Abstract
Background It is crucial to identify the high-risk factors associated with the recurrence and metastasis of endometrial cancer (EC) in order to implement more precise clinical stratification and management strategies for EC patients. Methods A total of 336 patients with stage I-III EC were retrospectively analyzed. According to the recurrence site, they were divided into locoregional recurrence (LR) and poor-prognosis recurrence (PPR). The factors that may affect the prognosis of EC were analyzed and the subgroups were analyzed. Results Among the no recurrence (NR), LR and PPR groups, 5-year OS were 89.4%, 60.2% and 46.8%, 5-year RFS were 100%, 15.4% and 6.4%. The FIGO stage, molecular classification, lymphovascular space invasion (LVSI) and smoking history were independent risk factors affecting 5-year OS and 5-year RFS in EC patients (p < 0.05). Pathological type and progesterone receptor (PR) were independent risk factors affecting 5-year OS (p < 0.05). Histologic Grade and adjuvant therapy were independent risk factors affecting 5-year RFS (p < 0.05). Myometrial invasion, LVSI and FIGO stage were independent risk factors in the LR subgroup (p < 0.05), FIGO stage, ER and PR were independent risk in the PPR subgroup (p < 0.05). Conclusions Patients with myometrial invasion ≥ 1/2 and substantial LVSI may be more likely to have LR, while patients with positive ER and PR are more likely to have PPR. We need to pay attention to these factors to help us judge the prognosis of EC patients.
Similar content being viewed by others
Introduction
Endometrial cancer (EC) comprises a spectrum of malignant neoplasms arising from the glandular epithelial and stromal cells of the endometrium. It represents the most prevalent gynecological malignancy in middle- and high-income countries1. In developed countries such as Europe and the United States, the incidence of EC has become the first malignant tumor of the female reproductive system, with 417,000 new diagnoses made globally in 20202。Surgery is the main treatment for EC3, especially for patients with early-stage EC, as it can prolong the survival period of patients. However, 10–20% of patients still experience postoperative recurrence or metastasis, EC patients after recurrence have a very poor prognosis, with a significantly reduced survival rate and a successful rate of re-salvage therapy as low as 40%4. Recurrence or metastasis is currently the main cause of treatment failure for EC. Currently, the FIGO staging system is widely used for treatment decision-making and prognosis evaluation of EC, but there are still cases with the same clinical stage but different prognoses, suggesting that there may be biological heterogeneity in EC patients5. Therefore, identifying high-risk factors for recurrence and metastasis of EC and conducting more precise clinical stratification management for EC patients is of vital importance.
Studies have shown that EC is a hormone-dependent tumor. According to the relationship of dependence on sex hormones, the content of hormone receptors is related to many clinical pathological features. Research has found that the abnormal expression of estrogen receptor (ER) and progesterone receptor (PR) is related to the occurrence and development of hormone-related cancers and can be used as a reference index for the prognosis assessment of hormone-related cancers6,7. Another study8 pointed out that the depth of myometrial invasion of the endometrium is one of the most important prognostic indicators and treatment decision factors for EC. The postoperative recurrence rate of EC patients with myometrial invasion depth ≥ 1/2 is significantly higher than that of patients with myometrial invasion depth < 1/2. However, it is still undetermined whether it is local regional recurrence or distant metastasis. In addition, lymphovascular space invasion (LVSI) is closely related to the prognosis of EC, but the research results are still controversial9,10. There is no definite conclusion about what outcomes are more likely to occur in patients with LVSI. This study retrospectively analyzed 336 patients with EC who underwent primary surgical treatment to explore the influence of clinical and pathological parameters on postoperative recurrence of EC, with the aim of providing a reference basis for standardized diagnosis and treatment of EC, early identification of high-risk patients for recurrence, and individualized treatment.
