Abstract
Aneurysmal subarachnoid hemorrhage (aSAH) is a life-threatening condition with high morbidity and mortality. Early prediction of prognosis remains challenging. This study aimed to develop a nomogram incorporating clinical and inflammatory biomarkers to predict short-term outcomes in postoperative aSAH patients. Thus optimizing the intervention strategy and improve patient quality of life. Logistic regression analysis was used to determine the single predictor of aneurysmal subarachnoid hemorrhage. Based on these independent predictors, a nomogram was created in R studio. The results showed that the aneurysmal site (3.35[95% CI, 1.05–10.66], P = 0.041), affected side (3.77[95% CI, 1.17–12.11], P = 0.026), hydrocephalus (0.03[95% CI, 0.01–0.12], P < 0.001), Hunt-Hess grade (4.13[95% CI, 1.17–14.49], P = 0.027), GCS score (4.08[95% CI, 1.02–16.25], P = 0.046), hypertension history (0.18[95% CI, 0.06–0.55], P = 0.003), WBC (3.49[95% CI, 1.06–11.56], P = 0.04), MLR (0.33[95% CI, 0.12–0.92], P = 0.035) were independent predictors. The nomogram demonstrated superior predictive accuracy compared to existing models, with lower calibration errors (training group: 0.018; validation group: 0.052) and high AUC values (0.95 and 0.901, respectively). Given the class imbalance (84.3% of patients had favorable outcomes), sensitivity analyses were performed to verify the consistency and reliability of the findings. The nomogram constructed based on aneurysm location, affected side, presence of hydrocephalus, Hunt-Hess grade, GCS score, hypertension, WBC and MLR can enables clinicians to identify high-risk aSAH patients early, facilitating targeted interventions such as anti-inflammatory therapy or hydrocephalus management. This tool may improve resource allocation and reduce disability rates in critical care settings. Thus optimizing the intervention strategy and improve patient quality of life.
Similar content being viewed by others
Introduction
Subarachnoid hemorrhage (SAH) is an acute cerebrovascular disease that seriously damages the central nervous system. It has pathophysiological effects on multiple organs of the body, resulting in high mortality and morbidity1]– [2. Hypertensive arteriosclerosis is the most common cause, followed by ruptured brain aneurysms. Current surgical methods include aneurysmal clipping and intravascular therapy. However, there are many complications during treatment, such as increased intracranial pressure, seizure, hyponatremia, delayed cerebral ischemia, etc., which can be life-threatening in severe cases3,4,5,6. Although the diagnosis and treatment of aSAH patients and the careful management of the intensive care unit (ICU) have improved significantly in recent years, the prognosis of ASAH patients is still the most concerned issue7]– [8. According to existing studies, patients with aSAH after surgery have a poor prognosis. Therefore, predicting prognostic outcomes is of great value in the treatment selection and evaluation of aSAH patients.
Current prognostic tools for aSAH primarily rely on clinical scales (e.g., Hunt-Hess, WFNS), yet emerging evidence highlights systemic inflammation as a key driver of secondary brain injury. Such as leukocytes, neutrophils, hypersensitive C-reactive protein, fibrinogen, etc., can be used as strong predictors for predicting the prognosis of patients with aSAH. These factors increase significantly after the occurrence of aSAH and are closely related to the severity of the disease and poor prognosis9,10,11,12,13. However, current changes in a single indicator may not provide clinicians with strong and sufficient clinical evidence to diagnose the disease. Predictive models are derivative statistical tools that help predict prognostic outcomes based on aggregated assessments of physical, laboratory, and radiological tests. High-quality predictive models can guide bedside decisions and patient consultations, ensure that resources are appropriately allocated to reduce healthcare costs, and improve the design and analysis of clinical trials. The establishment of a production model may be beneficial for the management of aSAH patients. Nomograms, as visual predictive tools, integrate multiple variables to estimate individualized risks and have been increasingly adopted in neurocritical care14. For example, Dongzhou Zhuang et al. have developed a dynamic nomogram for predicting poor prognosis after aSAH15. Xiao Jin et al. used serological indicators to construct a nomogram model of postoperative pneumonia after16. Xin Feng et al. developed and validated a novel nomogram for predicting aneurysm rupture in patients with multiple intracranial aneurysms17.
Therefore, this study aimed to collect clinical data, including baseline data, blood and inflammatory factor levels, of postoperative patients with aSAH through a two-center retrospective analysis and construct a nomogram model to predict the short-term prognosis of postoperative patients. Through this model, doctors can more accurately evaluate the recovery of patients and provide a scientific basis for clinical decision-making.
Materials and methods
Patient section
This is a two-center retrospective cohort study from China. The study included patients diagnosed with aSAH at two large medical centers in China between January 2020 and January 2024. Inclusion criteria are as follows: (1) Patients diagnosed aSAH by CTA, MRA or DSA; (2)Age > 18 years old; (3)After surgical treatment; The exclusion criteria are as follows: (1)Age below 18 years; (2)The admission blood drawing index is not perfect; (3)Recent use of hormones and other drugs; (4)Combined immune system and blood system diseases; (5)Excluding non-aneurysmal diseases, such as cerebral arteriovenous malformation, moyamoya disease, craniocerebral trauma, etc.; (6)No surgical treatment was performed. In this study, patients meeting the criteria in Huizhou Central People’s Hospital and Gaozhou People’s Hospital were summarized, and the patients were randomly divided into training groups and verification groups at a ratio of 7:3. Data access was restricted to authorized researchers, and the study complied with China’s Personal Information Protection Law (PIPL). The study has been approved by the Committee of Huizhou Central People’s Hospital, and due to the retrospective nature of the study, the Huizhou Central People’s Hospital Ethics Review Committee waived the need of obtaining informed consent. It complies with the Declaration of Helsinki and the Chinese Measures for Ethical Review of Biomedical Research Involving People.
