Abstract
Age-related hearing loss (ARHL) is associated with an increased risk of dementia, highlighting the need for early interventions to support cognitive functioning. Despite promising evidence supporting transcutaneous auricular vagus nerve stimulation (taVNS) for mitigating cognitive impairment, its impact on working memory (WM) in older adults with ARHL is unexplored. This study is the first attempt to investigate taVNS effects on WM in the older adults with hearing impairment (HI) and with typical hearing (TH). WM capacity was assessed using n-back tasks, varying by WM domains (verbal and visuo-spatial) and complexity levels (1-back and 2-back). Participants underwent a two-session, within-subjects, randomized crossover, single-blind sham-controlled protocol, receiving 20 min of continuous stimulation in the active session, whereas only 30 s at the start and end in the sham session. The HI group performed significantly worse than the TH group on the 2-back tasks. Within the HI group, taVNS significantly enhanced performance across all WM domains and complexity levels compared to the sham condition. These findings suggest that taVNS enhances WM in hearing-impaired older adults, underscoring its potential as a clinical intervention for addressing WM challenges associated with ARHL.
Similar content being viewed by others
Introduction
During the advanced stages of human aging, individuals typically encounter a range of physical and cognitive deteriorations. These changes include modifications in the structural and functional aspects of the auditory system. Consistent evidence from epidemiological studies strongly links sensory loss related to hearing with an elevated risk of developing dementia1,2 with this link becoming more pronounced with age3. The deprivation hypothesis, proposed by Baltes and Lindenberger3 has gained substantial support in explaining these connections4,5,6,7. It posits that prolonged periods of reduced auditory input over time due to untreated hearing impairment (HI) can lead to alterations in neural networks, subsequently affecting cognition and processing speed8. Overall, older adults with HI are now identified as preventative clinical populations in need of early cognitive interventions, given their demonstrated cognitive deficits relative to those with normal hearing9,10.
Given the potential for sensory deprivation to impact cognition, recent evidence from a meta-analysis highlights that treating HI with cochlear implantation (CI) can induce significant improvements in certain cognitive functions in older adults11. Specifically, CI has been shown to enhance executive function and verbal memory—domains closely linked to auditory processing—particularly within the first six months post-implantation, with these gains generally maintained up to 12 months. However, improvements in non-verbal memory, which is less directly associated with auditory input, tend to emerge later and may require additional time or supplementary domain-targeted interventions to achieve meaningful benefits. In some cases, with early-onset or profound HI, where individuals have relied on lipreading, superior visuospatial abilities have been reported12,13. This variability in cognitive outcomes depending on the type and severity of hearing loss suggests that targeted interventions beyond hearing rehabilitation may be essential for optimizing cognitive outcomes in older adults with HI.
Transcutaneous auricular vagus nerve stimulation (taVNS) has garnered recognition for modulating cognition by targeting the auricular branch of the vagus nerve. Research has covered various cognitive domains through taVNS, such as executive functions14 and inhibitory controls15with notable improvements on memory functions16,17,18,19,20,21. A recent study highlighted its potential to improve working memory (WM), particularly in the visuo-spatial n-back task performance, within a cohort of healthy young adults aged 18 to 23 years22. Further, patients with mild cognitive impairment (MCI) exhibited notable improvements in verbal memory functions, including both immediate and delayed recalls, following a 24-week intervention of taVNS23. These studies highlight taVNS as a promising noninvasive approach for improving memory issues and potentially mitigating cognitive decline associated with aging.
Recent studies are increasingly focusing on the link between cognitive decline and age-related hearing loss (ARHL), especially utilizing WM tasks to explore this relationship24,25,26. Previously, a marked correlation was observed between hearing ability, as indexed by peripheral auditory thresholds, and WM functioning in a group of 156 individuals aged 70 and above3. This study highlighted early markers and intervention points for cognitive decline with a specific emphasis on hearing loss in older adults as a possible precursor to dementia. More recently, an EEG study identified this connection by examining the association between hearing loss and WM functions, finding significant correlations between auditory P300 latency and WM capacity in individuals with HI27. Subsequent studies have further supported the idea that impaired hearing can significantly contribute to the deterioration of WM capacity28,29,30 suggesting that targeting cognitive function in older adults with ARHL early on could be a key intervention point to potentially slow further decline.