Results
General clinical features of patients and their correlation with recurrence
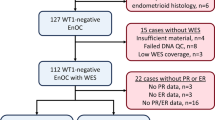
A total of 336 EC patients were enrolled in this study, with a median age of 54 years (range 27–75 years). A total of 123 patients had LR, 109 had PPR, and 104 had no recurrence (NR). There were182 patients with FIGO stage I, 55 patients with stage II, and 99 patients with stage III, detailed FIGO stage (2023) between different groups were shown in Supplementary Table 1. Significant differences were observed between the different groups in terms of age, pathological type, pathological differentiation, molecular classification, myometrial invasion, LVSI, ER status, PR status, smoking history, and adjuvant therapy (p < 0.05). Detailed general clinical characteristics were shown in Table 1.
Univariate and multivariate analysis of prognostic factors for EC
Univariate Cox regression analysis identified several clinicopathological factors significantly associated with 5-year survival outcomes. Age, FIGO stage, histologic type, histologic grade, molecular classification, myometrial invasion, LVSI, ER status, PR status, family history, and smoking history emerged as significant predictors for both OS and RFS (all p < 0.10). Notably, adjuvant therapy demonstrated additional prognostic value specifically for RFS (HR 1.908, 95% CI (1.400–2.600); p < 0.001). (Supplementary Table 2)
Subsequently, multivariate cox regression analysis was conducted for the above variables. Analysis showed that FIGO stage, molecular classification, LVSI and smoking history were independent risk factors affecting 5-year OS and 5-year RFS in EC patients (p < 0.05). Pathological type and PR were independent risk factors affecting 5-year OS (p < 0.05). Histologic Grade and adjuvant therapy were independent risk factors affecting 5-year RFS (p < 0.05) (Table 2).
Univariate and multivariate analyses of different recurrence subgroups for EC
According to the recurrence site, patients were divided into LR and PPR subgroups for univariate and multivariate analysis. Univariate cox regression analysis showed that variables associated with 5-year OS in the LR subgroup included age, FIGO stage, pathological type, pathological differentiation, myometrial invasion, LVSI, ER, PR, family history, smoking history and adjuvant therapy (p<0.05). Variables associated with 5-year OS in the PPR subgroup included FIGO stage, pathological type, pathological differentiation, myometrial invasion, LVSI, ER, PR, smoking history and adjuvant therapy (p<0.05) (Supplementary Table 3).
Multivariate cox regression analysis showed that FIGO stage, myometrial invasion, and LVSI were independent risk factors affecting 5-year OS in the LR subgroup (p<0.05). FIGO stage, ER and PR were independent risk factors for 5-year OS in the PPR subgroup (p<0.05) (Table 3).
Survival of different groups for EC
At a median follow-up of 73 months (IQR 50–93 months), a total of 69.0% (232/336) patients had recurrence and 48.8% (164/336) patients died during follow-up period. Among the myometrial invasion < 1/2 and myometrial invasion ≥ 1/2 groups, five-year OS were 73.3% and 53.2%, RFS were 37.9% and 39.7%, respectively. Among the LVSI no/focal (Ly0/Ly1) and LVSI substantial groups, five-year OS were 78.9% and 37.2%, RFS were 47.5% and 21.2%, respectively. Among the ER positive and negative groups, five-year OS were 84.6% and 49.2%, RFS were 49.0% and 30.5%, respectively. Among the PR positive and negative groups, five-year OS were 84.9% and 48.4%, RFS were 46.7% and 32.1%, respectively (Fig. 1).
Kaplan–Meier curves of the different factors. The 5-year overall survival rates of myometrial invasion (A), recurrence-free survival rates of myometrial invasion (B). The 5-year overall survival rates of LVSI (C), recurrence-free survival rates of LVSI (D). The 5-year overall survival rates of ER (E), recurrence-free survival rates of ER (F). The 5-year overall survival rates of PR (G), recurrence-free survival rates of PR (B). p values were calculated with the log-rank test.
There were 123 patients (36.6%) with LR and 109 (32.4%) patients with PPR. Among the NR, LR and PPR groups, five-year OS were 89.4%, 60.2% and 46.8%, five-year RFS were 100%, 15.4% and 6.4%. The K-M survival curves of those groups were show in Fig. 2.