Data collection and definition
This study collected baseline clinical data, blood routine, biochemistry, coagulation function, liver function, procalcitonin, and other test results. Baseline clinical data included gender, age, site, affected side, history of hypertension, diabetes, alcohol abuse, smoking, hydrocephalus, cerebral infarction, surgical method, Hunt-Hess grade, Fisher grade, Glasgow Coma Score(GCS) score, WFNS grade, etc. Laboratory parameters included hematological indices (e.g., white blood cell count, platelet count), biochemical markers (e.g., creatinine, albumin), and inflammatory ratios (NLR, MLR), etc. We compared the baseline data of the training and validation groups to verify the comparability of the data between the two groups.
Then, We calculated the inflammatory biomarker ratio using the following equation: NLR = neutrophil count/lymphocyte count, dNLR = neutrophil count/(white blood cell count - lymphocyte count), MLR = monocyte count/lymphocyte count, NMLR= (monocyte count + neutrophil count)/lymphocyte count, PLR = Platelet count/lymphocyte count, NHR = neutrophil count ratio/high-density lipoprotein, MHR = monocyte count/high-density lipoprotein, LHR = lymphocyte count/high-density lipoprotein, PHR = Platelet count/high-density lipoprotein, Systemic Inflammatory Response Index (SIRI) = neutrophil count × monocyte Count/lymphocyte count, systemic immunoinflammatory index (SII) = platelet count × neutrophil count/lymphocyte count, Systemic inflammatory index (AISI) = neutrophil count × platelet count × monocyte count/lymphocyte count, triglyceride-glucose index (TyG) = In{(fasting triglyceride × fasting blood glucose) /2}, glucose triglyceride /BMI index (TYG-BMI) = TyG/BMI.
Outcome
In this study, the Glasgow Outcome Scale (GOS) score was assessed 6 months post-discharge to evaluate short-term prognosis. Follow-up evaluations can through outpatient visits or telephone interviews. A GOS score > 3 indicates a good prognosis, while a GOS score ≤ 3 indicates a poor prognosis.
Statistical analysis
In this study, we first generate a table of random numbers using a simple random method with the PROC PLAN procedure statement of SAS 9.4 statistical software: 01,02,03,… According to this allocation method, 600 was allocated to the two groups according to a random number table, in which the training set was 420, and the verification set was 180. Patients were numbered from 01 to 600 successively according to the medical record number and finally assigned to the corresponding group according to the group planned by the number. Then, SPSS21.0 (SPSS Inc., Chicago, IL) was used to compare the baseline data between the training group and the validation group. Secondly, the data of the training group was divided into good and bad prognoses, and the clinical data and test results were compared between the groups. The Shapiro normality test was used to determine the normality of continuous data. If the data fit the normal distribution, the data were represented by mean ± standard deviation. Independent univariate ANOVA was used to compare the groups. If the normal distribution did not conform, the data were expressed by the median (25% quantile, 75% quantile), and the Kruskal-Wallis test was used to compare groups. Frequency (percentage) was used to describe categorical data, and the Chi-square or Fisher’s exact test was used to compare groups. The difference was considered statistically significant when the bilateral p-value was less than 0.05.
Logistic regression analysis was performed on all clinical data in the training group, and the mean was used as the dividing point for binary classification processing. More significant than the mean was defined as 1, and less than the mean was defined as 2. Then, univariate logistic regression analysis was performed. Factors with p < 0.1 in univariate analysis were included in multivariate logistic regression analysis to evaluate independent predictors of prognosis. For variable selection criteria, variables with p-value < 0.1 in univariate analysis were included in the multivariate logistic regression analysis, screened by stepwise regression (backward method), and finally retained independent predictors with p < 0.05 to construct the nomogram. For example, although age was significant in the univariate analysis (p = 0.001), it was excluded in the multivariate analysis due of collinearity with other variables.
Using R Studio (v4.2.2), a nomogram was constructed based on independent predictors. Model performance was evaluated via ROC curves (AUC), calibration plots (mean error), and decision curve analysis (DCA). Decision Curve Analysis (DCA) analyzed the model’s clinical benefit. All tests are bidirectional, and a P-value of less than 0.05 is considered significant.
To evaluate the robustness of the model, we conducted sensitivity analyses using two approaches: (1) applying random undersampling to balance the outcome classes, followed by re-running the entire logistic regression modeling process; and (2) evaluating alternative machine learning algorithms (Random Forest and Gradient Boosting) for comparative analysis. The consistency of predictors and model performance metrics (ROC, PR, calibration) was assessed.
Result
Prognostic relationship between clinical factors and aSAH
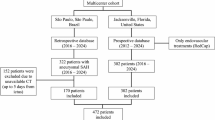
In this study, a total of 692 patients diagnosed with aSAH were collected from two large medical centers. A total of 92 patients were excluded due to the above factors, and 600 patients were finally included in a retrospective study, as shown in Fig. 1. There were 420 patients in the training set and 180 patients in the validation set. Patients with incomplete blood index at admission (92 cases) were excluded, and the proportion of missing data was 13.3% (92/692). All the analyses were based on the complete data, and no imputation method was used. Due to the low proportion of deletions and the random deletions, the impact on the results was limited.
The baseline data of the two groups were compared between the two groups. In the training set, there were 174 males (41.43%), median age 56 years [IQR:49,64], 145 patients (34.52%) with responsible aneurysms located in the internal carotid artery segment, and 202 patients (48.10%) with left-side aneurysms. There were 339 cases (80.71%) of aneurysm embolism, 305 cases (72.62%) of Hunt-Hess grade 1–2 and 261 cases (62.14%) of Fisher grade 1–2. There were 366 cases (87.14%) with a GCS score of 9–15, 319 cases (75.95%) with WFNS grade 1–3, 123 cases (29.29%) with hydrocephalus. Among them, the patients with hypertension, diabetes, smoking, alcoholism and cerebral infarction were 210 cases (50.00%), 27 cases (6.43%), 81 cases (19.29%), 19 cases (4.52%) and 27 cases (6.43%), respectively. There was no statistical difference in baseline data between the two groups (p > 0.05), indicating that the data were comparable (Table 1).
We then compared the data from the training group. The results showed that hydrocephalus, surgical method, Hunt-Hess scale, Fisher scale, GCS score, WFNS scale, history of hypertension, history of cerebral infarction, age, BMI, D-dimer, FBG, TP, Alb, The differences among PCT, ALT, AST, Urea, Cl, Ca, MLR, SIRI and AISI were statistically significant. (Table 2).
