Abstract
Managing actively bleeding gastric varices (GV) is clinically challenging. This study assessed the safety and efficacy of endoscopic band ligation (EBL) using large-volume ligators compared with endoscopic variceal obturation (EVO) in managing actively bleeding GV. Patients who were diagnosed with active GV bleeding via endoscopy and underwent EBL with large-volume band ligators or EVO were enrolled. Follow-up endoscopy was performed at 1, 3, and 6 months after endoscopic treatment. Primary outcomes were the initial haemostasis success rate, GV eradication rate within 3 months, 1-week rebleeding rate, 6-month cumulative rebleeding rate, and recurrence rate within 6 months. Secondary outcomes were the rate and average volume of blood transfusions in patients with rebleeding and adverse events related to endoscopic treatment. Overall, 154 patients were included (EBL group: n = 77; EVO group: n = 77). There were no statistically significant differences between the two groups regarding the initial haemostasis success rate, 1-week rebleeding rate, 3-month GV eradication rate and average number of sessions to GV eradication, cumulative rebleeding rate, and recurrence rate within 6 months. Three of the nine patients with rebleeding in the EVO group required blood transfusion with an average blood transfusion volume that was significantly lower than that required by the five patients with rebleeding in the EBL group (P = 0.024). The fever rate was lower in the EBL group than in the EVO group (P = 0.011). In the EVO group, one patient developed a pulmonary embolism and died during treatment, and three patients developed postoperative sepsis. The short-term efficacy of EBL with large-volume ligators in the treatment of actively bleeding GV is similar to that of EVO; however, postoperative rebleeding is often more dangerous in EBL than in EVO. Therefore, EBL represents a viable alternative in emergency endoscopic control of GV bleeding, provided that a contingency plan for early band slippage-related rebleeding is implemented.
Trial registration: Chinese Clinical Trial Registry (No. ChiCTR1900027588, 19/11/2019).
Similar content being viewed by others
Introduction
Gastric varices (GV) reportedly occur in 20% of patients with portal hypertension1, with 4–65% of patients with GV experiencing bleeding within 2 years of diagnosis2. GV has a mortality rate of 20% within 6 weeks of the first bleeding episode3. Therefore, timely and effective control of actively bleeding GV is necessary for patient survival. Compared with oesophageal varices, GV are often accompanied by gastrorenal shunts4, which often limit the choice of endoscopic cyanoacrylate injection for bleeding GV treatment. In addition, fewer established treatment guidelines are available for GV than for oesophageal varices5, especially regarding the control of active bleeding. Compared with other endoscopic methods, endoscopic variceal obturation (EVO) using cyanoacrylate for GV treatment yields favourable outcomes, with a higher haemostatic success rate and lower early and late rebleeding rates6. However, the use of cyanoacrylate is associated with the risk of serious complications, e.g. systemic embolism, which can lead to patient death7,8,9. Some studies have reported the incidences of pulmonary, cerebral, and mesenteric vein embolisms to be 5.2%, 3.1%10, and 2.1%11, respectively. Additionally, the incidence of sepsis due to cyanoacrylate injections was 5.38%12. Although endoscopic ultrasound-guided GV treatment using coils and cyanoacrylate injection aids in the prevention of systemic embolisms13,14, it is technically challenging to perform, requires complex equipment, and cannot completely prevent ectopic organ embolisms15. Endoscopic band ligation (EBL) can prevent these adverse events; nonetheless, its application in bleeding GV treatment remains controversial. Although some studies have reported that using EBL in bleeding GV treatment offers an advantage in achieving emergency haemostasis16, other studies have reported a poor efficacy of EBL in bleeding GV treatment17. However, the studies on the use of EBL for bleeding GV are outdated and, therefore, not relevant to the current endoscopic instruments and techniques. Most of the ligators used in previous studies were 6 Shooter Multi-Band Ligators18,19, which could only accommodate a small amount of variceal tissue. Furthermore, their indications and efficacy in bleeding GV treatment are limited, whereas the 10 Shooter Multi-Band Ligator20 has a longer transparent cap that can accommodate a large amount of variceal tissue. Moreover, a previous study showed that the use of large-volume ligators to eradicate GV had similar effects as cyanoacrylate injection20. Therefore, with the development of medical equipment and drugs, an up-to-date re-evaluation of the efficacy of EBL in bleeding GV treatment is warranted.
Accordingly, through a multicentre prospective randomised trial, we aimed to evaluate the efficacy and safety of EBL with large-volume ligators (10 Shooter Multi-Band Ligator) compared with EVO for the management of actively bleeding GV.
Patients and methods
Study design and patient selection
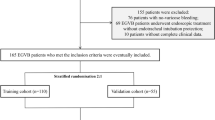
This prospective study was registered with the Chinese Clinical Trial Registry (No. ChiCTR1900027588, 19/11/2019). Patients with actively bleeding GV who presented at the Department of Gastroenterology, Ningbo No. 2 Hospital and the First People’s Hospital of Yongkang between January 2020 and June 2023 for the assessment and treatment of portal hypertension were enrolled in this study. The diagnosis of actively bleeding GV was confirmed using endoscopy in all patients. The study was conducted in accordance with the tenets of the Declaration of Helsinki, and the research protocol was approved by the Ethics Committee of each hospital (Ethical Approval Number: SL-NBEY-KY-2021-192-01). Written informed consent was obtained from all patients.