Extensive research on WM indicates that the specific domains and components of WM being targeted are considered critical when selecting WM tasks to examine individual differences in WM capacity31,32,33. For instance, in WM capacity across verbal and visuo-spatial domains, a study utilizing the digit and corsi span forward tests among patients in the early stages of Alzheimer’s disease (AD) and healthy control subjects found a significant decline in the visuo-spatial WM domain among mild AD patients34. However, the differences between these patients and the control group in the digit span test were minimal. These findings highlight the significance of considering distinct WM domains of incoming information when evaluating WM capacity, particularly evident in cognitively impaired older adults35,36,37.
Evidence from older adults with ARHL suggests that performance differences emerge depending on the WM task types, such as those in the verbal and visuo-spatial domains23,24,25. Some studies employed verbal WM tasks24,25 while others focused on the visuo-spatial domains of WM when studying older adults with ARHL20. The study, which examined the association between hearing ability and cognitive functions among older individuals with and without ARHL, focused on the verbal WM domain using the n-back task with letter presentation. It found that individuals with HI exhibited significantly slower reaction times and fewer correct responses on the 2-back task, although no substantial group differences were observed on the 0-back task37. Another group of researchers reported that individuals with HI exhibit WM deficits in the visuo-spatial domain, even in the absence of specific auditory challenges23,24,25,38. Despite the increasing research on WM deficits for older adults with ARHL, there have been no effort yet to apply the taVNS to improve WM functions for populations at risk of dementia due to ARHL. The current study aims to investigate the effects of taVNS on WM performance by systematically manipulating task complexity (1-back vs. 2-back) and WM domain (verbal vs. visuo-spatial). To the best of our knowledge, this represents the first attempt to examine these effects specifically in older adults with ARHL, a group in need of early cognitive intervention.
Methods
Participants
The study involved 56 participants aged over 60 years, consisting of 20 individuals with HI and 36 typical hearing (TH). All participants, who were native Korean speakers, met the following criteria: they obtained scores within normal ranges on the Korean version of the mini mental state examination (K-MMSE)39 the Seoul verbal learning test (SVLT), the digit span tests, and the Korean geriatric depression scale (KGDS; < 8 out of 15)40. All cognitive assessments were administered as part of the standardized Seoul Neuropsychological Screening Battery-II (SNSB-II)41. None of the participants reported any visual impairments, learning difficulties, or a history of brain injuries.
All experiments were conducted in accordance with relevant guidelines and regulations. This research was approved by the Institutional Review Board on Human Subjects of Ewha Womans University (Approval No. 2022-0084), and all procedures were performed following ethical standards and institutional policies. Prior to participation, all individuals provided written informed consent.
An independent sample t-test was conducted, revealing no statistically significant differences in age, education years, or screening results of neuropsychological tests between the TH and HI groups (all p-values > 0.05). Detailed demographic information and descriptive statistics are provided in Table 1.
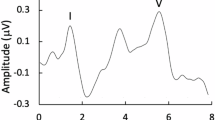
Audiology measurements
Participants with sensorineural hearing loss were assessed using a standard pure-tone audiometry device (AS608 Basic; Interacoustics A/S, Middelfart, Denmark) at audiometric frequencies. A weighted 4-frequency average (W4FA) was calculated using the formula [(a + 2b + 2c + d)/6, where a, b, c, and d represent the thresholds at 0.5, 1.0, 2.0, and 4.0 kHz, respectively], following the clinical guidelines of The Korean Audiological Society42. Participants were classified as having HI if their average hearing threshold in the better ear exceeded 25 decibels hearing level (dB HL)42,43. Only individuals whose hearing threshold differences between the two ears were within 15 dB HL were included. No participants reported using hearing aids or cochlear implants at the time of testing. Audiological reports for each group are detailed in Table 2, with the corresponding audiograms presented in Fig. 1.
Transcutaneous auricular vagus nerve stimulation (taVNS)
We administered stimulation using a commercial taVNS device (allearsTM TODOC, Seoul, South Korea) set at 25 Hz frequency, 200 µs pulse width, and a cycle of 30 s ON and 30 s OFF was repeated. The intensity of the stimulation was adjusted to 0.5 mA below each participant’s pain threshold. The stimulation was calibrated to induce a tingling sensation, indicative of activating the afferent fibers of the auricular vagus nerve44,45 and was targeted at the cymba concha of the ear, a site known for its strong activation of afferent vagal pathways46. The stimulation was applied to either the left or right ear, with counterbalancing across participants.