The prognosis of different molecular subtypes of EC is significantly different. POLE mutation has the best prognosis, followed by MMRd/MSI-H and NSMP, and p53abn has the worst prognosis. The 5-year overall survival rate and 5-year recurrence-free survival rate according to molecular subtype are shown in Fig. 3.
Discussion
EC is one of the common gynecological malignant tumors, which brings great impact on the quality of life and life safety of patients. Surgery is the first choice for the treatment of EC, and recurrence or metastasis is the main cause of treatment failure. Therefore, it is necessary to screen and closely follow up patients with high risk of recurrence in order to provide timely and effective postoperative adjuvant treatment, so as to improve the survival rate and quality of life of patients.
In this study, we analyzed the survival outcome and its influencing factors of 336 patients with stage I-III EC after surgery, in order to find the factors of screening patients with high risk of recurrence and guide clinical postoperative follow-up and treatment. Analysis showed that FIGO stage, molecular classification, LVSI and smoking history were independent risk factors affecting 5-year OS and 5-year RFS in EC patients. Previous studies have pointed out that clinicopathological parameters such as FIGO stage, pathological type, and tissue differentiation degree are closely related to postoperative recurrence and metastasis of EC11. This is consistent with the results of our current study. Our study again demonstrated that FIGO stage, molecular classification, LVSI and smoking history are important factors in evaluating the prognosis and guiding the treatment of EC. In addition, our results also showed that, Pathological type and PR were independent risk factors affecting 5-year OS. Histologic Grade and adjuvant therapy were independent risk factors affecting 5-year RFS. 60-70% of ECs express ER and PR. ER and PR are related to histological grade, pathological stage and clinical prognosis, which can be an objective indicator to comprehensively reflect the nature of the disease12. Further subgroup analysis revealed that myometrial invasion and LVSI were independent risk factors affecting 5-year OS in the LR subgroup, ER and PR were independent risk factors for 5-year OS in the PPR subgroup, This implies that patients with myometrial invasion ≥ 1/2 and substantial LVSI may be more likely to have LR, while patients with negative ER and PR are more likely to have distant metastasis. It is suggested that we need to pay attention to these factors to help us judge the prognosis of EC patients.
The depth of myometrial invasion can be categorized into deep and superficial types. When the extent of myometrial invasion is less than one-half, the severity of cancer cell infiltration is relatively limited, and satisfactory outcomes can be achieved through surgical resection of the affected area. However, when the myometrial invasion exceeds one-half, the tumor will invade into the deep layer, and the tumor will easily penetrate the seromuscular layer and cause extrauterine spread, which will increase the postoperative recurrence rate and aggravate the risk of poor prognosis13. Patients with myometrial invasion ≥ 1/2 are more likely to have local recurrence. In this study, we found that the EC patients with myometrial invasion < 1/2 have better OS and RFS than those with myometrial invasion ≥ 1/2, suggesting that EC patients with myometrial invasion < 1/2 have better prognosis. The results of univariate and multivariate analysis showed that myometrial invasion was an independent risk factor for OS of EC, and was closely related to LR. Tabernero et al.14 showed that the survival rate of EC patients with myometrial invasion more than 2/3 was worse. Statistical analysis conducted by Ren et al.15 also suggested that the depth of myometrial invasion was significantly associated with the survival prognosis of EC patients. Cao16 proved that the depth of myometrial invasion is an independent factor for the postoperative prognosis of EC patients. These results are consistent with the results of our study, but they did not mention the correlation between the degree of myometrial invasion and local recurrence. Our study suggests that we should focus on local recurrence in patients with myometrial invasion of 1/2 or more.