Inclusion criteria
All the patients in this study were enrolled after emergency endoscopic assessment. Patient inclusion was based on the following criteria: (1) active upper gastrointestinal bleeding and haematemesis, with or without a dark red bloody stool, with a history of liver cirrhosis or liver cancer and portal hypertension; (2) gastroesophageal varices, according to Sarin’s classification21, gastroesophageal varices type 1 (GOV1) or 2 (GOV2), isolated GV type 1 (IGV1), and cardiac and gastric variceal jet bleeding or gush-like bleeding confirmed using inverted gastroscopy; (3) absence of cardiac varices or GV jet bleeding on examination using an inverted gastroscope, but presence of cardiac varices or GV and accumulation of a large volume of bright red blood (judged to be > 100 ml using gastroscope suction) in the gastric fundus cavity and unstable vital signs (systolic blood pressure ≤ 90 mmHg and/or heart rate > 120 bpm); and (4) GV transverse diameter of < 2 cm.
Exclusion criteria
Patients with a history of endoscopic treatment (endoscopic injection or ligation) for GV, active oesophageal bleeding, isolated GV type 2 (IGV2) variceal bleeding, or bleeding due to other causes were excluded.
Procedure
All procedures were performed by endoscopists with prior experience in prophylactic treatment of over 200 cases of oesophageal varices and GV. A pre-study meeting was conducted to clarify the protocol to all endoscopists in this study.
After emergency endoscopic assessment, eligible patients were randomised into two treatment groups. The random allocation sequences were secured in consecutively numbered, opaque, sealed envelopes to maintain confidentiality. Operators were informed that patient group assignments were already finalised and they were excluded from this randomisation process. Follow-up physicians remained blinded. The EBL group underwent EBL with a large-volume ligator, whereas the EVO group underwent EVO. Participants in both groups underwent preoperative packed red blood cell transfusion (when their haemoglobin level was < 7 g/dl). Rehydration was first performed to stabilise the patient’s vital signs, followed by intubation to protect the airway. All patients underwent emergency portal vein computed tomography three-dimensional angiography (CTA) before endoscopic treatment to determine the presence or absence of a gastrorenal shunt. Participants were administered propofol (2 mg/kg) intravenously to induce anaesthesia before undergoing EBL or EVO. An endoscope (9.9 mm; GIF-Q260J; Olympus Optical Co., Ltd., Tokyo, Japan) was used to confirm the diagnosis of actively bleeding GV. A biopsy forceps (PTY1-2316U; Zhuji Pengtian Medical Devices Co., Ltd., China) with an opening width of 0.5 cm was used to measure GV with a transverse diameter ≤ 1 cm. A haemostatic clip (ROCC-D-26-195; Micro-Tech Co., Ltd., Nanjing, China) with an opening width of 1 cm was used to measure GV with a transverse diameter > 1 cm.
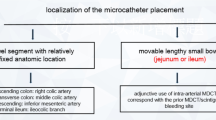
In the EBL group, the endoscope was fitted with a Saeed 10 Shooter Multi-Band Ligator (Wilson Cook, Winston-Salem, NC) and was introduced into the gastric fundus. The endoscope was then retroflexed (inverted) to observe bleeding varices (Figs. 1A, 2A, and 3A). GV at the bleeding site (Figs. 1B and 3B) was ligated first, followed by the ligation of the adjacent GV. If the bleeding site could not be determined due to the presence of a haematocele in the gastric fundus cavity (Fig. 2B) and the haematocele in the stomach did not hinder the endoscopic treatment, ligation was performed in the following order. For gastroesophageal varices, GV closest to the cardia were ligated first, followed by those from the cardia to the gastric body. Adjacent varices were then ligated using the same method20. For IGV1, ligation was performed starting at the corpus end of the varices20 (avoiding the ligation of the bulging varices first). The adjacent residual varices were then ligated clockwise. For all ligations, the distance between two ligation points was approximately 1 cm, including as much of the normal gastric mucosa adjacent to the varices.
Ligation of GOV1 variceal bleeding. (A) Jet bleeding of GOV1 varices is identified using an inverted gastrointestinal endoscope. (B) Endoscopic view of the GV within the ligator cap. (C) After EBL, endoscopic examination shows successful haemostasis. (D) One month after EBL, an inverted endoscopy reveals a post-ligation ulcer. GOV1, Gastroesophageal varices type 1; GV, Gastric varices; EBL, Endoscopic band ligation.