N-back task
We conducted n-back tasks targeting two distinct WM domains: verbal vs. visuo-spatial. The verbal n-back task was based on the SemBack version47 while the visuo-spatial n-back task was adapted from the study by Christensen and Wright48. To manipulate task complexity, we varied the ‘n’ values (1-back vs. 2-back). The number of task items was matched, with 22 target items out of 73 items in the 1-back condition and 22 targets out of 84 items in the 2-back condition. Each participant engaged in a preparatory block consisting of 10 practice items, including 2 targets, before beginning each n-back task. All task instructions for the n-back tasks were presented visually on the computer screen using written text prior to each task block.
In the verbal n-back task, each word in written form was presented on the screen, and participants were asked to press the spacebar if the current item belonged to the same semantic category as the item presented 1 or 2 back. The semantic categories included three distinct groups: fruits, animals, and clothes (Supplementary 1). The syllable length and structure in Korean were balanced across the three semantic categories.
The visuo-spatial task featured three-dimensional block cubes from Shepard and Metzler49 arranged in various configurations across four blocks. Participants were asked to press the spacebar when the current item matched the shape of the block presented 1 or 2 back.
All the series of stimuli used in this study were presented visually using PsychoPy50 on a 39.6 cm laptop screen (Samsung Galaxy Book Pro 39.6 cm Core™ i5), as illustrated in Fig. 2. Each trial began with the presentation of a fixation cross, which was displayed for 2750 ms, followed by a stimulus presented for 750 ms. Between each stimulus, the fixation cross was consistently displayed for 2750 ms, maintaining a regular interval throughout the experiment.
Experimental protocol
The study employed a two-session, within-subject, randomized crossover, single-blind, sham-controlled design (as detailed in Fig. 3). The two sessions were divided into an active session and a sham session, based on the presence or absence of taVNS stimulation, and the order of stimulation counterbalanced. Participants received both active taVNS and sham stimulation, with each session spaced at least 7 days apart. To ensure consistency, the sessions were preferably conducted at the same time of day.
Prior to each session, participants were instructed to refrain from tobacco (2 h prior), caffeine (6 h prior), medications, alcohol, and intense physical activity (24 h prior). To mitigate potential expectation biases, no information was provided regarding the specific stimulation condition administered in each session or its expected effects.
Experimental protocol for each session depending on stimulation condition. In the sham session (a), stimulation was administered for 30 seconds at the beginning and end of the session. During the active session (b), participants underwent a 15-minute pre-stimulation phase, and then received stimulation until they completed the n-back tasks (20 min), totaling approximately 35 minutes of stimulation.
The order of the verbal- and visuo-spatial n-back was balanced but consistent for individual participants across both sessions. Upon completing the tasks, stimulation ceased, and participants were given a questionnaire regarding any negative effects resulting from the stimulation.
Statistical analysis
Statistical analysis was conducted using Python package (v1.2.0). The dependent variables included accuracy (%) and response time (ms). Accuracy (%) was determined by considering trials where participants correctly responded in the n-back tasks. The number of correct responses were divided by the total number of responses (44) per condition, multiplied by 100 to calculate the percentage of correctly responded trials. Response time (RT)—the duration from the presentation of stimuli on the screen to the moment the button was pressed—was measured in milliseconds (ms). Only trials where participants responded correctly to the n-back tasks were included into the RT analyses.
For each dependent variable, two-separate four-way mixed-design analyses of variance (ANOVAs) were conducted with group (TH vs. HI), stimulation condition (Sham vs. Active), WM domain (Verbal vs. Visuo-spatial), and task complexity (1-back vs. 2-back) as independent variables.
Results
Table 3 displays the descriptive statistics of the verbal and visuo-spatial n-back performance for each group, detailing the accuracy (%) and RT (ms).
