscape of reduced immunosuppressive and pro-tumor signaling, underscoring the biological consistency between TIDE responsiveness and our NET-TME stratification. This alignment suggests that our combined model not only stratifies prognosis but may also serve as a surrogate indicator of immunotherapy sensitivity in ccRCC.
Exploring the expression of NRGs in CcRCC
We utilized the TCGA database and PCR experiments to further validate the expression of six NRGs in ccRCC tissues and cell lines. First, our analysis revealed that, aside from GOS2, which was significantly downregulated in ccRCC, the other five genes exhibited higher expression levels in ccRCC compared to normal tissues. This conclusion was also confirmed through PCR experiments on tissue samples. Additionally, we found that EREG, IL1B, S100A8, S100A9, and LYZ were significantly upregulated in five different ccRCC cell lines, while GOS2 expression was notably lower compared to HK2 (Fig. 7A-F).
Expression difference of NRGs in ccRCC. (A–F) Expression levels of six NRGs (GOS2, EREG, IL1B, S100A8, S100A9, and LYZ) in ccRCC tissues compared to normal tissues, as determined by TCGA database analysis and validated through PCR experiments. (A: EREG; B: S100A9; C: IL1B; D: LYZ; E: S100A8; F: G0S2).
Discussion
ccRCC accounts for 85–90% of kidney cancer cases, with less common subtypes including chromophobe, papillary, and collecting duct carcinoma. Pathologically, ccRCC typically presents with clear cell nuclei and abundant cytoplasm, originating from renal tubular epithelial cells and exhibiting marked heterogeneity35. A characteristic vascular-rich structure is observed, supported by an intricate vascular system, which may be accompanied by necrosis and hemorrhage. This structure is often accompanied by pathological manifestations such as necrosis and hemorrhage36. The precise etiology of RCC remains unclear, but hereditary conditions such as Von Hippel-Lindau (VHL) disease have been implicated in its pathogenesis37.
NETs are complex structures resembling webs, composed of granular and nuclear elements38. NETs primarily serve to prevent the growth of microorganisms and facilitate their removal39. However, uncontrolled NET release or impaired clearance can lead to unintended pro-inflammatory side effects40. While immune complexes and the subsequent production of cytokines are the primary indirect mechanisms through which NET-induced organ damage occurs, their direct effects on cells are also significant41. Neutrophils release NETs in cancer tissue, which is similar to the process of eliminating bacteria in certain aspects42. NETs are involved in immune responses and also serve as contributing factors to disease pathology43. Tumor tissue can not only induce the process of netosis but also participate in the inflammatory response, serving as a risk factor for tumor metastasis44. Neutrophils in the blood play an important role in this process, and their effects on systemic inflammatory responses and tumor tissue still require further validation and research. DNase I is a drug targeting NETs for systemic treatment, and its safety has been validated45. These findings indicate that NETosis plays a critical yet hazardous role in various renal diseases, including ccRCC46,47. Netosis promotes macrophage function, enhancing their phagocytic ability and capacity to participate in inflammatory responses48. Macrophages are involved in the clearance of NETs while also releasing IL-1β, IL-6, and TNF, positively regulating netosis through interferon. Overall, macrophages play a crucial role in the process of netosis46.The absence of a statistically significant difference in neutrophil recruitment in our model may be due to the complex and dynamic nature of neutrophil behavior in the TME. Neutrophils can exhibit a wide range of functional states, and their presence alone does not always correlate directly with NETosis activity or patient prognosis. Additionally, the recruitment of neutrophils may be transient and context-dependent, which can make it challenging to detect significant differences in recruitment levels across different patient groups. Our model, while focused on NRGs, may capture more stable and downstream immune alterations (e.g., macrophage activity) rather than the transient dynamics of neutrophil recruitment. Future studies could explore this further by examining the dynamic behavior and functional states of neutrophils in relation to NETosis and TME modulation.
The prognostic model of NETosis has been utilized in various cancer types, including lung cancer and cervical cancer49. Our study distinguishes itself by integrating NET scores with TME scores and utilizing single-cell data for further analysis. By incorporating tumor immune-related research, our study offers a comprehensive understanding of ccRCC50. In our combined model, we chose to merge the NET high–TME high and NET low–TME low groups based on their similar survival trends. This approach sharpened the prognostic contrast between the remaining two groups and enhanced the clinical applicability of the model. It also reflected the opposing biological influences of NETosis and immune infiltration in ccRCC progression, thereby improving the model’s ability to distinguish biologically meaningful patient subsets51. We identified differentially expressed NRGs in monocytes and used them to develop predictive risk models associated with immune cells and the netosis pathway. These models effectively predicted outcomes for renal cancer patients.