Ligation of GOV2 variceal bleeding. (A) GOV2 varices and blood accumulation in the gastric cavity are identified using an inverted gastrointestinal endoscope. (B) Endoscopic view of the GV within the ligator cap. (C) After EBL, endoscopic examination shows successful haemostasis. (D) Six months after EBL, an inverted endoscopy examination reveals white scars at the site of EBL. GOV2, Gastroesophageal varices type 2; GV, Gastric varices; EBL, Endoscopic band ligation.
Ligation of IGV1 variceal bleeding. (A) Jet bleeding in IGV1 varices and blood accumulation in the gastric cavity are observed using an inverted gastrointestinal endoscope. (B) Endoscopic view of GV within the ligator cap. (C) After EBL, endoscopic examination shows successful haemostasis. (D) Three months after EBL, an inverted endoscopy examination reveals scars at the site of EBL. IGV1, Isolated gastric varices type 1; GV, Gastric varices; EBL, Endoscopic band ligation.
In the EVO group, GV at the identifiable bleeding site (Fig. 4A and D) were injected via the sandwich technique using an injection needle (Olympus NM-200L-423; Olympus) with histoacryl (N-butyl-2-cyanoacrylate; Beijing Compont Medical Devices Co., Ltd., China) and lauromacrogol (Shaanxi Tianyu Pharmaceutical Co. Ltd., Shaanxi, China) (Fig. 4B and E). First, lauromacrogol (2–3 ml) was injected into the GV, followed by histoacryl (0.5–1 ml), and then finished with a flush of lauromacrogol (2–3 ml)20. If the bleeding site could not be determined, the injection was concentrated in the area with blood sacs or the most obvious varices. In patients with tortuous GV bleeding (Fig. 5A) and gastrorenal shunt on CTA (Fig. 5B), a haemostatic clip was used to clamp at the inflow or outflow of the varicose vein (Fig. 5C). Then, another haemostatic clip was used to clamp at the middle stenosis (Fig. 5D) so that the entire varicose vein was clamped as much as possible to slow down or completely block blood flow within the GV22. Subsequently, injection was performed using the ‘sandwich method’, first between the two clips (Fig. 5E), and then on the outer side of the clips. In patients with nodular or tumorous GV bleeding and gastrorenal shunt on CTA, haemostatic clips were deployed at both ends of the nodule or tumour, and then the ‘sandwich method’ injection was performed between the two clips.
EVO of GOV variceal bleeding. (A) Jet bleeding of GOV1 varices is identified using an inverted gastrointestinal endoscope. (B) Cyanoacrylate is injected into the bleeding site. (C) After EVO, endoscopic examination shows successful haemostasis. (D) Jet bleeding of GOV2 varices is identified using an inverted gastrointestinal endoscope. (E) The injection needle is close to the bleeding site of GV. (F) After EVO, endoscopic examination shows successful haemostasis. EVO, Endoscopic variceal obturation; GOV, Gastroesophageal varices; GOV1, Gastroesophageal varices type 1; GOV2, Gastroesophageal varices type 2; GV, Gastric varices.
EVO of tortuous GV bleeding with a gastrorenal shunt. (A) Tortuous variceal bleeding is identified using an inverted gastrointestinal endoscope. (B) CTA image of combined gastrorenal shunt. (C) A haemostatic clip is clamped at one end of the GV. (D) On the basis of (C), another haemostatic clip is clamped at the middle stenosis of the GV. (E) Cyanoacrylate is injected into the GV between the two clips. (F) Three months after EVO, inverted endoscopy examination reveals GV occlusion and one haemostatic clip remained. EVO, Endoscopic variceal obturation; GV, Gastric varices; CTA, Computed tomography three-dimensional angiography.
Excessive haemorrhage in the gastric cavity that might limit endoscopic observation and treatment was first removed via endoscopic suction using a basket for clot removal, as necessary. If haemostasis was successfully achieved by EBL (Figs. 1C, 2C, and 3C) or EVO (Fig. 4C and F), endoscopic observation was performed for an extra 5-min period before ending the procedure to confirm the absence of active bleeding. A transjugular intrahepatic portosystemic shunt (TIPS) was used if endoscopic haemostasis was not achieved. If the first EBL or EVO was successful in achieving haemostasis, but bleeding recurred within a week, repeat endoscopic treatment or TIPS was performed to achieve haemostasis. After a successful endoscopic haemostasis procedure, all patients fasted for 72 h and were treated with somatostatin to reduce portal pressure. Proton pump inhibitors and gastric mucosal protectors were routinely administered to patients to accelerate the healing of ulcers induced by endoscopic treatment. Moreover, non-selective β-blockers were used to prevent recurrent bleeding after endoscopic treatment.