We included all clinical factors in the training group into univariate logistic regression analysis, and the results showed that hydrocephalus, surgical method, Hunt-Hess rating, Fisher rating, GCS score, WFNS classification, history of hypertension, history of cerebral infarction, age, BMI, D-dimer, FBG, TP, Alb, PCT, ALT, AST, Urea, Cl, Ca, MLR, SIRI, AISI were all predictors of short-term prognosis. We then included the factors with p < 0.1 in the single factor into the multivariate binary logistic regression analysis. The results showed that the aneurysmal site (3.35[95% CI, 1.05–10.66], P = 0.041), affected side (3.77[95% CI, 1.17–12.11], P = 0.026), hydrocephalus (0.03[95% CI, 0.01–0.12], P < 0.001), Hunt-Hess grade (4.13[95% CI, 1.17–14.49], P = 0.027), GCS score (4.08[95% CI, 1.02–16.25], P = 0.046), hypertension history (0.18[95% CI, 0.06–0.55], P = 0.003), WBC (3.49[95% CI, 1.06–11.56], P = 0.04), MLR (0.33[95% CI, 0.12–0.92], P = 0.035) were independent predictors (Table 3).
Nomogram construction and evaluation
Based on multivariate analysis, a nomogram incorporating aneurysm location, affected side, hydrocephalus, Hunt-Hess grade, GCS score, hypertension, WBC, and MLR was developed using R Studio (Fig. 2).
We used R studio software to verify the predictive efficacy of patient nomograms. The ROC curve of the training group (FIG. 3A) suggested that the C index was 0.95 and the confidence interval was (0.929–0.972), while the ROC curve of the verification group (FIG. 3B) suggested that the C index was 0.901 and the confidence interval was (0.849–0.953), showing good prediction efficiency. The calibration curve of the training group (FIG. 4A) showed that the predicted value of the model was consistent with the observed value, with an average error of 0.018; the verification group (FIG. 4B) showed that the expected value of the model was consistent with the observed value, with an average error of 0.052. The DCA curve of the training group (FIG. 5A) suggested that the threshold value was between 0.01 and 0.98, and the DCA curve of the verification group (FIG. 5B) indicated that the threshold value was between 0.04 and 0.91, and the clinical benefit was good.
It is not difficult to see that the prognostic nomogram we constructed showed good predictive efficacy in both the training and validation groups, with minor errors, and could benefit most clinical patients.
Sensitivity analysis
The favorable prognosis group (n = 354) and the poor prognosis group (n = 66) showed a significant imbalance (5.4:1). To rigorously evaluate the potential impact of this imbalance on our findings, we implemented a comprehensive sensitivity analysis approach:
First, we performed random undersampling of the majority class to create a balanced dataset (1:1 ratio). When we reapplied logistic regression to this balanced cohort, the model consistently identified the same key predictors: MLR, WBC, hydrocephalus, Hunt-Hess grade, and GCS score. Importantly, both discrimination metrics (AUC-ROC:=0.967; AUC-PR:=0.968) and calibration performance remained strong (Table 4; Fig. 7), demonstrating the robustness of our original findings.
Machine learning model results. Data 6 A Random Forest Feature Importance: Hydrocephalus (41.6%). GCS (23%). Hunthess (15.9%). Hypertension (9.7%). WBC (3.5%). MLR (3.5%). Position (2.2%). Side (0.6%). Data 6 B Gradient Boosting Feature Importance: Hydrocephalus (39.4%). GCS (27.4%). WBC (10.5%). MLR (10%). Hunthess (5.6%). Hypertension (4.6%). Side (1.5%). Position (1.1%).
Furthermore, we conducted internal validation using random forest and gradient boosting machine models, both of which are more robust to class imbalance. Variable importance rankings derived from these models were highly consistent with the logistic regression results. Notably, GCS score and hydrocephalus consistently ranked as the top two predictors across all models (Fig. 6; Data 6 A; Data 6B).
These findings support the stability of the identified predictors and reinforce the clinical relevance of our nomogram under varied modeling strategies (Fig. 7).
Discussion
In an in-depth study and review of the published literature on the prognosis of patients with aSAH, we can find some standard features and factors. Specifically, men of older age, combined hypertension, a history of smoking, alcohol abuse, and poor scores on admission were more likely to have a poor prognosis. In addition, those patients with underlying diseases such as coronary heart disease, liver and kidney disease, and cerebral infarction are also more likely to face the risk of adverse prognosis. Therefore, we have considered including these factors in the analysis before conducting a multi-factor regression analysis, intending to minimize the impact of these potential confounders on the results.
After careful analysis and research, we came up with some significant findings. The results showed that aneurysmal location, affected side, presence or absence of hydrocephalus, Hunt-Hess grade, GCS score, hypertension, WBC, and MLR were all independent predictors of short-term poor prognosis in patients after aSAH. Based on these findings, we built a nomogram prediction model that can help doctors and researchers predict patient outcomes more accurately, providing strong support for clinical decision-making.
Previous studies have shown that patients with high Hunt-Hess grades and low GCS scores at the onset of disease tend to have poor predictive outcomes and high disability and mortality rates. The Hunt-Hess scale is a crucial indicator for assessing the degree of neurological damage and level of consciousness in patients with aSAH. It is divided into I-V scales. To a large extent, this rating directly indicates the severity of the disease. For patients with Hunt-Hess grades I to III, early surgical intervention is usually recommended because these patients have less blood loss and are relatively mild. Most patients can obtain a good prognosis with the active intervention of emergency surgery. However, for patients with Hunt-Hess grade IV-V intracranial aneurysms, the clinical prognosis is generally poor, whether surgical or conservative treatment is selected. Most of these patients will receive conservative treatment first and then consider further surgical intervention when the condition is stabilized. Numerous studies have shown that the higher the Hunt-Hess rating in aSAH patients, the higher the risk of poor prognosis18,19,20. Similarly, the GCS has been recognized as a clinical assessment tool worldwide and is of great significance for predicting patient outcome21,22,23. Although age was associated with prognosis in univariate analyses, its effect was overwritten in multivariate models by measures such as Hunt-Hess grading, GCS score, and MLR, suggesting that age may indirectly influence prognosis by influencing neurofunctional status or inflammatory responses.In addition, high blood pressure is also an independent risk factor. Long-term hypertension will lead to arterial wall damage and increase the risk of aneurysm rupture. Secondly, the vascular regulation function of hypertensive patients is impaired, which affects the recovery after bleeding24. Hypertensive patients also may co-exist with other cardiovascular and cerebrovascular diseases, such as coronary heart disease and heart failure, which further increases the risk of poor prognosis.