LVSI, the presence of cancer cells in the lymphatic vessels or vascular space within the myometrium, is a necessary prerequisite for lymphatic dissemination. LVSI is usually included in the prediction model of lymph node metastasis, and the score of LVSI is the highest, which is an independent risk factor for regional lymph node metastasis in EC17. The more poorly differentiated and highly malignant EC is, the more likely LVSI is to occur. Therefore, patients with LVSI have a lower long-term survival rate, which can be used as an important reference index for predicting the prognosis of early EC18. AlHilli et al. showed that patients with substantial LVSI were more likely to have LR19. The results of this study support the above findings. In our study, the Ly0/Ly1 LVSI group have better OS and RFS than substantial LVSI group, suggesting that EC patients with Ly0/Ly1 LVSI have a better prognosis. Univariate and multivariate analysis showed that LVSI was an independent risk factor for OS and RFS of EC. In subgroup analysis, LVSI was an independent risk factor for 5-year OS of LR subgroup. Therefore, early identification of the high-risk group of LVSI in EC is helpful to guide the selection of surgical methods and surgical scope, so that the potential lymph node metastasis can be removed. At the same time, radiotherapy-based postoperative adjuvant therapy can help to reduce the risk of local recurrence and reduce the impact of LVSI on the prognosis of patients to a certain extent.
In addition to myometrial invasion and LVSI, ER and PR are also non-negligible factors. EC is associated with factors such as long-term stimulation of estrogen, persistent endometrial hyperplasia, infertility, and delayed menopause20. As nuclear receptors for estrogen and progesterone, ER and PR regulate gene expression through activation and repression of transcription, and their loss of expression is associated with the aggressiveness of malignant tumors21. Numerous studies have shown that loss of ER and PR expression is associated with reduced disease-free survival and overall survival in EC22,23. The results of our study showed that the patients with ER (+) and PR (+) have better OS and RFS than those with ER (-) and PR (-). Multivariate analysis showed that ER and PR were independent risk factors for 5-year OS of EC. This is consistent with the results of existing studies24,25. In addition, subgroup analysis found that ER and PR were independent risk factors for 5-year OS in the PPR subgroup, patients with negative ER and PR are more likely to have distant metastasis. In clinical work, we should pay close attention to the distant metastasis of patients with ER (-) and PR (-), and follow up actively and regularly.
Existing evidence suggests that ER/PR status may correlate with specific molecular subgroups. For instance, NSMP tumors, characterized by hormonal receptor positivity in 70–85% of cases, often exhibit responsiveness to endocrine therapy, whereas MMRd tumors may show reduced PR expression due to epigenetic silencing of progesterone-related pathways1. Importantly, even within molecular subtypes, ER/PR heterogeneity exists—a recent meta-analysis reported that 15–20% of p53abn (serous-like) tumors retain ER/PR expression26. In current EC management, The Cancer Genome Atlas (TCGA)-based molecular classification (POLEmut, MMRd, p53abn, NSMP) is considered the most powerful prognostic tool. The results of this study show that molecular subtype is an independent risk factor for 5-year OS and RFS in patients with EC. In addition, survival analysis found that POLE mutation had the best prognosis, followed by MMRd/MSI-H and NSMP, and p53abn had the worst prognosis. This underscores the necessity of integrating both molecular and hormonal biomarkers to refine therapeutic decisions. While our study provides robust data on ER/PR and molecular subtypes as standalone predictors, future work combining molecular profiling with hormone receptor analysis is warranted to address this multidimensional complexity.
To be honest, our study also has some limitations. This study is a single-center retrospective study, and although the effect of confounding factors was adjusted by multivariate analysis, selection bias may not be completely avoided. The recurrence rate was higher in this study than in other studies. In the future, a larger sample size and more aspects are needed to confirm the prognostic factors of EC. The classification of relapsed patients into LR and PPR in this study has not been standardized by international guidelines and does not cover relevant molecular characteristics. In future studies, optimizing stratification with molecular subtypes could be considered (e.g., POLE mutations may change the recurrence pattern). In addition, we note that wide confidence intervals were observed in select subgroup analyses (e.g., [specific group in Table 3]), likely reflecting limited event numbers in these strata. While this introduces statistical uncertainty, we elected to retain these subgroups based on their distinct clinical relevance. Future studies with larger cohorts are needed to refine these estimates. This study primarily focused on baseline clinicopathological biomarkers, and detailed treatment data (adjuvant therapy types, recurrence management) are being analyzed separately due to the complexity of longitudinal treatment documentation across our cohort. These data will be published in our subsequent research manuscript.