Related definitions
The severity of GV was defined according to Hashizume et al.23, as follows: mild (F1), linear or slightly tortuous varices; moderate (F2), nodular-shaped varices; and severe (F3), tumorous huge varices. Active bleeding was defined as repeat haematemesis within several hours of endoscopic treatment, jet bleeding of cardiac or gastric fundus varices observed via endoscopy, new accumulation of fresh blood (judged to be > 100 ml by gastroscopic suction), or blood clots in the stomach cavity, with unstable vital signs despite the absence of jet bleeding on endoscopy. The initial haemostasis was defined as the cessation of bleeding after emergency endoscopic treatment without rebleeding within 1 week. Rebleeding was defined as the recurrence of clinically significant active bleeding events after bleeding control (haematemesis, melena, or blood in the stool; a decrease in systolic blood pressure by > 20 mmHg or increase in heart rate by > 20 beats/min; and a decrease in haemoglobin level by > 30 g/l in the absence of blood transfusion)24 confirmed by endoscopic examination as bleeding at the site of ligation or cyanoacrylate injection. Eradication was defined as the complete disappearance of GV after several endoscopic treatments (EBL group, Figs. 1D, 2D, and 3D) or complete occlusion or absence of GV, meaning that all injected varices were hard when touched by the catheter and white (EVO group, Fig. 5F). The GV eradication rate was defined as the proportion of cases achieving gastric variceal eradication confirmed by endoscopic follow-up after several endoscopic treatments to the total number of enrolled cases in that group. Recurrence was defined as an endoscopic follow-up revealing new GV after complete eradication. The recurrence rate was defined as the proportion of cases developing new gastric varices confirmed by endoscopic follow-up within 6 months after eradication to the total number of cases achieving eradication.
Outcomes and follow-up
The primary outcomes included the initial haemostasis success rate, 3-month GV eradication rate, 1-week rebleeding rate, 6-month cumulative rebleeding rate, and 6-month GV recurrence rate. Secondary outcomes were the blood transfusion rate and average blood transfusion volume in patients with rebleeding and endoscopic treatment-related adverse events, including fever, sepsis, distant embolisation, and death.
Endoscopic follow-up examinations were performed at 1, 3, and 6 months after the first endoscopic treatment. If bleeding recurred during this period or residual GV remained during the endoscopic follow-up, the same treatment was repeated. Follow-up was conducted for 6 months and terminated if initial haemostasis was unsuccessful or death occurred.
Statistical analysis
Based on previous studies, we predicted the 6-month cumulative rebleeding rate after controlling bleeding GV with EBL to be approximately 54.0%, whereas that with EVO was predicted to be 22.4%17,25. The minimum sample size required for this study was 50 patients per group. Descriptive statistical analyses were performed using SPSS for Windows (version 23.0; IBM Corp., Armonk, NY). Continuous variables are expressed as mean ± standard deviation (x ± s), and the two groups were compared using the independent sample t-test (for data following a normal distribution) or Mann–Whitney U test (for data following a non-normal distribution). Categorical data were expressed as n or %, as appropriate. Chi-square test or Fisher’s exact test was used for the comparison between the two groups of baseline data, while logistic regression was used for the comparison between the two groups of endoscopic treatment outcomes and related complications to control for the potential influence of confounding factors. Patients with recurrent bleeding were only included in the calculation of the eradication rate if the rebleeding event ceased following a repeat endoscopic treatment and GV was finally eradicated. A P value < 0.05 was considered statistically significant.
Results
Basic data
Over the study period, 316 patients presented with active upper gastrointestinal bleeding. According to the exclusion criteria, 108 patients with esophageal variceal bleeding, 49 with peptic ulcer bleeding, and five with Dieulafoy bleeding without gastric variceal bleeding were excluded. Overall, 154 patients with GV bleeding who met the inclusion criteria were enrolled in this study. The EBL and EVO groups included 77 patients each. There were 117 males and 37 females, with an average age of 56.41 ± 10.90 years. In the EBL group, 37 patients experienced GOV1, 24 experienced GOV2, and 16 experienced IGV1 lesions. In the EVO group, 46 patients experienced GOV1, 23 experienced GOV2, and eight experienced IGV1. Cirrhosis due to viral hepatitis was the most common underlying liver disease, followed by alcohol-related cirrhosis. GV were most commonly located in the cardia. On inverted endoscopy, jet bleeding was confirmed in nine and eight patients in the EBL and EVO groups, respectively, and intermittent jet or gush-like bleeding was confirmed in 38 and 31 patients, respectively. Jet- or gush-like bleeding was not observed in 30 and 38 patients in the EBL and EVO groups, respectively; however, a large volume of fresh blood (> 100 ml) or blood clots accumulated in these patients’ gastric cavity, and they had unstable vital signs. There were no significant differences in the demographic and clinical characteristics between the two groups (Table 1). The absence of active bleeding from oesophageal varices or varices outside the cardio-fundal region was confirmed in all patients.