Furthermore, it is not difficult to find that the specific location and affected side of the aneurysm also have an important impact on the prognosis of patients25. For example, the rupture risk and treatment difficulty of internal carotid aneurysms, middle cerebral aneurysms, anterior communicating aneurysms, posterior communicating aneurysms and basal aneurysms are different, and the symptoms produced by different parts of the damage are different, and these differences are directly related to the recovery degree and survival rate of patients. Compared with most people, the left side of the brain is the dominant hemisphere, with extremely important functions, and has a huge regulatory role in the language, action, understanding and cognitive functions of patients, while bleeding on the right side may lead to emotional indifference, memory disorders and other manifestations. However, the specific prognosis still needs to be combined with factors such as blood loss, aneurysm size, shape, patient age and basic health status.
Hydrocephalus is a common and severe complication of aSAH, and about 20–30% of people with aSAH will develop acute hydrocephalus due to impaired circulation or abnormal absorption of cerebrospinal fluid. Its mechanism may be because the blood clot prevents the average circulation of cerebrospinal fluid, or the blood affects the arachnoid particles, leading to the decrease of cerebrospinal fluid reabsorption or the excessive secretion of cerebrospinal fluid and other reasons, which can cause brain tissue displacement and injury by increasing intracranial pressure. Acute hydrocephalus will not only aggravate the early neurological damage of aSAH patients, further aggravate the clinical condition, but also damage the neurological function of patients in the recovery period after aSAH surgery26. Han-Yu Huang et al. established a column graph model for clinical outcomes of patients with severe subarachnoid hemorrhage and proposed that systemic inflammatory response and complications unrelated to surgery after SAH, especially hydrocephalus, delayed cerebral ischemia and pneumonia, may be important risk factors leading to poor prognosis in patients with severe SAH27. At the same time, Nicolai Maldaner et al. established hemorrhage, age, treatment, clinical status, and hydrocephalus (HATCH) scores and verified that HATCH scores were strong independent predictors of functional prognosis. Incorporating it into daily practice may benefit patient care in aSAH28.
In addition, a large number of studies have verified that hydrocephalus is a predictor of poor prognosis and is closely related to inflammation6,29,30. In patients with aSAH complicated with hydrocephalus, due to the damaged cerebrospinal fluid circulation pathway, the secretion or absorption of cerebrospinal fluid is unbalanced, which leads to the accumulation of inflammatory cells in the subarachnoid space and further exacerbates the inflammatory response. Various studies have proved that early systemic inflammatory changes are the prognosis factors affecting aSAH31. Inflammation runs through the whole process of aSAH injury mechanism32. When the aneurysm ruptures, the blood deposited in the subarachnoid space stimulates brain tissue and activates immune regulatory cells in the central nervous system, and a large number of inflammatory cells enter the subarachnoid space, rapidly causing inflammation33]– [34. The inflammatory response can activate the immune system to release inflammatory cells and inflammatory mediators, such as cytokines, adhesion molecules and chemokines, leading to the occurrence and development of cerebrovascular spasm, exacerbating the occurrence of brain injury and affecting the prognosis of patients35,36,37,38. For example, WBC studies have shown that aSAH can trigger brain injury and delayed cerebral ischemia by stimulating systemic cellular response, which will lead to an increase in the number of white blood cells39]– [40, while the growth and rupture of brain aneurysms are promoted by leukocyte infiltration and inflammatory response in the aneurysm wall41. Moreover, the thinning of the aneurysm wall is related to leukocytosis42. Similarly, higher white blood cell counts are associated with hematoma growth and early neurological deterioration43. Therefore, there is a significant relationship between high and low white blood cell count and the prognosis of patients.
Combined with previous studies, we found that MLR can predict the course of many diseases, such as diabetes, depression, heart disease, etc44,45,46,47,48,49,50,51. In our study, we found that MLR is closely related to the short-term prognosis of patients after aSAH, which has not been found in the past. We found that high levels of MLR may increase the risk of a poor prognosis six months after surgery. From previous studies, we can see that monocytes, which originate from bone marrow and circulate in the bloodstream52, are critical components of the innate immune system and play a vital role in the initiation, regulation and resolution of inflammation through cytokine production and antigen presentation53. aSAH can also trigger early monocyte activation54. In a study by Walsh et al., absolute monocyte counts were independently associated with 30-day mortality in 240 adult patients with cerebral hemorrhage (ICH)55. In a previous study by Mackey et al., elevated monocyte count was also an independent risk factor for 30-day death from disease56. In addition, a previous study calculated the lymphocyte to monocyte neutrophil (L/MN) gene list darr ratio in patients with aneurysms. It demonstrated that lower values were significantly associated with mortality during hospitalization. Therefore, it can also be concluded that monocyte and neutrophil activity increases after aSAH while lymphocyte response decreases57. Therefore, the greater the MLR ratio, the worse the prognosis of patients, which is consistent with the results of our study. It is important to note that the process of early brain injury, vasospasm, and delayed cerebral deficiency is actually complex and multifactorial. These processes may involve other mechanisms and pathways that interact with inflammatory pathways and monocytes58. This needs to be further studied.