In summary, FIGO stage, myometrial invasion, and LVSI are closely related to locoregional recurrence of EC after surgery. FIGO stage, ER and PR are closely related to poor prognosis recurrence of EC. We should pay attention to the myometrial invasion, LVSI, ER and PR of patients with EC, and formulate accurate individualized treatment and follow-up plan, which will be conducive to the clinical stratification management of patients with EC, so that more patients can benefit from it.
Methods
Patients
A total of 336 patients with stage I-III EC who were diagnosed and underwent surgical treatment in the First Affiliated Hospital of University of South China from January 2013 to December 2018 were retrospectively analyzed. All patients met the following inclusion criteria: (1) according to International Federation of Gynecology and Obstetrics (FIGO) staging criteria, patients with FIGO stage I-III EC were enrolled; (2) there was no distant metastasis before and during treatment; (3) had not received any antitumor therapy before; (4) denied the history related to other malignancies; (5) surgical treatment was performed in our hospital, and the surgical methods were Extrafascial Hysterectomy/Modified Radical Hysterectomy/Radical Hysterectomy/Extended Radical Hysterectomy; (6) actively cooperate with postoperative follow-up; (7) complete clinical data, examination data and follow-up data were available. Our exclusion criteria included: (1) pathological examination showed uterine sarcoma. (2) tumor metastasis from other sites to the endometrium; (3) distant metastasis was found or could not be ruled out before and during treatment; (4) patients who had received chemotherapy or radiotherapy prior to surgery; (5) complicated with severe infection, underlying diseases; (6) previous or concurrent history of other malignant tumors; (7) unable to complete the treatment.
The clinical and pathological data of all EC patients were collected, including age, FIGO stage, pathological type, surgical data, postoperative adjuvant treatment plan, some immunohistochemical markers related examination results, smoking history, family history, etc. All the patients were restaged according to the FIGO stage, version 2023. In this study, the fifth edition of the WHO classification of Tumors of the female Reproductive System (2020) was used to classify endometrial cancer, which was divided into endometrioid adenocarcinoma and other types (including serous carcinoma, clear cell carcinoma, undifferentiated carcinoma, mixed cell adenocarcinoma, mesonephrotic adenocarcinoma, squamous cell carcinoma, etc. Due to the small number of cases, these types were combined as “other types”). Based on the mutation status of exonuclease domain of POLE gene, MMR/MSI and p53, the molecular classification were divided into four subgroups: POLEmut, MMRd/MSI-H, NSMP and p53abn. The Ethics Committee of the First Affiliated Hospital of the University of South China approved this study (Approval Number: 2024LL0102001). The study analyzed anonymized information, so the requirement of informed consent was waived by the Ethics Committee of the First Affiliated Hospital of the University of South China. The study was conducted in accordance with relevant guidelines and legislation.
Surgical methods
The scope of surgery was evaluated according to the results of preoperative diagnostic curettage and the condition. There were two surgical methods: laparoscopic and open surgery. According to the condition, different ranges of staged surgery were adopted.
Pathology examination
All EC patients in this study were examined by the same method of pathological sections and immunohistochemistry, and the materials used were from the same manufacturer. The histological morphology was observed by two experienced pathologists to confirm the diagnosis, histological type, and myometrial invasion (Fig. 4). If the two opinions were inconsistent, the superior pathologist was asked to review. Histologic grade was defined per FIGO criteria: G1 (≤ 5% non-squamous solid), G2 (6-50%), G3 (> 50%). LVSI was grouped according to the 2020 WHO Classification27: no LVSI, no vessels were involved in each HE section; Focal LVSI, involving less than 5 vessels; substantial LVSI, involving ≥ 5 vessels (Fig. 4).