Outcomes and complications
Endoscopic treatment outcomes and associated complications are presented in Table 2. The initial haemostasis success rates of EBL and EVO in the treatment of actively bleeding GV were 98.70% (76/77) and 97.40% (75/77), respectively, and the difference was not statistically significant (univariate: χ2 = 0.340, P = 1.000; multivariate: P = 1.000). TIPS was required in one patient each in the EBL and EVO groups because of the accumulation of large volumes of blood in the gastric lumen, which prevented the exposure of the target varices during endoscopy. At the 3-month follow-up, the GV eradication rates in the two groups were 96.05% (73/76) and 93.33% (70/75), respectively, with no statistically significant difference (univariate: χ2 = 0.556, P = 1.000; multivariate: P = 1.000). The average numbers of sessions to GV eradication of the two groups were 1.57 ± 0.72 and 1.49 ± 0.60, respectively, with no statistically significant difference (t = − 0.367, P = 0.714). The mean number of bands per patient used to eradicate GV by EBL was 4.97 ± 2.19 loops. Rebleeding occurred in two patients (2.63%) after EBL and in three patients (4.00%) after EVO within 1 week and was stopped successfully using the initial treatment method. There was no significant difference in the rebleeding rate within 1 week between the two groups (univariate: χ2 = 0.221, P = 0.681; multivariate: P = 0.489). After 6 months of follow-up, there were five patients (6.58%) with rebleeding in the EBL group and nine (12.00%) in the EVO group, and the difference was not statistically significant (univariate: χ2 = 1.319, P = 0.251; multivariate: P = 0.176). The five patients with rebleeding (100.00%) in the EBL group required massive blood transfusion, with an average blood transfusion volume of 6.80 ± 1.30 units, whereas only three patients (33.33%) in the EVO group required blood transfusion, with an average blood transfusion volume of 2.33 ± 0.58 units. Univariate analysis showed a significant difference in the blood transfusion rate between the two groups of patients with rebleeding (univariate: χ2 = 5.833, P = 0.031), but multivariate analysis indicated no statistical significance (P = 0.790). However, there was a significant difference in the average blood transfusion volume between the two groups, that is, the average blood transfusion volume in the EBL group was significantly higher than that in the EVO group (t = − 0.263, P = 0.024). The recurrence rate in the EVO group (5.71%) was lower than that in the EBL group (9.59%); however, this difference was not statistically significant (univariate: χ2 = 0.756, P = 0.385; multivariate: P = 0.143). Nine patients (11.84%) in the EBL group developed a fever after treatment without other site infection; this proportion was significantly lower than that in the EVO group (20 patients, 26.67%), and the difference was statistically significant (univariate: χ2 = 5.346, P = 0.021; multivariate: P = 0.011). In the EVO group, three patients (4.00%) developed sepsis, and the infection symptoms improved after intravenous infusion of antibiotics. One patient (1.32%) developed pulmonary embolism after the injection of cyanoacrylate and died because of an ineffective rescue method. No treatment-related deaths or serious adverse events occurred after EBL.
Discussion
Currently, there is no generally accepted effective treatment for actively bleeding GV; therefore, this study investigated the efficacy and safety of EBL using large-volume ligators compared with EVO for the management of actively bleeding GV. Our results showed that the initial haemostasis success rates of EBL and EVO were 98.70% and 97.40%, respectively, indicating that both methods can effectively control active GV bleeding. These results are similar to the previously reported rates for cyanoacrylate injection (96.70–100.00%)26,27,28,29 and significantly higher than the rates previously reported for EBL (45.0–88.88%)17,26,30,31. In this study, the average treatment sessions for GV eradication within 3 months in the EBL group was 1.57, which was not statistically different from that (1.49) in the EVO group; however, it was lower than that previously reported (1.80–3.43)25,30,32,33. In addition, not only was the eradication rate higher than that previously reported (66.66–90.00%)25,30,33, but the average number of bands used to ligate GV per patient was less than that reported in previous studies (8.88)33. A possible explanation is that this study used a large-volume ligator (10 Shooter Multi-Band Ligator), which has a longer ligation cylinder and larger volume, allowing easy access to the target varices and accommodating more varices and tissues when turning the gastroscope, resulting in thorough GV ligation. However, previous studies used a small-volume ligator (6 Shooter Multi-Band Ligator)18,25. In terms of GV eradication, large-volume ligators compensate for the insufficiency of small-volume ligators in the full ligation of gastric variceal tissue and achieve therapeutic effects similar to those of EVO. This study’s results indicated that the use of large-volume ligators provides significant advantages in GV eradication.
In this study, the 1-week rebleeding and 6-month cumulative rebleeding rates after the initial success of haemostasis by EBL were much lower than previously reported rates (11.3–54.0%)10,17,29,34,35,36 and slightly lower than those in the EVO group. However, patients with rebleeding in the EBL group often had a large amount of bleeding and high bleeding speed. In this study, all five patients with rebleeding in the EBL group required massive blood transfusions. Although the rebleeding rate in the EVO group was slightly higher, only three of the nine patients with rebleeding needed blood transfusion, with an average blood transfusion volume significantly lower than that in the EBL group (2.33 vs 6.80 units). A possible reason for this is that the band falls off prematurely, leading to a large mucosal defect after ligation33. As ligation cannot block blood flow in the blood supply vessel, rebleeding caused by premature detachment of the band is often dangerous, and the peristalsis of the stomach and its acidic environment may be the main reasons for the premature slippage of the band17,37. Therefore, preventing premature band slippage remains a critical challenge in the EBL treatment of gastric varices. In contrast, in the EVO group, even if rebleeding occurred, the bleeding was relatively slower due to partial occlusion of the defect by retained adhesive material. The recurrence rate in the EBL group was 9.59%, which was higher than that in the EVO group (5.71%) although without statistical difference, and significantly lower than that in previous reports33. The discrepancies between our results and those of previous studies can be explained as follows. First, large-volume ligators can accommodate more varicose veins and tissues, making the ligation depth closer to the submucosa layer20, thus reducing the possibility of variceal recurrence. Second, the 1 cm distance between ligation points likely provided more intensive ligation than the previously used wider distances17. All visible GV could be ligated nearly completely using a 1-cm distance, thus reducing the risk of rebleeding if any band slipped.