Since the prevention and treatment of aSAH are of great clinical significance, it is necessary to evaluate the prognosis of patients as early as possible. Therefore, the development of the nomogram of adverse prognostic factors of aSAH has become a hot topic for many scholars in recent years. However, at present, there is no nomographic map for poor prognosis of patients with aSAH based on aneurysm location, affected side, hydrocephalus, Hunt-Hess grade, GCS score, hypertension, WBC and MLR. Meanwhile, the nomographic map in this study has good predictive performance. The construction of a nomogram based on the blood test results of patients admitted to the hospital can achieve clinical benefits for a large proportion of patients. Compared to the HATCH score (AUC = 0.82)28 and the FRESH score (AUC = 0.87)59, our nomogram achieved higher discriminative ability (AUC = 0.95). For another example, compared with the dynamic nomogram (AUC = 0.86) developed by Zhuang et al. (2023)15, the AUC of the training set and validation set of this model is 0.95 and 0.90, respectively, showing a higher degree of differentiation. Unlike previous models, we incorporated inflammatory biomarkers (e.g., MLR) and hydrocephalus status, which may enhance predictive accuracy for short-term outcomes. Beside, decision curve analysis (DCA) shows that the model provides a net benefit for clinical decisions when the threshold probability is in the range of 0.01 to 0.98. For example, if the physician thinks the probability of a poor patient prognosis exceeds 20% (threshold = 0.2), using this model can significantly reduce unnecessary interventions while avoiding missing high-risk patients. This implies that clinicians can confidently use the model to stratify high-risk patients for early interventions, even when varying the acceptable risk thresholds for treatment.
In this study, the model was constructed based on the data from two medical centers in China, and the internal validation set was conducted (AUC = 0.901), indicating that the model has good generalization ability. However, because the sample source is limited in southern China, the external validation in more geographical and ethnic populations is needed in the future to further confirm the universality of the model. Although individual factors (e.g. -Hunt-Hess grade, GCS score) have been reported as predictors of SAH outcome, for the first time integrated aneurysm location, affected side, hydrocephalus, hypertension, WBC, and MLR into one nomogram model. This multi-dimensional integration enables a more comprehensive assessment of short-term patient outcomes, providing an intuitive quantification tool for the clinic.
This study also has some advantages: (1) As a two-center retrospective study from China, the nomogram was verified by an external validation set, the model was reliable, and the application was simple and convenient; (2) The purpose of this study is to collect the relevant data of patient admission, so as to achieve the very early prediction and strive to benefit more patients; (3) However, this study also has some disadvantages: (1) patients have a certain rate of lost follow-up; (2) The center and data volume can be further expanded; (3) As a retrospective study, selection bias may be information bias (such as some confounders not documented). Imbalance in outcome categories is also the main limitation. Although sensitivity analyses supported the robustness of the main findings, future prospective, multi-center studies with a more balanced sample distribution are recommended. Despite the bias reduction through a multicenter design and strict exclusion criteria, future prospective studies are needed to verify the robustness of the model.
Conclusion
The nomogram constructed based on aneurysm location, affected side, presence of hydrocephalus, Hunt-Hess grade, GCS score, hypertension, WBC and MLR can help clinicians to identify high-risk aSAH patients early, facilitating targeted interventions such as anti-inflammatory therapy or hydrocephalus management. This tool may improve resource allocation and reduce disability rates in critical care settings. Thus optimizing the intervention strategy and improve patient quality of life.
Data availability
The data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- SAH:
-
Subarachnoid hemorrhage
- aSAH:
-
Aneurysmal subarachnoid hemorrhage
- GCS:
-
Glasgow Coma Score
- WBC:
-
White blood cell count
- LY:
-
Lymphocyte count
- MO:
-
Monocyte count
- PLT:
-
Blood platelet count
- NB:
-
Neutrophil count
- TBil:
-
Total bilirubin
- DBil:
-
Direct bilirubin
- ALT:
-
Alanine transaminase
- AST:
-
Aspartate aminotransferase
- Cre:
-
Creatinine
- Urea:
-
Urea
- HDL-C:
-
High density lipoprotein
- LDL-C:
-
Low density lipoprotein
- TC:
-
Total cholesterol
- TP:
-
Total protein
- Alb:
-
Albumin
- PCT:
-
Procalcitonin
- TG:
-
Triglyceride
- FBG:
-
Fasting blood glucose
- HCT:
-
Hematocrit
- K:
-
Potassium
- Na:
-
Sodium
- Cl:
-
Chlorine
- Ca:
-
Total calcium
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thrombin time
- D-dimer:
-
D-dimer
- FIB:
-
Fibrinogen
- NLR:
-
Neutrophil count/lymphocyte count
- dNLR:
-
Neutral Granulocyte count/(White blood cell count - Lymphocyte count)
- MLR:
-
Monocyte count/lymphocyte count
- NMLR:
-
(Monocyte count + neutrophil count)/lymphocyte count
- SIRI:
-
Neutrophil count × monocyte count/lymphocyte count
- SII:
-
Platelet count × neutrophil count/lymphocyte count
- PLR:
-
Blood plate count/lymphocyte count
- AISI:
-
Neutrophil count × platelet count × monocyte count/lymphocyte count
- NHR:
-
Neutrophil count ratio/high-density fat egg White
- MHR:
-
Monocyte count/high density lipoprotein
- LHR:
-
Lymphocyte count/high density lipoprotein
- PHR:
-
Platelet count/high density lipoprotein
- TyG:
-
Triglyceride-glucose index
- TyG-BMI:
-
Glucose triglyceride /BMI index
References
Muehlschlegel, S. Subarachnoid Hemorrhage. Continuum (Minneap Minn). doi: 10.1212/CON.0000000000000679. PMID: 30516599. (2018)Dec;24(6):1623–1657.
Claassen, J. & Park, S. Spontaneous subarachnoid haemorrhage. Lancet. ;400(10355):846–862. doi: 10.1016/S0140-6736(22)00938-2. Epub 2022 Aug 16. PMID: 35985353; PMCID: PMC9987649. (2022).
Lindgren, A. et al. Endovascular coiling versus neurosurgical clipping for people with aneurysmal subarachnoid haemorrhage. Cochrane Database Syst. Rev. 8 (8), CD003085. (2018).