We integrated NETosis-related gene expression with immune infiltration metrics to construct a combined prognostic model (NET-TME), highlighting the interaction between NETosis and TME in ccRCC. NETosis, mediated by activated neutrophils, leads to the release of NETs, which are known to modulate the TME by influencing immune cell recruitment, cytokine release, and intercellular signaling pathways. NETs can promote macrophage activation, modulate monocyte differentiation, and shape immune cell–tumor interactions, thereby contributing to tumor immune evasion or progression. Our single-cell analysis further confirmed that monocytes and macrophages, which play critical roles in NET clearance and downstream signaling, exhibit enhanced intercellular communication and altered gene expression in NET-high subgroups. This supports the view that NETosis activity is not isolated but functions within a dynamic immune context. By incorporating both NET and TME scores, our model more comprehensively reflects the complex crosstalk between neutrophil activity and immune microenvironmental remodeling, offering improved prognostic performance and mechanistic insight into ccRCC pathogenesis52.
Our findings also highlight the functional importance of immune checkpoints in shaping the tumor immune landscape of ccRCC. Immune checkpoints such as PDCD1 (PD-1), CTLA4, LAG3, BTLA, and TIGIT are critical inhibitory molecules that regulate T cell activity and maintain immune homeostasis. In the NET high–TME low subgroup, we observed significantly elevated expression of multiple immune checkpoints (Fig. 6E), suggesting an immune-exhausted phenotype characterized by impaired cytotoxic T cell function and reduced anti-tumor activity. This checkpoint-enriched microenvironment likely contributes to immune evasion by tumor cells, resulting in worse prognosis despite high immune infiltration. Conversely, the NET low–TME high group exhibited reduced expression of checkpoint genes and lower TIDE scores, indicating a more immunoreactive environment that may be more responsive to immune checkpoint blockade (ICB) therapy. These findings suggest that NETosis may influence the expression of immune checkpoints, thereby indirectly shaping the responsiveness of ccRCC tumors to immunotherapy.
Taken together, our integrative model provides a new perspective on how neutrophil-driven inflammation and checkpoint-mediated immune suppression converge to influence clinical outcomes and treatment response in ccRCC. This highlights the potential of targeting checkpoint molecules in NETosis-dominant immune contexts as part of personalized immunotherapy strategies.
In our study, we systematically integrated NRGs with clinical data and TCGA gene expression data, employing immune infiltration algorithms to calculate cell type proportions. To develop models related to immune infiltration and netosis, we utilized univariate, multivariate, and LASSO Cox regression analyses. Our results indicated significant variations in pathway activities between immune infiltration and NET groups, particularly between the NET low-TME high group and the NET high-TME low group. WGCNA analysis revealed differences in gene modules between these groups, supported by FGSEA analysis. Single-cell data further indicated that elevated expression levels of key genes within the NET model were associated with enhanced intercellular communication in ccRCC cells. Key genes identified in our analysis, such as EREG, LYZ, S100A8, S100A9, GOS2, and IL1B, play critical roles in shaping the TME and tumor progression. EREG (Epiregulin) is known to promote cancer cell proliferation, migration, and invasion through the EGFR pathway, and it has also been implicated in creating an immunosuppressive environment that fosters tumor progression, influenced by NETs, making it relevant to NETosis in the TME29. LYZ (Lysozyme) is an antimicrobial protein often associated with neutrophil activity, including NETosis, and modulates immune responses, regulating inflammation and immune cell infiltration within the TME53. S100A8 and S100A9 are involved in tumor growth, invasion, metastasis, and immune modulation within the TME. These genes promote an inflammatory environment that supports tumor progression and have been linked to NET formation, serving as markers for NETosis-related processes54. G0S2 (G0/G1 Switch Gene 2) is involved in the regulation of apoptosis and cellular energy metabolism, influencing the balance between cell survival and death, thus playing a role in suppressing tumor growth55. IL1B (Interleukin-1 Beta) is a pro-inflammatory cytokine that can either promote tumor progression or facilitate anti-tumor immune responses, depending on the context, and is involved in modulating immune responses within the TME56.