Accuracy
Our analysis revealed significant main effects of group (F(1,54) = 18.5, p < 0.001; TH group > HI group), WM domain (F(1,54) = 17.2385, p < 0.001; verbal > visuo-spatial), and task complexity (F(1,54) = 206.1979, p < 0.001; 1-back > 2-back), while stimulation condition did not reach significance (F(1,54) = 2.6406, p = 0.110). Specifically, the accuracy for the HI group was significantly worse compared to the TH counterparts. Furthermore, the accuracy was significantly lower for visuo-spatial than the verbal WM domain, and for the 2-back compared to the 1-back task.
Next, a significant two-way interaction between group (TH vs. HI) and stimulation condition (Active vs. Sham) was observed (F(1,54) = 6.1515, p = 0.016). This was attributed to the fact that, unlike the TH group (91.28% for active vs. 91.95% for sham), the HI group (87.21% for active vs. 83.63% for sham) showed a significantly improved performance in the active condition compared to the sham condition, see Fig. 4a.
Additionally, a significant two-way interaction was observed between group and task complexity (F(1,54) = 17.2221, p < 0.001). This interaction stemmed from the HI group displaying significantly lower accuracy compared to the TH group, specifically during the 2-back task (85.03% for TH vs. 73.29% for HI), see Fig. 4b.
Response time
In the RT analyses, no significant main effects were observed for group (F(1,54) = 0.0170, p = 0.897) or stimulation condition (F(1,54) = 0.7978, p = 0.376). However, significant main effects were found for WM domain (F(1,54) = 17.8593, p < 0.001; verbal > visuo-spatial) and task complexity (F(1,54) = 135.6700, p < 0.001; 1-back < 2-back), indicating that RTs were significantly longer in the 2-back than the 1-back task, and for verbal compared to visuo-spatial WM domain.
Furthermore, a significant two-way interaction was identified between WM domain and task complexity (F(1,54) = 8.3440, p = 0.006). The two-way interaction was attributed to significant differences in the 1-back condition between the verbal and visuo-spatial WM domain (843.36 ms for verbal vs. 745.88 ms for visuo-spatial) compared to those differences in the 2-back (999.95 ms for verbal vs. 916.51 ms for visuo-spatial) (Fig. 5). No other interactions were significant (all p values > 0.05).
Discussion
Our findings are in line with previous research on MCI—recognized as an early stage of dementia—where taVNS showed promising improvements in verbal memory functions21. Given the limited research on the efficacy of taVNS in aging populations, our exploration serves as an important step in highlighting the clinical potential of taVNS, stressing the need for further exploration into its potential to support cognitive function in ARHL as a high-risk group who may be progressing towards dementia.
The previous investigations into the impact of taVNS on WM have been limited to specific domains—namely verbal WM21 or visuo-spatial WM22. Our research extends this scope, demonstrating taVNS’s efficacy across a wider array of WM domains. The current finding suggests that taVNS enhanced WM performance, particularly in terms of accuracy across the WM domains within the HI group. This indicates that taVNS may exert a similar impact on both verbal and visuo-spatial domains in individuals with ARHL. Further research is necessary to extend these WM enhancement effects after taVNS to a broader range of populations at risk.
Another standout in our data is that the significant interaction between group performance and task complexity unveils a clear performance disparity between the HI group and the TH group, especially on the cognitively more challenging 2-back tasks. This distinction is critical as it corroborates the link between ARHL and cognitive decline, aligning with previous studies that have observed differences in n-back task performance among older adults with various cognitive impairments, including MCI51,52 and AD53. Further, patients with amnestic MCI (aMCI) showed comparable performance to that of healthy controls in the 1- and 2-back tasks. However, they exhibited inferior discrimination ability in the 3-back task compared to healthy controls54. Our research highlights the importance of supporting cognitive function in individuals with HI, who are at elevated risk of cognitive decline1,2 rather than solely focusing on addressing hearing loss itself. It pinpoints the cognitive domains affected by ARHL, providing a foundation for developing evidence-based interventions and strategies to support cognitive health targeting WM enhancements.