Estrogen receptor (ER) and progesterone receptor (PR) detection
Formalin-fixed paraffin-embedded (FFPE) tissue sections were analyzed using a fully automated immunohistochemistry staining platform (Leica BOND-III). Antibody Information: ER: Monoclonal antibody, clone SP1 (Ventana, Cat# 790–4325), diluted at 1:100; PR: Monoclonal antibody, clone 1E2 (Roche, Cat# 790–4296), diluted at 1:150. Positivity Criteria: ≥1% tumor cell nuclear staining was defined as positive (referencing ASCO/CAP guidelines for breast cancer). Scoring System: The H-score (range 0–300) was calculated as: H-score = (% weakly stained × 1) + (% moderately stained × 2) + (% strongly stained × 3).
The threshold of ≥ 1% for ER/PR positivity aligns with established standards in endometrial cancer research and clinical practice. This threshold balances sensitivity and clinical relevance, avoiding the exclusion of patients who may benefit from hormonal therapy due to overly stringent criteria (e.g., ≥ 10%).
Determination of MMR status, p53 abnormalities and POLE mutations
MMR status: Assessed by immunohistochemistry (IHC) using antibodies against MLH1 (clone ES05, Leica Biosystems, 1:100), PMS2 (clone EP51, Agilent Dako, 1:50), MSH2 (clone FE11, Agilent Dako, 1:200), and MSH6 (clone EP49, Abcam, 1:100). Protein loss was defined as complete absence of nuclear staining in tumor cells with intact staining in internal controls (lymphocytes/stroma). Tumors with loss of ≥ 1 protein were classified as mismatch repair-deficient (dMMR); intact expression denoted proficient MMR (pMMR).
p53 status: Evaluated by IHC using anti-p53 antibody (clone DO-7, Agilent Dako, 1:500). Abnormal expression was defined as: (1) > 80% tumor cells with strong nuclear staining (overexpression), (2) 0% nuclear staining (null pattern), or (3) diffuse cytoplasmic staining. All other patterns were considered wild-type.
POLE mutation status: Detected by next-generation sequencing (NGS) targeting the exonuclease domain (exons 9–14) on the Illumina NextSeq 550 platform. DNA was extracted from FFPE tissue (QIAamp DNA FFPE Kit, Qiagen). Variants with allele frequency ≥ 5% and depth ≥ 100× were classified as pathogenic using ACMG/AMP guidelines, with hotspot mutations (e.g., p.Pro286Arg, p.Val411Leu) confirmed as POLE-mutated.
Endpoint and follow-up
The primary endpoint of the study was overall survival (OS, defined as calculated from the start of treatment to the date of death from any cause). The secondary endpoints were recurrence-free survival (RFS, defined as calculated from the start of treatment to the date of tumor recurrence). According to the follow-up results, the recurrence and metastasis were recorded. According to the recurrence site, they were divided into locoregional recurrence (LR, including vaginal, pelvic, pelvic lymph nodes, para-aortic lymph nodes) and poor-prognosis recurrence (PPR, including abdominal lymph nodes or other metastases such as liver, brain, and lung). Patients were followed up at least every 3 months for the first 2 years after completion of treatment and at least every 6 months for 2 to 5 years after completion of treatment, or until death. Efficacy evaluation was performed according to RECIST Version 1.1 of the Efficacy Evaluation Criteria for solid tumors. The follow-up period ended on December 31, 2023.