Regarding severe complications, there were three cases of sepsis and one case of pulmonary embolism in the EVO group, as well as 9 and 20 cases of postoperative fever after EBL and EVO, respectively. The patient who developed pulmonary embolism died of systemic cyanoacrylate embolism. These results indicate that EBL has a significant advantage over EVO in preventing these complications. Distant organ embolism is an inherent disadvantage of cyanoacrylate injection that cannot be completely avoided. The presence of a portosystemic vascular shunt is the main risk factor for embolism38. Cases of death caused by pulmonary embolism due to tissue glue have been frequently reported38,39,40. One death caused by tissue glue injection in this study was closely related to its apparent gastrorenal shunt. Therefore, it is essential to perform emergency computed tomographic angiography for patients with GV bleeding when clinically stable, and then evaluate whether alternative approaches should be employed for those with gastrorenal shunts. Once systemic embolism is detected, all hemostatic agents should be discontinued and low-molecular-weight heparin administered in all patients1. In this study, the incidence of sepsis in the EVO group was 4%, which is slightly higher than that reported in previous studies41. In addition to gastrointestinal bacterial contamination of the injection needle and its direct entry into blood vessels, sepsis may also be associated with blood transfusion before emergency haemostasis41. Therefore, it is recommended that patients receiving emergency cyanoacrylate injection be administered prophylactic antibiotics.
Overall, the results of this study demonstrated that EBL with large-volume ligators for the treatment of GV bleeding had a high success rate of initial haemostasis and GV eradication, prevented the occurrence of sepsis and distant embolism, and reduced fever and rebleeding rates. Therefore, EBL can serve as an alternative approach for emergency endoscopic management of GV bleeding. However, rebleeding resulting from early band slippage often poses a life-threatening risk. Vigilant monitoring for rebleeding is imperative after successful initial hemostasis with EBL, and a predefined management strategy for early band slippage-related rebleeding must be established. Although EVO is associated with a relatively high rebleeding rate, such rebleeding events are typically manageable. Additionally, EVO demonstrates a low recurrence rate and an extremely rare incidence of fatal pulmonary embolism38. When technically feasible, EVO remains a viable option for controlling GV bleeding. However, for cases with large gastrorenal shunt, EVO should be selected with caution.
This study has limitations when considering the application of the findings in clinical practice. First, the follow-up period was short (6 months), which affected the observation of the long-term efficacy of EBL in the treatment of GV. Second, because studies on large-volume band ligators are limited, we estimated the 6-month cumulative rebleeding rate based on data for the six-shooter ligator to calculate the minimal sample size. However, we also increased our actual sample size to make the results more credible. Third, formal cost-effectiveness assessment was not conducted to guide emergency endoscopic hemostasis in active GV bleeding, warranting future research. Additionally, a control comparison with small-volume ligators is required. Therefore, future randomised controlled trials with large sample sizes and long-term follow-up are needed to support the safety and efficacy of EBL with large-volume ligators in the treatment of GV rupture and active bleeding.
Conclusions
Our findings indicate that the short-term efficacy of EBL with large-volume ligators in the treatment of actively bleeding GV is similar to that of EVO, but postoperative rebleeding is often more dangerous in EBL than in EVO. Therefore, EBL represents a viable alternative in emergency endoscopic control of GV bleeding, provided that a contingency plan for early band slippage-related rebleeding is implemented. Importantly, our findings provide up-to-date evidence of the efficacy of EBL in the treatment of active GV bleeding.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Tseng, Y. et al. Thromboembolic events secondary to endoscopic cyanoacrylate injection: Can we foresee any red flags?. Can J. Gastroenterol. Hepatol. https://doi.org/10.1155/2018/1940592 (2018).
Northup, P. G. & Caldwell, S. H. Treatment of bleeding gastric varices. J. Gastroenterol. Hepatol. 20(11), 1631–1633. https://doi.org/10.1111/j.1440-1746.2005.04042.x (2005).
D’Amico G, De Franchis R, Cooperative Study Group. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology 38(3), 599–612. https://doi.org/10.1053/jhep.2003.50385 (2003).
Rao, A. S. et al. Combined endoscopic-interventional radiologic approach for the treatment of bleeding gastric varices in the setting of a large splenorenal shunt. Gastrointest Endosc. 76(5), 1064–1065. https://doi.org/10.1016/j.gie.2011.10.013 (2012).