While the impact of taVNS on the accuracy of WM tasks is evident, RT appears to be relatively unaffected. Our study did not find significant changes in RTs following the application of taVNS. The primary advantage of taVNS, as evidenced in our study, is its significant contribution to boosting decision-making accuracy in WM tasks among older adults with hearing loss. The enhancement in task performance is likely associated with the heightened selective attention induced by taVNS22. However, the effects of stimulation did not extend to accelerating processing speed sufficiently to be reflected in reduced RT. This observation aligns with prior research on taVNS/tVNS effects in verbal word order53 and visuo-spatial22 memory tasks in healthy individuals, where the improvements were noted in task performance without a reduction in RT. However, a study investigating the effect of taVNS on epilepsy patients demonstrated significant decreases in RT due to taVNS55. Highlighting the need for further investigation into the effects of taVNS on processing speed in WM tasks across diverse clinical populations, including ARHL.
The suggested directions for future research are as follows: The average hearing loss in the HI group was classified as mild, with levels around 33 dB HL. Notably, the finding that taVNS effectively elicited WM enhancement even at this mild level of hearing loss is particularly significant. It is important to conduct further research to examine the effects of taVNS across a broader spectrum of hearing loss severities, which would be essential to comprehensively understand its efficacy in populations with more severe levels of hearing loss. Secondly, given that our study concentrated on the immediate effects following a single session of taVNS, this presents a clear rationale for initiating intervention studies involving multiple sessions. Such studies should feature extended intervention periods of taVNS treatment to comprehensively evaluate the long-term therapeutic impacts of taVNS.
Conclusion
The current study provides compelling evidence that individuals with ARHL experience significant memory difficulties in WM tasks compared to those with normal hearing, even when these tasks do not involve auditory challenges. Remarkably, applying taVNS to the HI group led to significant improvements in their WM performance. This finding highlights the potential of taVNS to help slow the trajectory of cognitive decline, particularly by targeting the decrease in WM capacity linked to hearing loss.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Livingston, G. et al. Dementia prevention, intervention, and care: 2020 report of the lancet commission. Lancet 396, 413–446. https://doi.org/10.1016/S0140-6736(20)30367-6 (2020).
Panza, F., Solfrizzi, V. & Logroscino, G. Age-related hearing impairment-a risk factor and frailty marker for dementia and AD. Nat. Rev. Neurol. 11, 166–175. https://doi.org/10.1038/nrneurol.2015.12 (2015).
Lindenberger, U. & Baltes, P. B. Sensory functioning and intelligence in old age: A strong connection. Psychol. Aging 9, 339–355. https://doi.org/10.1037/0882-7974.9.3.339 (1994).
Belin, P., Zatorre, R. J., Hoge, R., Evans, A. C. & Pike, B. Event-related fMRI of the auditory cortex. Neuroimage 10, 417 – 29. (1999). https://doi.org/10.1006/nimg.1999.0480
Oster, C. Sensory deprivation in geriatric patients. J. Am. Geriatr. Soc. 24, 461–464. https://doi.org/10.1111/j.1532-5415.1976.tb03261.x (1976).
Valentijn, S. A. et al. Change in sensory functioning predicts change in cognitive functioning: results from a 6-year follow-up in the Maastricht aging study. J. Am. Geriatr. Soc. 53, 374–380. https://doi.org/10.1111/j.1532-5415.2005.53152.x (2005).
Wong, P. C., Ettlinger, M., Sheppard, J. P., Gunasekera, G. M. & Dhar, S. Neuroanatomical characteristics and speech perception in noise in older adults. Ear Hear. 31, 471–479. https://doi.org/10.1097/AUD.0b013e3181d709c2 (2010).
Baltes, P. B. & Lindenberger, U. Emergence of a powerful connection between sensory and cognitive functions across the adult life span: A new window to the study of cognitive aging?. Psychol. Aging 12, 12–21. https://doi.org/10.1037/0882-7974.12.1.12 (1997).
Dupuis, K. et al. Effects of hearing and vision impairments on the Montreal cognitive assessment. Aging Neuropsychol. Cogn. 22, 413–437. https://doi.org/10.1080/13825585.2014.968084 (2015).
Harrison Bush, A. L., Lister, J. J., Lin, F. R., Betz, J. & Edwards, J. D. Peripheral hearing and cognition: evidence from the staying keen in later life (SKILL) study. Ear Hear. 36, 395–407. https://doi.org/10.1097/AUD.0000000000000142 (2015).