Our investigation was not without its limitations. First, we constructed and evaluated a netosis-related prognostic model using standard univariate and Lasso regression risk assessments. While this approach has been recognized and utilized in several studies, we aim to enhance our research in the future by employing more sophisticated methodologies. Second, we were unable to acquire additional parameters for model validation; the data analysis in this study was solely based on publicly accessible datasets. Third, the NRGs included in our analysis were identified based on existing evidence of their involvement in disease progression; however, prospective data is needed to further validate their clinical significance. Forth, another key limitation of our study is the lack of direct histological evidence to confirm that the infiltration and expression of NRGs originated from NET-forming neutrophils. While our single-cell and CellChat analyses demonstrated high expression of NRGs (e.g., S100A8, S100A9, LYZ, IL1B, EREG) in monocytes and macrophages—cells involved in NET clearance and inflammation—this cannot fully substitute for direct visualization of NET structures (e.g., CitH3, MPO, extracellular DNA) within ccRCC tissues. We plan to conduct future studies using immunofluorescence or immunohistochemistry to validate NET structures and strengthen the mechanistic link between NRG expression and NETosis in situ.
Conclusion
This study highlights the significant role of NRGs in shaping the TME and influencing tumor progression in ccRCC. Key NRGs, including EREG, LYZ, S100A8, S100A9, GOS2, and IL1B, were identified as crucial players in immune modulation and intercellular communication. Our prognostic model, integrating NETosis and immune infiltration factors, effectively predicted patient outcomes and immunotherapy responses. Despite some limitations, these findings provide a basis for further exploration of personalized treatments targeting NETosis and the immune microenvironment in ccRCC.
Data availability
The data that support the findings of this study are openly available in TCGA(https://www.cancer.gov/ccg/research/genome-sequencing/tcga) and GEO(https://www.ncbi.nlm.nih.gov/geo/, GSE29609,GSE171306) datasets.
References
Motzer, R. J. et al. Kidney cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J. Natl. Compr. Cancer Network: JNCCN. 20 (1), 71–90 (2022).
Vermassen, T., De Meulenaere, A., Van de Walle, M. & Rottey, S. Therapeutic approaches in clear cell and non-clear cell renal cell carcinoma. Acta Clin. Belg. 72 (1), 12–18 (2017).
Chowdhury, N. & Drake, C. G. Kidney cancer: an overview of current therapeutic approaches. Urologic. Clin. North. Am. 47 (4), 419–431 (2020).
Lai, Y. et al. The tumour microenvironment and metabolism in renal cell carcinoma targeted or immune therapy. J. Cell. Physiol. 236 (3), 1616–1627 (2021).
Njeim, R. et al. NETosis contributes to the pathogenesis of diabetes and its complications. J. Mol. Endocrinol. 65 (4), R65–R76 (2020).
Papayannopoulos, V. Neutrophil extracellular traps in immunity and disease. Nat. Rev. Immunol. 18 (2), 134–147 (2018).
Brinkmann, V. et al. Neutrophil extracellular traps kill bacteria. Sci. (New York NY). 303 (5663), 1532–1535 (2004).
Takei, H., Araki, A., Watanabe, H., Ichinose, A. & Sendo, F. Rapid killing of human neutrophils by the potent activator phorbol 12-myristate 13-acetate (PMA) accompanied by changes different from typical apoptosis or necrosis. J. Leukoc. Biol. 59 (2), 229–240 (1996).
Farrera, C. & Fadeel, B. Macrophage clearance of neutrophil extracellular traps is a silent process. J. Immunol. (Baltimore Md: 1950). 191 (5), 2647–2656 (2013).
Hakkim, A. et al. Impairment of neutrophil extracellular trap degradation is associated with lupus nephritis. Proc. Natl. Acad. Sci. U.S.A. 107 (21), 9813–9818 (2010).
Behnen, M. et al. Immobilized immune complexes induce neutrophil extracellular trap release by human neutrophil granulocytes via FcγRIIIB and Mac-1. J. Immunol. (Baltimore Md: 1950). 193 (4), 1954–1965 (2014).
Keshari, R. S. et al. Cytokines induced neutrophil extracellular traps formation: implication for the inflammatory disease condition. PloS One. 7 (10), e48111 (2012).
Schorn, C. et al. Monosodium urate crystals induce extracellular DNA traps in neutrophils, eosinophils, and basophils but not in mononuclear cells. Front. Immunol. 3, 277 (2012).
Yalavarthi, S. et al. Release of neutrophil extracellular traps by neutrophils stimulated with antiphospholipid antibodies: a newly identified mechanism of thrombosis in the antiphospholipid syndrome. Arthritis Rheumatol. (Hoboken NJ). 67 (11), 2990–3003 (2015).