Hwang, J. H. et al. The role of endoscopy in the management of variceal hemorrhage. Gastrointest Endosc. 80(2), 221–227. https://doi.org/10.1016/j.gie.2013.07.023 (2014).
Lim, Y. S. Practical approach to endoscopic management for bleeding gastric varices. Korean J. Radiol. 13(11), S40–S44. https://doi.org/10.3348/kjr.2012.13.S1.S40 (2012).
Probst, A. et al. Portal vein embolism after injection of cyanoacrylate for bleeding gastric varices. Gastrointest Endosc. 90(1), 161–162. https://doi.org/10.1016/j.gie.2019.03.012 (2019).
Mansoor-Ul-Haq, M. et al. Treatment of bleeding gastric varices by endoscopic cyanoacrylate injection: A developing-country perspective. Cureus. 12(2), e7062. https://doi.org/10.7759/cureus.7062 (2020).
Frassei, J. D. S. et al. Cyanoacrylate pulmonary embolism after endoscopic sclerotherapy of gastric varices. Einstein (Sao Paulo) 19, eAI5778. https://doi.org/10.1744/einstein_journal/2021AI5778 (2021).
Monsanto, P. et al. Endoscopic treatment of bleeding gastric varices with histoacryl (N-butyl-2-cyanoacrylate): A South European single center experience. Indian J. Gastroenterol. 32(4), 227–231. https://doi.org/10.1007/s12664-012-0191-3 (2013).
Belletrutti, P. J. et al. Endoscopic management of gastric varices: efficacy and outcomes of gluing with N-butyl-2-cyanoacrylate in a North American patient population. Can J. Gastroenterol. 22(11), 931–936. https://doi.org/10.1155/2008/389517 (2008).
Choi, M. H. et al. The secondary prophylactic efficacy of beta-blocker after endoscopic gastric variceal obturation for first acute episode of gastric variceal bleeding. Clin. Mol. Hepatol. 19(3), 280–287. https://doi.org/10.3350/cmh.2013.19.3.280 (2013).
Robles-Medranda, C. et al. Endoscopic ultrasonography-guided deployment of embolization coils and cyanoacrylate injection in gastric varices versus coiling alone: A randomized trial. Endoscopy 52(4), 268–275. https://doi.org/10.1055/a-1123-9054 (2020).
Kozieł, S. et al. Endoscopic ultrasound-guided treatment of gastric varices using coils and cyanoacrylate glue injections: Results after 1 year of experience. J. Clin. Med. 8(11), 1786. https://doi.org/10.3390/jcm8111786 (2019).
Baig, M., Ramchandani, M. & Puli, S. R. Safety and efficacy of endoscopic ultrasound-guided combination therapy for treatment of gastric varices: A systematic review and meta-analysis. Clin. J. Gastroenterol. 15(2), 310–319. https://doi.org/10.1007/s12328-022-01600-0 (2022).
Yoshida, H. et al. New methods for the management of gastric varices. World J. Gastroenterol. 12(37), 5926–5931. https://doi.org/10.3748/wjg.v12.i37.5926 (2006).
Lo, G. H. et al. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology 33(5), 1060–1064. https://doi.org/10.1053/jhep.2001.24116 (2001).
Seleem, W. M. & Hanafy, A. S. Management of different types of gastric varices with band ligation: A 3-year experience. Eur. J. Gastroenterol. Hepatol. 29(8), 968–972. https://doi.org/10.1097/MEG.0000000000000893 (2017).
Singh, V. et al. Propranolol vs. band ligation for primary prophylaxis of variceal hemorrhage in cirrhotic patients with ascites: A randomized controlled trial. Hepatol. Int. 16(4), 944–953. https://doi.org/10.1007/s12072-022-10361-4 (2022).
Shi, D. & Liu, J. Comparing large-volume band ligators and cyanoacrylate injection for gastric variceal eradication: A prospective study. Medicine 101(46), e31939. https://doi.org/10.1097/MD.0000000000031939 (2022).
Abby Philips, C. & Sahney, A. Oesophageal and gastric varices: Historical aspects, classification and grading: Everything in one place. Gastroenterol. Rep. (Oxf). 4(3), 186–195. https://doi.org/10.1093/gastro/gow018 (2016).
Zhang, M. et al. Clip-assisted endoscopic cyanoacrylate injection for gastric varices with a gastrorenal shunt: A multicenter study. Endoscopy 51(10), 936–940. https://doi.org/10.1055/a-0977-3022 (2019).
Hashizume, M. et al. Endoscopic classification of gastric varices. Gastrointest Endosc. 36(3), 276–280. https://doi.org/10.1016/s0016-5107(90)71023-1 (1990).
Xu, X. et al. Guidelines for the management of esophagogastric variceal bleeding in cirrhotic portal hypertension. J. Clin. Transl. Hepatol. 11(7), 1565–1579. https://doi.org/10.14218/JCTH.2023.00061 (2023).