An, S., Jo, E., Jun, S. B. & Sung, J. E. Effects of cochlear implantation on cognitive decline in older adults: A systematic review and meta-analysis. Heliyon 9 https://doi.org/10.1016/j.heliyon.2023.e18762 (2023).
Bavelier, D., Dye, M. W. G. & Hauser, P. C. Do deaf individuals see better? Trends Cogn. Sci. 10, 512–518. https://doi.org/10.1016/j.tics.2006.09.006 (2006).
Rudner, M., Keidser, G., Hygge, S. & Rönnberg, J. Better visuospatial working memory in adults who report profound deafness compared to those with normal or poor hearing: data from the UK biobank resource. Ear Hear. 37, 620–622. https://doi.org/10.1097/AUD.0000000000000339 (2016).
Klaming, R., Simmons, A. N., Spadoni, A. D. & Lerman, I. Effects of noninvasive cervical vagal nerve stimulation on cognitive performance but not brain activation in healthy adults. Neuromodulation 25, 424–432. https://doi.org/10.1111/ner.13313 (2022).
Beste, C. et al. Effects of concomitant stimulation of the GABAergic and norepinephrine system on inhibitory control - A study using transcutaneous vagus nerve stimulation. Brain Stimul. 9, 811–818. https://doi.org/10.1016/j.brs.2016.07.004 (2016).
Giraudier, M., Ventura-Bort, C. & Weymar, M. Transcutaneous vagus nerve stimulation (tVNS) improves high-confidence recognition memory but not emotional word processing. Front. Psychol. 11, 1276. https://doi.org/10.3389/fpsyg.2020.01276 (2020).
Hansen, N. Memory reinforcement and Attenuation by activating the human locus coeruleus via transcutaneous vagus nerve stimulation. Front. Neurosci. 12, 955. https://doi.org/10.3389/fnins.2018.00955 (2019).
Jacobs, H. I., Riphagen, J. M., Razat, C. M., Wiese, S. & Sack, A. T. Transcutaneous vagus nerve stimulation boosts associative memory in older individuals. Neurobiol. Aging. 36, 1860–1867. https://doi.org/10.1016/j.neurobiolaging.2015.02.023 (2015).
Mertens, A. et al. Transcutaneous vagus nerve stimulation does not affect verbal memory performance in healthy volunteers. Front. Psychol. 11, 551. https://doi.org/10.3389/fpsyg.2020.00551 (2020).
Ventura-Bort, C., Wirkner, J., Wendt, J., Hamm, A. O. & Weymar, M. Establishment of emotional memories is mediated by vagal nerve activation: evidence from noninvasive TaVNS. J. Neurosci. 41, 7636–7648. https://doi.org/10.1523/JNEUROSCI.2329-20.2021 (2021).
Wang, L. et al. The efficacy and safety of transcutaneous auricular vagus nerve stimulation in patients with mild cognitive impairment: A double blinded randomized clinical trial. Brain Stimul. 15, 1405–1414. https://doi.org/10.1016/j.brs.2022.09.003 (2022).
Sun, J. B. et al. Transcutaneous auricular vagus nerve stimulation improves Spatial working memory in healthy young adults. Front. Neurosci. 15, 790793. https://doi.org/10.3389/fnins.2021.790793 (2021).
Loughrey, D. G., Parra, M. A. & Lawlor, B. A. Visual short-term memory binding deficit with age-related hearing loss in cognitively normal older adults. Sci. Rep. 9, 12600. https://doi.org/10.1038/s41598-019-49023-1 (2019).
Kestens, K., Degeest, S., Miatton, M. & Keppler, H. Visual and verbal working memory and processing speed across the adult lifespan: the effect of age, sex, educational level, awakeness, and hearing sensitivity. Front. Psychol. 12, 668828. https://doi.org/10.3389/fpsyg.2021.668828 (2021).
Janse, E. & Jesse, A. Working memory affects older adults’ use of context in spoken-word recognition. Q. J. Exp. Psychol. 67, 1842–1862. https://doi.org/10.1080/17470218.2013.879391 (2014).
Nagaraj, N. K. & Atcherson, S. R. Investigating the association between working memory, speech identification in noise, and P300 in adults with hearing impairment. J. Hear. Sci. 7, 1. https://doi.org/10.17430/903455 (2017).