Lindgren, A. et al. Endovascular coiling versus neurosurgical clipping for people with aneurysmal subarachnoid haemorrhage. Cochrane Database Syst. Rev. 8 (8), CD003085. (2018)
Busl, K. M. & Rabinstein, A. A. Prevention and Correction of Dysnatremia After Aneurysmal Subarachnoid Hemorrhage. Neurocrit Care. ;39(1):70–80. (2023). https://doi.org/10.1007/s12028-023-01735-z. Epub 2023 May 3. PMID: 37138158.
Kuo, L. T. & Huang, A. P. The pathogenesis of hydrocephalus following aneurysmal subarachnoid hemorrhage. Int. J. Mol. Sci. 22 (9), 5050. https://doi.org/10.3390/ijms22095050 (2021). PMID: 34068783; PMCID: PMC8126203.
Connolly, E. S. Jr et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke. ;43(6):1711-37. (2012). https://doi.org/10.1161/STR.0b013e3182587839. Epub 2012 May 3. PMID: 22556195.
Serrone, J. C., Maekawa, H., Tjahjadi, M. & Hernesniemi, J. Aneurysmal subarachnoid hemorrhage: pathobiology, current treatment and future directions. Expert Rev. Neurother. 15 (4), 367–380 (2015). Epub 2015 Feb 26. PMID: 25719927.
Geraghty, J. R. et al. Systemic Immune-Inflammation index predicts delayed cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery 89 (6), 1071–1079. https://doi.org/10.1093/neuros/nyab354 (2021). PMID: 34560777; PMCID: PMC8600162.
Kasius, K. M., Frijns, C. J., Algra, A. & Rinkel, G. J. Association of platelet and leukocyte counts with delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage. Cerebrovasc. Dis. 29 (6), 576–583. https://doi.org/10.1159/000306645 (2010). Epub 2010 Apr 8. PMID: 20375501.
Mahta, A. et al. Association of early white blood cell trend with outcomes in aneurysmal subarachnoid hemorrhage. World Neurosurg. 151, e803–e809. https://doi.org/10.1016/j.wneu.2021.04.124 (2021). Epub 2021 May 5. PMID: 33964501.
Zhou, Y. et al. Dynamic changes of platelets before and after surgery predict the prognosis of patients with aneurysmal subarachnoid hemorrhage. Heliyon 10 (18), e37706. https://doi.org/10.1016/j.heliyon.2024.e37706 (2024). PMID: 39381250; PMCID: PMC11458939.
Yu, T. & Wang, Z. Use of A systemic inflammatory response index to predict Non-Traumatic Non-Aneurysmal subarachnoid hemorrhage patient outcomes. J. Stroke Cerebrovasc. Dis. 31 (12), 106863. https://doi.org/10.1016/j.jstrokecerebrovasdis.2022.106863 (2022). Epub 2022 Oct 29. PMID: 36323168.
Wang, X. et al. From past to future: bibliometric analysis of global research productivity on nomogram (2000–2021). Front. Public. Health. 10, 997713. https://doi.org/10.3389/fpubh.2022.997713 (2022). PMID: 36203677; PMCID: PMC9530946.
Zhuang, D. et al. A dynamic nomogram for predicting unfavorable prognosis after aneurysmal subarachnoid hemorrhage. Ann. Clin. Transl Neurol. 10 (7), 1058–1071 (2023). Epub 2023 May 17. PMID: 37198730; PMCID: PMC10351672.
Jin, X. et al. Development and external validation of a nomogram for predicting postoperative pneumonia in aneurysmal subarachnoid hemorrhage. Front. Neurol. 14, 1251570 (2023). PMID: 37745673; PMCID: PMC10513064.
Feng, X. et al. Development and validation of a novel nomogram to predict aneurysm rupture in patients with multiple intracranial aneurysms: a multicentre retrospective study. Stroke Vasc Neurol. 6 (3), 433–440. https://doi.org/10.1136/svn-2020-000480 (2021). Epub 2021 Feb 5. PMID: 33547231; PMCID: PMC8485246.
Salary, M., Quigley, M. R. & Wilberger, J. E. Jr Relation among aneurysm size, amount of subarachnoid blood, and clinical outcome. J Neurosurg. ;107(1):13 – 7. (2007). https://doi.org/10.3171/JNS-07/07/0013. PMID: 17639867.
Mittal, A. M. et al. The Hunt-Hess score at 48 h improves the outcome of grade 5 aneurysmal subarachnoid hemorrhage. World Department Neurosurg. March. 171, e874–e878. https://doi.org/10.1016/j.wneu.2023 (2023). 01.018. January 7, Epub 2023.PMID: 36627019.
Wang, H. R. et al. Combination of albumin/fibrinogen ratio and admission Hunt-Hess scale score as an independent predictor of clinical outcome in aneurysmal subarachnoid hemorrhage. World Neurosurg. 181, e322–e329. https://doi.org/10.1016/j.wneu.2023.10.047 (2024). Epub 2023 Oct 14. PMID: 37839575.
Middleton, P. M. Practical application of the Glasgow coma scale; a comprehensive narrative review of the GCS method. Australas Emerg. Nurs. J. August. 15 (3), 170–183. https://doi.org/10.1016/j.aenj.2012 (2012). August 3,06.002.Epub 2012.PMID: 22947690.
Bae, I. S., Chun, H. J., Choi, K. S. & Yi, H. J. Modified Glasgow coma scale for predicting outcome after subarachnoid hemorrhage surgery. Med. (Baltim). 100 (19), e25815. https://doi.org/10.1097/MD.0000000000025815 (2021). PMID: 34106620; PMCID: PMC8133269.
Yuwapattanawong, K. et al. The association between illness severity scores and In-hospital mortality after aneurysmal subarachnoid hemorrhage. J. Neurosurg. Anesthesiol. 35 (3), 299–306. https://doi.org/10.1097/ANA.0000000000000840 (2023). Epub 2022 Mar 17. PMID: 35297396.
Zheng, J., Xu, R., Liu, G., Guo, Z. & Sun, X. Effect of premorbid hypertension control on outcome of patients with aneurysmal subarachnoid hemorrhage. Acta Neurochir (Wien). ;160(12):2401–2407. (2018). https://doi.org/10.1007/s00701-018-3699-1. Epub 2018 Oct 12. PMID: 30315363.