Statistical analysis
SPSS version 26.0 (IBM Corporation, Armonk, NY, USA) and GraphPad Prism 8.0.2 (GraphPad Software, San Diego, California USA) were used for all statistical analyses and statistical plots. The general characteristics of patients were compared with frequency and descriptive statistics. A chi-square test or Fisher’s exact test was used to compare the characteristics of patients in different groups. To plot survival curves and compare survival among groups, Kaplan-Meier and Log rank tests were used. P < 0.05 indicated an important statistical significance.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- EC:
-
Endometrial cancer
- ER:
-
Estrogen receptor
- PR:
-
Progesterone receptor
- LVSI:
-
Lymphovascular space invasion
- OS:
-
Overall survival
- RFS:
-
Recurrence-free survival
- LR:
-
Locoregional recurrence
- PPR:
-
Poor-prognosis recurrence
- NR:
-
No recurrence
- HR:
-
Hazard ratio
- CI:
-
Confidence interval
References
Makker, V. et al. Endometrial cancer. Nat. Rev. Dis. Primers 7(1), 88. https://doi.org/10.1038/s41572-021-00324-8 (2021).
Crosbie, E. J. et al. Endometrial cancer. Lancet 399 (10333), 1412–1428. https://doi.org/10.1016/S0140-6736(22)00323-3 (2022).
Harkenrider, M. M. et al. Radiation therapy for endometrial cancer: an American society for radiation oncology clinical practice guideline. Pract. Radiat. Oncol. 13 (1), 41–65. https://doi.org/10.1016/j.prro.2022.09.002 (2023).
Ureyen, I. et al. Factors predicting recurrence in patients with stage IA endometrioid endometrial cancer: what is the importance of LVSI? Arch. Gynecol. Obstet. 301 (3), 737–744. https://doi.org/10.1007/s00404-019-05418-z (2020).
Berek, J. S. et al. FIGO staging of endometrial cancer: 2023. J. Gynecol. Oncol. 34 (5), e85. https://doi.org/10.3802/jgo.2023.34.e85 (2023).
Ma, H. et al. Body mass index at age 18 years and recent body mass index in relation to risk of breast cancer overall and ER/PR/HER2-defined subtypes in white women and African-American women: a pooled analysis. Breast Cancer Res. 20(1), 5. https://doi.org/10.1186/s13058-017-0931-5 (2018).
Zhang, C. X. et al. Prognostic analysis of recurrence of stage I-III endometrial carcinoma based on clinicopathological parameters. J. Heze Med. Coll. 35(4):14–1838. https://doi.org/10.3969/j.issn.1008-4118.2023.04.004 (2023).
Dane, C. & Bakir, S. The effect of myometrial invasion on prognostic factors and survival analysis in endometrial carcinoma. Afr. Health Sci. 19 (4), 3235–3241. https://doi.org/10.4314/ahs.v19i4.47 (2019).
Bosse, T. et al. Substantial lymph-vascular space invasion (LVSI) is a significant risk factor for recurrence in endometrial cancer–A pooled analysis of PORTEC 1 and 2 trials. Eur. J. Cancer. 51 (13), 1742–1750. https://doi.org/10.1016/j.ejca.2015.05.015 (2015).
Feng, J. et al. Prognostic evaluation of lymph-vascular space invasion in patients with endometrioid and non-endometrioid endometrial cancer: A multicenter study. Eur. J. Surg. Oncol. 50 (4), 108261. https://doi.org/10.1016/j.ejso.2024.108261 (2024).
Lee, L. J. et al. Clinical outcomes and dosimetric predictors of toxicity for re-irradiation of vaginal recurrence of endometrial cancer. Brachytherapy 21 (3), 263–272. https://doi.org/10.1016/j.brachy.2021.12.010 (2022).
Ishikawa, A. et al. Expression of keratinocyte growth factor and its receptor in human endometrial cancer in Cooperation with steroid hormones. Int. J. Oncol. 32 (3), 565–574 (2008).
Wang, F. Analysis of influencing factors of recurrence of endometrial cancer and corresponding treatment strategy. Chin. J. Cancer, 32(05), 820–822. (2017).
Tabernero, J. M. et al. Endometrial cancer stages I and II. Analysis of survival and prognostic factors. Eur. J. Gynaecol. Oncol. 16 (1), 18–25 (1995).
Ren, Y. L. et al. [Combined treatment and prognostic factors for stage III and IV endometrial carcinoma]. Zhonghua Fu Chan Ke Za Zhi. 43 (7), 523–527 (2008). PMID: 19080517.