Desjardins, J. L. & Doherty, K. A. Age-related changes in listening effort for various types of masker noises. Ear Hear. 34, 261–272. https://doi.org/10.1097/AUD.0b013e31826d0ba4 (2013).
Pichora-Fuller, M. K. & Singh, G. Effects of age on auditory and cognitive processing: implications for hearing aid fitting and audiologic rehabilitation. Trends Amplif. 10, 29–59. https://doi.org/10.1177/108471380601000103 (2006).
van Boxtel, M. P. et al. Mild hearing impairment can reduce verbal memory performance in a healthy adult population. J. Clin. Exp. Neuropsychol. 22 (200002)22:1;1), 147–154. https://doi.org/10.1076/1380-3395 (2000). -8;FT147.
Alloway, T. P., Gathercole, S. E. & Pickering, S. J. Verbal and visuospatial short-term and working memory in children: are they separable? Child. Dev. 77, 1698–1716 (2006).
Camos, V. Domain-specific versus domain-general maintenance in working memory: reconciliation within the time-based resource sharing model. Psychol. Learn. Motiv. 67, 135–171. https://doi.org/10.1016/bs.plm.2017.03.005 (2017).
Kane, M. J. et al. The generality of working memory capacity: a latent-variable approach to verbal and visuospatial memory span and reasoning. J. Exp. Psychol. Gen. 133, 189–217. https://doi.org/10.1037/0096-3445.133.2.189 (2004).
Orsini, A., Trojano, L., Chiacchio, L. & Grossi, D. Immediate memory spans in dementia. Percept. Mot Skills. 67, 267–272. https://doi.org/10.2466/pms.1988.67.1.267 (1988).
Carlesimo, G. A., Fadda, L., Lorusso, S. & Caltagirone, C. Verbal and Spatial memory spans in alzheimer’s and multi-infarct dementia. Acta Neurol. Scand. 89, 132–138. https://doi.org/10.1111/j.1600-0404.1994.tb01648.x (1994).
Egerházi, A., Berecz, R., Bartók, E. & Degrell, I. Automated neuropsychological test battery (CANTAB) in mild cognitive impairment and in alzheimer’s disease. Prog Neuropsychopharmacol. Biol. Psychiatry. 31, 746–751. https://doi.org/10.1016/j.pnpbp.2007.01.011 (2007).
Kessels, R. P., Meulenbroek, O., Fernández, G. & Olde Rikkert, M. G. Spatial working memory in aging and mild cognitive impairment: effects of task load and contextual cueing. Aging Neuropsychol. Cogn. 17, 556–574. https://doi.org/10.1080/13825585.2010.481354 (2010).
Völter, C., Gotze, L., Falkenstein, M., Dazert, S. & Thomas, J. P. Application of a computer-based neurocognitive assessment battery in the elderly with and without hearing loss. Clin. Interv Aging. 12, 1681–1690. https://doi.org/10.2147/CIA.S142541 (2017).
Somnath, A., Gundmi, A., Bhargavi, P. G. & Rai, S. Comparison of cognitive functions in elderly population with and without hearing loss. Indian J. Otolaryngol. 26, 163–167. https://doi.org/10.4103/indianjotol.INDIANJOTOL_65_19 (2020).
Kang, Y. A normative study of the Korean-Mini mental state examination (K-MMSE) in the elderly. Korean J. Psychol. Gen. 25, 1–12 (2006).
Jung, I. K., Kwak, D. I., Joe, S. H. & Lee, H. S. A study of standardization of Korean form of geriatric depression scale (KGDS). Geriatr. Psychiatry Med. 1, 61–72 (1997).
Kang, Y., Jahng, S. & Na, D. L. Seoul neuropsychological screening battery (SNSB-II). 2nd Edn. Seoul: Human Brain Research & Consulting Co.; Seoul, Korea (2012).
The Korean Audiological Society. National Clinical Guidelines for Audiologyp. 39 (The Korean Audiological Society, 2019).
World Health Organization. Report of the Informal Working Group on Prevention of Deafness and Hearing Impairment Programme Planning: Geneva, 18–21 June 1991 (World Health Organization, 1991).