Roethlisberger, M. et al. Swiss SOS group. Impact of very small aneurysm size and anterior communicating segment location on outcome after aneurysmal subarachnoid hemorrhage. Neurosurgery 92 (2), 370–381. https://doi.org/10.1227/neu.0000000000002212 (2023). Epub 2022 Nov 17. PMID: 36469672.
Wang, L. et al. Risk factors and predictive models of poor prognosis and delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage complicated with hydrocephalus. Front. Neurol. 13, 1014501. https://doi.org/10.3389/fneur.2022.1014501 (2022). PMID: 36353134; PMCID: PMC9638116.
Huang, H. Y. et al. A novel nomogram model for clinical outcomes of severe subarachnoid hemorrhage patients. Front. Neurosci. 16, 1041548. https://doi.org/10.3389/fnins.2022.1041548 (2022). PMID: 36507324; PMCID: PMC9729550.
Maldaner, N. et al. External validation of the HATCH (Hemorrhage, age, treatment, clinical state, Hydrocephalus) score for prediction of functional outcome after subarachnoid hemorrhage. Neurosurgery 91 (6), 906–912. https://doi.org/10.1227/neu.0000000000002128 (2022). Epub 2022 Sep 7. PMID: 36069543.
Kwon, M. S. et al. Methemoglobin is an endogenous toll-like receptor 4 ligand-relevance to subarachnoid hemorrhage. Int. J. Mol. Sci. 16 (3), 5028–5046. https://doi.org/10.3390/ijms16035028 (2015). PMID: 25751721; PMCID: PMC4394463.
Wu, F. et al. Inflammation and oxidative stress: Potential targets for improving prognosis after subarachnoid hemorrhage. Front. Cell. Neurosci. 15, 739506. https://doi.org/10.3389/fncel.2021.739506 (2021). PMID: 34630043; PMCID: PMC8497759.
Muhammad, S. & Hänggi, D. Inflammation and Anti-Inflammatory targets after aneurysmal subarachnoid hemorrhage. Int. J. Mol. Sci. 22 (14), 7355. https://doi.org/10.3390/ijms22147355 (2021). PMID: 34298971; PMCID: PMC8304004.
Lai, X., Zhang, W., Ye, M., Liu, X. & Luo, X. Development and validation of a predictive model for the prognosis in aneurysmal subarachnoid hemorrhage. J. Clin. Lab. Anal. 34 (12), e23542. https://doi.org/10.1002/jcla.23542 (2020). Epub 2020 Aug 29. PMID: 32860455; PMCID: PMC7755773.
Lucke-Wold, B. P. et al. Aneurysmal subarachnoid hemorrhage and neuroinflammation: A comprehensive review. Int. J. Mol. Sci. 17 (4), 497. https://doi.org/10.3390/ijms17040497 (2016). PMID: 27049383; PMCID: PMC4848953.
Sercombe, R., Dinh, Y. R. & Gomis, P. Cerebrovascular inflammation following subarachnoid hemorrhage. Jpn J Pharmacol. ;88(3):227 – 49. (2002). https://doi.org/10.1254/jjp.88.227. PMID: 11949877.
Sarrafzadeh, A., Schlenk, F., Gericke, C. & Vajkoczy, P. Relevance of cerebral interleukin-6 after aneurysmal subarachnoid hemorrhage. Neurocrit Care. ;13(3):339 – 46. (2010). https://doi.org/10.1007/s12028-010-9432-4. PMID: 20725805.
Feng, Y. et al. Postoperative neutrophil-lymphocyte ratio predicts unfavorable outcome of acute ischemic stroke patients who achieve complete reperfusion after thrombectomy. Front. Immunol. 13, 963111. https://doi.org/10.3389/fimmu.2022.963111 (2022). PMID: 36275640; PMCID: PMC9585914.
Wu, F., Wang, Q., Qiao, Y., Yu, Q. & Wang, F. A new marker of short-term mortality and poor outcome in patients with acute ischemic stroke: mean platelet volume-to-lymphocyte ratio. Med. (Baltim). 101 (40), e30911 (2022). PMID: 36221422; PMCID: PMC9542671.
Stuckey, S. M., Ong, L. K., Collins-Praino, L. E. & Turner, R. J. Neuroinflammation as a key driver of secondary neurodegeneration following stroke?? Int. J. Mol. Sci. 22 (23), 13101. https://doi.org/10.3390/ijms222313101 (2021). PMID: 34884906; PMCID: PMC8658328.
Al-Mufti, F. et al. White Blood Cell Count Improves Prediction of Delayed Cerebral Ischemia Following Aneurysmal Subarachnoid Hemorrhage. Neurosurgery. ;84(2):397–403. (2019). https://doi.org/10.1093/neuros/nyy045. PMID: 29528448.
Yao, P. S. et al. Higher leukocyte count predicts 3-month poor outcome of ruptured cerebral aneurysms. Sci Rep. ;8(1):5799. (2018). https://doi.org/10.1038/s41598-018-23934-x. Erratum in: Sci Rep. 2018;8(1):13060. doi: 10.1038/s41598-018-31339-z. PMID: 29643435; PMCID: PMC5895753.
Sawyer, D. M., Amenta, P. S., Medel, R. & Dumont, A. S. Inflammatory mediators in vascular disease: Identifying promising targets for intracranial aneurysm research. Mediators Inflamm. 2015, 896283. https://doi.org/10.1155/2015/896283 (2015). Epub 2015 Apr 1. PMID: 25922566; PMCID: PMC4397479.
Kataoka, K. et al. Structural fragility and inflammatory response of ruptured cerebral aneurysms. A comparative study between ruptured and unruptured cerebral aneurysms. Stroke. ;30(7):1396 – 401. (1999). https://doi.org/10.1161/01.str.30.7.1396. PMID: 10390313.
Lattanzi, S., Cagnetti, C., Provinciali, L. & Silvestrini, M. Neutrophil-to-Lymphocyte ratio predicts the outcome of acute intracerebral hemorrhage. Stroke 47 (6), 1654–1657. https://doi.org/10.1161/STROKEAHA.116.013627 (2016). Epub 2016 May 10. PMID: 27165957.