Cao X. Analysis of prognostic factors of endometrial cancer. Chin. Natl. Folk Med., 22(08), 22–23 (2013) (in Chinese).
Stålberg, K. et al. Lymphovascular space invasion as a predictive factor for lymph node metastases and survival in endometrioid endometrial cancer - a Swedish gynecologic Cancer group (SweGCG) study. Acta Oncol. 58 (11), 1628–1633. https://doi.org/10.1080/0284186X.2019.1643036 (2019).
Tortorella, L. et al. Substantial lymph-vascular space invasion (LVSI) as predictor of distant relapse and poor prognosis in low-risk early-stage endometrial cancer. J. Gynecol. Oncol. 32 (2), e11. https://doi.org/10.3802/jgo.2021.32.e11 (2021).
AlHilli, M. M. et al. Development and validation of a comprehensive clinical risk-scoring model for prediction of overall survival in patients with endometrioid endometrial carcinoma. Gynecol. Oncol. 163 (3), 511–516. https://doi.org/10.1016/j.ygyno.2021.09.008 (2021).
Cancer Genome Atlas Research Network et al. Integrated genomic characterization of endometrial carcinoma [published correction appears in nature. 2013;500(7461):242]. Nature 497 (7447), 67–73. https://doi.org/10.1038/nature12113 (2013).
Jeon, Y. T. et al. Steroid receptor expressions in endometrial cancer: clinical significance and epidemiological implication. Cancer Lett. 239 (2), 198–204. https://doi.org/10.1016/j.canlet.2005.08.001 (2006).
Zhang, Y. et al. Prognostic role of hormone receptors in endometrial cancer: a systematic review and meta-analysis. World J. Surg. Oncol. 13, 208. https://doi.org/10.1186/s12957-015-0619-1 (2015).
Guan, J. et al. The prognostic significance of Estrogen and progesterone receptors in grade I and II endometrioid endometrial adenocarcinoma: hormone receptors in risk stratification. J. Gynecol. Oncol. 30 (1), e13. https://doi.org/10.3802/jgo.2019.30.e13 (2019).
Tomica, D. et al. Impact of oestrogen and progesterone receptor expression in the cancer cells and myometrium on survival of patients with endometrial cancer. J. Obstet. Gynaecol. 38 (1), 96–102. https://doi.org/10.1080/01443615.2017.1328591 (2018).
Bendifallah, S. et al. Just how accurate are the major risk stratification systems for early-stage endometrial cancer? Br. J. Cancer. 112 (5), 793–801. https://doi.org/10.1038/bjc.2015.35 (2015).
Van Gool, I. C. et al. Blinded histopathological characterisation of POLE exonuclease domain-mutant endometrial cancers: sheep in wolf’s clothing. Histopathology 72 (2), 248–258. https://doi.org/10.1111/his.13338 (2018).
WHO Classification of Tumours. 5th, Edition. Female Genital Tumours (International Agency for Research on Cancer, Lyon, 2020).
Funding
This work was supported by grants from the Scientific Research Project of Hunan Provincial Health Commission (No. 202215014474).
Author information
Authors and Affiliations
Contributions
Y.L. conceived the original idea and wrote the proposal. Y.L. and D.Y. designed the study. Y.L., D.Y., X.L.Z., Y.N.T., P.L., and J.Y.H. organized the data collection and analyzed the data. Y.L. and D.Y. performed the statistical analysis and wrote the manuscript for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This study was conducted in accordance with the Helsinki Declaration and approved by the Ethics Committee of the First Affiliated Hospital of the University of South China. Participant information is confidential. The need for informed consent was waived by the Ethics Committee of the First Affiliated Hospital of the University of South China.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, D., Zhang, X., Tan, Y. et al. Analysis of postoperative prognosis of non-metastatic endometrial carcinoma under different recurrence patterns. Sci Rep 15, 26506 (2025). https://doi.org/10.1038/s41598-025-12399-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-12399-4