Cai, Z. et al. Metformin potentiates nephrotoxicity by promoting NETosis in response to renal ferroptosis. Cell. Discovery. 9 (1), 104 (2023).
Masucci, M. T., Minopoli, M., Del Vecchio, S. & Carriero, M. V. The emerging role of neutrophil extracellular traps (NETs) in tumor progression and metastasis. Front. Immunol. 11, 1749 (2020).
Zhang, S. et al. Immune infiltration in renal cell carcinoma. Cancer Sci. 110 (5), 1564–1572 (2019).
Ye, B. et al. iMLGAM: integrated machine learning and genetic Algorithm-driven multiomics analysis for pan-cancer immunotherapy response prediction. iMeta 4 (2), e70011 (2025).
Ye, B. et al. Navigating the immune landscape with plasma cells: A pan-cancer signature for precision immunotherapy. BioFactors (Oxford England). 51 (1), e2142 (2025).
Dai, S. et al. Intratumoral CXCL13(+)CD8(+)T cell infiltration determines poor clinical outcomes and immunoevasive contexture in patients with clear cell renal cell carcinoma. Journal Immunotherapy cancer 9(2). (2021).
Au, L. et al. Determinants of anti-PD-1 response and resistance in clear cell renal cell carcinoma. Cancer Cell. 39 (11), 1497–1518e1411 (2021).
Tabata, M. et al. Inter- and intra-tumor heterogeneity of genetic and immune profiles in inherited renal cell carcinoma. Cell. Rep. 42 (7), 112736 (2023).
Wettersten, H. I., Aboud, O. A., Lara, P. N. Jr. & Weiss, R. H. Metabolic reprogramming in clear cell renal cell carcinoma. Nat. Rev. Nephrol. 13 (7), 410–419 (2017).
Zhang, Y. et al. A signature for pan-cancer prognosis based on neutrophil extracellular traps. Journal Immunotherapy cancer 10(6). (2022).
Qi, L. et al. Deciphering the role of NETosis-related signatures in the prognosis and immunotherapy of soft-tissue sarcoma using machine learning. Front. Pharmacol. 14, 1217488 (2023).
Kanehisa, M., Furumichi, M., Sato, Y., Matsuura, Y. & Ishiguro-Watanabe, M. KEGG: biological systems database as a model of the real world. Nucleic Acids Res. 53 (D1), D672–d677 (2025).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28 (1), 27–30 (2000).
Kanehisa, M. Toward Understanding the origin and evolution of cellular organisms. Protein Science: Publication Protein Soc. 28 (11), 1947–1951 (2019).
Cheng, W. L. et al. The role of EREG/EGFR pathway in tumor progression. International J. Mol. Sciences 22(23). (2021).
Gu, Z. et al. Aberrant LYZ expression in tumor cells serves as the potential biomarker and target for HCC and promotes tumor progression via csGRP78. Proc. Natl. Acad. Sci. U.S.A. 120 (29), e2215744120 (2023).
Pruenster, M., Vogl, T., Roth, J. & Sperandio, M. S100A8/A9: from basic science to clinical application. Pharmacol. Ther. 167, 120–131 (2016).
Zhang, D. et al. Sijunzi Decoction targets IL1B and TNF to reduce neutrophil extracellular traps (NETs) in ulcerative colitis: evidence from silicon prediction and experiment validation. Drug. Des. Devel. Ther. 17, 3103–3128 (2023).
Dinarello, C. A. Interleukin-1 beta, interleukin-18, and the interleukin-1 beta converting enzyme. Ann. N. Y. Acad. Sci. 856, 1–11 (1998).
Heckmann, B. L., Zhang, X., Xie, X. & Liu, J. The G0/G1 switch gene 2 (G0S2): regulating metabolism and beyond. Biochim. Biophys. Acta. 1831 (2), 276–281 (2013).
Li, Y. et al. Histopathologic and proteogenomic heterogeneity reveals features of clear cell renal cell carcinoma aggressiveness. Cancer Cell. 41 (1), 139–163e117 (2023).
Schödel, J. et al. Hypoxia, Hypoxia-inducible transcription factors, and renal Cancer. Eur. Urol. 69 (4), 646–657 (2016).
Reigle, J. et al. Tobacco smoking induces metabolic reprogramming of renal cell carcinoma. The J. Clin. Investigation 131(1). (2021).
Yipp, B. G. & Kubes, P. NETosis: how vital is it? Blood 122 (16), 2784–2794 (2013).