Tan, P. C. et al. A randomized trial of endoscopic treatment of acute gastric variceal hemorrhage: N-butyl-2-cyanoacrylate injection versus band ligation. Hepatology 43(4), 690–697. https://doi.org/10.1002/hep.21145 (2006).
Park, S. J. et al. Cyanoacrylate injection versus band ligation for bleeding from cardiac varices along the lesser curvature of the stomach. Clin. Mol. Hepatol. 22(4), 487–494. https://doi.org/10.3350/cmh.2016.0050 (2016).
Kamani, L. et al. Safety of endoscopic N-butyl-2 cyanoacrylate injection for the treatment of bleeding gastric varices in children. Pak. J. Med. Sci. 34(6), 1363–1368. https://doi.org/10.12669/pjms.346.16044 (2018).
Elsebaey, M. A. et al. Endoscopic injection sclerotherapy versus N-butyl-2 cyanoacrylate injection in the management of actively bleeding esophageal varices: A randomized controlled trial. BMC Gastroenterol. 19(1), 23. https://doi.org/10.1186/s12876-019-0940-1 (2019).
Liu, X. et al. A retrospective cohort study of intensive gastric variceal ligation versus endoscopic gastric variceal obturation in the management of gastric variceal bleeding. Ann. Palliat. Med. 11(3), 1038–1047. https://doi.org/10.21037/apm-22-138 (2022).
Tantau, M. et al. Band ligation vs. N-butyl-2-cyanoacrylate injection in acute gastric variceal bleeding: A prospective follow-up study. Ann. Hepatol. 13(1), 75–83 (2013).
Lee, M. S. et al. Use of detachable snares and elastic bands for endoscopic control of bleeding from large gastric varices. Gastrointest. Endosc. 56(1), 83–88. https://doi.org/10.1067/mge.2002.125104 (2002).
Puente, A. et al. Drugs plus ligation to prevent rebleeding in cirrhosis: An updated systematic review. Liver Int. 34(6), 823–833. https://doi.org/10.1111/liv.12452 (2014).
Mansour, L. et al. Randomized controlled trial of scleroligation versus band ligation alone for eradication of gastroesophageal varices. Gastrointest Endosc. 86(2), 307–315. https://doi.org/10.1016/j.gie.2016.12.026 (2017).
Sugimoto, N. et al. Endoscopic hemostasis for bleeding gastric varices treated by combination of variceal ligation and sclerotherapy with N-butyl-2-cyanoacrylate. J. Gastroenterol. 42(7), 528–532. https://doi.org/10.1007/s00535-007-2041-0 (2007).
Elwakil, R. et al. N-butyl-2-cyanoacrylate, iso-amyl-2-cyanoacrylate and hypertonic glucose with 72% chromated glycerin in gastric varices. World J. Gastrointest Endosc. 7(4), 411–416. https://doi.org/10.4253/wjge.v7.i4.411 (2015).
Kang, E. J. et al. Long-term result of endoscopic histoacryl (N-butyl-2-cyanoacrylate) injection for treatment of gastric varices. World J. Gastroenterol. 17(11), 1494–1500. https://doi.org/10.3748/wjg.v17.i11.1494 (2011).
Chi, X. T. et al. Advances in the endoscopic management of gastric varices. Dig. Endosc. 36(8), 884–894. https://doi.org/10.1111/den.14770 (2024).
Prasoppokakorn, T. & Rerknimitr, R. An unusual complication of endoscopic cyanoacrylate injection for gastric varix. Gastroenterology 163(5), 1186–1187. https://doi.org/10.1053/j.gastro.2022.06.002 (2022).
Harth, C. et al. Fatal acute pulmonary embolism following endoscopic cyanoacrylate injection for gastric fundal varices. Acta Gastroenterol. Belg. 87(4), 531–534. https://doi.org/10.51821/87.4.13020 (2024).
Burke, M. P., O’Donnell, C. & Baber, Y. Death from pulmonary embolism of cyanoacrylate glue following gastric varix endoscopic injection. Forensic. Sci. Med. Pathol. 13(1), 82–85. https://doi.org/10.1007/s12024-016-9835-4 (2017).
Cheng, L. F. et al. Low incidence of complications from endoscopic gastric variceal obturation with butyl cyanoacrylate. Clin. Gastroenterol. Hepatol. 8(9), 760–766. https://doi.org/10.1016/j.cgh.2010.05.019 (2010).
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding
This work was supported by the Medical Scientific Research Foundation of Zhejiang Province, China (Grant No. 2022KY326). The funding agency had no role in the study design, data collection/analysis/interpretation, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
DS and GX contributed to study conception and design. All authors contributed to the acquisition and analysis of data. DS and WP contributed to data interpretation. GX drafted the manuscript, and DS revised the manuscript critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shi, D., Xu, G. & Pan, W. A randomized controlled trial comparing large-volume band ligator and cyanoacrylate injection in the endoscopic management of actively bleeding gastric varices. Sci Rep 15, 27134 (2025). https://doi.org/10.1038/s41598-025-12600-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-12600-8