Velasco, A. et al. Neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and monocyte-to-lymphocyte ratio in depressed patients with suicidal behavior: A systematic review. Eur. Psychiatry 2023 Apr 16:1–25. https://doi.org/10.1192/j.eurpsy.2023.18. Epub ahead of print. PMID: 37062531.
Wang, H., Guo, Z. & Xu, Y. Association of monocyte-lymphocyte ratio and proliferative diabetic retinopathy in the U.S. Population with type 2 diabetes. J. Transl Med. 20 (1), 219. https://doi.org/10.1186/s12967-022-03425-4 (2022). PMID: 35562757; PMCID: PMC9102352.
Dong, C. H., Wang, Z. M. & Chen, S. Y. Neutrophil to lymphocyte ratio predict mortality and major adverse cardiac events in acute coronary syndrome: A systematic review and meta-analysis. Clin Biochem. ;52:131–136. doi: 10.1016/j.clinbiochem.2017.11.008. Epub 2017 Nov 11. PMID: 29132766. (2018).
Li, H., Zhou, Y., Ma, Y., Han, S. & Zhou, L. The prognostic value of the platelet-to-lymphocyte ratio in acute coronary syndrome: A systematic review and meta-analysis. Kardiol Pol. 75 (7), 666–673. https://doi.org/10.5603/KP.a2017.0068 (2017). Epub 2017 Apr 10. PMID: 28394006.
Wang, Q., Ma, J., Jiang, Z. & Ming, L. Prognostic value of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in acute pulmonary embolism: A systematic review and meta-analysis. Int. Angiol. 37 (1), 4–11. https://doi.org/10.23736/S0392-9590.17.03848-2 (2018). Epub 2017 May 24. PMID: 28541022.
Li, X., Liu, M. & Wang, G. The neutrophil-lymphocyte ratio is associated with all-cause and cardiovascular mortality in cardiovascular patients. Sci. Rep. 14 (1), 26692. https://doi.org/10.1038/s41598-024-76836-6 (2024). PMID: 39496711; PMCID: PMC11535400.
Dong, G. et al. The neutrophil-lymphocyte ratio as a risk factor for all-cause and cardiovascular mortality among individuals with diabetes: evidence from the NHANES 2003–2016. Cardiovasc. Diabetol. 22 (1), 267. https://doi.org/10.1186/s12933-023-01998-y (2023). PMID: 37775767; PMCID: PMC10541705.
Dong, G. et al. Neutrophil-lymphocyte ratio is a predictor for all-cause and cardiovascular mortality in individuals with prediabetes in a National study. Endocrine. Oct 23. (2024). https://doi.org/10.1007/s12020-024-04075-w. Epub ahead of print. PMID: 39438396.
Mitchell, A. J., Roediger, B. & Weninger, W. Monocyte homeostasis and the plasticity of inflammatory monocytes. Cell Immunol. (2014). Sep-Oct;291(1–2):22–31 https://doi.org/10.1016/j.cellimm.2014.05.010. Epub 2014 Jun 11. PMID: 24962351.
Ma, W. T., Gao, F., Gu, K. & Chen, D. K. The role of monocytes and macrophages in autoimmune diseases: A comprehensive review. Front. Immunol. 10, 1140. https://doi.org/10.3389/fimmu.2019.01140 (2019). PMID: 31178867; PMCID: PMC6543461.
Mohme, M. et al. Immune characterization in aneurysmal subarachnoid hemorrhage reveals distinct monocytic activation and chemokine patterns. Transl Stroke Res. 11 (6), 1348–1361. https://doi.org/10.1007/s12975-019-00764-1 (2020). Epub 2019 Dec 19. PMID: 31858408.
Walsh, K. B. et al. Monocyte count and 30-Day case fatality in intracerebral hemorrhage. Stroke 46 (8), 2302–2304. https://doi.org/10.1161/STROKEAHA.115.009880 (2015). Epub 2015 Jun 30. PMID: 26130090; PMCID: PMC4519364.
Adeoye, O. et al. Peripheral monocyte count is associated with case fatality after intracerebral hemorrhage. J. Stroke Cerebrovasc. Dis. 23 (2), e107–e111 (2014). Epub 2013 Oct 8. PMID: 24119622; PMCID: PMC3946748.
Pera, J. et al. Gene expression profiling of blood in ruptured intracranial aneurysms: in search of biomarkers. J. Cereb. Blood Flow. Metab. 33 (7), 1025–1031. https://doi.org/10.1038/jcbfm.2013.37 (2013). Epub 2013 Mar 20. PMID: 23512133; PMCID: PMC3705426.
van Lieshout, J. H. et al. An introduction to the pathophysiology of aneurysmal subarachnoid hemorrhage. Neurosurg. Rev. 41 (4), 917–930. https://doi.org/10.1007/s10143-017-0827-y (2018). Epub 2017 Feb 18. PMID: 28215029.
Witsch, J. et al. Prognostication of long-term outcomes after subarachnoid hemorrhage: the FRESH score. Ann. Neurol. 80 (1), 46–58. https://doi.org/10.1002/ana.24675 (2016). Epub 2016 May 25. PMID: 27129898.
Acknowledgements
Not applicable.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
HHL and GZ designed this study. YCW, XYL and MJL are responsible for writing articles, conducting statistical analysis, reviewing articles, and creating images.WCL are responsible for collecting data and conducting statistical analysis.All authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethical approval
Data access was restricted to authorized researchers, and the study complied with China’s Personal Information Protection Law (PIPL). The study has been approved by the Committee of Huizhou Central People’s Hospital, and due to the retrospective nature of the study, the Huizhou Central People’s Hospital Ethics Review Committee waived the need of obtaining informed consent. It complies with the Declaration of Helsinki and the Chinese Measures for Ethical Review of Biomedical Research Involving People.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wei, Y., Lin, X., Lin, M. et al. Constructing a nomogram for short-term prognosis in postoperative patients with aneurysmal subarachnoid hemorrhage: a two-center retrospective study. Sci Rep 15, 28153 (2025). https://doi.org/10.1038/s41598-025-11894-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-11894-y