Ben-Menachem, E., Revesz, D., Simon, B. J. & Silberstein, S. Surgically implanted and non-invasive vagus nerve stimulation: A review of efficacy, safety, and tolerability. Eur. J. Neurol. 22, 1260–1268. https://doi.org/10.1111/ene.12629 (2015).
Yuan, H. & Silberstein, S. D. Vagus nerve and vagus nerve stimulation: a comprehensive review: part II. Headache 56, 259–266. https://doi.org/10.1111/head.12650 (2016).
Yakunina, N., Kim, S. S. & Nam, E. C. Optimization of transcutaneous vagus nerve stimulation using functional MRI. Neuromodulation 20, 290–300. https://doi.org/10.1111/ner.12541 (2017).
Wright, H. H., Downey, R. A., Gravier, M., Love, T. & Shapiro L. P. Processing distinct linguistic information types in working memory in aphasia. Aphasiology 21, 802–813. https://doi.org/10.1080/02687030701192414 (2007).
Christensen, S. C. & Wright, H. H. Verbal and non-verbal working memory in aphasia: what three n-back tasks reveal. Aphasiology 24, 752–762. https://doi.org/10.1080/02687030903437690 (2010).
Shepard, R. N. & Metzler, J. Mental rotation of three-dimensional objects. Science 171, 701–703. https://doi.org/10.1126/science.171.3972.701 (1971).
Peirce, J. W. PsychoPy—psychophysics software in Python. J. Neurosci. Methods. 162, 8–13 (2007).
Borkowska, A., Drozdz, W., Jurkowski, P. & Rybakowski, J. K. The Wisconsin card sorting test and the N-back test in mild cognitive impairment and elderly depression. World J. Biol. Psychiatry. 10, 870–876. https://doi.org/10.1080/15622970701557985 (2009).
Guild, E. B. et al. Dynamic working memory performance in individuals with single-domain amnestic mild cognitive impairment. J. Clin. Exp. Neuropsychol. 36, 751–760. https://doi.org/10.1080/13803395.2014.941790 (2014).
Fraga, F. J. et al. Early diagnosis of mild cognitive impairment and alzheimer’s with event-related potentials and event-related desynchronization in N-back working memory tasks. Comput. Methods Programs Biomed. 164, 1–13. https://doi.org/10.1016/j.cmpb.2018.06.011 (2018).
Kaan, E. et al. C. A transcutaneous vagus nerve stimulation study on verbal order memory. Neurolinguistics 59, 100990. https://doi.org/10.1016/j.jneuroling.2021.100990 (2021).
Pan, L. et al. Transcutaneous auricular vagus nerve stimulation improves working memory in Temporal lobe epilepsy: A randomized double-blind study. CNS Neurosci. Ther. 30, e14395. https://doi.org/10.1111/cns.14395 (2024).
Funding
This work was supported by the National Research Foundation of Korea (NRF) grants funded by the Ministry of Science and ICT (MSIT) (No. 2022R1A2C2005062, RS-2024-00461617), by the NRF grant funded by the Ministry of Education (MOE) (No. NRF-2022R1I1A4063209), and by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health and Welfare (No. HI23C0156).
Author information
Authors and Affiliations
Contributions
J.S. conceptualized the study, conducted formal analysis, designed the methodology, and visualized the results. She also wrote the original draft of the manuscript. S.N. and J.P. were responsible for data curation, investigation, and writing—review & editing. S.B.J. and J.E.S. contributed to the study’s conceptualization, funding acquisition, and supervision, and they also participated in writing—review & editing. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors state that they have no known competing financial interests or personal relationships that could appear to have influenced the work presented in this paper.
Generative AI and AI-assisted technologies
During the preparation of this work the author(s) used [ChatGPT 4.0] to [improve readability and check for grammar corrections]. After using this tool/service, the author(s) reviewed and edited the content as needed and take(s) full responsibility for the content of the publication.
Ethics approval and consent to participate
This research was approved by the Institutional Review Board on Human Subjects of Ewha Womans University (No. 2022-0084). Prior to participation, all individuals provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shin, J., Noh, S., Park, J. et al. Transcutaneous auricular vagus nerve stimulation enhanced working memory in older adults with age-related hearing loss. Sci Rep 15, 26629 (2025). https://doi.org/10.1038/s41598-025-11363-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-11363-6