Vorobjeva, N. V. & Chernyak, B. V. NETosis: molecular mechanisms, role in physiology and pathology. Biochem. Biokhimiia. 85 (10), 1178–1190 (2020).
Thiam, H. R., Wong, S. L., Wagner, D. D. & Waterman, C. M. Cellular mechanisms of NETosis. Annu. Rev. Cell Dev. Biol. 36, 191–218 (2020).
de Bont, C. M., Boelens, W. C. & Pruijn, G. J. M. NETosis, complement, and coagulation: a triangular relationship. Cell Mol. Immunol. 16 (1), 19–27 (2019).
Raftery, M. J. et al. β2 integrin mediates hantavirus-induced release of neutrophil extracellular traps. J. Exp. Med. 211 (7), 1485–1497 (2014).
Demers, M. et al. Cancers predispose neutrophils to release extracellular DNA traps that contribute to cancer-associated thrombosis. Proc. Natl. Acad. Sci. U.S.A. 109 (32), 13076–13081 (2012).
Cedervall, J., Zhang, Y. & Olsson, A. K. Tumor-Induced NETosis as a risk factor for metastasis and organ failure. Cancer Res. 76 (15), 4311–4315 (2016).
Thomson, A. H. Human Recombinant DNase in cystic fibrosis. J. R. Soc. Med. 88 (Suppl 25(Suppl 25), 24–29 (1995).
Poli, V. & Zanoni, I. Neutrophil intrinsic and extrinsic regulation of NETosis in health and disease. Trends Microbiol. 31 (3), 280–293 (2023).
Kazzaz, N. M., Sule, G. & Knight, J. S. Intercellular interactions as regulators of NETosis. Front. Immunol. 7, 453 (2016).
Monteith, A. J., Miller, J. M., Maxwell, C. N., Chazin, W. J. & Skaar, E. P. Neutrophil extracellular traps enhance macrophage killing of bacterial pathogens. Sci. Adv. 7 (37), eabj2101 (2021).
Yipp, B. G. et al. Infection-induced NETosis is a dynamic process involving neutrophil multitasking in vivo. Nat. Med. 18 (9), 1386–1393 (2012).
Fu, J. et al. Large-scale public data reuse to model immunotherapy response and resistance. Genome Med. 12 (1), 21 (2020).
Cristinziano, L. et al. Neutrophil extracellular traps in cancer. Sem. Cancer Biol. 79, 91–104 (2022).
Birebent, R. et al. Surrogate markers of intestinal dysfunction associated with survival in advanced cancers. Oncoimmunology 14 (1), 2484880 (2025).
Liang, Y. et al. NET-Related Gene as Potential Diagnostic Biomarkers for Diabetic Tubulointerstitial Injury. Journal of diabetes research 2024:4815488. (2024).
Sprenkeler, E. G. G. et al. S100A8/A9 is a marker for the release of neutrophil extracellular traps and induces neutrophil activation. Cells 11(2). (2022).
Wang, Y., Zhang, Y., Zhu, Y. & Zhang, P. Lipolytic inhibitor G0/G1 switch gene 2 inhibits reactive oxygen species production and apoptosis in endothelial cells. Am. J. Physiol. Cell. Physiol. 308 (6), C496–504 (2015).
Rébé, C. & Ghiringhelli, F. Interleukin-1β and Cancer. Cancers 12(7). (2020).
Funding
This work was supported by China Postdoctoral Science Foundation (Certificate Number: 2023M731413), Natural Science Foundation of Jiangsu Province (NO: BK20230738),National Natural Science Foundation of China (NO: 82300773), Postgraduate Research & Practice Innovation Program of Jiangsu Province(KYCX23_1952) and Jiangsu Funding Program for Excellent Postdoctoral Talent (NO: 2022ZB727).
Author information
Authors and Affiliations
Contributions
Zijie Yu designed this work. Xi Zhang and Zihao Xu wrote the manuscript. Zijie Yu and Wenchuan Shao performed the bioinformatics analysis. Xinghan Yan, Da Zhong and Tingfei Jiang performed the data review. Yichun Wang provided administrative and financial support. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All patients provided written informed consent, and the study protocol was approved by the The First Affiliated Hospital of Nanjing Medical University ethical committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yu, Z., Xu, Z., Zhang, X. et al. NETosis-based prognostic model reveals immune modulation in clear cell renal cell carcinoma using single-cell and bulk RNA sequencing. Sci Rep 15, 27156 (2025). https://doi.org/10.1038/s41598-025-11095-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-11095-7